Regional anatomy 12 -- abdomen & pelvis 2
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
Pelvis & perineum
Interrelated regions associated with pelvis bones & terminal parts of vertebral column
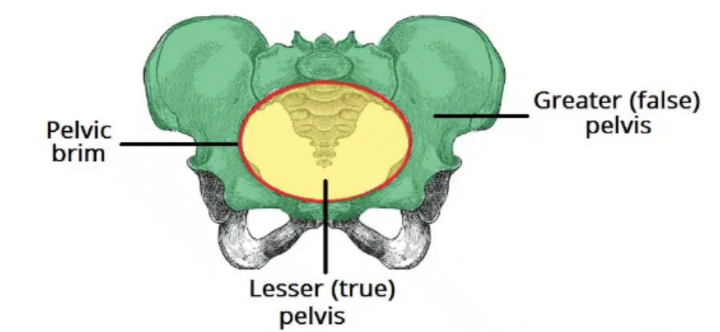
Pelvis is divided into 2 regions —
Greater pelvis (false pelvis) —
Superior, provides support of lower abdominal viscera (ex. ileum & sigmoid colon)
Little obstetric (childbirth) relevance
Related to upper parts of pelvic bones & lower lumbar vertebrae — considered part of abdominal cavity
Lesser pelvis (true pelvis) —
Inferior, contains pelvic cavity & pelvic viscera
Related to inferior parts of pelvic bones, sacrum, & coccyx
Has both an inlet & an outlet
Junction between greater & lesser pelvis — pelvic inlet
Outer bony edges of pelvis inlet — pelvic brim
Perineum is inferior to floor of pelvic cavity — its boundaries form the pelvic outlet
The perineum contains the external genitalia & external openings of the genitourinary & gastrointestinal systems
Functions of the pelvis
Main functions —
Transfer of weight from upper axial skeleton to lower appendicular skeleton, especially during movement
Provides attachment for a number of muscles & ligaments used in locomotion
Contains & protects the abdominopelvic & pelvic viscera
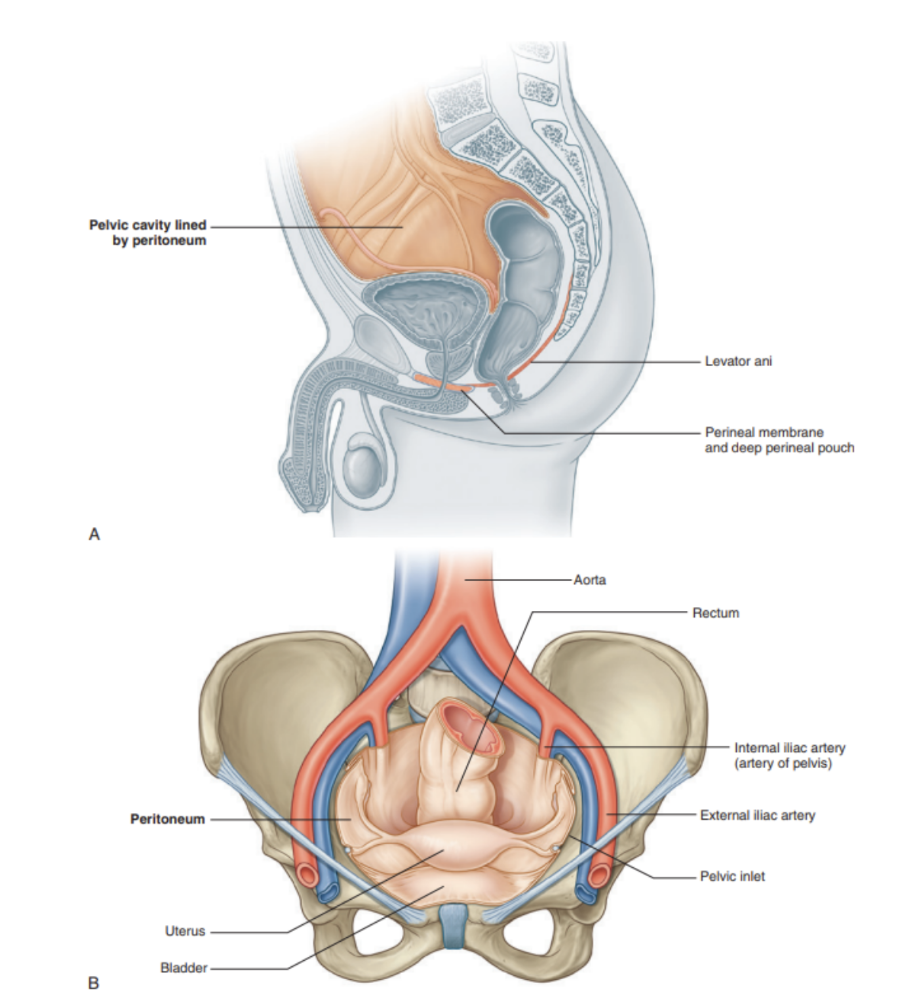
In the pelvic cavity, the bladder is anterior with the rectum posterior in the midline
The bladder —
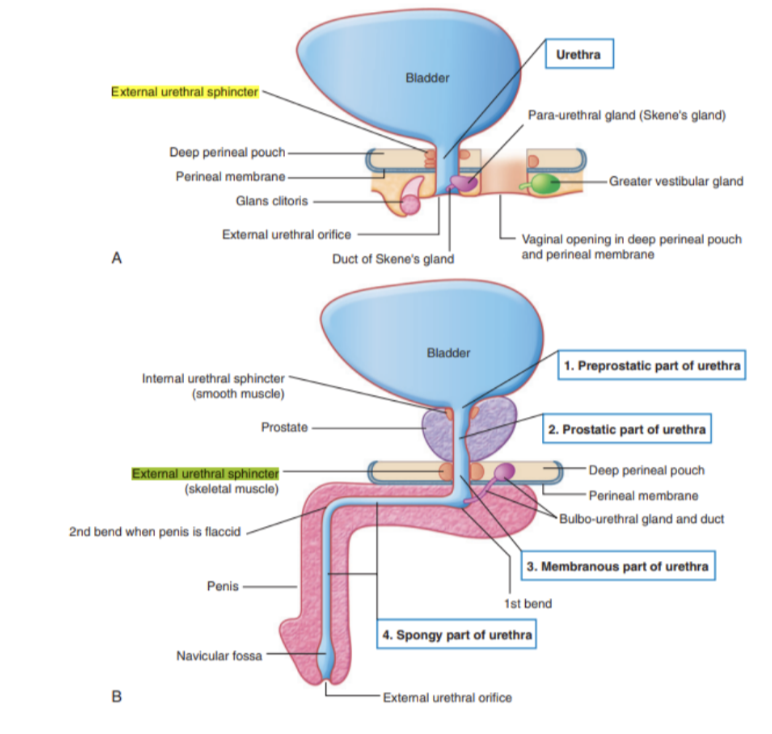
As it fills, it expands superiorly into the abdomen, suppeorted by adjacent elements of the pelvic bone & the pelvic floor. The urethra passes through the pelvic floor to the perineum, where in women it opens externally, & in men it enters the base of the penis
The rectum —
Continuous with the sigmoid colon at S3 and terminating at the anal canal, penetrating through the pelvic floor to open into the perineum
The flexure between the rectum & pelvic floor is maintained by muscles of the pelvic floor — relaxed during defecation
A skeletal muscle sphincter is associated with the anal canal & urethra as each passes through the pelvic floor
The pelvic cavity also contains most of the reproductive tract in woemn & part of it in men —
In women, vagina penetrates pelvic floor to connect with uterus in the pelvic cavity, with the uterus located between the rectum & the bladder, and a uterine/fallopian tube extending laterally on each side toward the pelvic wall to open near the ovary
In men, the pelvic cavity holds the site of connection between urinary & reproductive tracts, also containing major reproductive glands — prostate & 2 seminal vesicles
The pelvis — structure wise (overall)
Pelvic girdle — a ring-like bondy structure in the lower part of the trunk, connecting the axial skeleton to the lower limbs
Posteriorly the inlet is bordered by the body of S1, which projects into the inlet as the sacral promontory
On each side of this vertebra, wing-like transverse processes called the alae (wings) contribute to the margin of the pelvic inlet
Laterally, a prominent rim on the pelvic bone continues the boundary of the inlet forward to the pubic symphysis — where both pelvic bones join on the midline
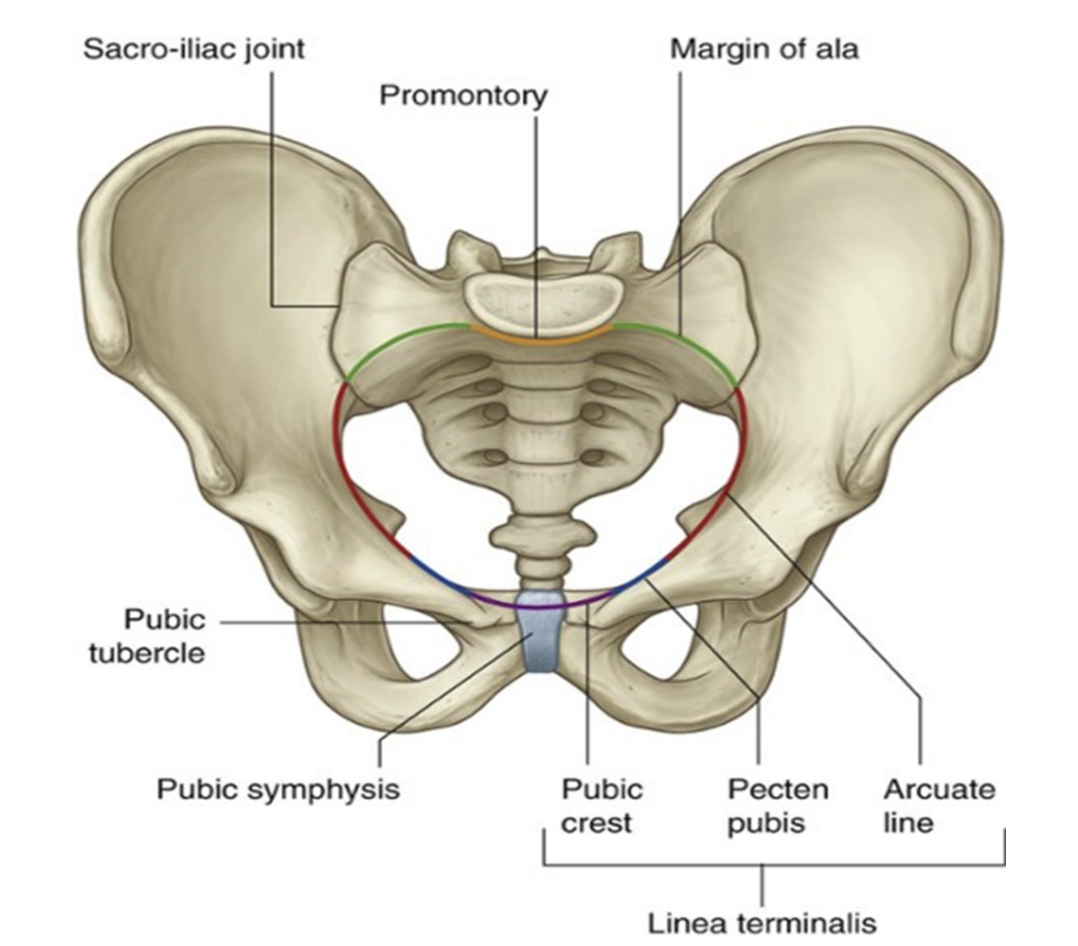
Pelvic inlet
The bony edge/rim surrounding & thus defining the pelvic inlet is the pelvic brim — formed by —
