Internal Environment: Oxygen & Carbon Dioxide (PHYSIOLOGY E2: Part 4)
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
What are Partial Pressure Gradients?
Based upon percentages
PN2 → 600 mmHg
PO2 → 160 mmHg
PCO2 → 0.3 mmHg
**** DO NOT MEMORIZE THESE VALUES ****
NOT IMPORTANT
Dissolved in blood
Dependent upon solubility
Establishes partial pressure gradients
What are the Different Partial Pressures of Alveolar Air?
These are values in Alveolar / Arterial blood
PH2O → 47 mmHg
PN2 → 563 mmHg
PO2 → 150 mmHg lowered to 100 mmHg
Need to know PO2 → 100 mmHg
Small fluctuations
2,200 mL RV & 350 mL fresh
PCO2 → 40 mmHg
Also need to know PCO2 → 40 mmHg
DO NOT MEMORIZE THESE VALUES!!! (Except 100 & 40 mmHg)
O2 / CO2 Net Diffusion Gradients between Lung & Tissues Diagram
The Only important values you need to know:
PO2 → 100 mmHg
PO2 in arterial blood
PCO2 in alveoli → 40 mmHg
PCO2 in arterial blood (even though its in pulmonary vein)
Due to no gas exchange (go thru heart, no gas exchange)
When get to aorta & all arterioles, at arterial end of capillary:
PO2 —> 100 mmHg
PCO2 → 40 mmHg
When we get to tissues, our tissues are burning Oxygen
So PO2 is less than (<) 40 mmHg
Tissues are producing CO2
So PCO2 → greater than (>) 46 mmHg (but equilibrates to 46)
Need to know these numbers for venous blood because thats what goes up for Gas exchange
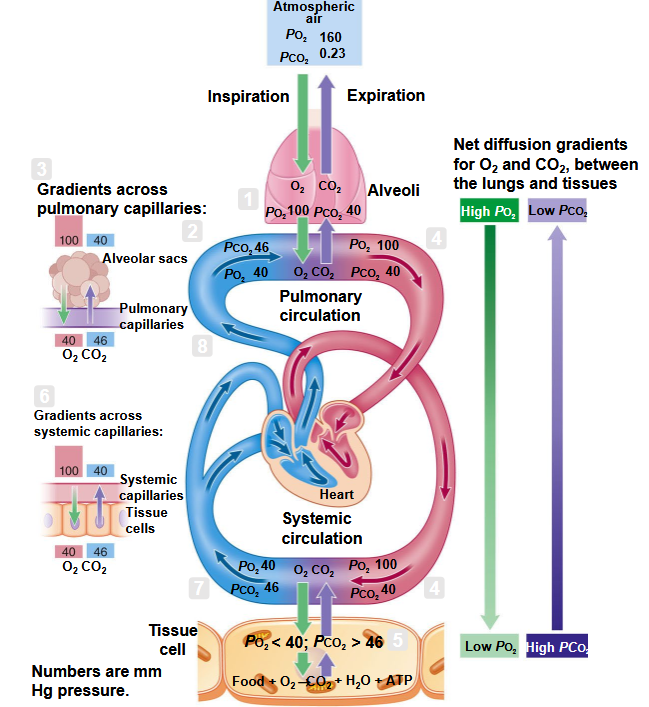
How is Gas Exchanged?
Venous PO2 → 40 mmHg
Venous PCO2 → 46 mmHg
Travels down concentration gradients (partial pressure gradient)
If we increase the difference, we increase the rate of exchange
Increasing difference increases exchange
What influences Gas Exchange?
Surface Area (SA)
Membrane thickness
Solubility
CO2 more soluble than O2
Diseases
Increase membrane thickness
Reduction in surface area (SA)
Hoping to Train to See:
If Patient has Respiratory Disorder → They probably have acid-base disorder b/c ability to compensate is impaired (for metabolic acidosis or smth like that)
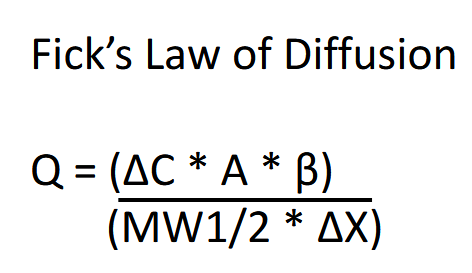
Fick’s Law of Diffusion
Q = ((ΔC x A x β) / (MW (1/2) x ΔX))
How is Oxygen Transported?
