The Respiratory System: V/Q Mismatch and Control Mechanisms
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
111 Terms
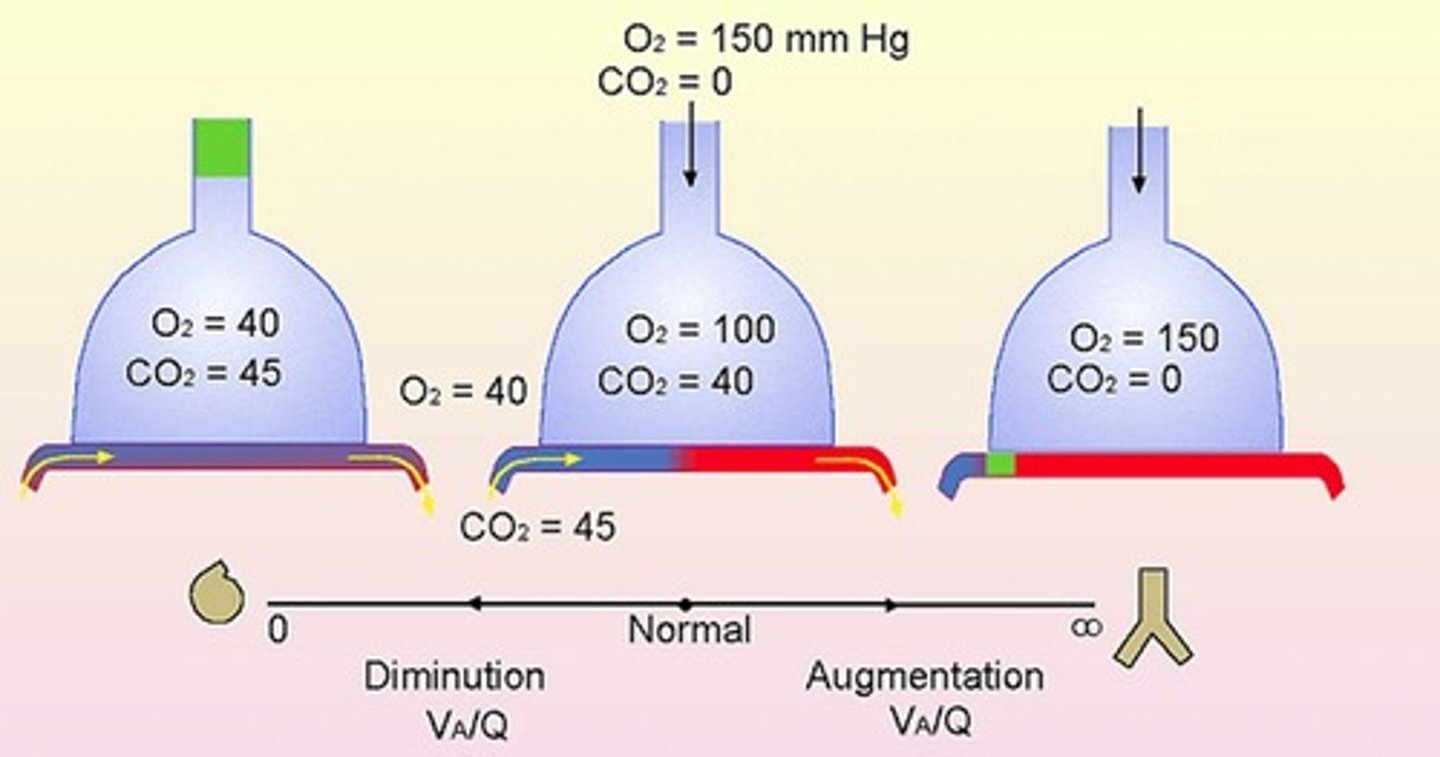
V/Q
Refers to the ventilation-perfusion ratio, indicating the efficiency of gas exchange in the lungs.
