Anti-platelets and Anti-coagulants
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
40 Terms
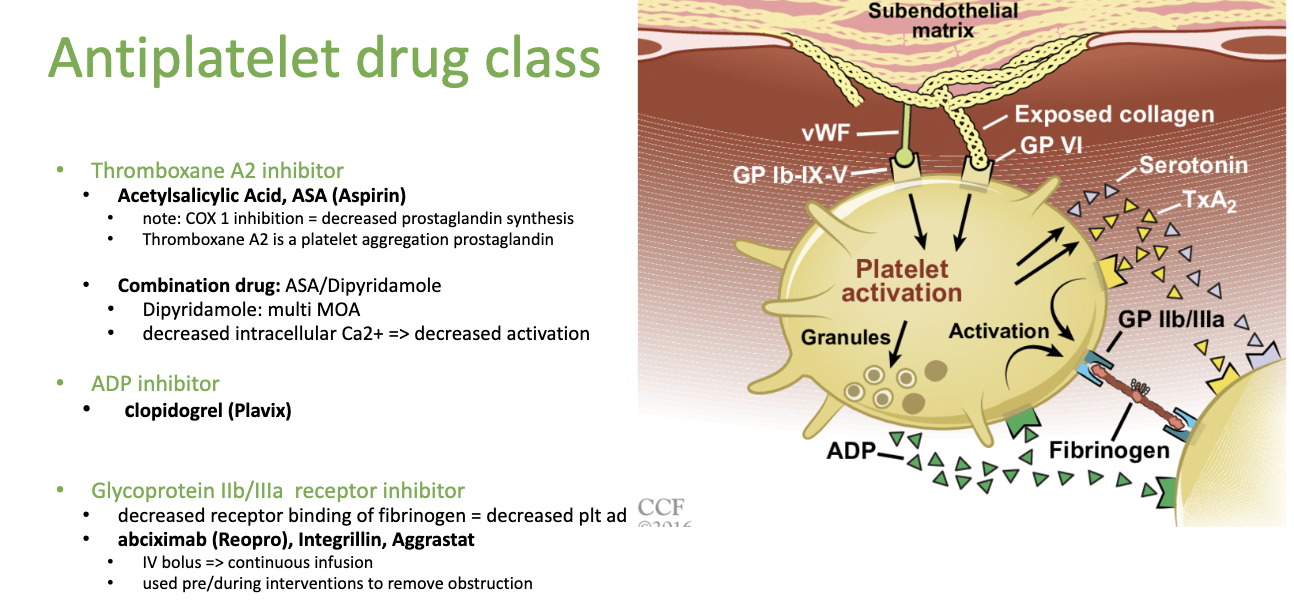
What are the 3 anti-platelet drug classes?
Thromboxane A2 inhibitor (inhibits Thromboxane A2) = prostaglandin
ADP Inhibitor
Glycoprotein IIb/IIIa receptor inhibitor
When platelets are activated via collagen and vWF, they release ADP, glycoprotein IIb, IIIa sites for attachment and Thromboxane A2 to recruit more platelets
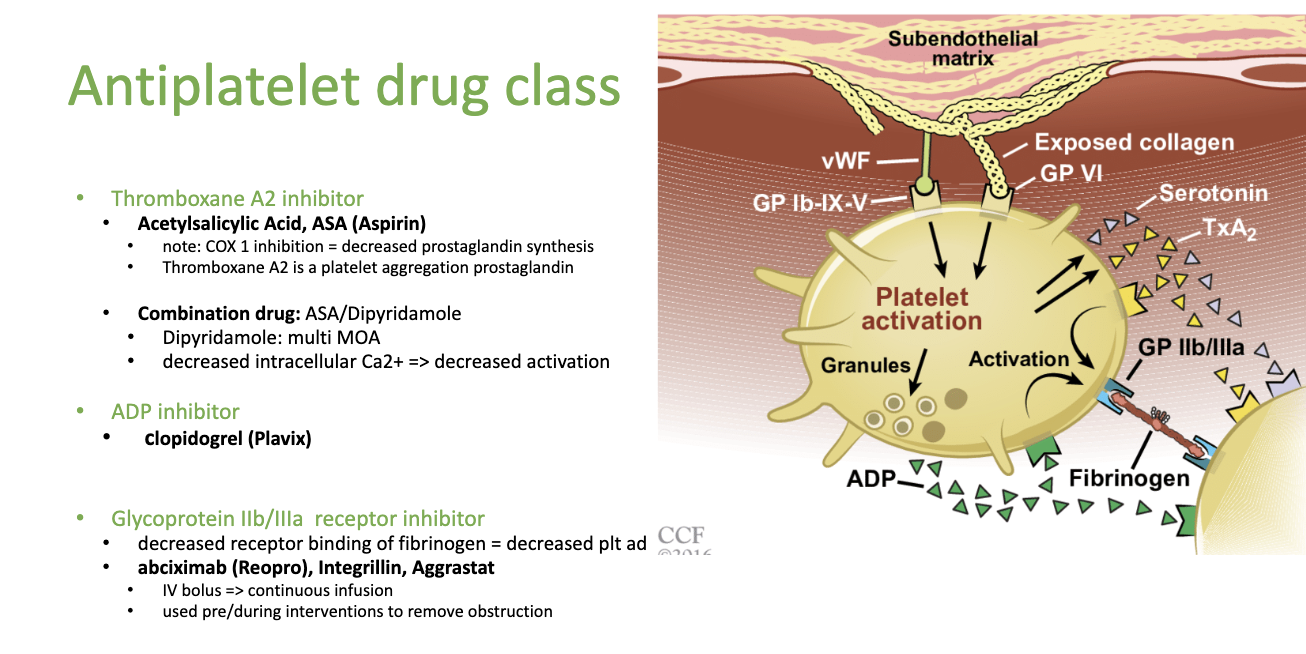
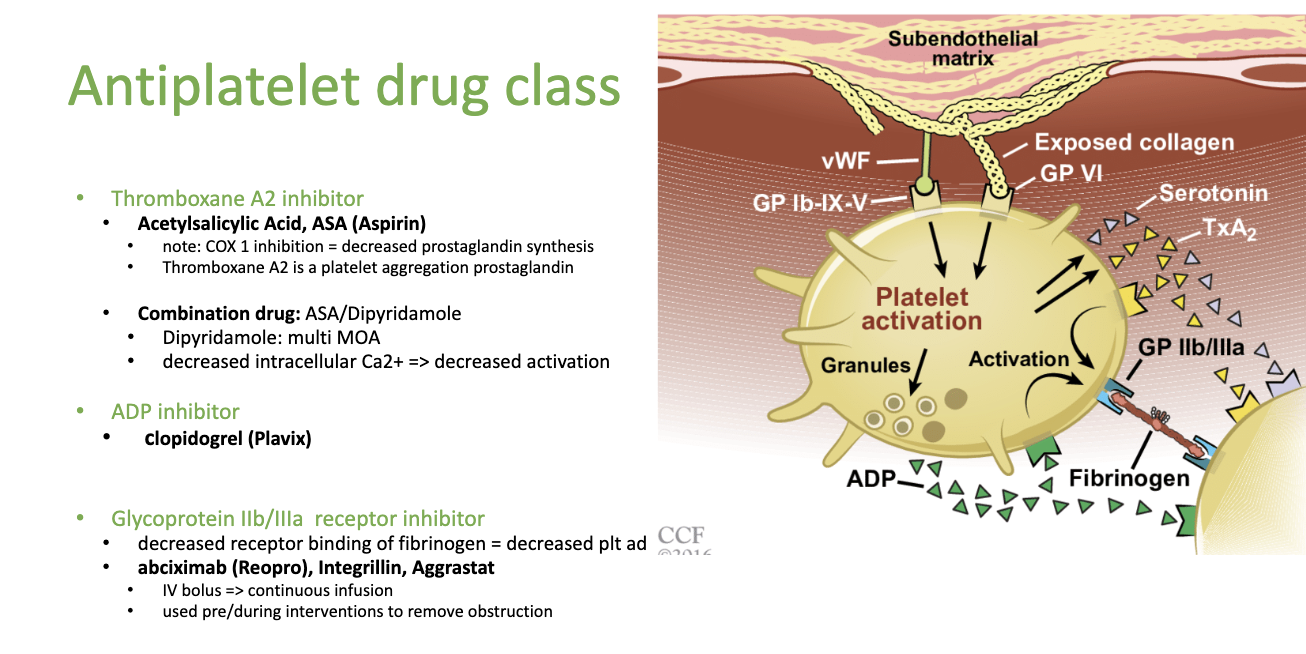
How does Thromboxane A2 inhibitors work?