Poorly soluble in plasma (1.5%)
Attached to hemoglobin (Hb)
98.5%
Reduced Hb → not combined with oxygen
Oxyhemoglobin → Oxygen combined with the iron (heme) group
Hemoglobin saturation
What is the Law of Mass Action?
Reversible Reaction
Hb + O2 ←→ HbO2
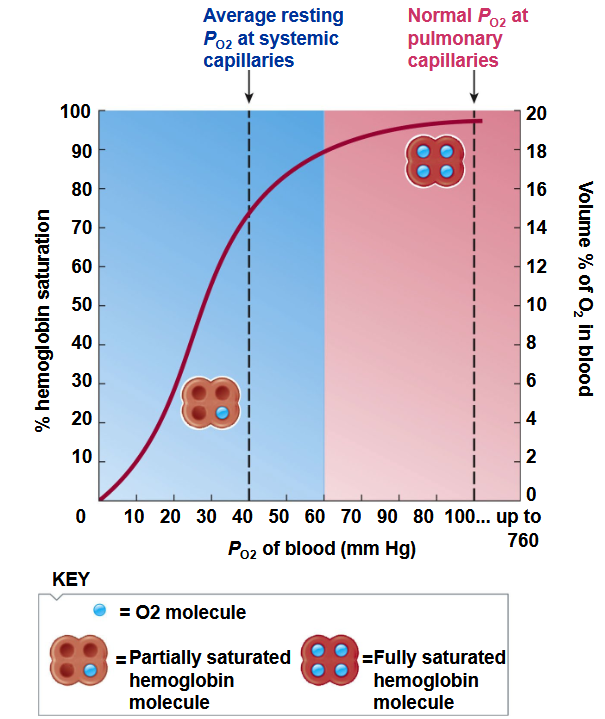
What is the Oxygen-Hemoglobin Saturation Curve
Utilizes the Law of Mass Action (reversible)
We have oxygen + hemoglobin = oxyhemoglobin (can go backwards)
If have high Oxygen & high hemoglobin, will form oxyhemoglobin
If get to tissues & have low oxygen, & a lot of oxyhemoglobin → will release Oxygen & form hemoglobin independent
PO2 and Percentage (%) Hemoglobin (Hb) saturated
PO2 100 mmHg = 97.5% Hb saturated
PO2 60 mmHg = 90% Hb saturated
DO NOT MEMORIZE THESE NUMBERS
Just know curve & what curve means
PO2 is dissolved
% Hb saturated is what’s bound to hemoglobin
what’s bound to hemoglobin comes off & replaces what’s dissolved (used by tissue)
Steep portion
As blood PO2 falls, Hb releases more O2
As PO2 in tissues gets lower, hemoglobin releases more oxygen (in non-linear way)
Break in color (Blue to Pink)
At 60 PO2 → at that point, if PO2 in arterial blood was 60, that would trigger emergency respiration & oxygen need
That break in color is when we switch from CO2 driving Respiration to Oxygen Driving Respiration
CO2 particularly hydrogen generated by CO2 is what drives normal day-to-day respiration
Oxygen doesn’t b/c we don’t get that low
EX in Class: Euthanasia in Vets (Agonal Breathing)
PO2 has dropped to emergency respiration point
brain is already dead but PO2 has dropped to point that reflexes in carotid body trigger emergency respiration
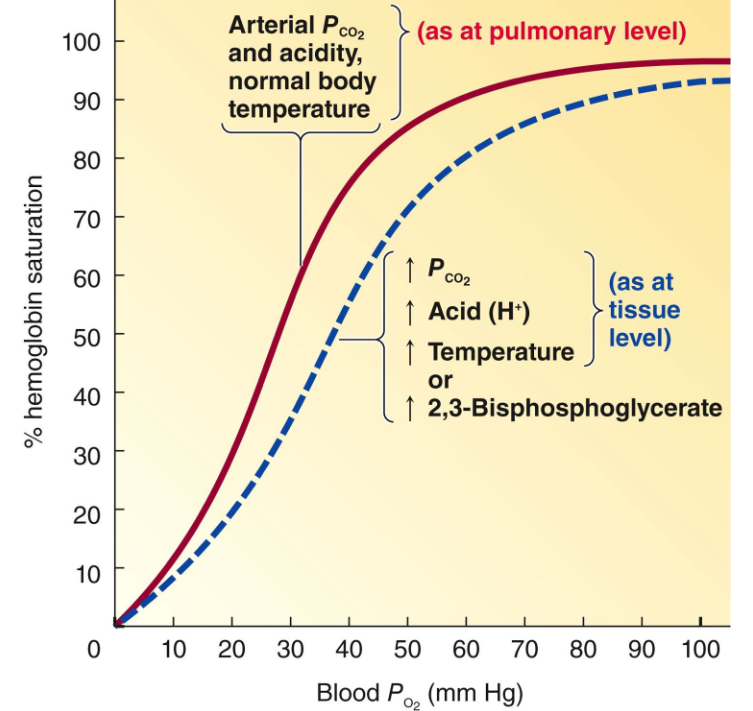
What are the Influences of Oxygen Affinity?