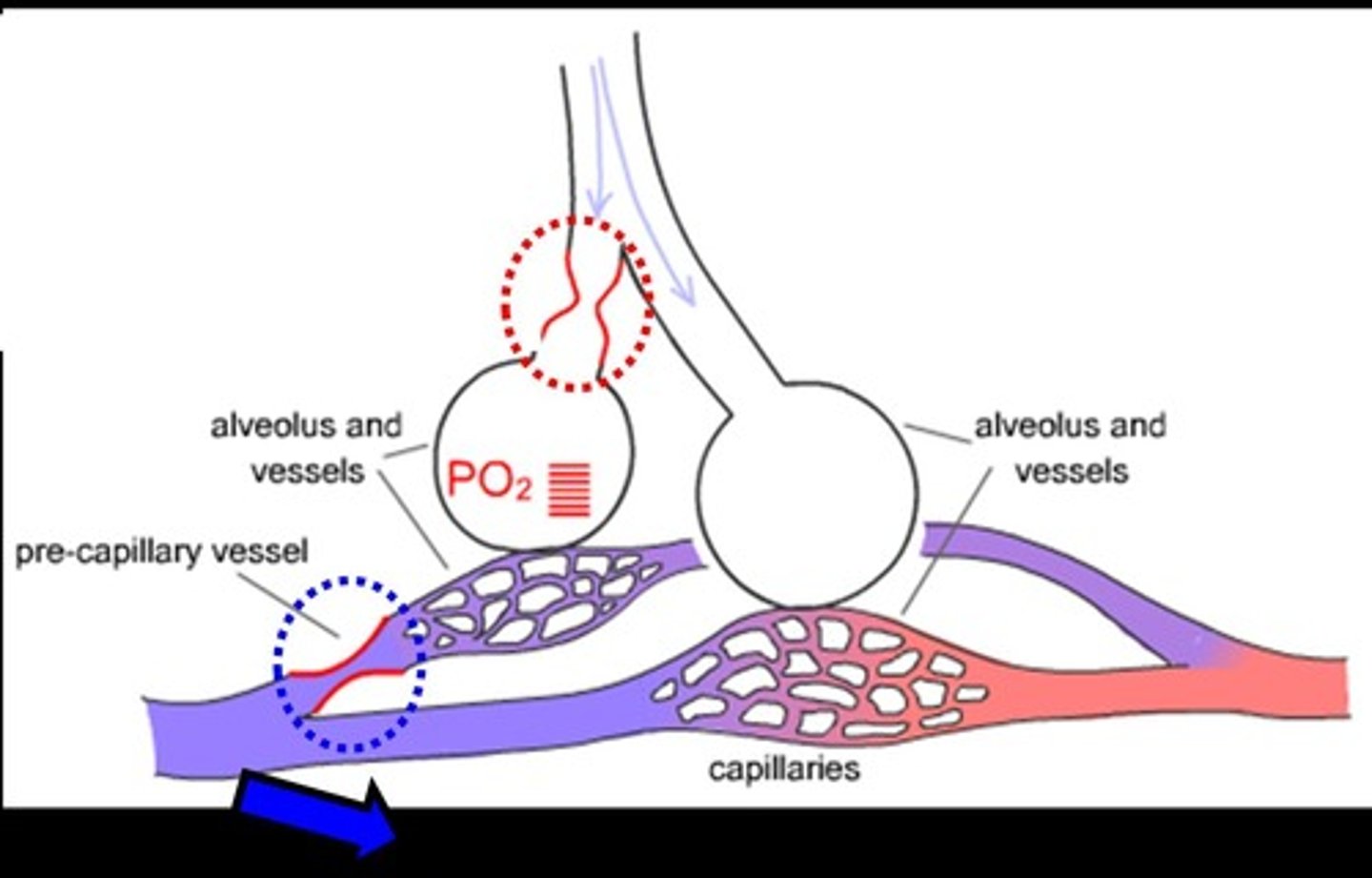
Hypoxic Pulmonary Vasoconstriction (HPV)
An intrinsic property of the lung where smooth muscles constrict in response to hypoxia, diverting blood flow to better-ventilated areas.
Control of Ventilation
Breathing parameters are controlled by spontaneous discharge of neurons in the respiratory control center and inputs from receptors.
Dorsal Respiratory Group (DRG)
Located in the medulla, it contributes mostly to inspiration.