COX 1 inhibition d/t ASA: causes decreased prostaglandin synthesis
Thromboxane A2 is a platelet aggregation prostaglandin = meaning it makes platelets stick together to form a plug
Vasoconstriction: = thromboxane A2 also constrict blood vessels
**Thromboxane A2 is made in activated platelets
What drugs fall under the Thromboxane A2 inhibitors?
ASA (Acetylsalicylic Acid) —> ASA
Combo drug: ASA/Dipyridamole (has multiple MOA)
**it’s an NSAID and anti-platelet
NSAID because it blocks the COX pathway that forms the THA2
What does Dipyridamole do?
it’s an anti-platelet drug that reduces/inhibits Thromboxane A2
Combo drug from ASA + Dipyridamole
**Decreases intracellular Ca 2+ and decreases activation of platelets!!
since Ca 2+ is Factor V that turns:
prothrombin into thrombin
fibrin into fibrinogen
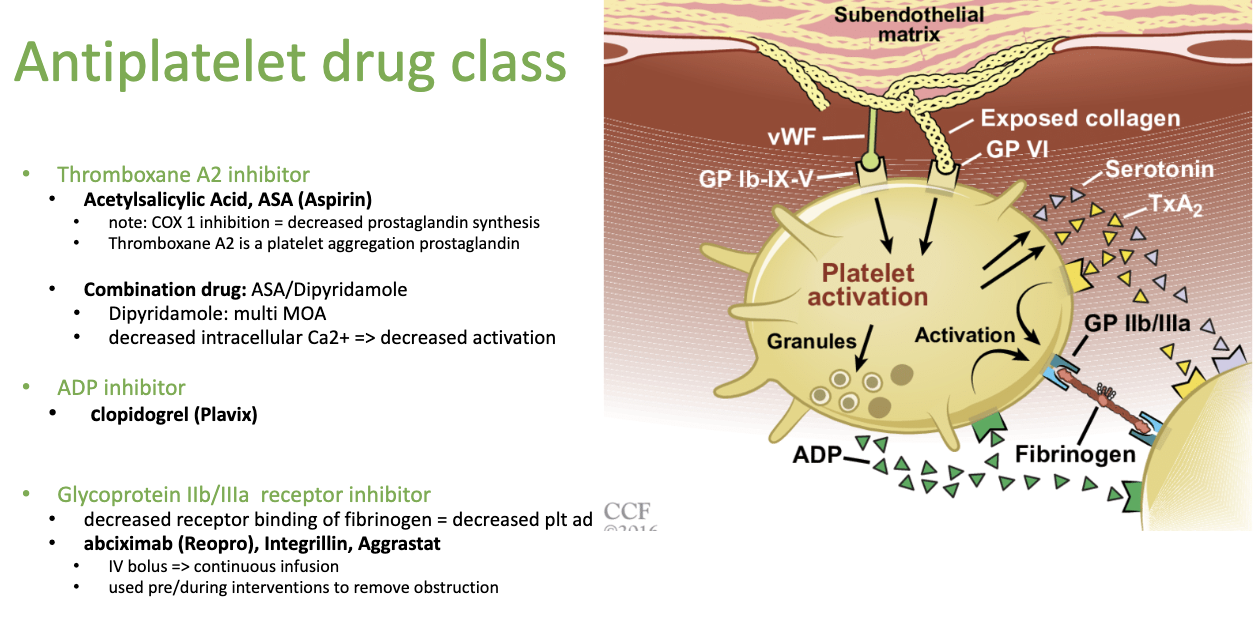
What is an ADP inhibitor drug?
Clopidogrel (Plavix) —> Plavix for Kid “play with kids”
An anti-platelet drug that is used for pediatric populations
it inhibits ADP
Where does ADP, thromboxane and glycoproteins all come from?
because they’re the 3 main factors released when platelets are activated, hence why we’re blocking them.
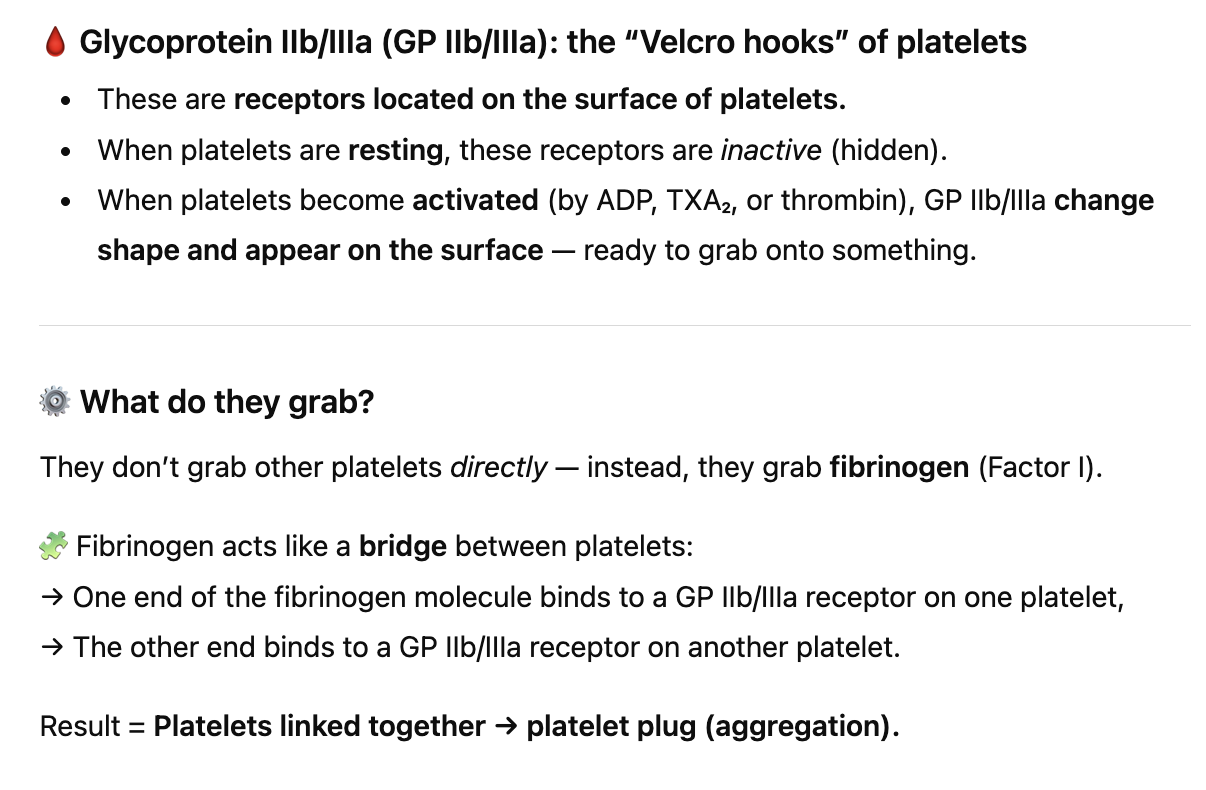
Activated platelets:
Release ADP, Thromboxane A₂ (TXA₂), and Serotonin → to recruit more platelets.