Promontory & ala of the sacrum
(superior surface of its lateral part, adjacent to the sacrum)
Right & left linea terminalis (terminal line) form a continuous oblique ridge together, consisting of the —
Arcuate line on inner ilium surface
Pecten pubic (pectineal line) and pubic crest, forming the superior border of the superior ramus & body of the pubis
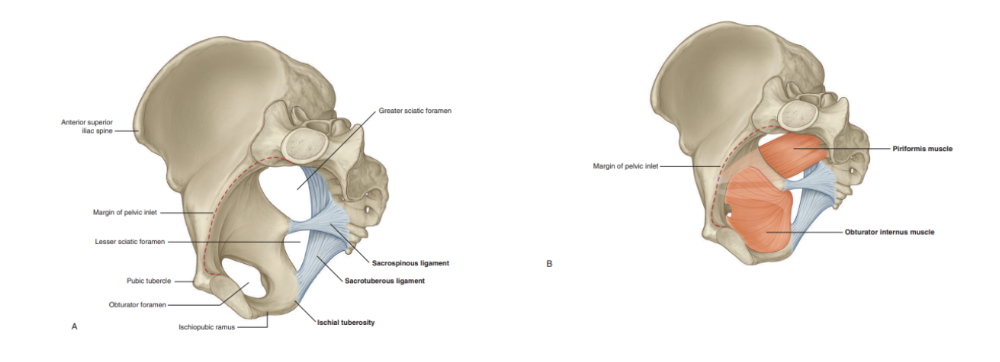
Pelvic wall
Consist of bone, muscle, and ligaments —
Bones —
Sacrum, coccyx, & inferior half of pelvic bones
Ligaments — 2 main —
Sacrospinous ligaments & Sacrotuberous ligaments, which function to link each pelvic bone to the sacrum & coccyx
Also convert 2 notches on the pelvic bones — greater & lesser sciatic notches — into foramina on the lateral pelvic walls
Muscle — specifically the obturator internus & piriformis muscles
Arise in the pelvis & exit through the sciatic foramina to act on the hip joint
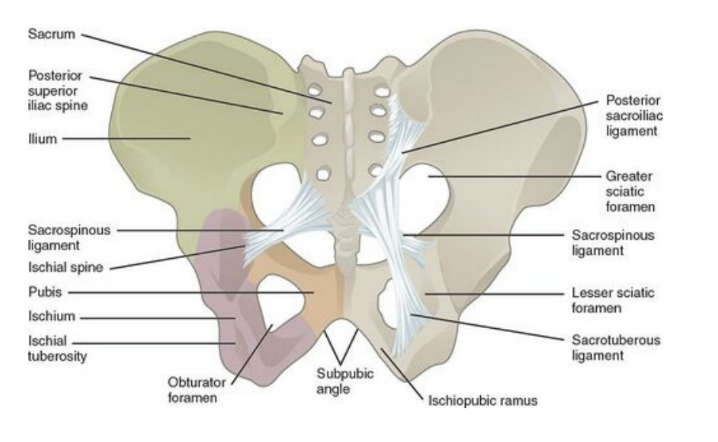
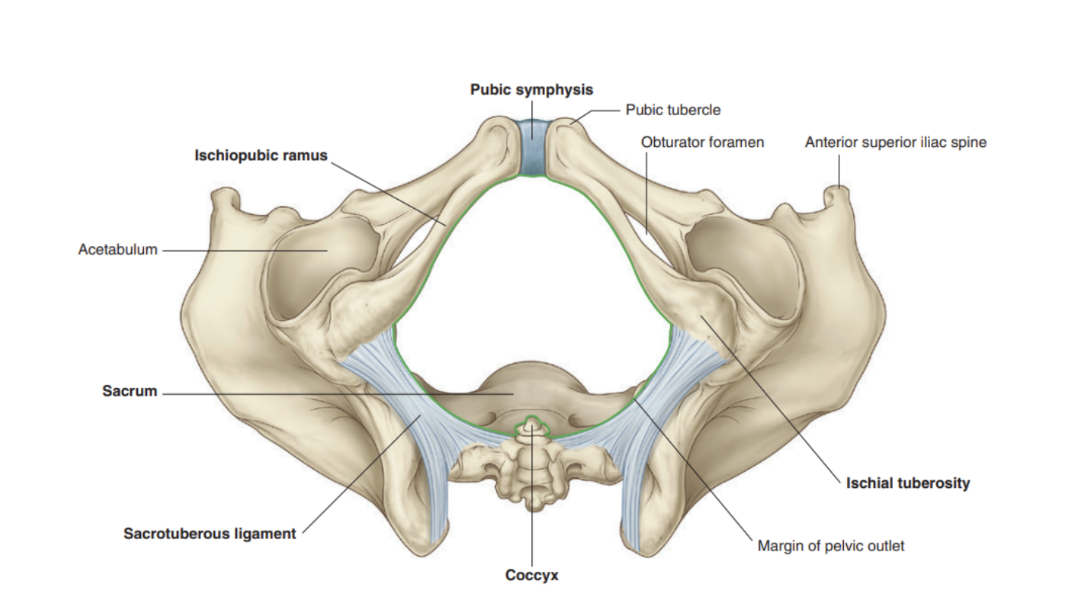
Pelvic outlet
Formed by bone & ligaments —
Bone — on each side, the inferior margin of the pelvic bone projects posteriorly & laterally from the pubic symphysis to end in a prominent tuberosity — ischial tuberosity
These elements construct the pubic arch, forming the margin of the anterior half of the pelvic outlet. The sacrotuberous ligament continues this margin posteriorly from the ischial tuberosity to the coccyx & sacrum
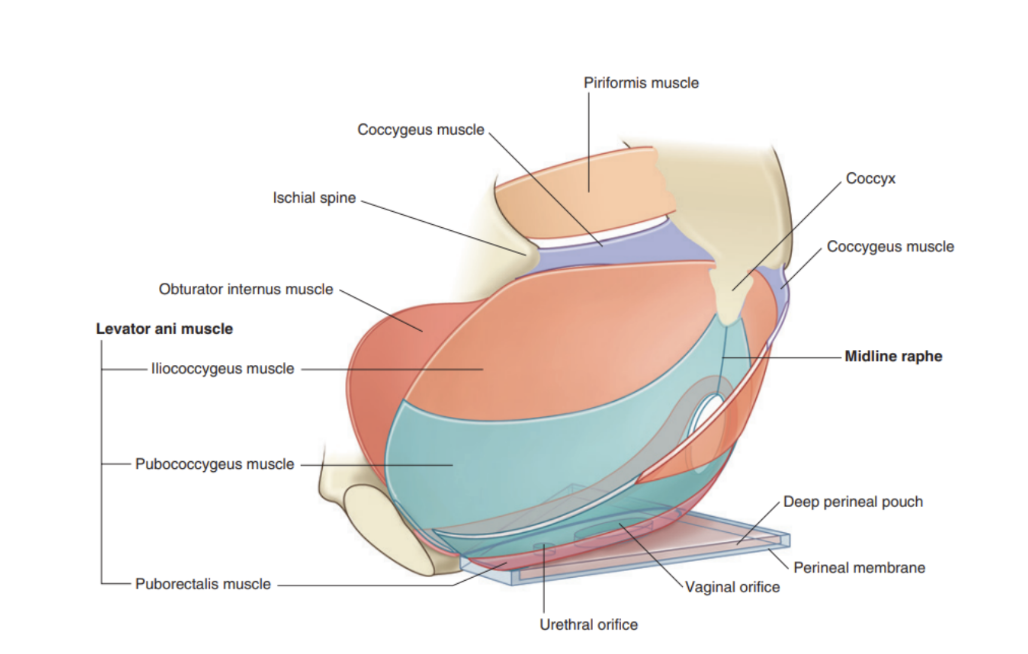
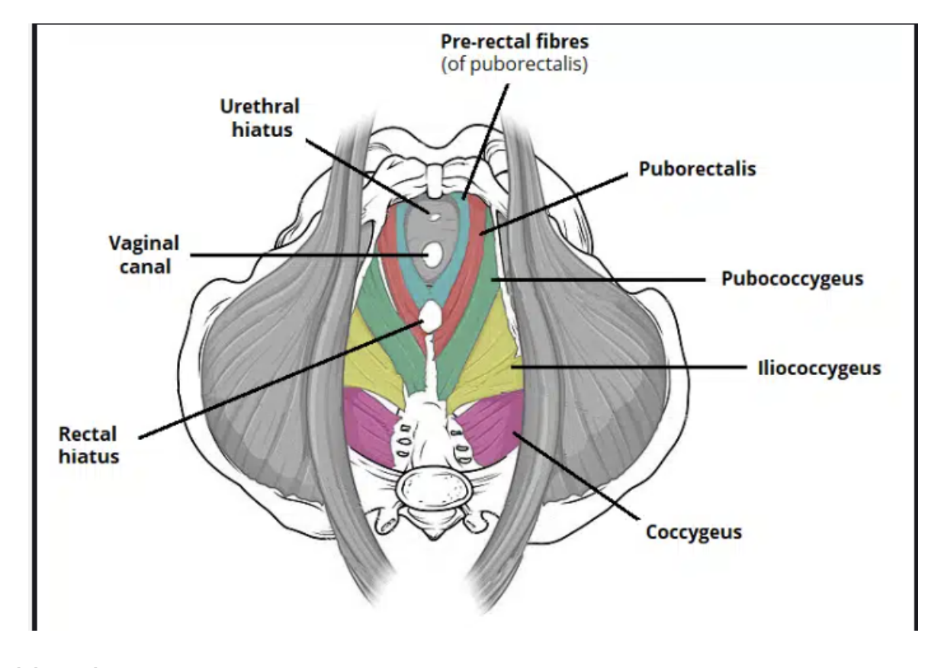
Pelvic floor
Formed by muscles & fascia —
Pelvic diaphragm — one of largest components, with its largest distribution comes from the 2 levator ani muscles attaching peripherally at the connective tissue raphe, with the diaphragm completed by the coccygeous muscles, who overlie the sacrospinous ligamenets & pass between the margins of the sacrum, coccyx, & ischial spine (prominent spine on pelvic bone)
The pelvic diaphragm forms most of the pelvic floor & in its anterior regions contains a U-shaped defect, associated with elements of the urogenital system —
The anal canal passes from pelvis to perineum through a posterior circular orifice in the pelvic diaphragm
Supported anteriorly by —
Perineal membrane — thick triangular fascial sheet filling space between arms of pubic arch, with a free posterior border
Muscles in the deep perineal pouch — a narrow region superior to the perineal membrane
Pelvic cavity
Covered by the peritoneum continuous with that of the abdominal cavity that drapes over the superior aspects of the pelvic viscera, but in most regions doesn’t reach the pelvic floor
The pelvic viscera are located in the midline of the pelvic cavity — bladder anterior & rectum posterior, with the uterus (in women) lying between them
Other structures, such as vessels & nerves, lie deep to the peritoneum in association with the pelvic walls on either side of the pelvic viscera
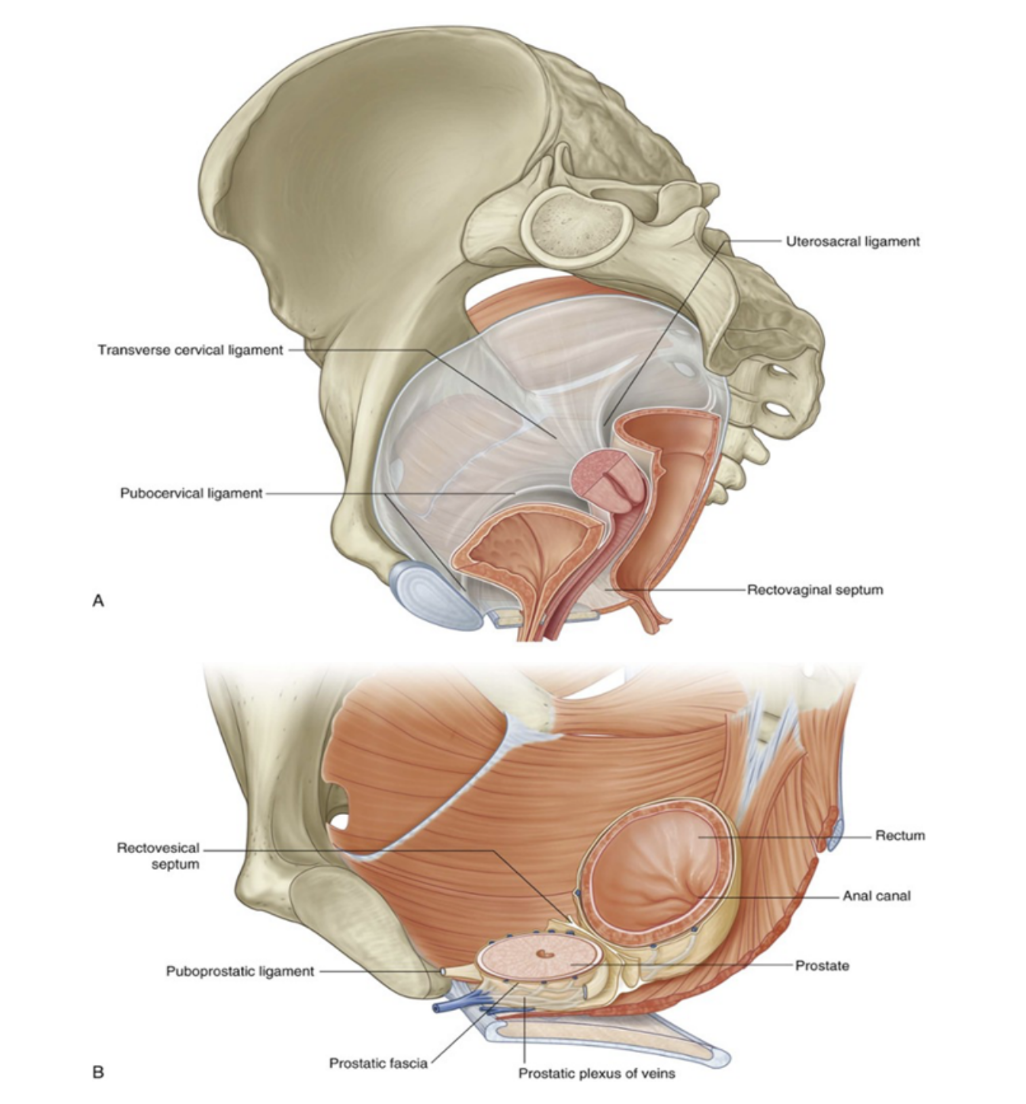
Pelvic fascia
Lines the pelvic walls, surrounds bases of pelvic viscera, & forms sheaths around blood vessels & nerves that course medially from the pelvic walls to reach the viscera in the midline
This pelvic fascia is a continuation of the extraperitoneal connective tissue layer found in the abdomen, with both parietal & visceral compartments