Increased (↑) CO2 causes Hb to release more O2
Shifts curve to Right
More metabolic activity (more CO2), shift to right
Decreased (↓) CO2 causes Hb to release less O2
Shifts to the Left
Increased (↑) H+ concentration (decrease pH)
Shifts curve to Right
Increased H+ Concentration (decreasing pH) due to more metabolic activity
Decreased (↓) H+ causes Hb to release less O2
Shift to Left
2,3-diphosphoglycerate (2,3-DPG)
Shifts Right
Carbon Monoxide (CO)
Shifts Left (Carboxyhemoglobin)
Increase (↑) in Temperature
Shifts Right
Decrease (↓) in Temperature
Shifts Left
Left Shifts are All Pathologic
Right Shift can be Pathologic or Physiologic
Partial Pressure of Blood Oxygen (O2) vs. Percentage (%) Hemoglobin Saturation Graph
Right Shifted Curve (Factors That Shift Curve to Right)
Curve physically shifted to right hand side graph
Factors that Shift to Right:
PCO2
ACID (H+)
Increase (↑) Temperature
Increase (↑) 2,3-Bisphosphoglycerate
Under these conditions, hemoglobin releases more oxygen to the tissues
Hemoglobin has to transport & release it
In Right Shift → causes tissues to have higher Oxygen Availability
Tissues are well-oxygenated in conditions of right shift
EX: Dozing off in class
Shift off to right curve
Resp rate drops, CO2 builds up, but tissues very well oxygenated b/c shifted to the right
Hemoglobin is releasing more than usual amount oxygen to tissues
In a Left Shift Curve:
In alkalosis, we’re shifting to Left
Tissues are hypoxic & have tendency to go into ventricular fibrillation
Right Shift in Heart:
Delivers 80% oxygen to tissue (20% hemoglobin saturation)
In a HARD RIGHT SHIFT, Hemoglobin doesn’t saturate
hemoglobin gets to lungs & hemoglobin can’t carry oxygen from alveoli
Begins to carry less oxygen to tissue
PATHOLOGIC RIGHT SHIFT
EX: Really high fever, severe acidosis
Hemoglobin doesn’t pick up O2, doesn’t saturate well
Fetal Hemoglobin:
Left Shifted Curve
Need more Oxygen, but doesn’t have big partial pressure differences
Hemoglobin has to load much better
Myoglobin
Even further & is LEFT SHIFT
Myoglobin in muscle is terminal thing
Myoglobin holds Oxygen for the exercising muscle
Myoglobin in exercising muscle gets very close to 100% saturated at 10 mmHg
Left shift in myoglobin helps maintain oxygen available for exercise
What happens in a Left Shift in Saturation Curve?
Our tissue is more like 8% oxygenated (8% delivered to tissue)
92% hemoglobin saturated (oxygen still in hemoglobin)
Tissues are hypoxic
In the heart Saturation Curve (20 mmHg)
Only deliver ~40% of oxygen to tissue
Need ~65% oxygen delivery to tissue to function normally
Heart tissue will be hypoxic
heart will fibrillate
For Pts in hypothermia, have high risk of ventricular fibrillation
How is Carbon Dioxide (CO2) Transported?
CO2 + H2O ←→ H2CO3 ←→ H+ + HCO3-
Reaction requires Carbonic Anhydrase
60% CO2 is transported as HCO3- (Bicarbonate)
#1 transport of CO2 is bicarb
30% CO2 transported as carbaminohemoglobin
#2 transport of CO2 is bound to globin portion of hemoglobin (called carbaminohemoglobin)
10% CO2 dissolved in Plasma
#3 Transport is physically dissolved in plasma
What is the Mechanism of Carbon Dioxide Transport?