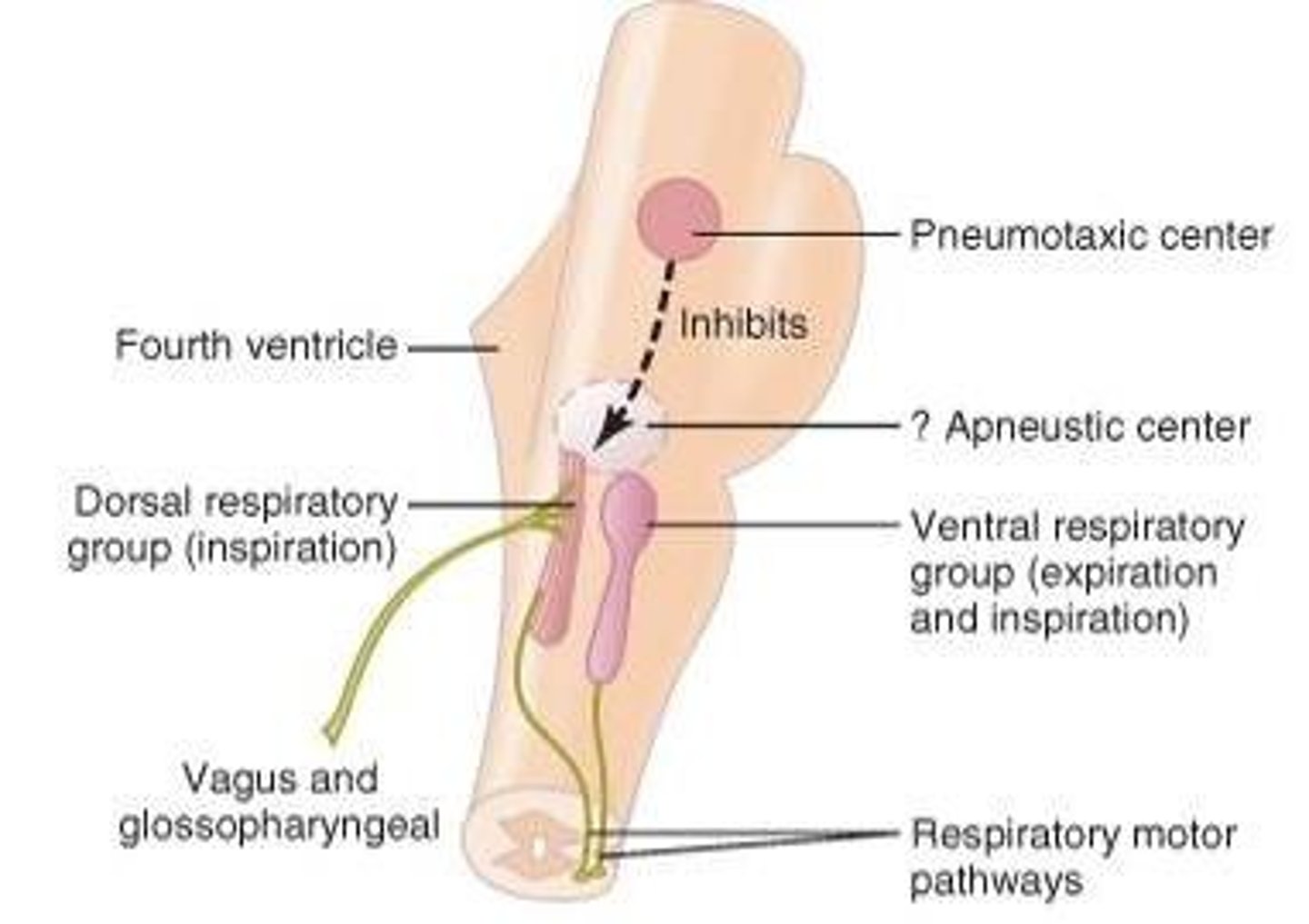
Ventral Respiratory Group (VRG)
Functions in both inspiration and expiration and plays a role in forced expiration.
Hering-Breuer Reflex
A negative feedback mechanism that stops further inspiration when the lungs become overly inflated.
Peripheral Chemoreceptors
Located in the carotid artery and aorta, they are sensitive to large decreases in arterial PO2.