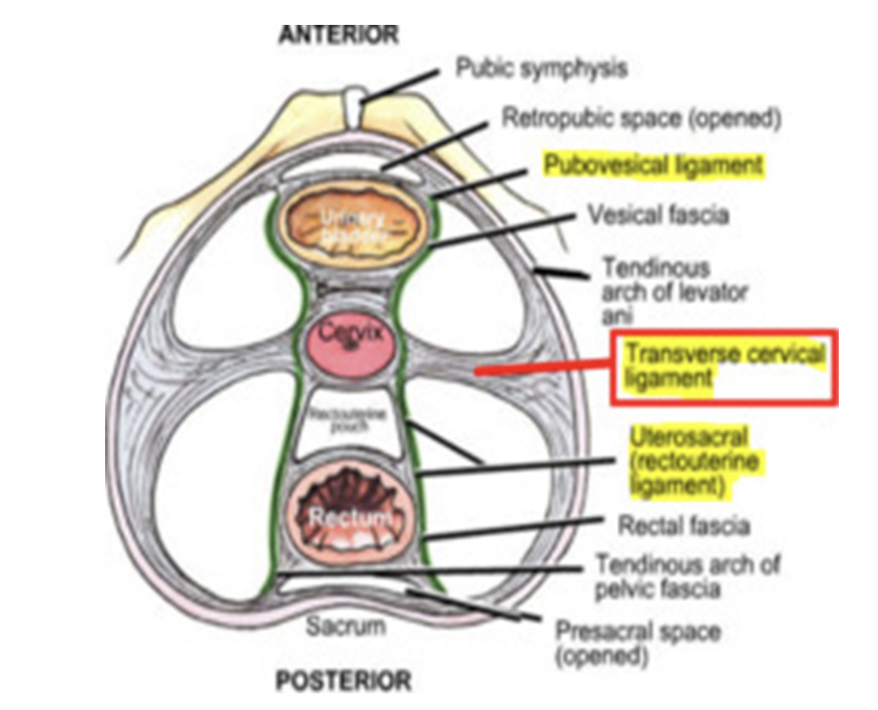
In women (A) —
A rectovaginal septum separates the posterior surface of the vagina from the rectum
Condensations of fascia form ligaments extending from the cervix to the anterior (pubocervical ligament), lateral (transverse cervical or cardinal ligament), and posterior (uterosacral ligament) pelvic walls
These ligaments, along with the perineal membrane, levator ani muscles, & perineal body, are thought to stabilize the uterus in the pelvic cavity
Most important ligaments = transverse cervical or cardinal — extend laterally from each side of cervix & vaginal vault to related pelvic wall
In men (B)
A condensation of fascia around anterior & lateral region of the prostate (prostatic fascia) contains & surrounds the prostatic plexus of veins, continuous posteriorly with the rectovesical septum, which separates the posterior surface of the prostate & base of the bladder from the rectum
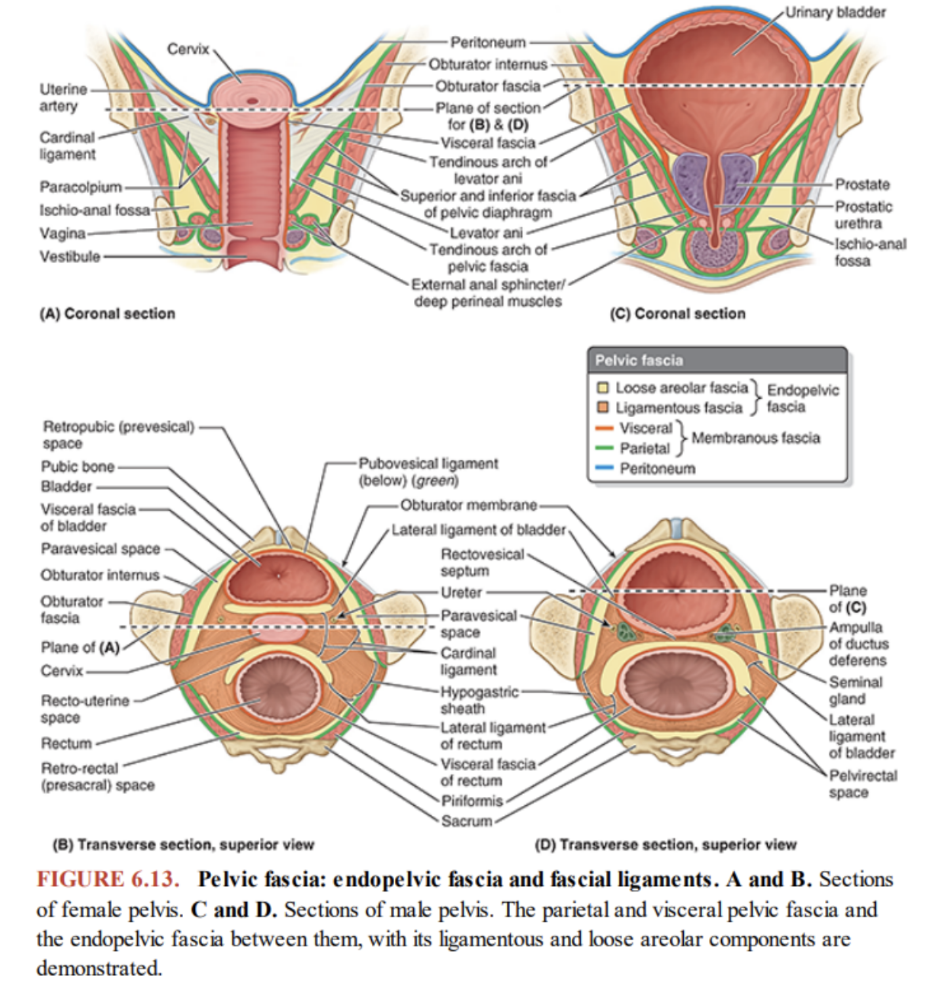
Specificities of pelvic fascia — ligaments (tendinous arch)
Visceral pelvic fascia includes the membranous fascia that directly ensheathes the pelvic organs, forming the adventitial layer of each
Membranous parietal & visceral layers become continuous where the organs penetrate the pelvic floor —
Here, the parietal fascia is thickened, forming the tendinous arch of pelvic fascia, a continuous bilateral band running from the pubis to the sacrum along the pelvic floor adjacent to the viscera
The anteriormost part of this tendinous arch — puboprostatic (males) or pubovesical (females) ligament — connects prostate to pubic in male or fundus (base) of bladder to pubis in female
The posteriormost part of this tendinous arch runs as the sacrogenital ligaments from the sacrum around the side of the rectum to attach to the prostate in the male or the vagina in the female
In females, the lateral connection of the visceral fascia of the vagina with the tendinous arch of the pelvic fascia is the paracolpium
The paracolpia suspend the vagina between the tendinous arches, assisting it in bearing the weight of the fundus of the bladder
Internal iliac artery (overall)
Major artery of the pelvis, originating at bifurcation of common iliac artery at level L5-S1
Descends inferiorly between the external iliac vein & obturator nerve, crossing pelvic inlet to enter the lesser pelvis
At the superior border of the greater sciatic foramen, it divides into anterior & posterior trunks
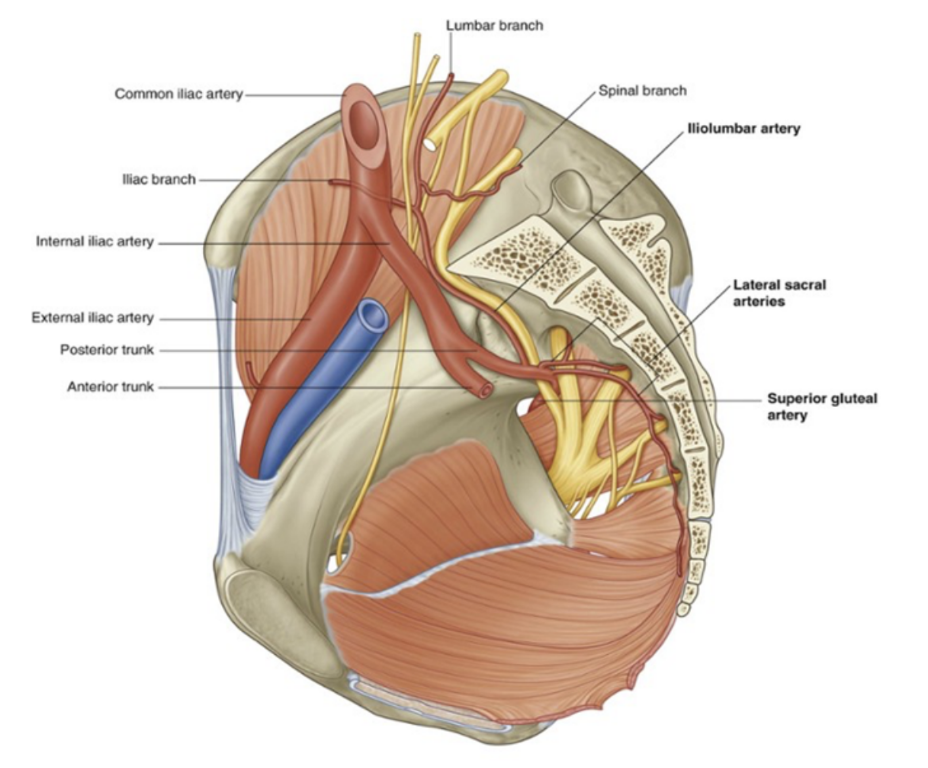
Posterior trunk of internal iliac artery
3 branches —
Iliolumbar artery —
Ascends laterally back out of pelvic inlet to divide into a lumbar & an iliac branch —
Lumbar branch — contributes to supply of posterior abdominal wall, psoas & quadratus lumborum muscles, and cauda equina, via a small spinal branch passing through the intervertebral foramen between LV & S1
Iliac branch — passes laterally into iliac fossa to supply muscle & bone
Lateral sacral arteries (usually 2) —
Course medially & inferiorly along posterior pelvic wall, giving rise to branches that pass into the anterior sacral foramina to supply related bone & soft tissues, structures in the sacral vertebral canal, and skin & muscle posterior to the sacrum
Superior gluteal artery —