All we need to know about Carbon Dioxide Transport
Picking up CO2 & Dropping off O2 in tissues
In lungs, we’re Dropping off O2 to tissues & picking up CO2 from Tissues
This is saying that oxyhemoglobin will drop off oxygen off, & hemoglobin will bind to CO2 to make Carbaminohemoglobin
Hemoglobin will bind to Hydrogen to make HbH (Hydrogen Hemoglobin)
Chloride Shift: Bicarbonate-Chloride Exchange
Should shift Bicarbonate out of tissue cell with antiport exchange pump
& shift chloride into cell
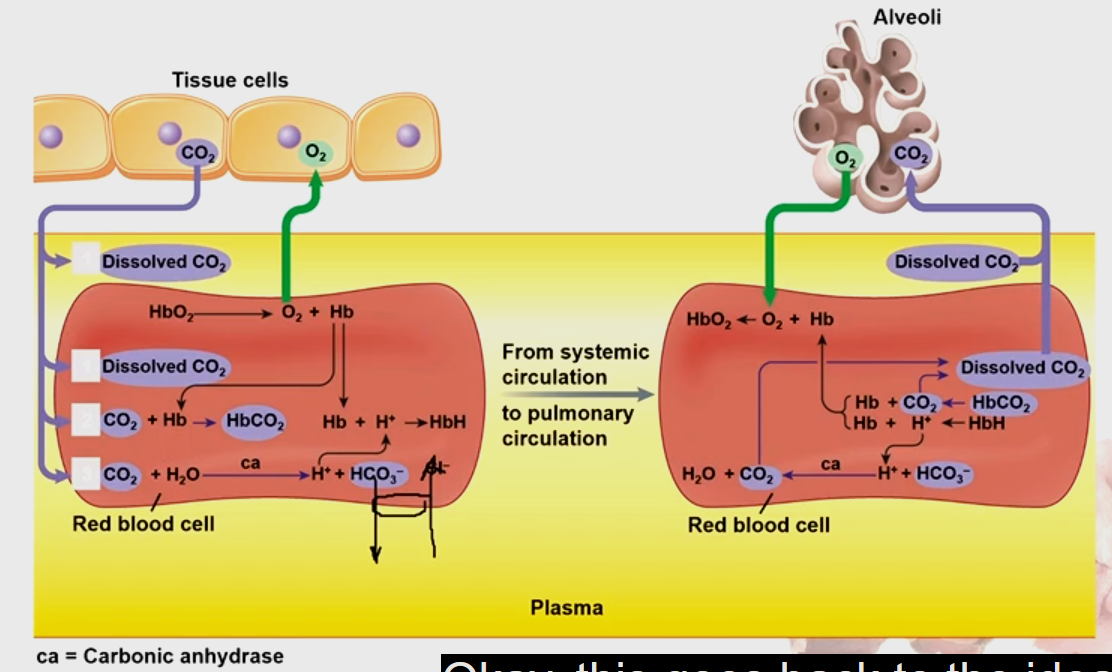
What Prevents Hydrogen from Recombining w/ Bicarbonate & going back to Water & Carbon Dioxide?
This is because Bicarbonate is pumped out of cell & no longer available
Chloride is in
Hydrogen dissociated from Hemoglobin & not allowed to interact with Bicarbonate & pumped out of cell
Differences between Bohr Effect vs. Haldane Effect?
Deals with Reduced Hemoglobin (which isn’t common)
Deals with more pathological conditions
What influences the Rhythmic Breathing Patterns?