Expose Glycoprotein IIb/IIIa receptors → helps them stick together (aggregation).
What do glycoprotein IIb/IIIa receptor inhibitors do?
Glycoprotein IIb/IIIa is the binding sites on platelets, so when they’re exposed, there drugs bind instead inhibiting from the coagulation cascade from taking place
If we decrease the receptor binding of fibrinogen, we decrease the platelet adhesion
What drugs are Glycoprotein IIb/IIIa inhibitors?
abciximab (Reopro)
Integrillin
Aggrastat
**usually an IV bolus continous infusiom
used pre/during interventions to remove obstruction
What anti-platelet drug is used during the Cath lab to prevent clotting?
abciximab (Reopro) —> “opro = operation anti-platelet”
Cardiovascular disease —> if nitroglycerine doesn’t work, we intervene with the Cath lab (mechanical intervention), and to prevent clotting we put them on abciximab (Reopro)
What is the one condition where we use low dose asparin for kids?
Kawasaki Disease
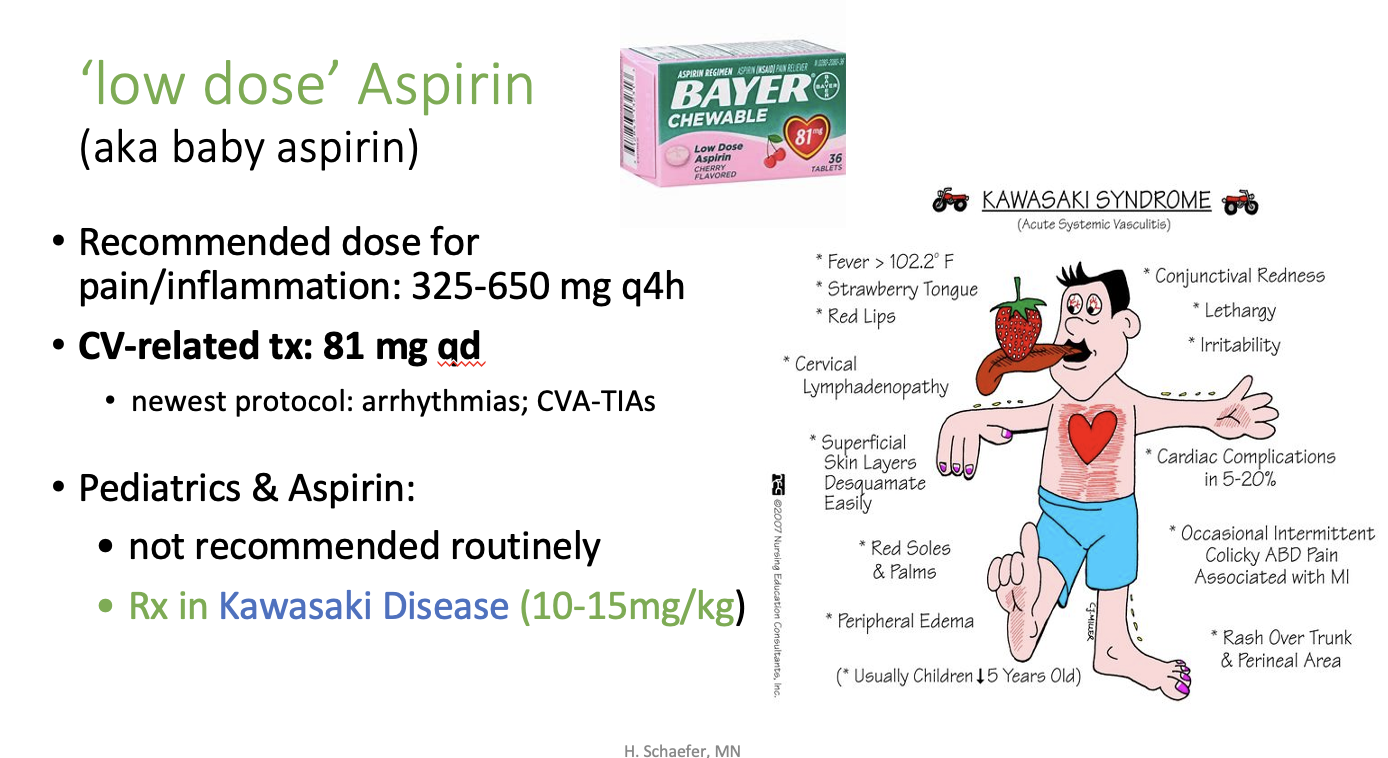
How much ASA do we use for kids with kawasaki disease?
10-15 mg/kg
What is the recommended dose of ASA for pain and inflammation?
325-650 mg q4h
If it’s CV related we use 81 mg qd
•newest protocol: arrhythmias; CVA-TIAs
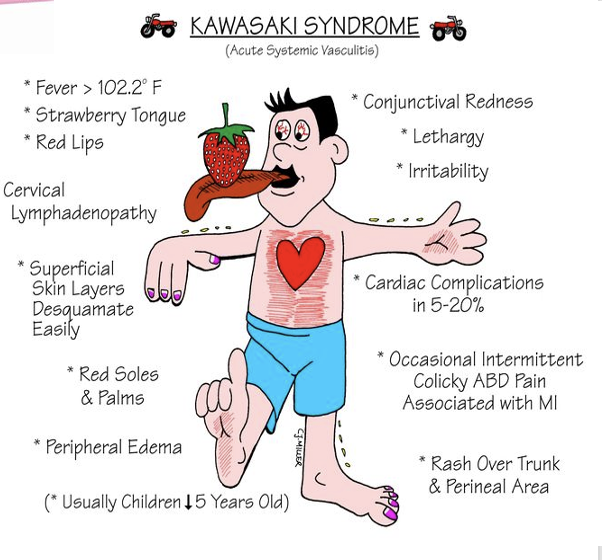
Why is kawasaki disease used for peds and why is it dangerous?