Largest branch of internal iliac artery — terminal continuation of posterior trunk, coursing posteriorly, usually between lumbosacral trunk & anterior ramus of S1, to leave the pelvic cavity through the greater sciatic foramen above the piriformis muscle to enter the gluteal region of the lower limb
It makes a substantial contribution to the lood supply of muscles & skin in the gluteal region & also supplies branches to adjacent muscles & bones of the pelvic walls
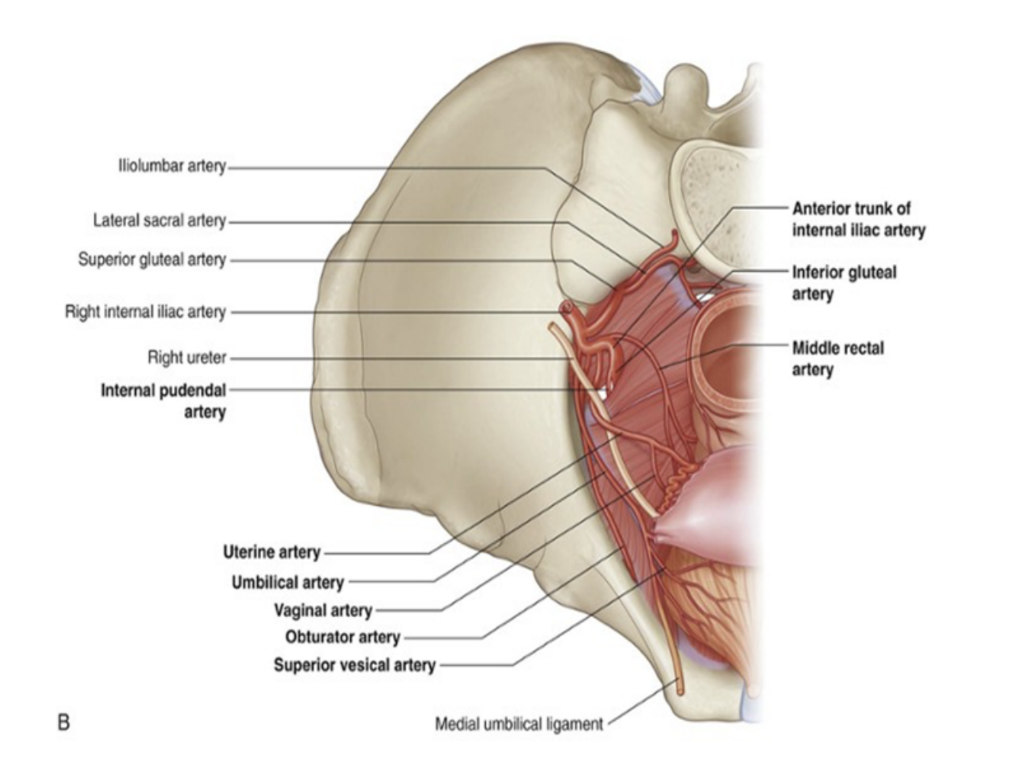
Anterior trunk of internal iliac artery
Gives rise to numerous branches supplying the pelvic organs, perineum, and gluteal &adductor regions of the lower limb —
Obturator artery —
Travels through obturator canal, accompanies by the obturator nerve & vein, to supply the muscles of the thigh’s adductor regions
Umbilical artery —
Gives rise to the superior vesical artery, supplying the superior aspect of the urinary bladder
During pregnancy, transports deoxygenated blood from the fetus to the placenta
Inferior vesical artery —
Supplies lower aspect of bladder, and in males also supplies the prostate gland & seminal vesicles
Vaginal artery (female) — (from uterine)
Descends to vagina, supplying additional branches to inferior bladder & rectum
Uterine artery (female) —
Travels in the cardinal ligament to reach the cervix, where it ascends along the lateral aspect of the uterus
At origin of fallopian tubes, it anastomoses with the ovarian artery
During its course, it crosses the ureters superiorly
Middle rectal artery —
Travels medially to supply the distal part of the rectum, also forming anastomoses with the superior rectal artery (derived from the inferior mesenteric) and the inferior rectal (from internal pudendal)
Internal pudendal artery —
Moves inferiorly to exit pelvis via greater sciatic foramen, and then is accompanied by the pudendal nerve as it enters the perineum via the lesser sciatic foramen
Main artery responsible for blood supply to perineum
Inferior gluteal artery —
Terminal branch of anterior trunk, leaving pelvic cavity via greater sciatic foramen, emerging inferiorly to the piriformis muscle in the gluteal region
Contributes to blood supply of gluteal muscles & hip joint
Venous drainage of pelvis
Internal iliac vein (hypogastric vein) —
Short vessel found in pelvis, arising from several smaller veins just above the greater sciatic foramen
Has a short superior course over the iliacus muscle, after which it merges with external iliac vein to form the common iliac vein
Main function — coveys blood from pelvic viscera into common iliac vein, also providing an alternative route for venous return of lower extremity in the case of external iliac vein obstruction
Single deep dorsal vein draining erectile tissues of clitoris/penis doesn’t follow branches of internal pudendal artery into the pelvic cavity — instead passes directly into cavity through a gap between the arcuate pubic ligament & anterior margin of perineal membrane, to join the prostatic plexus of veins in men or vesical/bladder plexus of veins in women
(Superficial veins draining skin of penis/clit drain into external pudendal veins, which are tributaries of the great saphenous vein in the thigh)
In addiiton to tributaries of internal iliac vein, median sacral & ovarian veins parallel courses of median sacral & ovarian artery to leave the pelvic cavity to join veins in the abdomen —
