Germs Test 2
1/156
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
157 Terms
Spontaneous Generation
Living organisms and life arose from nonliving matter
Louis Pasteur
From Paris Academy of Sciences, his 1858 experiment showed pasteurization with bend (No growth) vs no bend (growth) in glass
Pasteurization
A method that heats food to kill pathogenic bacteria without ruining the flavor, some bacteria survive
Life From Life
Bacterial growth required exposure to bacteria
Miasma Theory
Ancient origins; disease caused by bad air from rotting/illness, encouraged sanitation
Germ Theory
Microbe life can cause disease, act as pathogens, a less accepted but competing idea
Pathogen
An organism that has potential to cause disease to the host
Robert Koche
Founded Koche’s Postulates, which contributed to Germ Theory
Koche’s Postulates
Microbe must be found in all cases of disease
Microbe must be isolated and cultured in the lab
Microbe must cause the disease when introduced to an uninfected host
Microbe must be isolated from the new diseased host
Stomach Ulcers
Caused by Helicobacter pylori bacteria, spreads via oral-fecal body fluids, infects 50-75% of all people
Ulcer
An open wound that fails to heal
Common Pathogens
The common cold (rhinoviruses)
Gingivitis (S. mutans + P.gingivalis)
Strep Throat (S.pyogenes)
Common Cold
Caused by many major viral groups, over 50% of cases from Rhinoviruses
Common Cold Transmission
Spread via aerosolized droplets from respiratory track and contact with contaminated surface and mucous membrane
Common Cold Infection & Symptoms
Last 7-14 days, include: sore throat, runny nose, coughing, sneezing, headache, tiredness
Common Cold Treatment & Prevention
Most cases resolved by 2nd + 3rd levels of immune defense, social distancing, hand washing, and masks may help although not extensively studied in Rhinoviruses
Gingivitis
Bacteria, Streptococcus mutans and Porphyromonas givgivalis, infesting gingival crevice and creating biofilms that cause plaque
Gingivitis Transmission
S. mutans and P. gingivalis are part of our microbiome, can also be spread from infected individuals via saliva
Gingivitis Infection & Symptoms
Bleeding gums, pockets further enabling bacterial infection
Gingivitis Treatment & Prevention
Can be reversed if not too extensive through removal of plaque and biofilm buildup, regular disruption of biofilm from brushing, flossing, and dental cleaning
Strep Throat
Caused by Streptococcus pyogenes, a group A streptococcus, highly adapted to living in humans
Strep Throat Transmission
Spread via aerosolized droplets from respiratory system, highly contagious and most common in kids. not contagious 24-48 hours after antibiotic treatment
Strep Throat Infection & Symptoms
White streaks on tonsils, red patches, painful and inflamed throat, fever
Strep Throat Treatment & Prevention
identified on blood agar plates then reduced via antibiotics, isolate until antibiotic treatment
Household Pathogens
Tinea
Black Mold
Serratia
Tinea
Caused by Dermatophytes (9 genera of multicellular fungi), include Athletes Foot, Jock Itch, and ringworm on body
Tinea Transmission
Spread vi direct contact with mycelium or specialized spores from humans, animals, or the environment, potentially by clothing, body hair, or surface contact
Tinea Infection & Symptoms
Hyphae and specialized spored (arthroconidia) grow on epidermis, red, rash-like skin which may appear in a ring, inflamed and hyper-sensitive skin that hurts to touch
Tinea Treatment & Prevention
Primarily anti-fungal creams/drugs, limit public exposure when infected
Black Mold
Caused by Stachybotrys chartarum, favors damp/waterlogged habitats, feeds on the plant product cellulose
Black Mold Transmission
Homes with sufficient moisture and warm temps enable mycelium growth, spreading of spores
Black Mold Infection & Symptoms
Not intentionally a human pathogen, caused by respiratory reactions to released spores and organic compounds. Sneezing, coughing, congestion, eye irritation
Black Mold Treatment & Prevention
Removing with anti-microbial cleaners, removing old food source (decaying, damp wood/plant-based products), reduce home moisture levels, address water damage
Serratia
Caused by Serratia marcescens bacterua that consume phosphorous-based substances (soaps and shampoos), favors damp environments
Serratia Transmission
Regularly grow on grout, tiling, curtains, etc. in bathrooms around sinks or drains