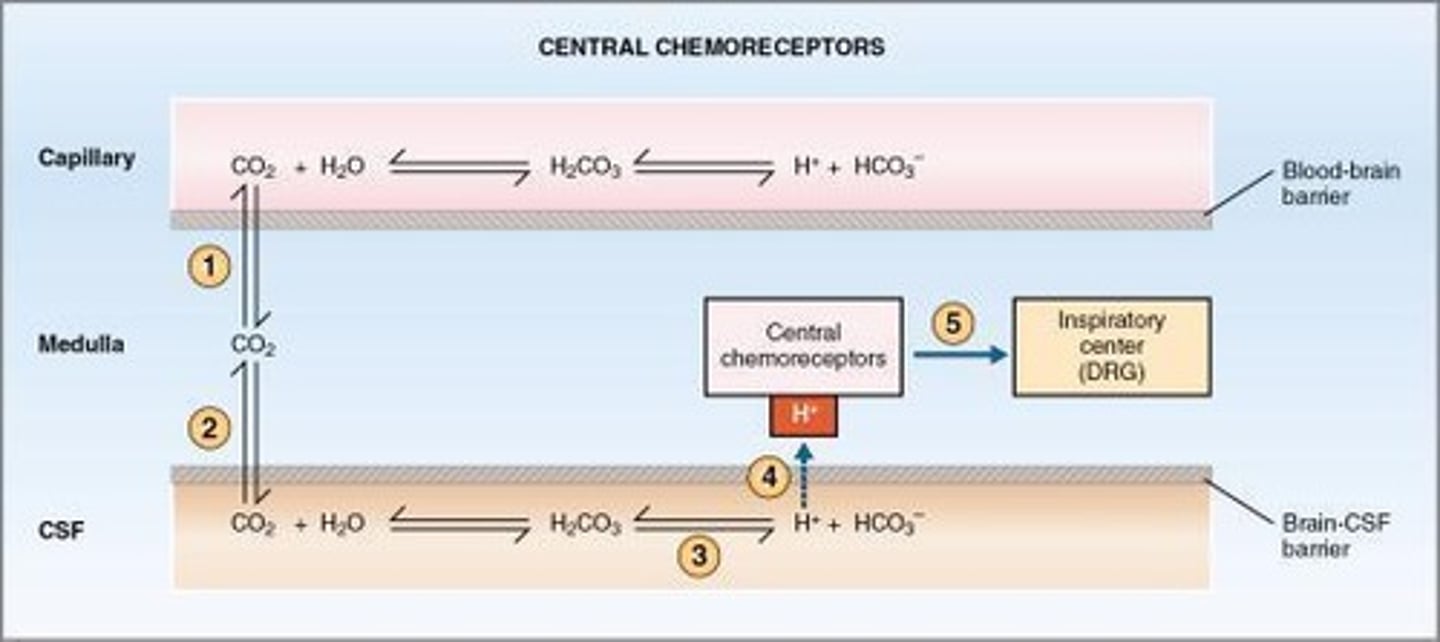
Central Chemoreceptors
Located in the medulla, they respond primarily to a rise in PaCO2 and changes in the pH of the CSF.
Acid-base Homeostasis
The respiratory system, along with renal and buffering systems, plays an important role in maintaining pH balance in the body.
Respiratory Centres
Control the duration of the filling phase, regulate depth of inflation, and provide extra boost to inspiratory drive.
Inputs to Respiratory Centres
Include activities such as speaking, singing, swallowing, coughing, heavy lifting, and meditation.
Stimulation of Diaphragm
Involves the stimulation of diaphragm and external intercostal muscles for breathing.
Stimulation of Abdominal Muscles
Involves the stimulation of abdominal and internal intercostal muscles during forced expiration.
PaO2
Partial pressure of oxygen in arterial blood, normally around 100 mmHg.
PaCO2
Partial pressure of carbon dioxide in arterial blood, normally around 40 mmHg.
CSF
Cerebrospinal fluid, which is affected by CO2 levels and pH changes.
Increased Pulmonary Resistance
Occurs when blood flow is diverted to better-ventilated areas of the lung due to HPV.
Right Side of the Heart Workload
Increases due to higher pulmonary resistance from hypoxic pulmonary vasoconstriction.
Respiratory Control Centre
Located in the brain stem, it regulates the rate and depth of breathing.
Chemo Receptors
Sensory receptors that respond to chemical changes in the blood, particularly oxygen and carbon dioxide levels.
Negative Feedback in Breathing
Mechanism that prevents over-inflation of the lungs during inspiration.
Inspiration
The process of inhaling air into the lungs.
Expiration
The process of exhaling air from the lungs.
Henderson-Hasselbach equation
The relationship between pH, CO2 and HCO3- levels in the blood.
Normal HCO3- values
22-26 mmol/L (22-26 mEq/L).
Normal PCO2 values
35-45 mmHg.
Normal blood pH values
7.35 - 7.45.