Median sacral veins — coalesce to form a single vein joining either left common iliac vein or junctions of 2 common iliac veins into inferior vena cava
Overian veins — follow course of corresponding arteries — on left join left renal vein, on right join inferior vena cava
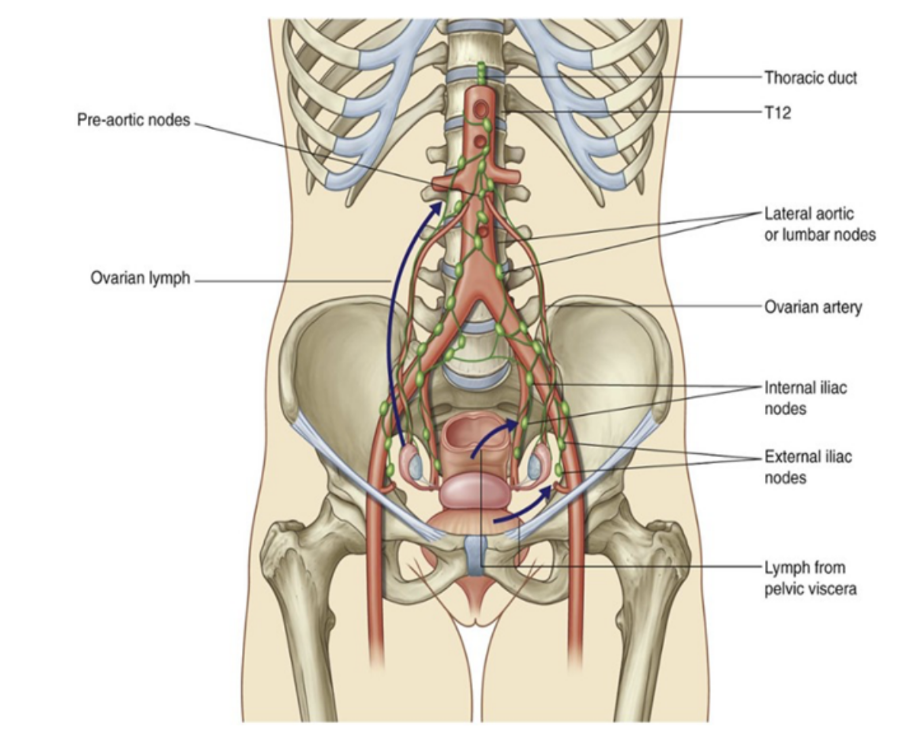
Lymphatics of pelvis
Lymphatics from most pelvic viscera mainly drain into lymph nodes along the internal & external iliac arteries, as well as their associated branches, which drain into nodes associated with the common iliac arteries & then into the lateral aortic or lumbar nodes associated with the lateral surfaces of the abdominal aorta
In turn, these lateral aortic or lumbar nodes drain into the lumbar trunks, which continue to the origin of the thoracic duct at approximately vertebral level T12
Lymphatics from ovaries & related parts of uterus/uterine tubes leave pelvic cavity superiorly
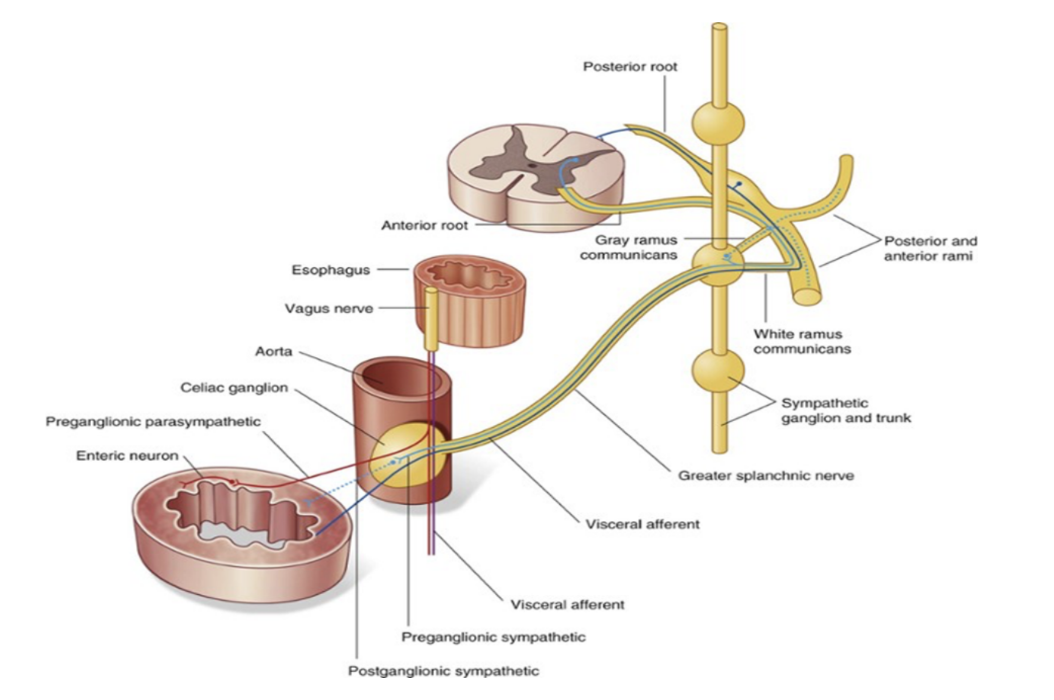
Pelvic splanchnic nerves
Only splanchnic nerves that carry parasympathetic fibers — don’t originate from the sympathetic trunks, rather directly from the anterior rami of S2-S4
Preganglionic parasympathetic fibers originating in the sacral spinal cord pass from S2-S4 spinal nerves to the inferior hypogastric plexus
Once in this plexus, some pass upward to enter the abdominal prevertebral plexus & distribute with the arteries supplying the hindgut
This provides the pathway for innervation of the distal 1/3 of the transverse, descending, & sigmoid colon by preganglionic parasympathetic fibers
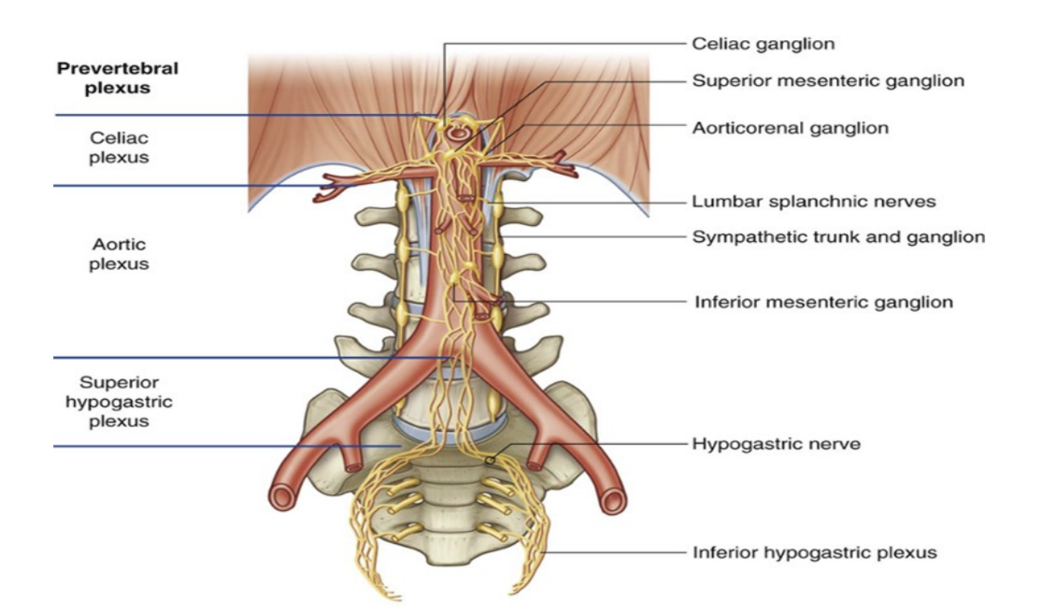
Abdominal prevertebral plexus & ganglia
Abdominal prevertebral plexus — collection of nerve fibers surrounding the abdominal aorta & is continuous onto its major branches
Scattered throughout the length of the plexus are cell bodies of postganglionic sympathetic fibers, some of which are organized into distinct ganglia, while others are more random in their distribution
The ganglia are usually associated with specific branches of the abdominal aorta, named after these branches
3 major divisions —
Celiac, aortic, & superior hypogastric plexuses
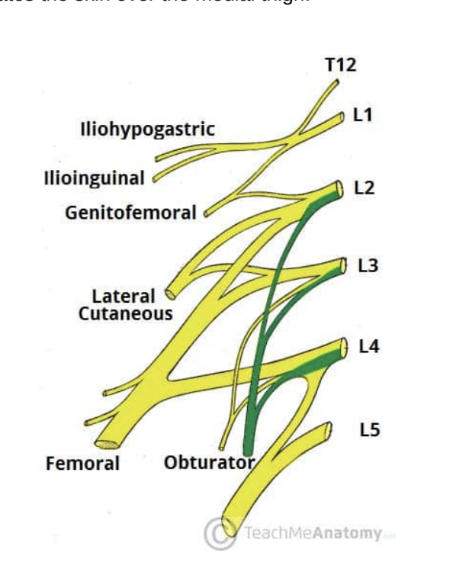
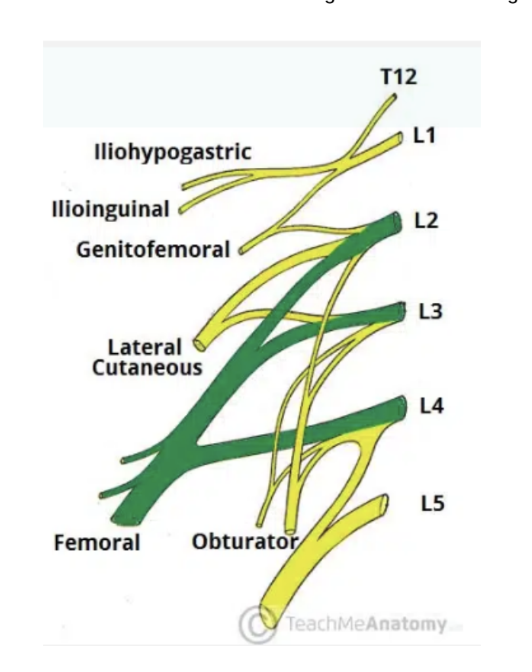
Lumbar nerve plexus
Network of nerve fibers that supplies the skin & musculature of the lower limb — located in lumbar region, in the substance of the psoas major muscle & anterior to the transverse processes of the lumbar vertebrae
Formed by the anterior rami of L1-4, also receiving contributions from T12
These anterior rami then divide into several cords that combine together to form the 6 major peripheral nerves of the lumbar plexus, which descend down the posterior abdominal wall to reach the lower limb, where they innervate their target structures — branches —
Iliohypogastric, Ilioinguinal, Genitofemoral, Lateral cutaneous, Obturator, & Femoral — pneumonic —
I, I Get Leftovers On Fridays
Iliohypogastric nerve
First major branch of lumbar plexus — runs to iliac crest, across quadratus lumborum muscle of the posterior abdominal wall, to then perforate the trasversus abdominis & divide into its terminal branches
Roots — L1 (with T12 contributions)
Motor function — innervates internal oblique & transversus abdominis