Serratia Infection & Symptoms
Generally not a risk, can be issue if internalized in bloodstream via catheters, IVs, needles
Serratia Treatment & Prevention
Antibiotics, although resistance is an issue, prevented by bleach and other conventional household cleaners
Waterborne Pathogens
Crypto (Cryptosporadium parvum)
Giardia (Giardia lamblia)
Crypto (Cryptosporidiosis)
Caused by Cryptosporidium parvum, single-celled eukaryote common in bodies of untreated water, has a high chlorine tolerance
Crypto Transmission
Fecal contamination (both cow and human waste are major spreaders)
Crypto Infection & Symptoms
Burrows into mucous membrane of small intestine, cleared out by immune system defenses in 1-2 weeks if healthy, causes extensive, watery diarrhea
Crypto Treatment & Prevention
Generally by immune defense, clean water to prevent dehydration from diarrhea, prevented by clean drinking water
Giardia (Giardiasis)
Caused by Giardia lamblia, single-celled eukaryote often in bodies of water that contain aquatic wildlife
Giardia Transmission
Fecal-oral contamination, swimming and swallowing water from lakes or ponds, bever ponds are a prominent source
Giardia Infection & Symptoms
1-2 weeks incubation, diarrhea 2-5x per day for 10+ days, abdominal pain, gas, bloating, vomiting and weight loss, lasts 2-6 weeks
Giardia Treatment & Prevention
Generally left up to immune defense, anti-patristics, clean water to prevent dehydration from diarrhea, avoiding swallowing untreated water from ponds/lakes
Foodborne Pathogens
Food molds
Listeria (food) Poisoning (Lysteria monocytogenes)
Food Poisoning (E. coli)
Salmonella (food) poisoning (Salmonella typhi/typhimurium)
Food Molds
Many species, such as penicillin, often affect humans through irritation/allergies to spored or mycotoxins released from hyphae
Food Molds Transmission
Fungal spore ubiquitous in air, porous, moist food at warmer temps
Food Molds Infection & Symptoms
Various illnesses based on species, from mild upset/food poisoning to cancer
Food Mold Treatment & Prevention
No treatment, dispose of any food with indications of mold, reducing moisture and keeping food at colder temps, preservatives
Listeria Poisoning
Caused by Listeria monocytogenes, can cause severe and potentially deadly food poisoning, 3rd leading cause of US foodborne deaths
Listeria Poisoning Transmission
Normally found in soil, spread between people via fecal-oral contamination, often improperly treated or contaminated dairy, mean, produce
Listeria Poisoning Infection & Symptoms
2-4 week incubation, infects intestines and possible into tissues by piercing through cell membrane, diarrhea, vomiting to flu-like symptoms, stiff neck, seizures, confusion, loss of balance
Listeria Poisoning Treatment & Prevention
Immune system if not severe, antibiotics for severe cases, follow basic hand-washing procedures and wash, separate, cook, chill protocols
Food Poisoning
Disease caused by consuming pathogenic microbes
Food Poisoning Infection & Symptoms
Diarrhea, stomach pain/cramps, nausea, vomiting, fever
Food Poisoning Treatment & Prevention
Clean, Separate, Cook, and Chill, washing utensils, produce, and hands, cook animal products to proper temp
Salmonella Poisoning
Caused by Salmonella typhimurium and Salmonella Typhi, several species cause disease and food poisoning in different ways, most common US food poisoning and related death
Salmonella Poisoning Transmission
S. Typhimurium often zoonotic from animal feces, S. Typhi via oral-fecal contamination between humans
Salmonella Poisoning Infection & Symptoms
Inhabit small intestine, develop in 12-72 hours, standard food poisoning symptoms, possible bloody diarrhea, lasts 4-7 days.
Typhoid Fever
Caused by S. typhi, where bacteria inhabit small intestine, but also travels to liver and spleen, symptoms include food poisoning, rash on body/stomach, delirium & convulsions
Salmonella Poisoning Treatment & Prevention
Generally delt with by immune system, antibiotics used in severe cases, wash hands after handling at-risk animals, standard wash, separate, cook chill protocols
E. Coli Poisoning
2nd most common cause of food poisoning, over 700 strains with 6 being the main causes
E. Coli Poisoning Transmission
Most of 6 species directly via human feces, 1 via cattle feces
E. Coli Poisoning Infection & Symptoms
Various parts of gastro-intestinal tract, most outbreaks due to “shiga toxin”, general food poisoning symptoms