Normal arterial pH
7.4.
Hypoventilation
Can lead to abnormally high CO2 levels in the body.
Respiratory acidosis
Occurs when pH < 7.35 and CO2 > 45 mm Hg.
Metabolic acidosis
Suspected if pH < 7.35 and PCO2 levels are normal or below normal.
Hyperventilation
Can lead to respiratory alkalosis by eliminating more CO2 than required.
Respiratory alkalosis
Occurs when pH > 7.45 and CO2 < 35 mm Hg.
Metabolic alkalosis
Suspected if pH > 7.45 and PCO2 levels are normal or above normal.
Boyle's Law
A formula relating the pressure and volume of a gas.
Compliance
A measure of the lung's ability to expand.
Laplace's Law
Describes the pressure difference across a curved surface.
Poiseuille's Law
Describes the flow of fluid through a cylindrical pipe.
Reynold's number
A dimensionless number used to predict flow patterns in different fluid flow situations.
Time constant
The time it takes for a system to respond to a change.
Fick's Law
Describes the diffusion of gases.
Physiological dead space
The volume of air that does not participate in gas exchange.
Determinants of PACO2
Factors that influence the partial pressure of carbon dioxide in the alveoli.
Oxygen deficit in inspired air
Occurs at high altitude or low FiO2.
Alveolar hypoventilation
Can occur due to defective neuronal stimulus or defective equipment.
V/Q mismatch
A condition that can lead to inadequate oxygen delivery due to unequal ventilation and perfusion.
Histotoxic hypoxia
Occurs due to cyanide poisoning.
PaO2