Sensory function — innvervates posteriolateral gluteal skin in pubic region
*tip to remember iliohypogastric is before ilioinguinal — H is before I in alphabet
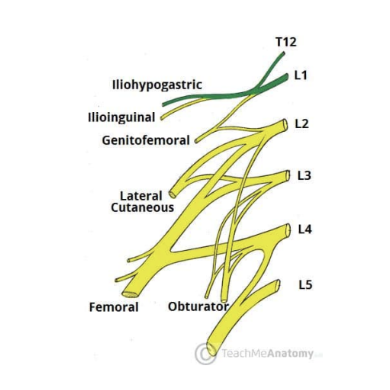
Ilioinguinal nerve
2nd branch of lumbar plexus — follows same anatomical course as the larger iliohypogastric nerve — after innervating muscles of anterior abdominal wall, it passes through the superficial inguinal ring to innervate the skin of the genitalia & middle thigh
Roots — L1
Motor functions — innervates internal oblique & transversus abdominis
Sensory functions — Innervates skin on superior antero-medial thigh
In males also supplies skin over root of penis & anterior scrotum
In females also supplies skin over mons pubis & labia majora
Genitofemoral nerve —
3rd branch of lumbar plexus — after leaving psoas major muscle, quickly divides into a genital & femoral branch
Roots — L1 & L2
Motor functions — Genital branch innervates cremasteric muscle
Sensory functions — Genital branch innervates skin of anterior scrotum in males, or skin over mons pubis & labia majora in females. Femoral branch innervates skin on upper anterior thigh
Lateral cutaneous nerve of the thigh —
4th branch of lumbar plexus — purely sensory function — enters thigh at lateral aspect of inguinal ligament, where it provides cutaneous innervation to the skin there
Roots — L2 & L3
Motor functions — none
Sensory functions — innervates anterior & lateral thigh down to knee level
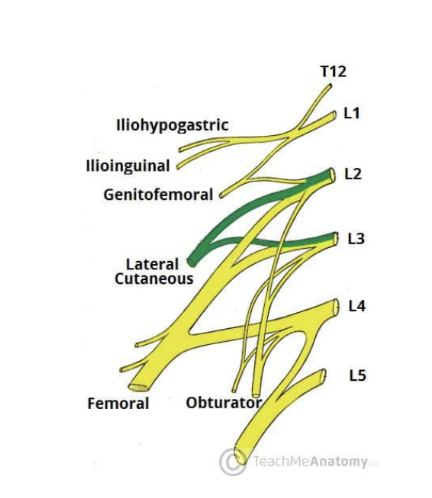
Obturator nerve
5th branch of lumbar plexus
Roots — L2, L3, L4
Motor functions — innervates muscles of medial thigh —
Obturator externus, adductor longus, adductor brevis, adductor magnus & gracilis
Sensory functions — innervates skin over medial thigh
Femoral nerve —
6th/last branch of lumbar plexus
Roots — L2,L3,L4
Motor functions — innervates muscles of anterior thigh —
Iliacus, pectineus, sartorius, & quadriceps femoris
Sensory functions — innervates skin on anterior thigh & medial leg
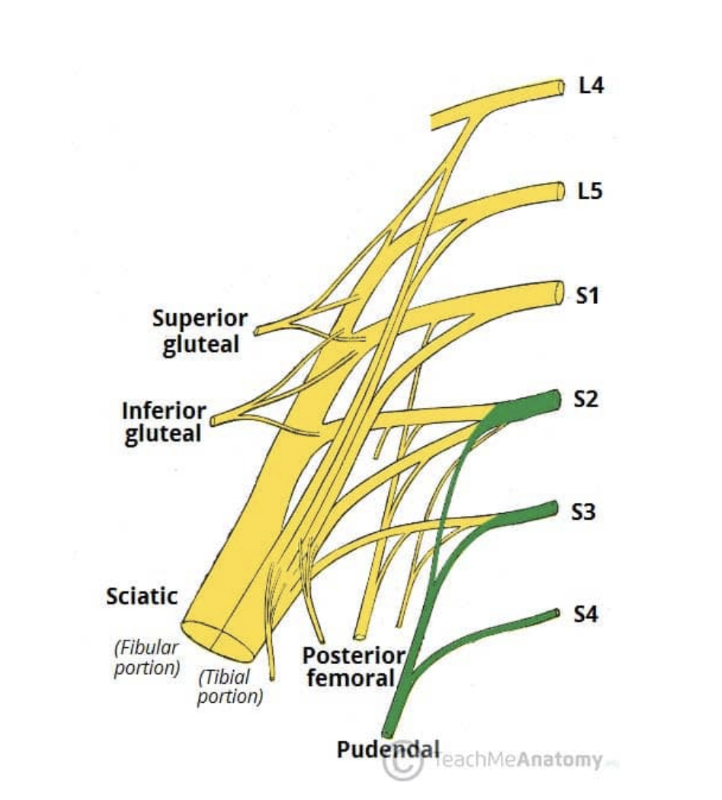
Sacral & coccygeal plexus
Sacral plexus — network of nerve fibers supplying skin & muscles of pelvis & lower limb, located on surface of the posterior pelvic wall anterior to the piriformis muscle
Formed by the anterior rami of S1-S4, aswell as contributions from L4 & L5
L4 & L5 form lumbosacral trunk, then descending into pelvis to meet sacral roots as they emerge from spinal cord
5 main peripheral Branches —
Superior gluteal, Inferior gluteal, Sciatic, Posterior femoral cutaneous, Pudendal
Mmnemonic — Some Irish Sailor Pesters Polly
2 main destinations for the branches —
Leave pelvis via greater sciatic foramen, entering the gluteal region of the lower limb to innervate the structures there
Remain in the pelvis — innervating pelvic muscles, organs, & perineum
Superior gluteal nerve
1st main branch of Sacral plexus — leaves pelvis via greater sciatic foramen to enter the gluteal region superiorly to piriformis muscle, along with the superior gluteal artery & vein
Roots — L4, L5, S1
Motor functions — innervates gluteal minimus, gluteus medius, & tensor fascia lata
Sensory functions — none

Inferior gluteal nerve
2nd main branch of Sacral plexus — leaves pelvis via greater sciatic foramen to enter gluteal region inferiorly to piriformis muscle, along with inferior gluteal artery & vein