Because kawasaki disease causes vasculitis so inflammation in the vessels due to cardiac complications
so we use ASA because it blocks Thromboxane A2 and helps with arrhythmia’s and CVA = Cerebrovascular Accident and a transiet ischemic attack (clot in brain); so it stops clotting
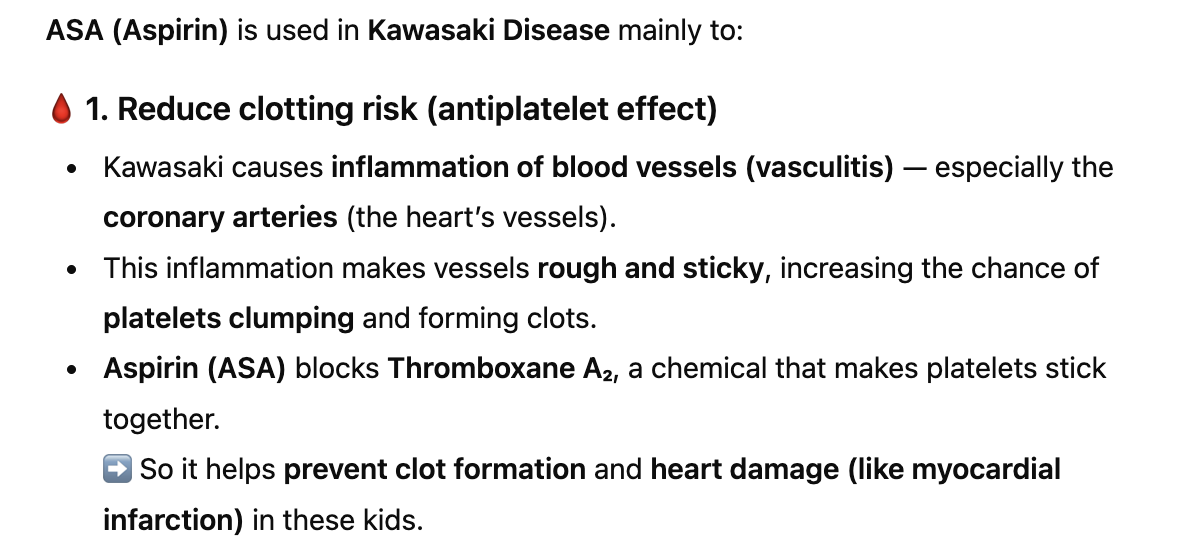
What are some symptoms of Kawasaki disease?
Strawberry tongue
red soles and palms
peripheral edema
epithelial layer isn’t then protective anymore
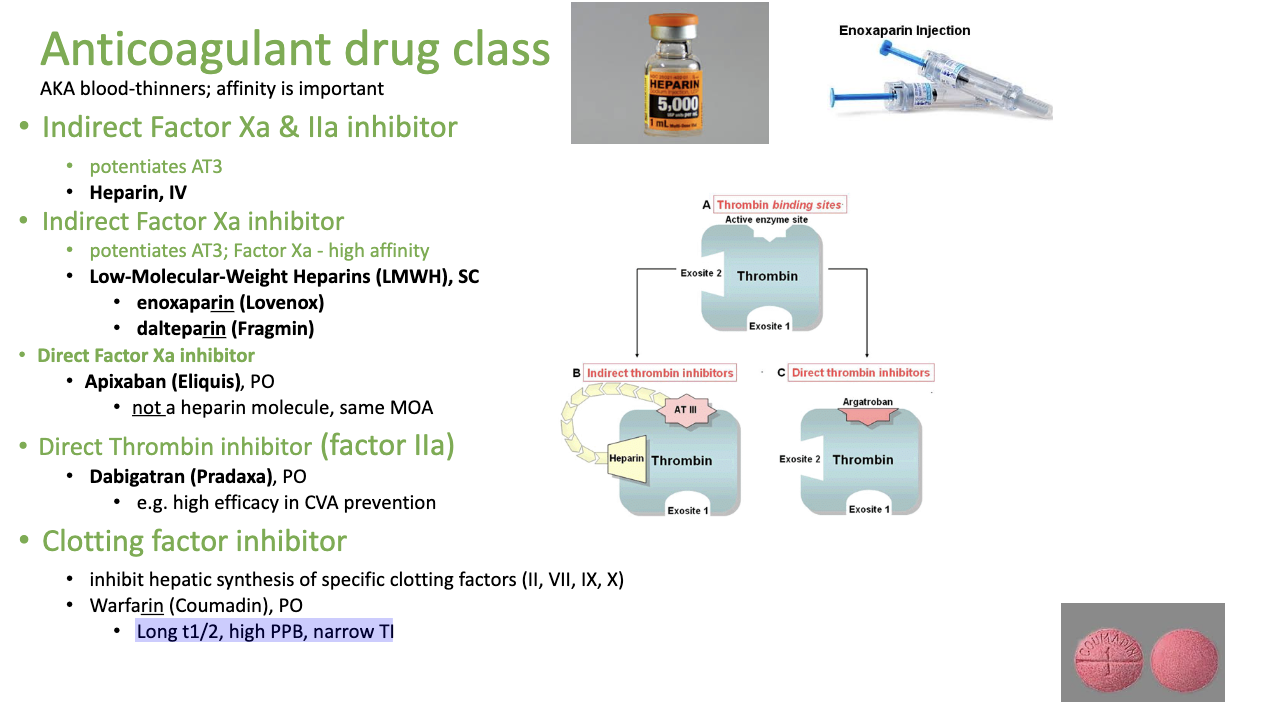
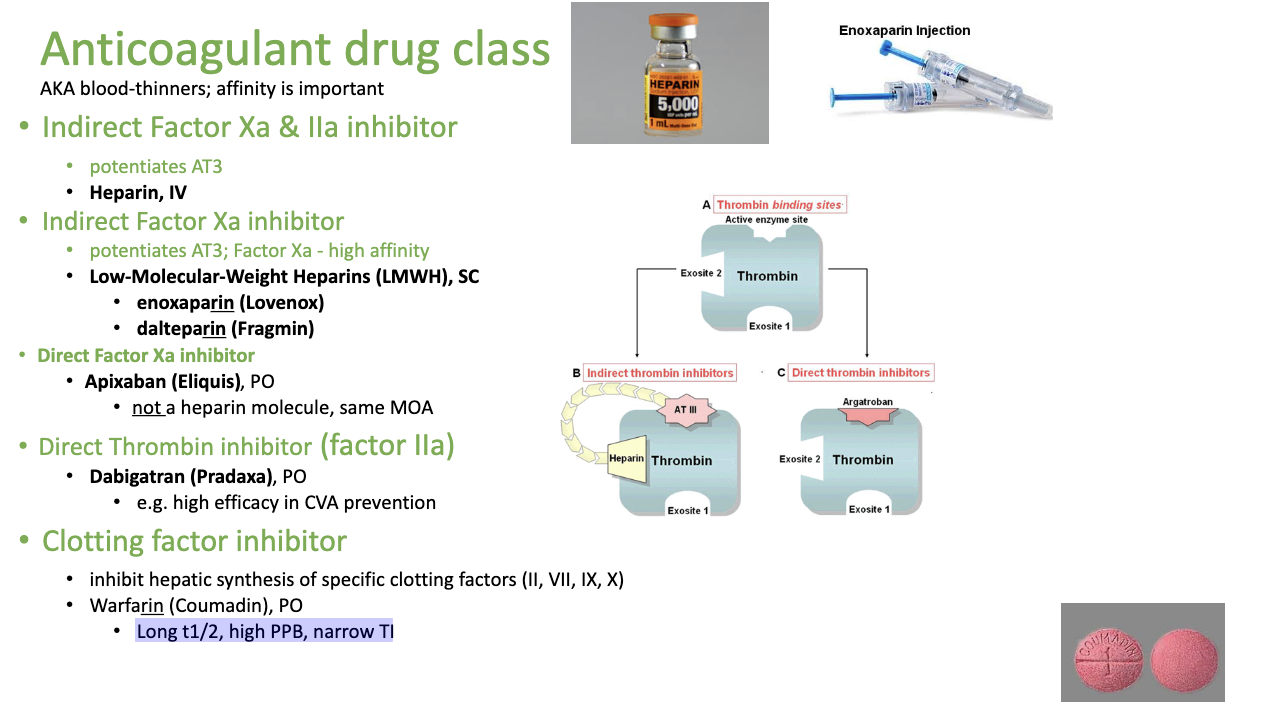
What are the 5 drug classes for anti-coagulation drug class (blood thinners)
Indirect Factor Xa & IIa inhibitor
Indirect Factor Xa inhibitor
Direct Factor Xa
Direct Thrombin inhibitor
Clotting factor inhibitor
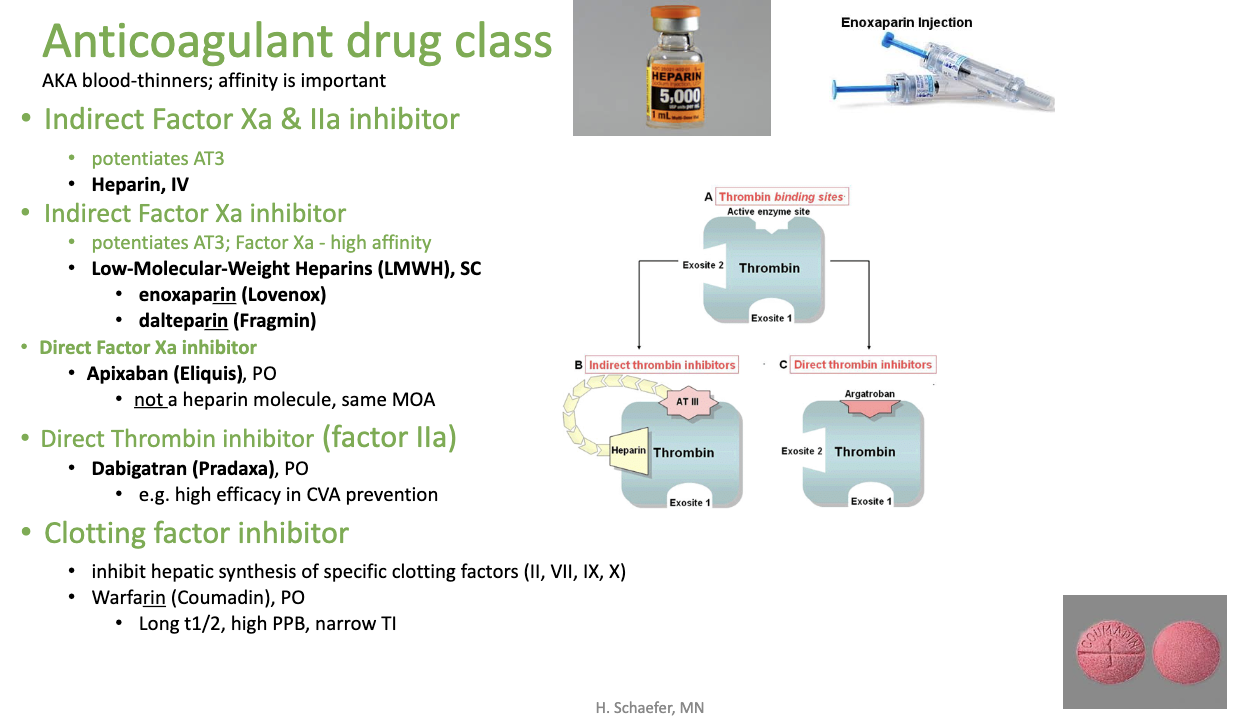
What is the indirect Factor Xa & IIa inhibitor?
Heparin IV + heparin like drug
potentiates (drives) AT3
What is the indirect Factor Xa inhibitor? (-parin)
Low-Molecular-Weight Heparins (LMWH), SC
enoxaparin (Lovenox)
dalteparin (Fragmin)
potentiates (drives) AT3
high affinity for Factor Xa (if factor Xa is inhibited, no prothrombin can be made)