Medullary Respiratory Center
Rostral Ventromedial Medulla (Pre-Botzinger Complex)
Pacemaker
Rely in Pre-Botzinger to breathe quietly
Feeds into Dorsal Respiratory Group (DRG)
Fires about every 5-6 sec & tells DRG to fire for 2 seconds & stop firing
Dorsal Respiratory Group (DRG)
Stimulation = Inspiration
DRG causes diaphragm to contract & cause (some) external intercostals to contract
In order to inhale (over 2 secs & stops)
Everything relaxes (to passively exhale)
Lack of stimulation = expiration
Ventral Respiratory Group (VRG)
Inspiratory & Expiratory Neurons
Active Inspiration & Expiration
VRG is triggered when you think about breathing (conscious thought)
Normal moment-by-moment quiet breathing is handled by medulla of brain
Fracture of C1 is often fatal (b/c takes out Pre-Botzinger or DRG)
Sometimes can take out either Pre-Botzinger or DRG
Patient has to continually think about breathing
Pontine Respiratory Centers
Pneumotaxic Center
Limits duration of Inhalation by the DRG
Tells DRG to stop inhaling
Apneustic Center
Prevents inhibition of the DRG
Tells DRG to keep inhaling
Both centers balance each other out
Pons augments & makes breathing look smooth
Damage to Pontine Centers (E.G. central pontine myelinolysis) causes ragged breathing
Phrenic Nerve
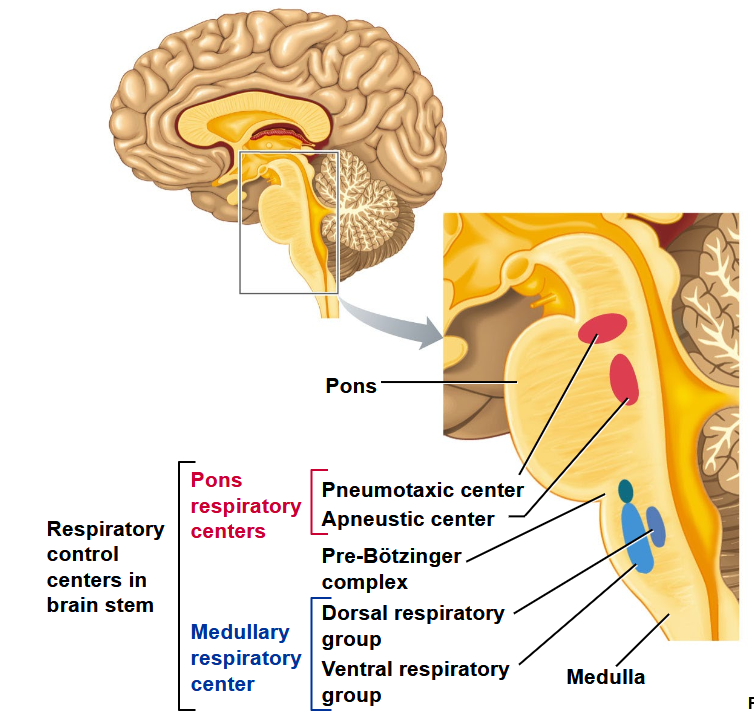
What is enough to handle quiet Breathing?
Pre-Botzinger Complex
Dorsal Respiratory Group (DRG)
Anytime we need modification to breathing, we pull in Ventral Respiratory Group (VRG)
Sympathetic NS changes bronchial diameter (dilate bronchioles) but doesn’t effect rate
Rate effected through high brain coming down & tying to Ventral Respiratory Group (VRG)
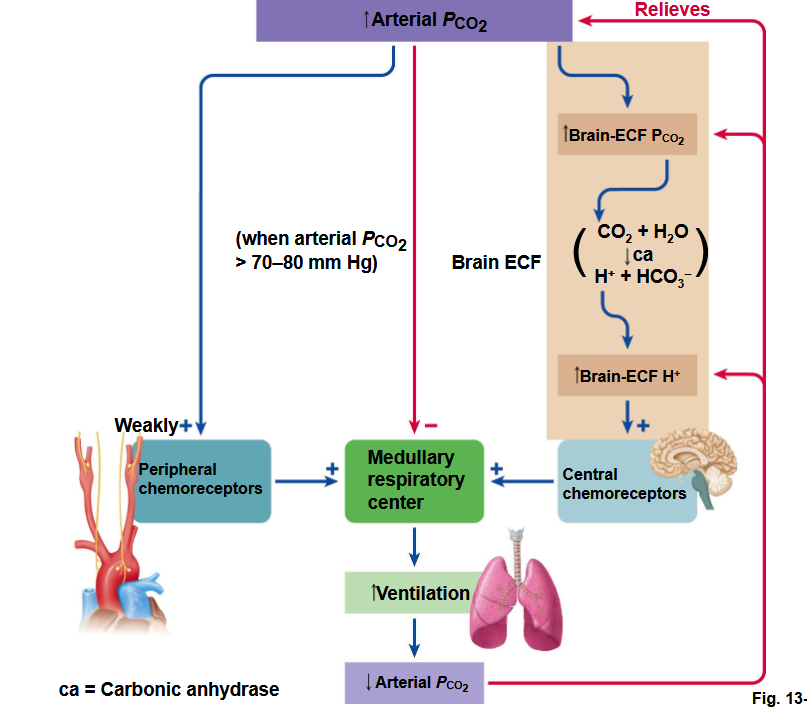
What are the Influences of Chemical Factors on Respiration?
