Lifespan Development Exam 1 (Weeks 3-5)
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
The five sensory contributors to cognition (in order)
Touch (1st)
Proprioceptive/Vestibular
Smell/Taste
Auditory
Vision (Last)
Basic elements of cognitive development
Visual attention (1-4 months)
Spatial relationships (4-10 months)
Cause and effect (10-12 months)
Trial and error (12-18 months)
Basic elements of psychosocial development
Diffuse attachments (0-6 months)
Separation anxiety “attachment to primary caregiver” (6-12 months)
Multiple attachments/affection (12-18 months)
Expresses feelings (18-24 months)
Concern for autonomy (2-3 years)
Basic elements of speech and language development
Babbling, cooing (0-6 months)
Single words (6-12 months)
20-100 words (12-24 months)
Basic elements of oral motor development
Suck, swallow, breathe priority (0-6 months)
Against-gravity movement of body segments allowing for eating semi-solids, solids, and mouthing of toys (by 12 months)
Sound production (by 12 months)
suck swallow breath
liquid ingestion
active oral pattern expanded to vertical movements of the jaw and tongue
controlled movement against gravity and coordinated
Basic elements of fine motor development
Eyes on a target (by 3 months) - first locates the target visually
Eye-head tracking (2-5 months) - the head joins the eyes on the target
Functional reach and grasp – what main systemic components are required?
ALL MUST BE PRESENT
Visual fixation
Anticipatory adaptation
Proximal stability
Manual capture and release
Object manipulation
In-hand manipulation
Fast twitch fibers required → precise movement
Shift (hand manipulation)
Movment of an object on the surface OR among fingers
Rotation (hand manipulation)
Movment of an object around its axis
Translation/Penny test
Movement from finger → palm AND palm → finger
Describe the importance of play in develompment
Play is their exercise.
Play is more related to sensory-motor interaction (0-2 years)
Order of types of play by age (don’t need to know years?)
pretend by 2 years
role-play by 3 years
constructive play by 2 years,
Rule games by 6 years
complex rule games by 10 years.
3 Stages of play (infancy, one year, school)
Infancy: Repetitive gross motor activity without purpose
Improves control of motor patterns, provides stimulation for visual and auditory development, and increases strength and endurance
One-year: Exercise play (running, chasing)
School age: Rough and tumble, aids in socialization → aggression vs. play
Self-centered play
(year 1): Child is playing alone
Parallel play
(Year 2-4): Children play alongside each other but NOT with each other
Cooperative play
(Year 4-5): They play together, take turns, and influence each other
Social interaction of play (years)
5-7 years: observation of rules
7-12 years: circle of friends outside family
12-16: team sports, driven socially, intellectually, and artistically
Define the mechanostat theory and how it contributes to bone development
Mechanical input is used to develop effeicient load-bearing bones → bones adapt to the mechanical strain placed upon them by the pull of muscles or gravity in weight bearing positions.
Otherwise, osteoclast activity is favored = ↑ bone resorption due to lack of exposure to strain. This is how we develop osteopenia and osteoporosis
Newborn femur features
The angle of inclination is GREATER than in the adults
Weightbearing has a major role in ↑ congruency with the acetabulum
How does muscle contraction assist bone growth?
As muscle pulls on bone, it creates a traction force that increases density according to the mechanostat theory
Osteoporosis, how do we slow the process?
It becomes accelerated with:
Reduced calcium intake (diet or due to medications that ↓ Ca+ reabsorption)
Intestinal calcium absorption DECREASES with age
How to help?
Require Vitamin D supplements to enhance Ca+ absorption
Describe joint changes in older adults (65 +)
Joints become stiffer (↓flexible) due to losing synovial fluid (lubrication)
This can also be to to inactivity and aging structural changes
Cartilage becomes thinner
Decrease in elastic fibers
Ligament and cartilage degeneration
Ages for growth spurs
1-4 years
10 years
How does PA impact length, size, curvature, and shape of bone?
PA BEFORE puberty supports growth in bone and muscle mass
HIgh impact activities → ↑bone growth (mechanostat theory)
This sets up the individual for optimal bone function across the lifespan
LE + pelvic changes as infant begins to move
LEs + pelvis undergo angular, rotational and length changes
These changes also occur in the tibia + ankle/foot complex. ER of the tibia increases from newborn → adult
This relationship changes from genu varum → genu valgus by 3 years old
Stabilizes by 7 years → then ↓ by 5 degrees
Femoral angle of inclination decreases = improved lever arm for ABDuctors
How does the spine and curvatures develop?
Cervical LORDOSIS present at birth (early ossification of the occipital bone)
More evident by 3 months due to head control development
Lumbar LORDOSIS develops as the infant learns to sit ~8 months
When is skeletal maturity obtained?
epiphyseal plates close by age 25
Can bone lengthen after epiphyseal plate closure?