Roots — L5, S1, S2
Motor functions — innervates gluteus maximus
Sensory functions — none
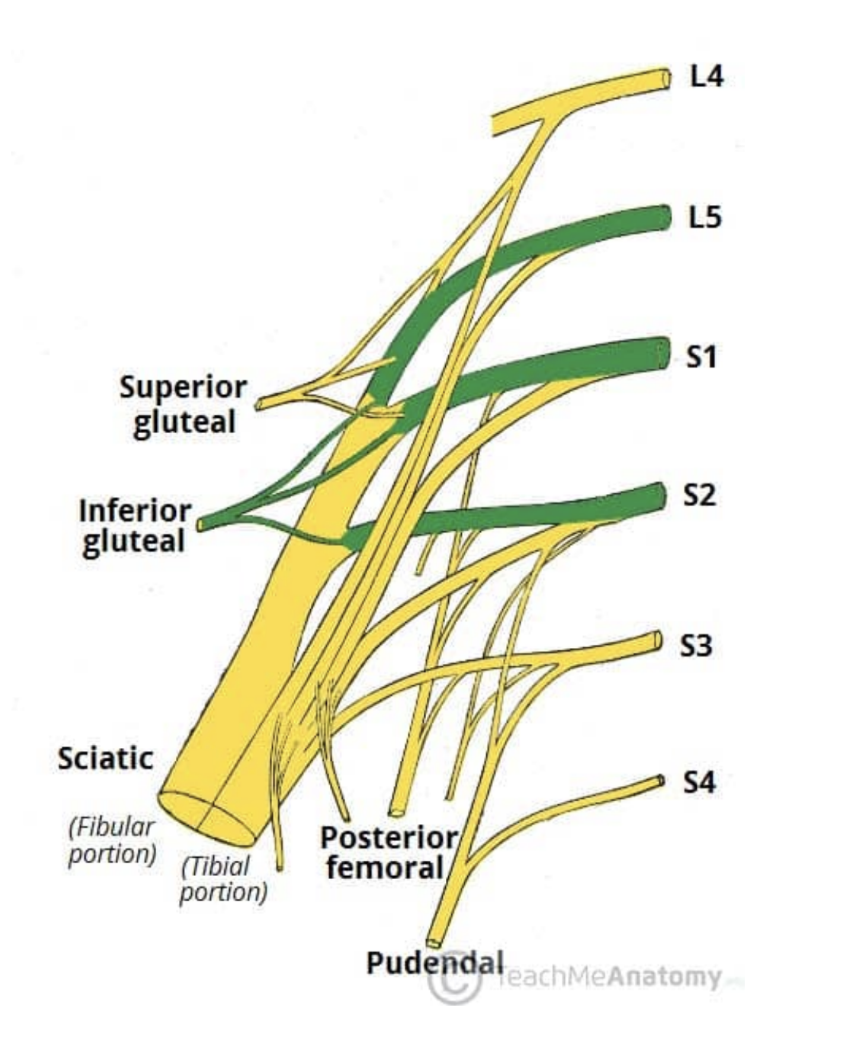
Sciatic nerve
3rd major branch of sacral plexus
Roots — L4, L5, S1, S2, S3
Motor functions —
Tibial portion — innervates muscles in posterior compartment of the thigh *except for short head of biceps femoris), and the hamstring component of adductor magnus. Innervates all muscles in the posterior compartment of the leg & sole of foot
Common fibular portion — innervates short head of biceps femoris, all muscles in anterior & lateral compartments of leg, & extensor digitorum brevis
Sensory functions —
Tibial portion — supplies skin of posterolateral leg, lateral foot, & sole of foot
Common fibular portion — supplies skin of lateral leg & dorsum of the foot
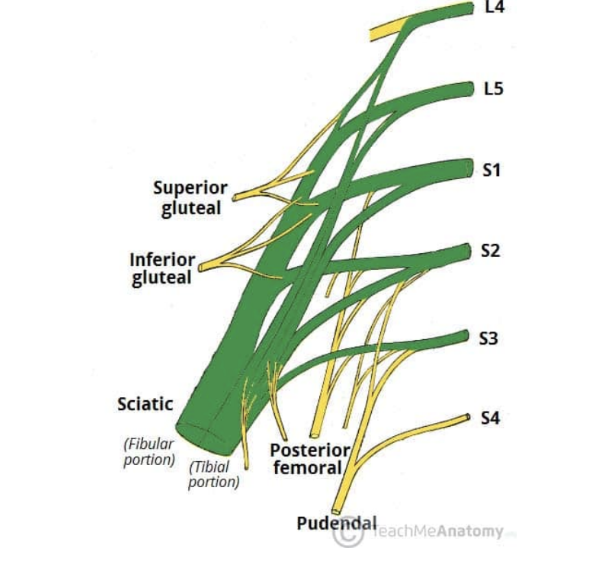
Posterior femoral cutaneous
4th major nerve of Sacral plexus — leaves pelvis via greater sciatic foramen, enterior gluteal region inferiorly to the piriformis muscle, where it then descends deep to the gluteus maximus & runs down back of thigh to the knee
Roots — S1, S2, S3
Motor functions — none
Sensory functions — innervates skin on posterior surface of the thigh & leg, also innervating skin of perineum
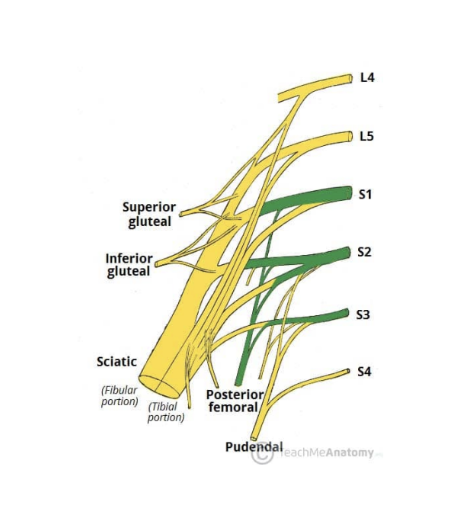
Pudendal nerve
5th/last major nerve of Sacral plexus — Leaves pelvis via greater sciatic foramen, then re-renters via lesser sciatic foramen, then moves anterosuperiorly along the lateral wall of the ischiorectal fossa, terminating by dividing into several branches
Roots — S2, S3, S4
Motor functions — innervates skeletal muscles in perineum, external urethral sphincter, external anal sphincter, & levator ani
Sensory functions — innervates penis/clitoris and most of skin of perineum
(functions of pudendal nerve mmnemonic — S2, S3, S4 keeps poo off the floor!)
Other branches of Sacral plexus
Other than the 5 major branches, there are a number of smaller branches — tend to directly supply muscles —
Nerve to piriformis
Nerve to obturator internus
Nerve to quadratus femoris
Exceptions —
Perforating cutaneous nerve — supplies skin over inferior gluteal region
Pelvic splanchnic nerves — innervate abdominal viscera
Sacral sympathetic trunks
Inferior continuation of the lumbar sympathetic trunks — each sacral trunk is smaller than the lumbar & usually includes 4 sympathetic ganglia
The sacral trunks descend on the pelvic surface of the sacrum (just medial to pelvic sacral foramina) and converge to form the small median ganglion impar (coccygeal ganglion) anterior to the coccyx
They then descend posterior to the rectum in the extraperitoneal connective tissue & send communicating branches (gray rami communicantes) to each of the anterior rami of the sacral & coccygeal nerves
Also send small branches to median sacral artery & inferior hypogastric plexus
Primary function — provide postsynaptic fibers to the sacral plexus for sympathetic (vasomotor, pilomotor, & sudomotor) innervation of the lower limb
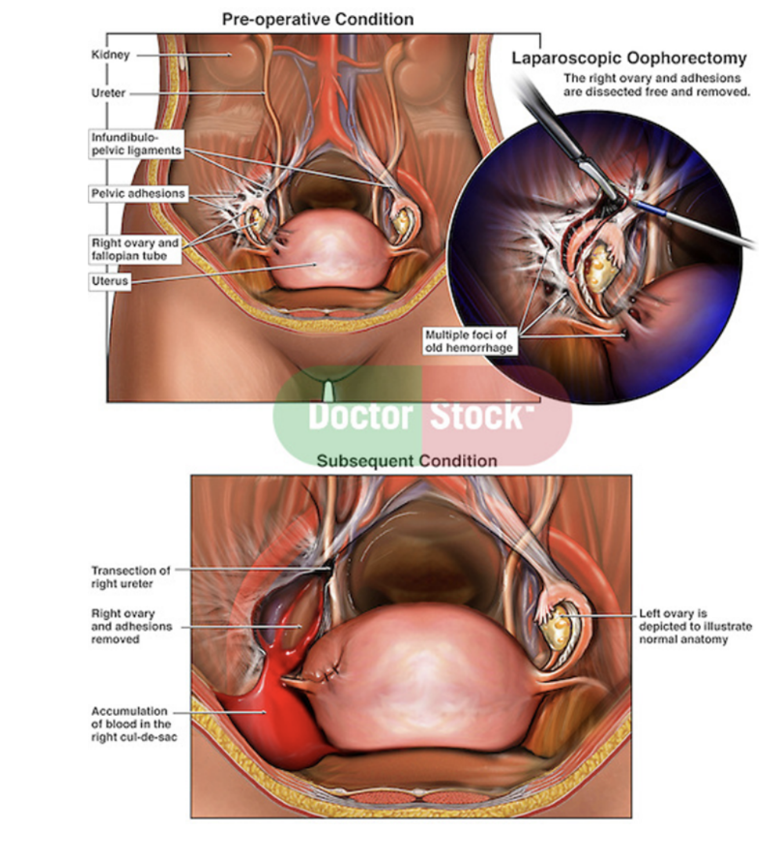
Clinical drop — Oophorectomy
Surgical removal of 1 or both ovaries — can be done laparoscopically (tube camera) unless otherwise indicated
May be performed for ovarian pathology (ex. neoplasm), risk-reducing purposes (reducing risk of reoperation or cancer), or fertility preservation