Decrease in PO2 in Arterial Blood
Low Oxygen in Arterial Blood is only important when getting below (<) 60 mmHg (emergency mechanism)
EX: Agonal gasp/breathing at this area
Oxygen only has depressive effect on Central Nervous System (< 60 mmHg)
stop respiration (Respiration stops when O2 levels below 60)
happens at death
Increase in PCO2 in Arterial Blood (Increase in H+ in brain ECF)
CO2 itself in arterial blood only has weak stimulation
CO2 in Arterial blood converts to Hydrogen (H+) in brain
Hydrogen in brain dominate control of ventilation
When hyperventilating
Respiration stops b/c CO2 in brain is above 70-80 mmHg
happens during death
Increase [H+] in Arterial Blood
Important in Acid-Base Balance
** In most cases, they’re influencing the Pre-Botzinger (Pacemaker) **
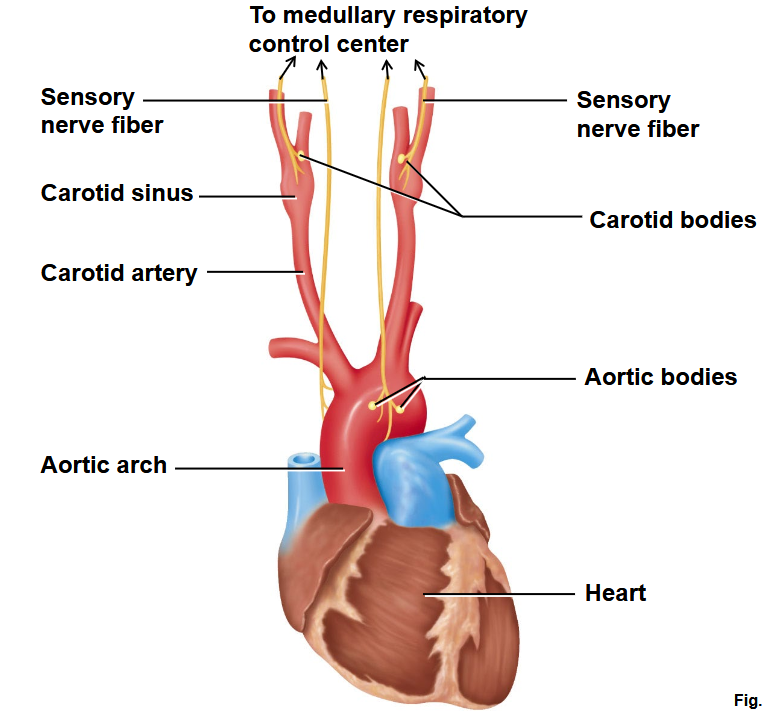
Have Peripheral Receptors & Central Receptors
Peripheral → aortic arch & carotid body receptors (same ones as blood pressure)
Central → Associated w/ Pre-Botzinger Complex
EX: What’s Danger of Sleep Apnea?
Hypertensive Crisis while Sleep
Wake up w/ possible scleral haemorrhage, or possible aneurysm
Due to Blood Pressure & Respiratory Centers (Peripheral) tied together
Normal Walk-around drive for respiration:
Hydrogen concentration in brain from CO2
![<ul><li><p>Decrease in P<sub>O2</sub> in Arterial Blood</p><ul><li><p>Low Oxygen in Arterial Blood is only important when getting below (<) 60 mmHg (emergency mechanism)</p><ul><li><p>EX: Agonal gasp/breathing at this area</p></li></ul></li><li><p>Oxygen only has <strong>depressive effect on Central Nervous System (< 60 mmHg)</strong></p><ul><li><p>stop respiration (Respiration stops when O2 levels below 60)</p><ul><li><p>happens at death</p></li></ul></li></ul></li></ul></li><li><p>Increase in P<sub>CO2</sub> in Arterial Blood (Increase in H+ in brain ECF)</p><ul><li><p><strong>CO<sub>2</sub> itself in arterial blood </strong>only has <strong>weak stimulation</strong></p></li><li><p><strong>CO<sub>2</sub> in Arterial blood converts to Hydrogen (H<sup>+</sup>) in brain</strong></p><ul><li><p>Hydrogen in brain <strong>dominate control of ventilation</strong></p><ul><li><p>When hyperventilating</p></li></ul></li></ul></li><li><p>Respiration stops b/c CO2 in brain is above 70-80 mmHg</p><ul><li><p>happens during death</p></li></ul></li></ul></li><li><p><strong>Increase [H+] in Arterial Blood</strong></p><ul><li><p>Important in <strong>Acid-Base Balance</strong></p></li></ul></li><li><p><strong><em>** In most cases, they’re influencing the Pre-Botzinger (Pacemaker) </em>**</strong></p></li><li><p><strong>Have Peripheral Receptors & Central Receptors</strong></p><ul><li><p>Peripheral → aortic arch & carotid body receptors (same ones as blood pressure)</p></li><li><p>Central → Associated w/ <strong>Pre-Botzinger Complex</strong></p></li></ul></li><li><p>EX: <strong>What’s Danger of Sleep Apnea?</strong></p><ul><li><p><strong>Hypertensive Crisis while Sleep</strong></p></li><li><p>Wake up w/ possible scleral haemorrhage, or possible aneurysm</p></li><li><p>Due to Blood Pressure & Respiratory Centers (Peripheral) tied together</p></li></ul></li><li><p>Normal Walk-around drive for respiration:</p><ul><li><p>Hydrogen concentration in brain from CO2</p></li></ul></li></ul><p></p>](https://knowt-user-attachments.s3.amazonaws.com/24a85d77-d09f-4521-83f1-a96c87a28c00.png)
Heart to Medullary Control Center Connection
How does the Medullary Respiratory Center regulate Arterial CO2 Partial Pressure (PCO2)?