What is the direct Factor Xa inhibitor?
Apixaban (Eliquis), PO
• not a heparin molecule, same MOA
What is the direct thrombin inhibitor (factor IIa)?
Dabigatran (Pradaxa), PO
• e.g. high efficacy in CVA prevention
What is clotting factor inhibitor?
WARFARIN —> WAR —→ STOPPING CLOTTING FACTORS
this works via. Liver —> so it stops the liver from producing clotting factors at all. HENCE WHY IT’S DANGEROUS
Long t1/2, high PPB, narrow TI
5 DRUG CLASSES FOR ANTICOAGULATION + Drugs:
Indirect Factor Xa and IIa inhibitor: —> heparin IV
Indirect Factor Xa inhibitor —> -parin (lovenox, fragmin)
Direct Factor Xa inhibitor —> Apixaban, PO
Direct Thrombin Factor IIa Inhibitor: Dabigabtran
Direct Factor X or Factor IIa inhibitor = ban and tran anticoagulants
Apixaban = X
Dabigatran = IIa
What is HIT?
heparin induced thrombocytopenia
Why are anticoagulants also used with viruses like COVID 19?
because inflammation increases risk for clotting
What’s the difference between direct and indirect inhibitors?
Indirect inhibitors: needs a helper like AT3 (Heparin doesn’t block thrombin by itself — it binds to AT III, and that combo then inactivates thrombin.)