No, but it can still change in denisity
What factors contribute to IV disk changes in adults >30?
Nucleus pulposus loses ability to absorb water → becomes dehydrated → ↓ ability to work as a shock absorber
Nucleus fibrous becomes fibrotic? → disk flattened and less resilient
Incidence of back pain reported between 30-50
Osteopenia
Organic or inorganic components of bone fail to develop
Osteomalacia
Abnormal bone mineralization of matrix. Due to Ca+, vitamin D, or increased reabsorption. Bone chemistry is normal
Osteoporosis
Reduction in bone mass due to decreased formation or increased reabsorption, while bone chemistry is normal
Contributing factors: Hormones, diet, ↓ and activity
H: ↓ estrogen = ↑ bone reabsportion
D: lack of vitamin D and calcium
Does bone grow faster than muscle, and if so, what are the implications?
Yes. Muscles can become tight, and if there is also a neurological or fibrous diagnosis, this can easily become contracture.
Type I Fibers
Slow twich, small, fatigue resistant. POSTURAL (SOLEUS)
Type II Fibers
Fast twitch, large, aerobic and anaerobic. FAST MOVEMENTS (GASTROC)
Does prenatal development of muscle fibers rely on motor neurons? Proteins?
They rely on proteins prenatally during the fetal period. We do get differentiation of fibers in weeks 31-37.
What is the best predictor of strength in adolescence?
Height
In both boys and girls, what hormone has the biggest influence in early puberty?
Testosterone
Explain the strength decline in adults and older adults in terms of isometric and concentric strength
Decline in muscle strength starts at 50-70 years old (then rapid decline)
Concentric strength decreases more
Isometric strength decreased follows
Eccentric strength is maintained better in older adults
What is sarcopenia? How can we avoid the effects of sarcopenia in older adults?
loss of flesh” – Loss of muscle mass, quality, and strength seen during normal aging
↑ intramuscular and body fat levels
Decline of strength in the muscle mass remaining is due to the decline in muscle quality
Need to help them stay active, nutritional counseling, and functional training (balance too).nutritional
What is apoptosis?
Programmed cell death that is inevitable with aging.
Does resistive exercise negatively impact growth and development in children?
NO
Are maximal weight lifts and competition-style weightlifting recommended in adolescents before skeletal maturity?
No. Need skeletal maturity first. (ACSM)
Is frailty in older adults a contraindication to exercise?
No but you need to know their tolerance and progress accrodingly
Can older adults still improve and regain function with training?
Yes
Before birth, circulation permits most of the oxygenated blood to bypass the liver and lungs via which three shunts?
Ductus venosus
Ductus arteriosus
Foramen ovale
These will close “neonate” (as soon as they are born)
What regulates the HR and contractiliy?
Originiates in the medulla → carried by the autonomic nervous system (ANS - PNS + SNS)
How do the sympathetic and parasympathetic systems affect HR and vasoconstriction/dilation?
SNS: ↑HR and contractility (EPI and NE) / ↑ vasoconstriction
PNS: ↓HR and contractility (Ach via vagus n.) / ↑ vasodilation
Where/what are the receptors that relay sensory information to the ANS and what is their role in BP regulation?
Baroreceptors and chemoreceptors relay sensory information through the NS. They detect changes in BP, oxygen and CO2 levels, and pH in blood.
Baroreceptors in aorta and cortid sinus (stretch)
Chemoreceptors in the aortic and carotid bodies
How do the SNS and PNS affect the pulmonary system?
SNS: BronchoDILATION
Remember that you need your lungs “open” when you are running from a bear :)
PNS: Bronchoconstriction
What coordinates the rythmic ventilatory cycle and mantain the depth of ventilation?
Brain stem centers (3 - PNS/SNS/Motor) in the medulla and pons
How is bloodflow regulated in the system?
By pressures exterted by various structures
Preload
Amount of pressure needed to stretch the ventricles during filling
Afterload
Amount of pressure needed to be exterted by the ventricles to overcome aortic pressure (open the valve → push blood out to the periphery)
Components of the conduction portion of the CP system
Bronchi - hyaline cartilage + smooth muscle
Bronchioles - smooth muscle + elastic fibers
PNS system input via vagus nerve - contraction of smooth muscle cells that changes the diameter (↓) of the bronchial tree
Components of the respiratory portion of the CP system
Branches of the bronchial tree
Alveolar ducts
Alveolar sacs
Alveoli
What is the difference between the conductive and respiratory bronchioles?
The respiratory bronchioles contrain alveoli along their walls
Where does gas exchange take place?
In the capillaries
What is surfactant? What produces it?
A detergent-like substance that mixes with water to decrease alveolar surface tension; allowing the alveoli to open more easily during respiration.