Reason why hydrogen has to be tied to CO2 is because:
Hydrogen itself doesn’t cross blood-brain barrier b/c it’s ionized (charged)
CO2 is lipid-soluble so crosses blood-brain barrier to convert to Hydrogen in brain
Acid-Base Disorders Presentation (By: Dr. Wolfshohl)
Won’t ask any Specific questions on the exam regarding his slides
He doesn’t write questions for exam
However, understanding his material WILL HELP
EX: Won’t ask for U in MUDPILES when he brings it up in class
Understanding Anion gap, & things that influence it is important (b/c we also cover it!) however
Which is true?
1. A Left ventricle became
2.
3. Cardiac output same on left than right side
4. Caridac outpu
5.
50 y/o man w/ CO 6 L/min.
6L = 6000mL/min
6000mL/75 = 80mL/beat
preload = 120mL
80/120 = 66%
6000
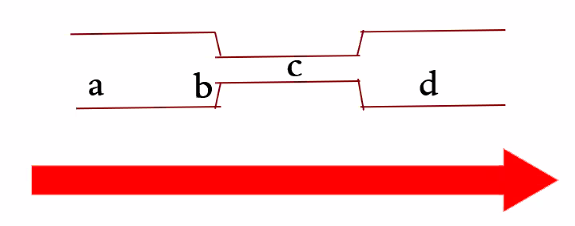
Hypothetial arteriole
Constricting vessel at point A (increase pressure) would increase flow
Will increase pressure gradient to increase flow rate
Velocity has to do with surface area (point C to D is will slow
Has surface area increases, velocity will go down (TRUE)
Nitric Oxide (NO) release from endothelial
False b/c A1 stimulation would decrease flow b/c of vasoconstriction
Pressure is lowest at D (TRUE)
due to pressure gradient
What would decrease venous return?
A. Venous valves collapsing
B. Decreased sympathetic activity
C. Vein Capacitance
How much blood the vein will actually hold
If the vein holds onto more blood, it is actually not returning to the heart (which is venous return)
D. A & B, not C
E. A, B, & C
An increase in which would increase Glomerular Filtration rate (GFR)?