Direct Thrombin Inhibitors (like Dabigatran (IIa), Apixaban (Xa))
Directly bind to thrombin’s active site and block it.
they sit right on the enzyme and stop it from working
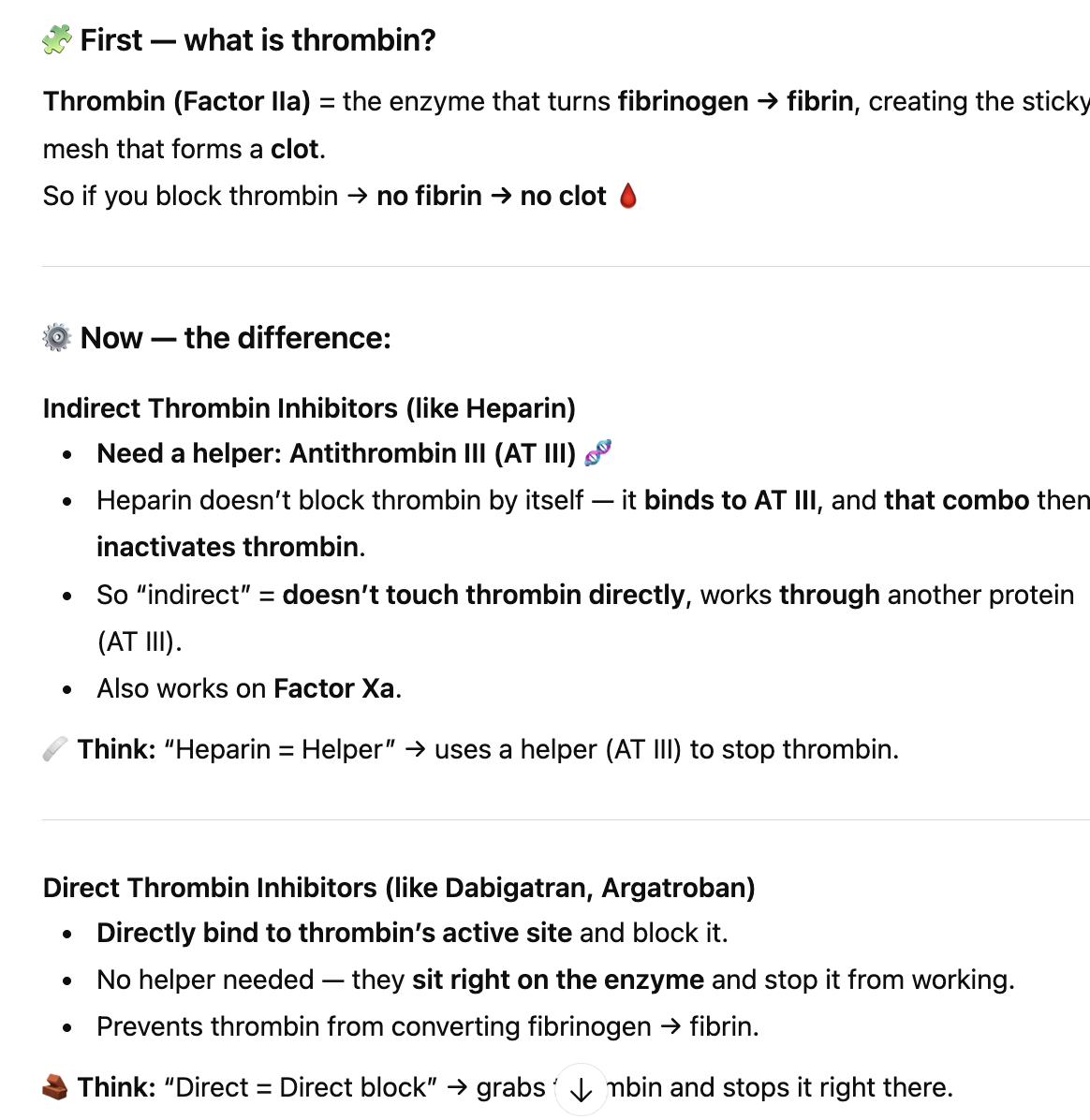
What is AT3?
What Antithrombin III (AT III) actually is
AT III is a natural protein made by your liver that’s already floating around in your blood all the time.
Its job is to act like a brake on clotting — it weakly, slowly inactivates enzymes like Thrombin (Factor IIa) and Factor Xa.
indirect drugs do
Heparin and LMWH (enoxaparin, dalteparin) don’t bind thrombin directly.
Instead, they bind to AT III and enhance it → This makes AT III way more efficient at sticking to and neutralizing Thrombin and Factor Xa.
What is thrombocytopenia?
Thrombocytopenia = low platelet count.
What happens with heparin induce thrombocytopenia (low platelets)
Immune reaction to heparin (& platelet factor 4)
• => activation of thrombin => DIC
Disseminated Intravascular Coagulation (DIC):
clotting and bleeding at the same time
What is DIC and why does it occur with heparin?
So if someone has an immune reaction to heparin, it activates thrombin instead and the body experiences DIC
Something triggers massive clotting activation —> heparin immune reaction
All clotting factors + platelets get used up in forming tiny clots all over the body.
When the body later needs to clot (like at an injury site), there’s nothing left → severe bleeding.
What happens if we prolong coagulation, aka. how do we monitor for bleeding?
Kidneys: renal bleeding in the urine
In stool as well (upper GI vs. Lower GI)
Changes in bloodwork —> hematocrit is lower, RBC IS LOWER when bleeding duh
They tell us they feel light-headed or dizzy, petechia (depending on where blood is aka. disseminated coagulation
BRUISING; EASILY
Consistent Nosebleeds!!
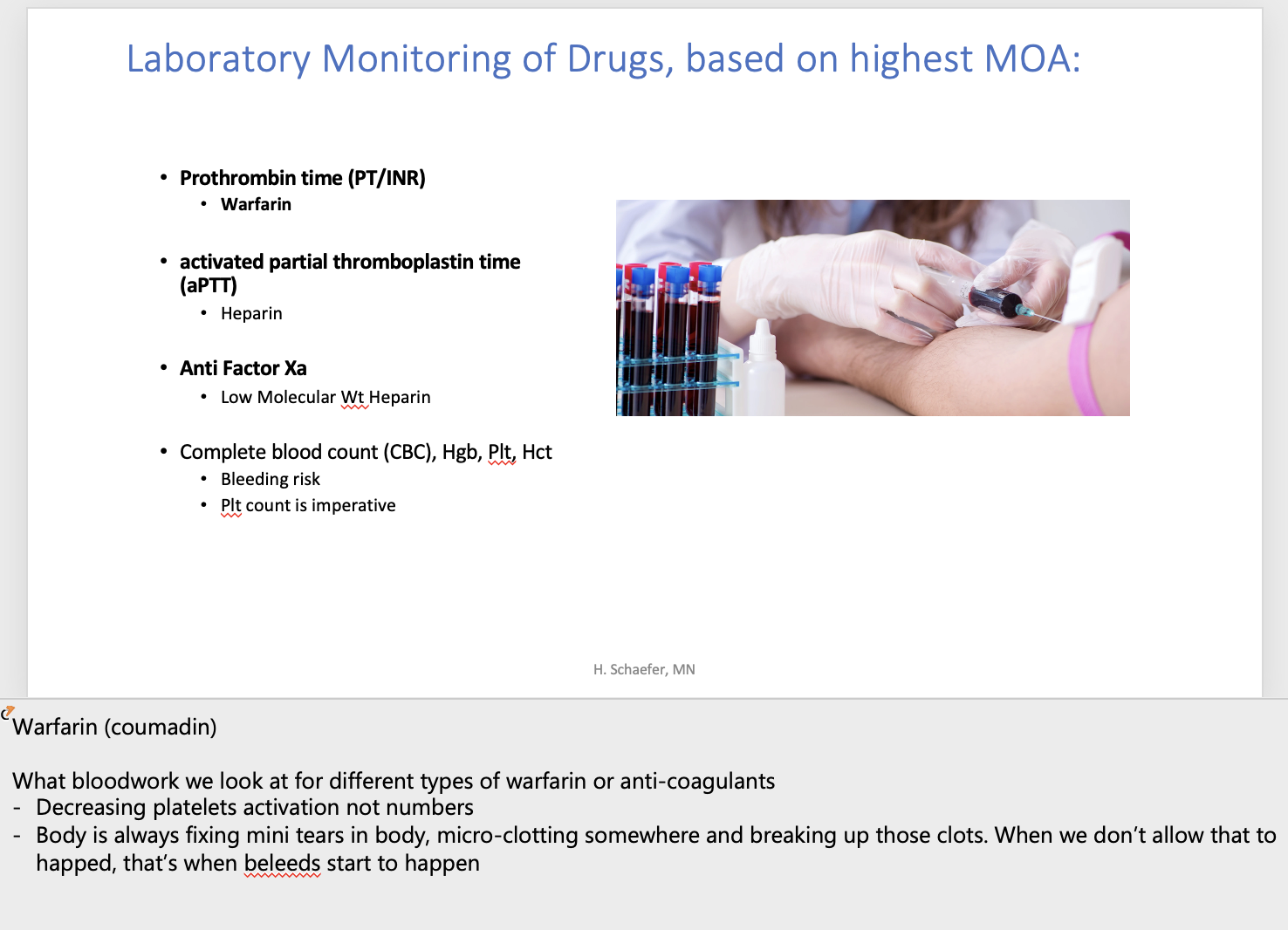
How do we monitor warfarin?