Produced by Type II Epithelium
Without surfactant, what condition can occur?
Atelectasis- alveolar collapse
Identify the muscles involved in breathing - “Ventilatory pump”
Controls the flow of air, using:
Diaphragm
Rib cage musculature (intercostals, parasternals, scalenes, and SCM)
Abdominal muscles
Why are chemoreceptors important? Where are they located?
Detect changes in the blood levels of oxygen and CO2, and pH of the blood, which → stimulates appropriate respiratory changes
Located in the aortic and carotid bodies
Order of events with mechanics of ventilation
Inspiration:
intercostal muscles contract to elevate the rib cage
The diaphragm also contracts, increasing the diameter of the thoracic cavity
Together, the plural cavity expands and results in increased negative pressure in the thoracic cavity
Atmospheric air rushes in, and the lungs expand
This expansion activates stretch receptors, inhibiting inspiration
Exhalation:
Exhalation occurs passively with muscle relaxation and elastic recoil
Inhibitory input to inspiration is decreased, once again activating inspiration
When can a prenatal heartbeat be detected?
At 22 DAYS of gestation
In the prenatal time frame, what provides the baby with oxygen saturation of the blood?
Oxygen saturation of blood is from the umbilical circulation until birth when nearly all independent oxygen saturation occurs at birth within minutes.
When is surfactant first produced
At 20-22 weeks of gestation
What are the CV and Pulmonary adjustments made at birth?
Fluid inside the lungs is pushed out through the nose and mouth during labor. Remaining fluid is drained by the pulmonary vessels and the lymphatic system → The infant breathes spontaneously
Blood is shunted into the pulmonary circulation to recieve oxygen from the alveoli
Occlusion of the umbilical cord → ductus venosus (IVC) closes = decrease in pressure in IVC and RA
The foramen ovale and ductus arteriosus of the heart close
This marks the full transition into adult-like circulation
Can hypertension be a problem in both children and adults? And what are the health risks to hypertension?
Yes for both! Poor nutrition (high in sugar and fat), smoking.
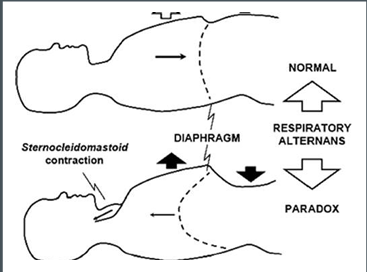
Define paradoxical breathing
The belly protrudes with inhalation instead of the chest expanding (chest sinks instead).
NOT normal if:
child is older than 3-6 months (when the rib cage and its musculature develop)
can happen with disease, frail chest injuries, and paralysis of the cervical levels and T6-12.
At what age is the muscle developed in the walls of arteries found at alveoli?
At 19 years old
Age-related changes of the heart
Hypertrophy of cardicac cells, but hypoplasia (↓#)
Heart valves become stiffer (calcify)
pacemaker heart cells in the SA node decrease
pseudohypertrophy and thickening in the L ventricle
HR decreases
BP increases
↓ vascular compliance = ↑ resting BP
Premature ventricular contractions (PVCs) are seen in older adults, due to changes in the conduction system
Describe the age related changes in vasculature
Vessels are thicker, rigid, and dilated (↓efficiency)
Thickening of the elastic arteries, fragmenting the fibers, leading to lipid infiltration and calcification
This makes vasodilation and vasoconstriction more difficult
Become more prone to orthostatic hypotension
T/F: Dilation of vessels occurs in distal vessels, while the proximal vessels show a thickening of the arterial wall with age
FALSE. Dilation occurs PROXIMALLY (in the aorta), then the arterial wall thickens in the PERIPHERAL vessels
Arteriosclerosis
Decrease arterial compliance due to age-related changes
Atherosclerosis
PATHOLOGICAL deposition of plaques in the inner layer of a blood vessel
This can be prevented with regular aerobic and endurance exercise = ↓ CVD risk
Age-related losses (summary by Dr. Morgan)
CO (Q) and oxygen uptake decrease with age
Reduced baroreceptors activity
Decreased adaptability of the CVS
Decreased SNS responses to drops in BP (orthostatic hypotension risk)
Decreased ability to ↑ heart rate
Decreased contractility
Decreased ability for vasodilation of the vessels in response to stress
T/F:While older adults are still trainable and can respond to the benefits of exercise, they need to continue to be consistent with exercise to lower BP over time truly
True
Decreased strength, ANS control, muscle enzyme levels, and the size of capillary networks all contribute to _________________
Functional losses
Age related changes to the pulmonary system
Stiff bony thorax
Osteoporosis and poor posture
↓ lung elasticity and compliance
Insufficient respiratory musculature
↓ Alveolar surface area
↓ Pulmonary blood flow and volume