Partial pressure of O2 (gas) dissolved in arterial blood.
O2 supply
18 ml O2 / min.
O2 requirement
250 ml O2 / min at rest (VO2 at rest).
O2 Saturation (O2 Sat %)
Represents the saturation of hemoglobin's (Hb) binding sites by oxygen in arterial blood.
Normal O2 Saturation
96-100% in arterial blood.
Tissue O2 Saturation
75% saturation in tissues.
Oxygen Content of Arterial Blood (CaO2)
O2 content = amount of O2 in blood (mL O2 / 100 mL blood).
O2 content formula
(% Saturation X O2 binding capacity) + dissolved O2.
O2 content calculation
SaO2 [Hb] 1.34 ml O2 /g Hb + 0.003*PaO2.
O2 content example
98% 15g Hb/100 ml 1.34mlO2/gHb + 0.003 * 100 mm Hg = 20.0 ml O2 / 100 ml blood.
Solubility of O2 in blood
0.003 mL O2/100 mL blood per mm Hg.
Hemoglobin A binding capacity
1 g of hemoglobin A can bind 1.34 mL O2.
Normal concentration of hemoglobin A
15 g/100 mL.
Oxygen-Hb Saturation Curve
Describes the relationship between PO2 in the plasma and the amount of O2 bound to Hb (%O2 saturation).
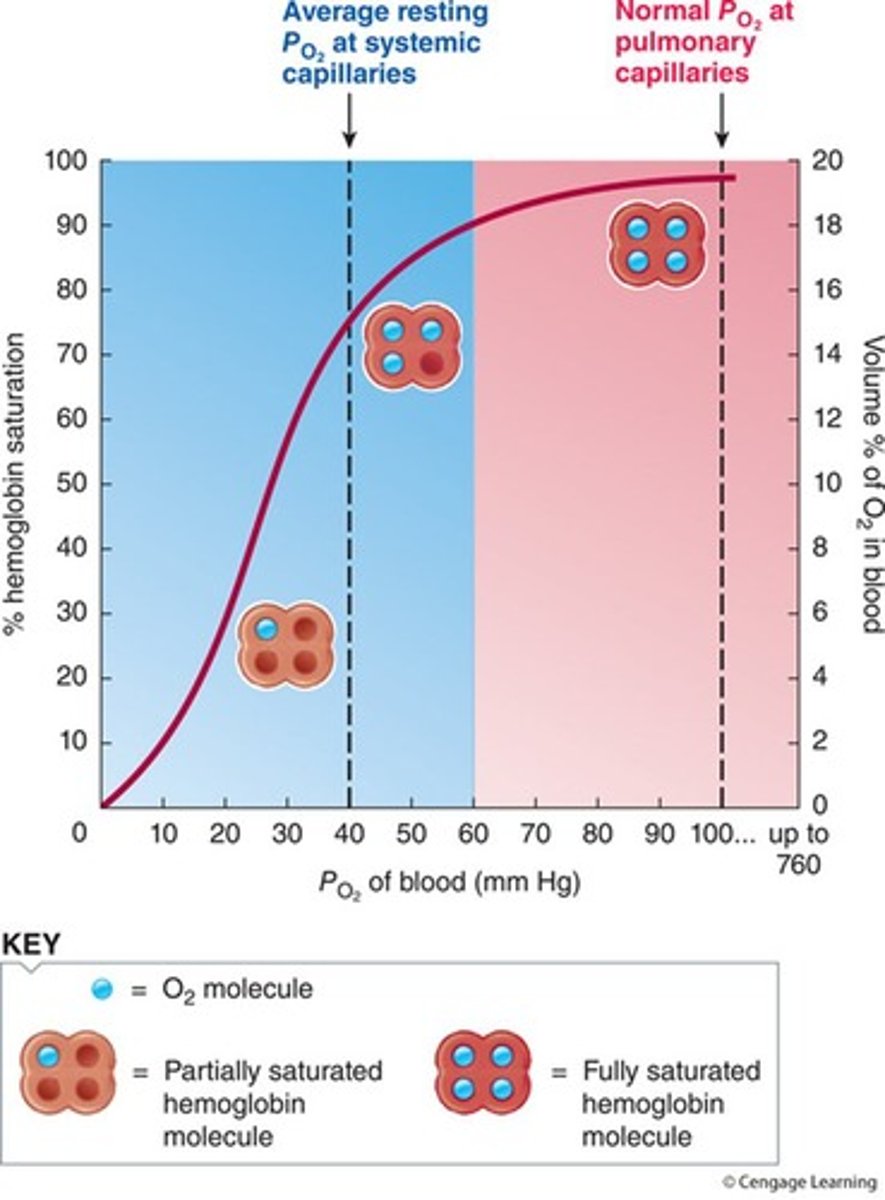
P50
The partial pressure of O2 at which Hb is 50% saturated.
CO2 transport
CO2 is soluble enough that it does not need a protein carrier like oxygen needs hemoglobin.
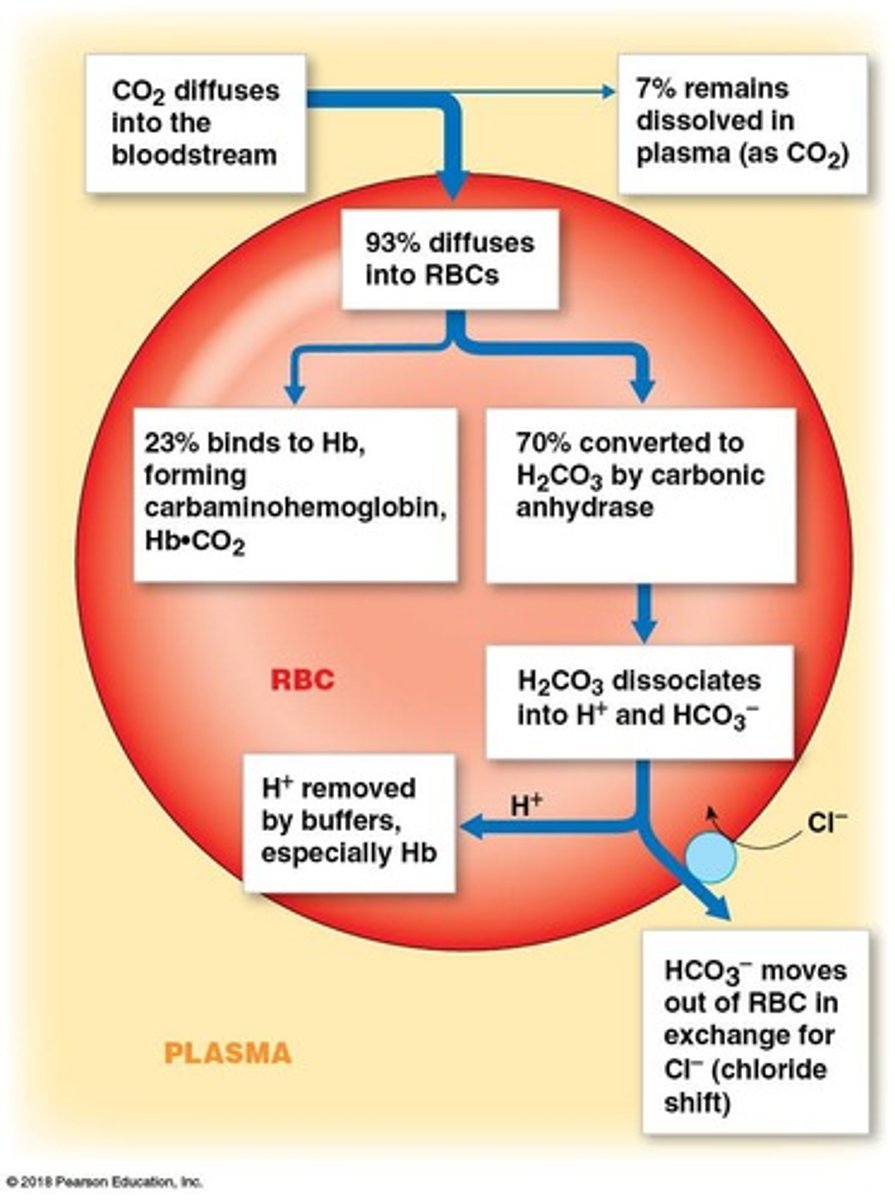
Dissolved CO2
Forms carbonic acid, which can threaten pH homeostasis.
Bound CO2
15 - 25% of CO2 is bound to hemoglobin.
Dissolved CO2 percentage
~ 7% of CO2 is dissolved.
Bicarbonate CO2 percentage
~ 70% of CO2 is transported as bicarbonate (HCO3-).