•Prothrombin time (PT/INR)
How do we montior Heparin?
activated partial thromboplastin time
How do we monitor LMWH?
anti factor Xa
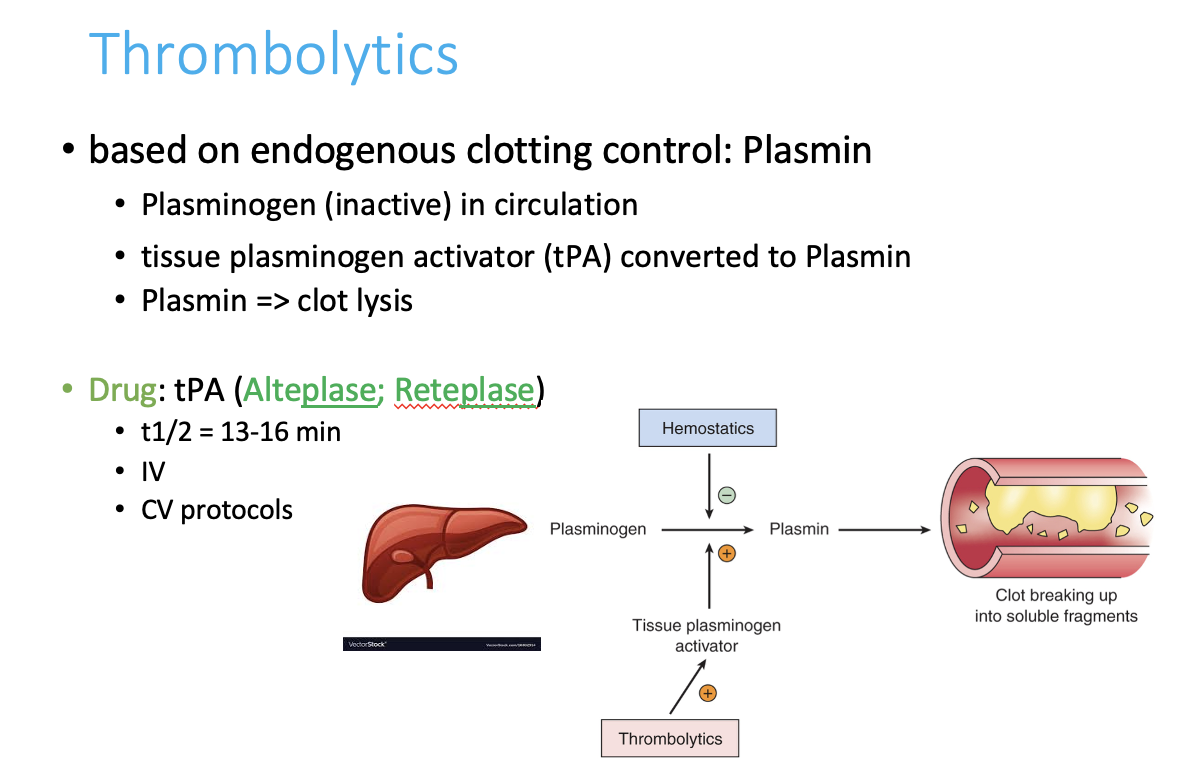
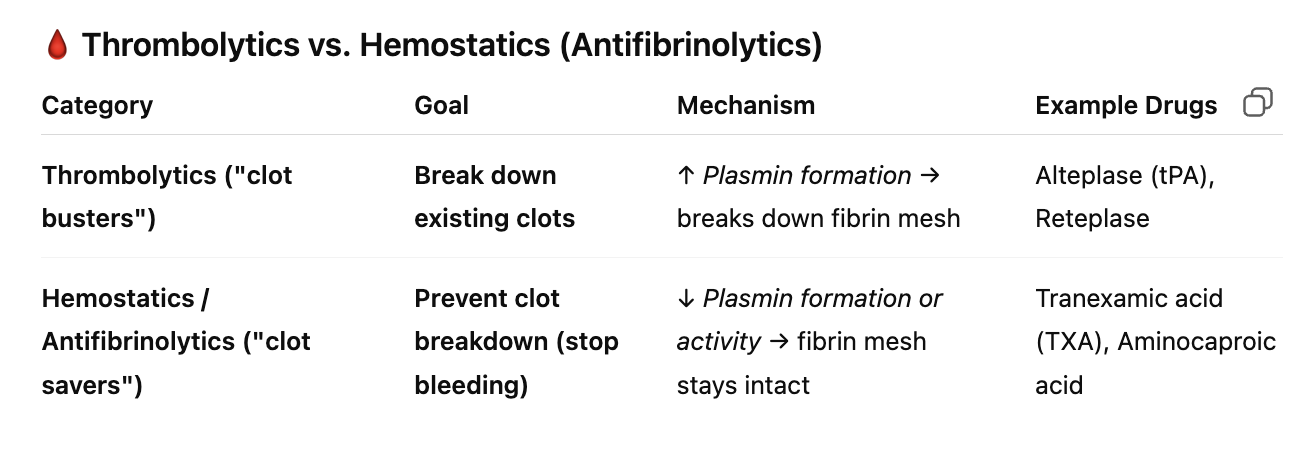
What do thrombolytics (clot busters) do?