A. Local nitric oxide release in the afferent arterioles of the kidneys
B. Total body dilation of arterioles
If dilating everything, then whole blood pressure drops
Not enough blood flowing through afferent arteriole (not as much dilation of afferent arterioles in kidney)
C. An increase in Plasma proteins
D. A & B
E. All of the above
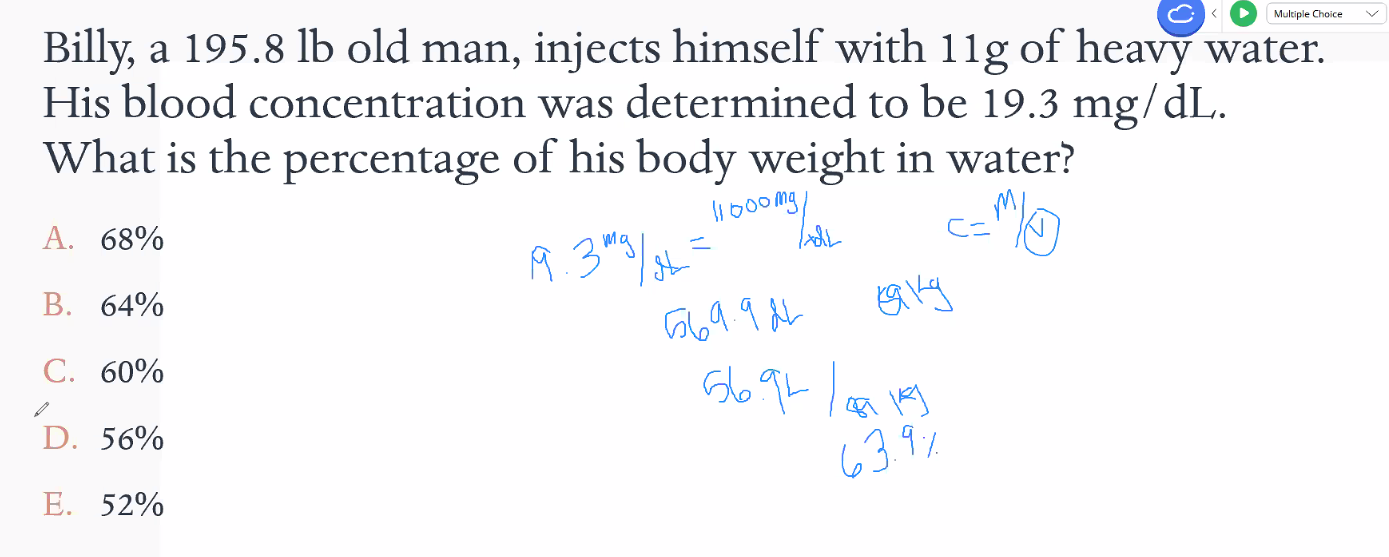
Billy (195.8 lb) injects himself w/ 11 g heavy water
Find volume of heavy water
19.3 mg / dL = (11,000 mg) / (x dL)
Find Volume & convert to percentage
Hyperventilation can result in muscle spasms. which is true?
A. plasma proteins have higher affinity for Ca2+ than H+, making more Ca2+ bioavailable
If plasma have high affinity → it would make it not bioavilable
A is incorrect
B. an increase in pH makes less CA2+ bioavailable
C. A decrease in H+ ECF concentration causes threshold to drop & cell becomes hyperexcitable
alkalosis = less free H = proteins in the blood that want to bind to something (they can either bind H or Ca) = so if theres less H they will pick Ca = if they bind Ca less is freely floating in the ECF so essentially you lower ECF [ca] so threshold lowers = easier to cause excitability and you get muscle spasms
basically the proteins have to grab either H or Ca and if H were green marbles and Ca were blue marbles in a bag, they just reach in and grab one. If you cnage the amount of marbles in the bag, i.e. hyperventilate, you get rid of green marbles and youre more likely to take the blue ones out of the bag if you reach your hand in. that's what albumin is doing
D. B & C are correct (TRUE)
Hyperventilation → Alkalotic
hyperventilate = less co2
less co2= less acid
less acid = alkalosis
alkalosis = low H
low H = high affinity for Ca
less free Ca in blood lowers threshold so we spasm
Less hydrogen, more calcium would be bound so less calcium would be bioavailable
Given following labs
Since pH is low, we know it’s acidosis
Since PCO2 is low,
Bicarbonate levels are also low
What does vomiting cause?
Vomiting causes alkalosis (metabolic alkalosis)
Vomiting is always metabolic
Body compensates w/ respiratory acidosis
vomit = lose acid = so body is basic
need to compensate with some kind of acid so you compensate with respiratory acidosisQuestion 10!
Question’s won’t be as hard on exam
Billy lost complete function of Dorsal REspiratory Group (DRG), which may occur?
He can still breathe, he just has to THINK ABOUT IT
Why does billy go to Denver to train?
if we’re higher in altitude is there less or more oxygen available in the air
and do our tissues still need the same amount of oxygen
A. Immediate left shift of oxyhemoglobin curve stimulates 2,3-DPG compensatory mechanism
B. After acclimation, an overall right shift in the oxyhemoglobin curve increases overall oxygen capacity
High Altitude would cause immediate left shift
since theres less o2 we're gonna shift left so that our body releases more oxygen to the tissues
cool so since theres less o2 we're gonna shift left so that our body Carries more oxygen to the tissues
then when we're back to normal levels the curve will shift right to compensate and more O2 gets released
athletic advantage, more capacity etc