Total Ventilation
Total Ventilation = volume x rate.
Dead Space
Part of the air we inhale that does not reach the alveoli and is not useful in gas exchange.
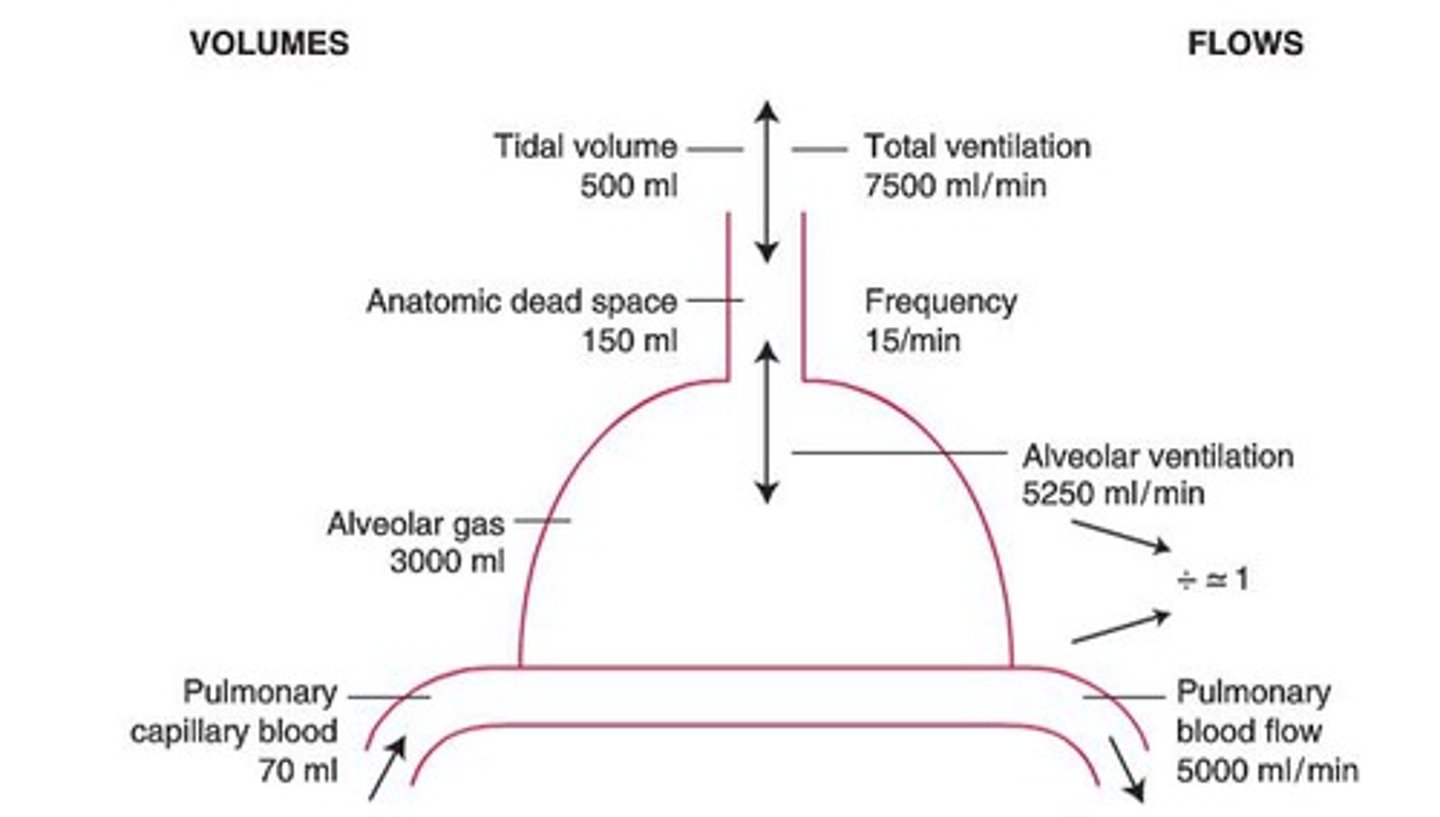
Physiological Dead Space
The total volume of dead space in the lungs, including both anatomical and alveolar dead space.
Anatomical Dead Space
The volume of the conductive airways.
Alveolar Dead Space
Represents alveoli not participating in gas exchange (not receiving blood).
VD
Physiological dead space measured in mL.
VT
Tidal volume measured in mL.
PACO2
Alveolar CO2 levels, often approximated as PaCO2.
PECO2
PCO2 in mixed expired air.
Alveolar Ventilation (VA)
The true volume of air that participates in meaningful gas exchange, calculated by subtracting dead space volumes from tidal volume.
Total Ventilation (Vtot)
Calculated as respiratory rate multiplied by tidal volume.
Alveolar Ventilation Equation
VA = Vtot - VD.
Factors determining PA gases
Includes PACO2 and PAO2, which are influenced by ventilation and gas exchange efficiency.
PAO2
Roughly equal to PaO2 in a normal lung; a decrease indicates a problem with gas exchange.
Alveolar Gas Equation
Estimates whole lung alveolar PO2 as the inspired PO2 minus the arterial PO2 divided by the respiratory exchange ratio.
PiO2
Inspired oxygen, calculated as FiO2 multiplied by (PATM - PH2O).
R
Metabolic quotient calculated as CO2 produced divided by O2 consumed, typically 0.8.
A-a Gradient