They’re based on endogenous clotting control: They don’t prevent new clots like anticoagulants do — instead, they actively dissolve existing clots that are already blocking blood flow
so thrombolytics kill normal clots already made
Liver makes plasminogen --> tissue plasminogen activator (tpa) —> plasmin destroys clots
What is the main enzyme that breaks down clots?
Plasmin
How do thrombolytics work? (-plase) = plasmin
Alteplase (tPA) and Reteplase
are synthetic forms of tPA.
They mimic your body’s natural tPA, rapidly activating plasminogen → plasmin → fibrin breakdown.
Given IV (intravenous)
Very short half-life: 13–16 minutes
Used in CV emergencies, such as:
Ischemic stroke (CVA)
Myocardial infarction (MI)
Massive pulmonary embolism (PE)
decreasing plasmin increases ____________
clotting
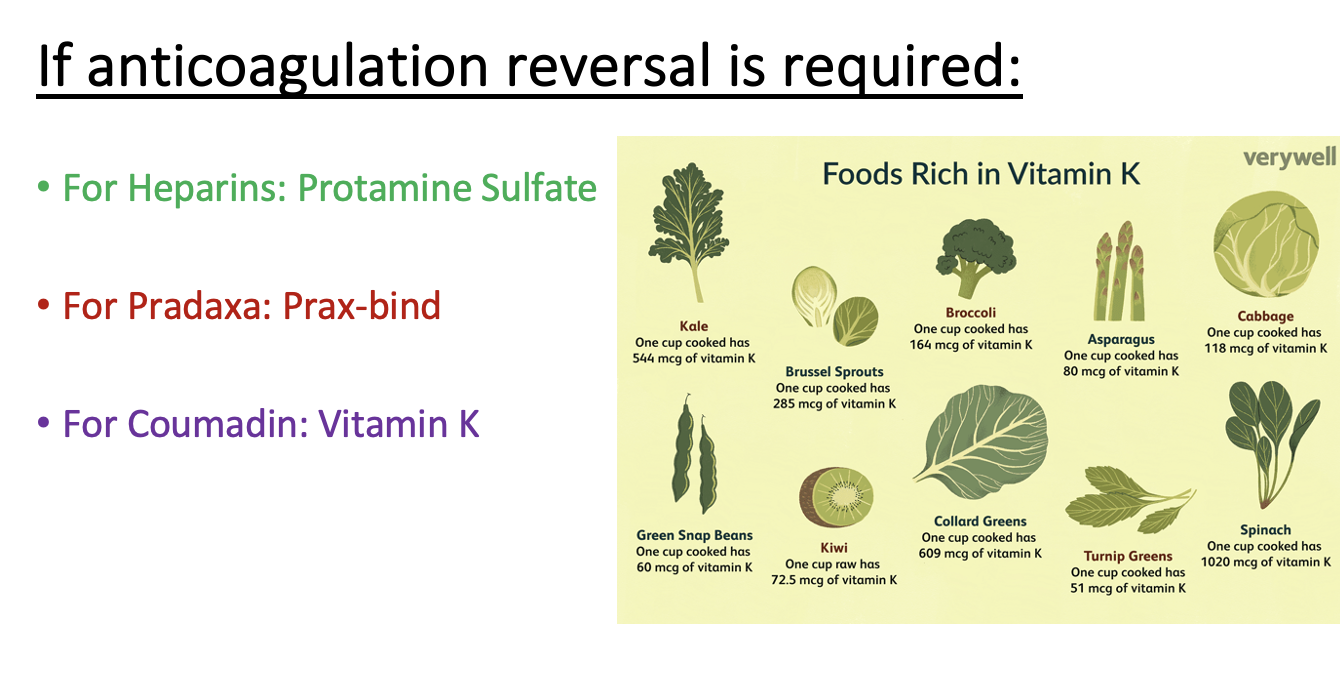
How do we reverse anticoagulation for heparin?
Protamine sulfate
How do we reverse anti-coagulation (so increase clotting) for Pradaxa?
Prax-bind
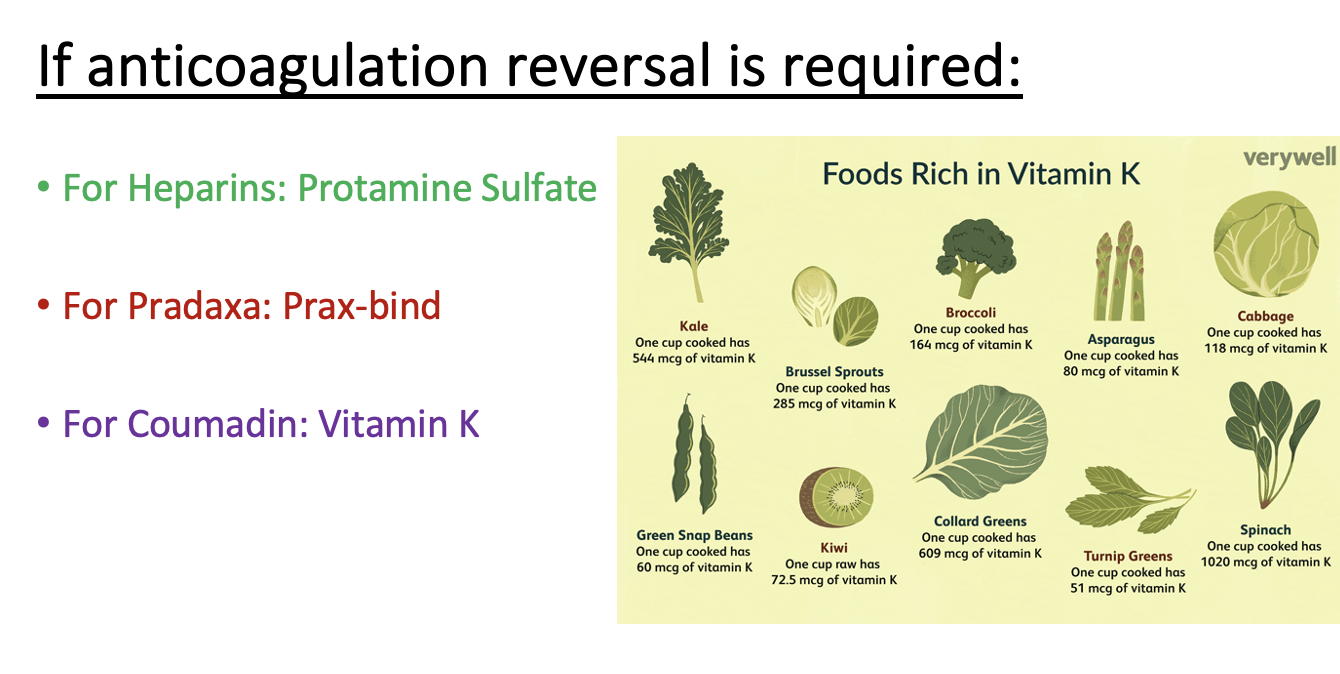
How do we reverse anti-coagulation (so increase clotting) for Warfarm/Coumadin?
Vitamin K
All of your greens are rich in vitamin K and patients on coumadin should avoid them as it’ll increase clotting and fight warfarin