E. Coli Poisoning Treatment & Prevention
Dealt with by immune system, blood or urinary use antibiotics, following proper hand-washing and wash, separate, cook, chill procedures
Desiccation
Dehydrating cells; can preserve foods while killing pathogens, endospores and fungal spores may be preserved
Clinical Microbiology
The study of microbes to diagnose and treat pathogenic diseases, must accurately obtain pathogens
Culturing
Growing pathogens; required pathogens to be kept at optimal temperatures in a nutritional medium
Agar
a Jello-like extract of seaweed used to culture many bacteria
Colony
A visible cluster of bacteria derived from 1 cell
Sequencing
After culturing, microbes are examined in multiple ways (shape, metabolism, gram stain cell wall) for diagnosis
Eosin Methylene Blue (EMB) Plate
Dark red/purple, semi transparent. Key for detecting fecal based microbes based on lactose metabolism, purpleish border=fecal-based bacteria, clear colonies = non-fecal bacteria
Blood Agar Plate (BAP)
Color from sheep blood, opaque. key for detecting microbes that can rupture blood cells, Alpha (mild cell rupture, green) Beta (complete rupture, no red around) and gamma (cannot rupture)
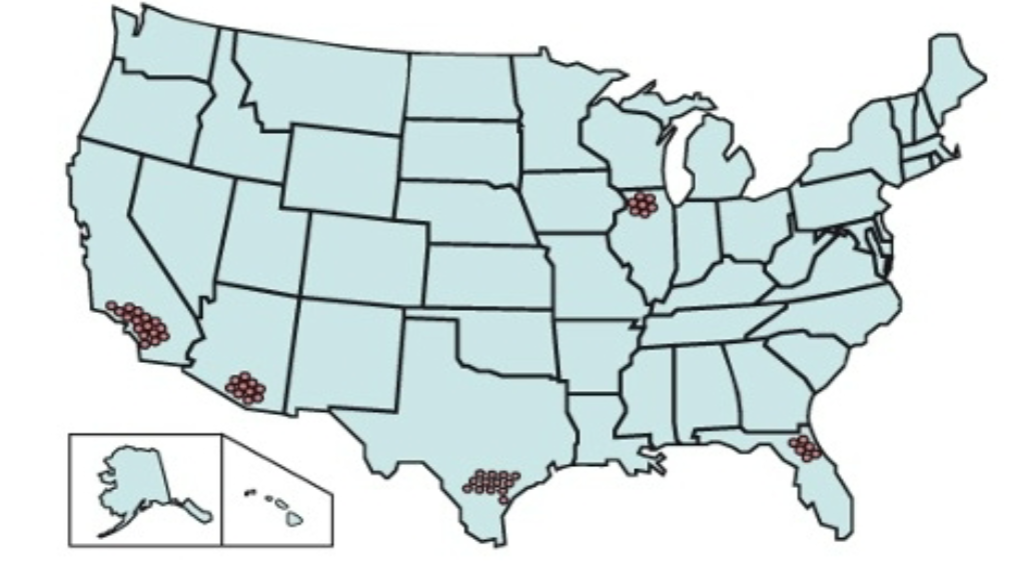
Epidemiology
The tracking and analysis of pathogenic disease distribution patterns, two major focal points are Surveillance and identifying key trends from surveillance
Sporadic
Pathogen reported at irregular intervals at random locations

Endemic
Pathogen as steady frequency over a long period of time in a specific location

Epidemic
Prevalence of pathogen increases over a sporadic or endemic rate
Pandemic
Multiple epidemics across multiple continents

Dr. John Snow
Attempted to identify the source of the cholera outbreak in London in 1854, used epidemiology and ended the outbreak by finding the right water pump
Cholera
Caused by Vibrio cholera, ingested from fecal contamination in water (or food)
Cholera Transmission
Through fresh/saltwater; some live with shellfish, ingested from fecal contamination in water or food
Cholera Infection & Symptoms
1-5 day incubation, infects the small intestine and causes water and electrolytes to flow out of intestinal cells, 10-20 liters of water diarrhea per day, 50-60% rate of death within hours via dehydration
Cholera Treatment & Prevention
Rehydration Therapy (water + glucose + electrolytes), bacteria flushed out of system, antibiotics can help, modern water treatment services
Alexander Flemming
Discovered mold (Penicillin) that killed microbes when studying staphylococci bacteria in 1928
Antibiotic
“Anti-life” toxin that killed bacteria and only bacteria, metabolic by-product of fungal and bacterial microbes
Main Misuses of Antibiotics
Doctors giving when not needed
Patient using when not needed or not fully using amount prescribed
Extensive livestock preventative use
These mean more bacterial cells are regularly exposed to antibiotics and develop antibiotic resistance
Antibiotic Resistance
When bacteria are no longer affected by previously effective antibiotic
Plasmids & Conjugation
How Bacteria Share Antibiotic Resistance Traits
Opportunistic Infections
When microbes find an immune weakness and become pathogenic
Methicillin-resistant Staphylococcus aureus (MRSA)
Resists methicillin, numerous strains also resist other antibiotics
Vancomycin Resistant Enterococci (VRE)
Vancomycin antibiotic a strong response to methicillin and related resistances, some species have become resistant (including MRSA’s)
Enterococci
bacteria common in out intestines, mouths, and female genital tract, opportunistic; serious infections often from major injuries, surgeries, or other hospital procedures
Smallpox
Caused by Variola virus, one of the most deadly human pathogens (about 30% average fatality rate, 3-4 million deaths per year)
Smallpox Transmission
Airborne due to viral load in mouth and contact due to infected skin cells
Smallpox Infection & Symptoms
7-19 day incubation, mostly through upper respiratory system, fever, aches, vomiting, sores in mouth and rash on all skin, scabs
Smallpox Treatment & Prevention
No known treatment, vaccine
Edward Jenner
Pioneered the first vaccination attempt, removed sore from a milkmaid with cowpox and put in in an 8-year-old, then inoculates 8-year-old with smallpox sore and had no ill impact
How Vaccines Work
Mimic antigens for the third defense to learn how to attack