Measures the difference between PAO2 and PaO2, reflecting the efficiency of gas exchange in the lungs.
Hyperventilation
Condition characterized by increased ventilation leading to decreased PACO2 and increased PAO2.
Hypoventilation
Condition characterized by decreased ventilation leading to increased PACO2 and decreased PAO2.
Calculated Alveolar PO2 (PAO2)
PAO2 calculated as PiO2 minus PACO2 divided by R.
Example of PiO2 Calculation
PiO2 = 0.21% x (760 - 47) = 150 mmHg.
PACO2 ~ PaCO2
Typically approximated as 40 mmHg.
PAO2
The partial pressure of oxygen in the alveoli, calculated as PAO2 = PiO2 - (PACO2 / R).
PACO2
The partial pressure of carbon dioxide in the alveoli, which can only be decreased by ventilation.
A-a gradient
The difference between alveolar and arterial PO2, which is normal at no more than 5-10 mmHg in a healthy young person.
Factors affecting A-a gradient
Age, ventilation/perfusion (V/Q) mismatch, diffusion limitations, and shunt.
High A-a gradient
An indicator of underlying respiratory problems such as pneumonia, pulmonary edema, or chronic obstructive pulmonary disease (COPD).
Normal lung
A scenario where the A-a gradient is within normal limits.
Hypoventilation
A scenario where ventilation is insufficient to meet the body's needs.
Impaired diffusion
A scenario where gas exchange is hindered due to issues in the alveolar-capillary membrane.
Inadequate perfusion
A scenario where blood flow to the lungs is insufficient.
Ventilation (V)
The process of air flow into a group of alveoli.