In children & adolescents specifically — ovarian sparing surgery is a viable approach in most cases of torsion & benign ovarian masses —
Ovaries are responsible for sex hormone synthesis — thus risk of bilateral oophorectomy must be weighed against the benefits — reviewing anatomy & physiology of ovaries, indications & techniques for oophorectomy, & complications for gynecologic adnexal surgery
Perineum —
The shallow compartment of the body (perineal compartment) bounded by the pelvic outlet & separated from the pelvic cavity by the fascia covering the inferior aspect of the pelvic diaphragm (formed by the levator ani & coccygeus muscles)
In the anatomical position, the perineal region is the narrow region between the proximal parts of the thigh
However, when thighs are abducted, it is a diamond shaped area extending from mons pubic anteriorly in females, the medial surfaces (insides) of the thighs laterally, and the gluteal folds & superior end of the intergluteal (natal) cleft posteriorly
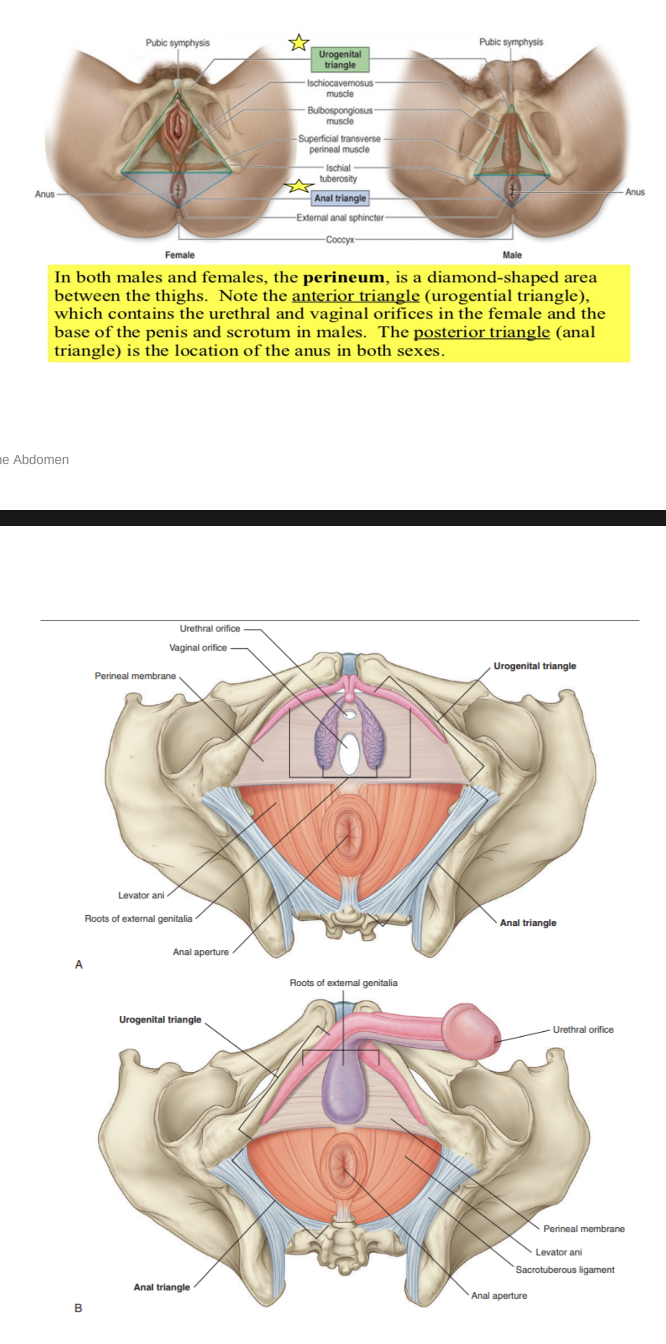
An imaginary line between the ischial tuberosities divides the perineum into 2 triangular regions —
Anteriorly — urogenital triangle —
Contains roots of external genitalia, and — in women openings of uterus & vagina — in men istal part of urethra is enclosed by erectile tissues & opens at the end of the penis
Posteriorly — anal triangle —
Contains anal aperture
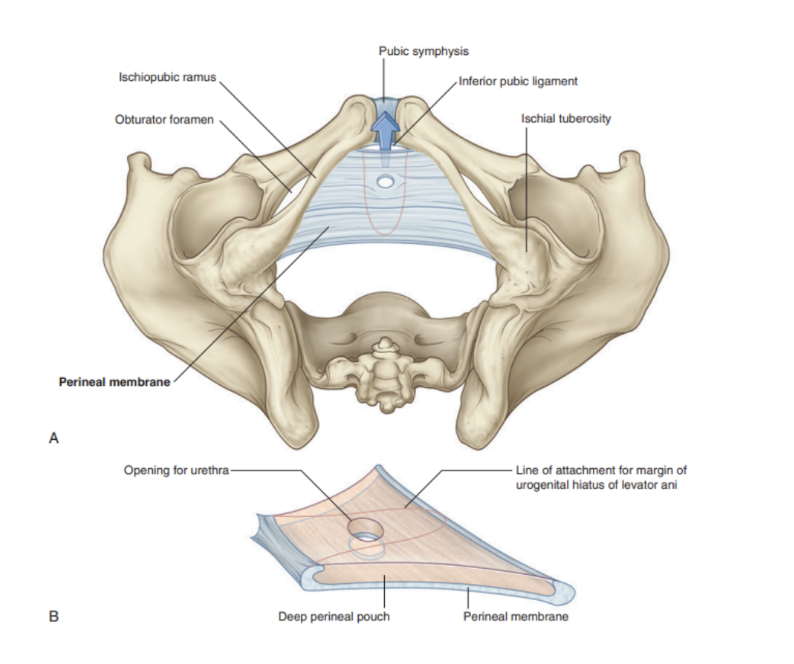
Perineal membrane
Thick fascial, triangular structure attached to bony framework of pubic arch
Oritented in horizontal plane with a free posterior margin
Anteriorly, presence of small gap between membrane & inferior pubic ligament (a ligament associated with pubic symphysis)
Related to a thin space called the deep perineal pouch/space, which contains a layer of skeletal muscle & various neurovascular elements
Perineal body
An ill-defined but important connective tissue structrue into which muscles of pelvic floor & perineum attach
Positioned in the midline along the posterior border of the perineal membrane, to which it attaches
It is also attached to the posterior end of the urogenital hiatus in the levator ani muscles
The deep transverse perineal muscles intersect in the perineal body
In women, the sphincter urethrovaginalis also attaches
Other muscles attaching —
External anal sphincter
Superficial transverse perineal muscles
Bulbospongiosus muscles of perineum
Perineal fascia
Continuity of the abdominal fascia — 2 components —
Deep fascia —
Covers superficial perineal muscles & protruding structures (ex. penis/clit)
Superficial fascia is composed of a further 2 layers —
Superficial layer —
Continuous with Camper’s fascia of anterior abdominal wall
Deep layer (Colle’s fascia) —
Continuous with Scarpa’s fascia of anterior abdominal wall
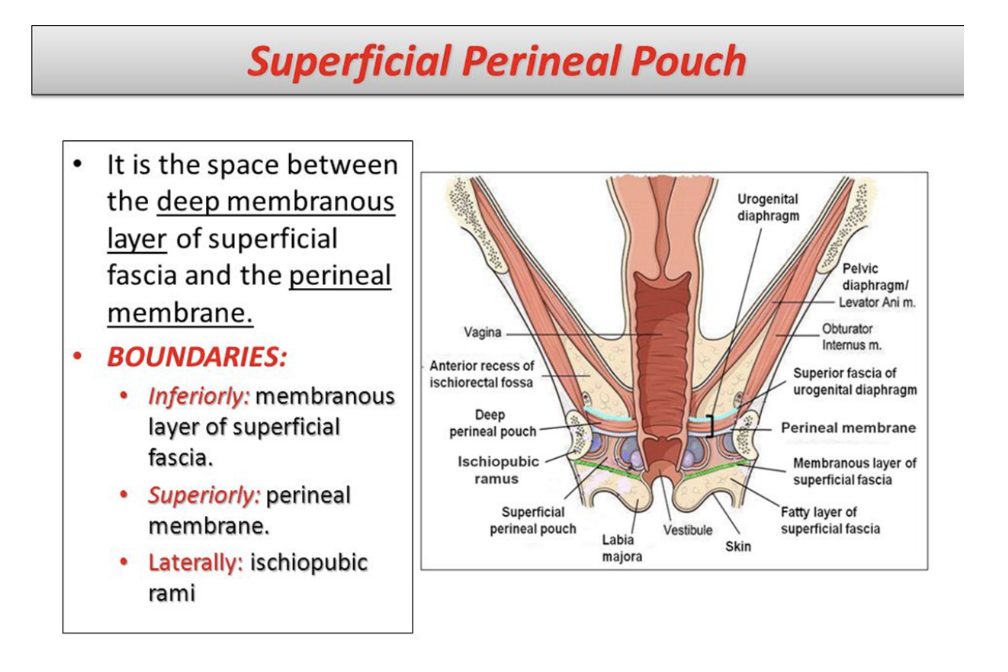
Superficial perineal pouch
Potential space between perineal membrane (superiorly) & the superficial perineal fascia (inferiorly)
Contains erectile tissues forming penis or clitoris, and 3 muscles — ischiocavernosus, bulbospongiosus, & superficial transverse perineal muscles
Also contain the greater vestibular (Bartholin’s) glands
The pouch is bounded posteriorly to the perineal body
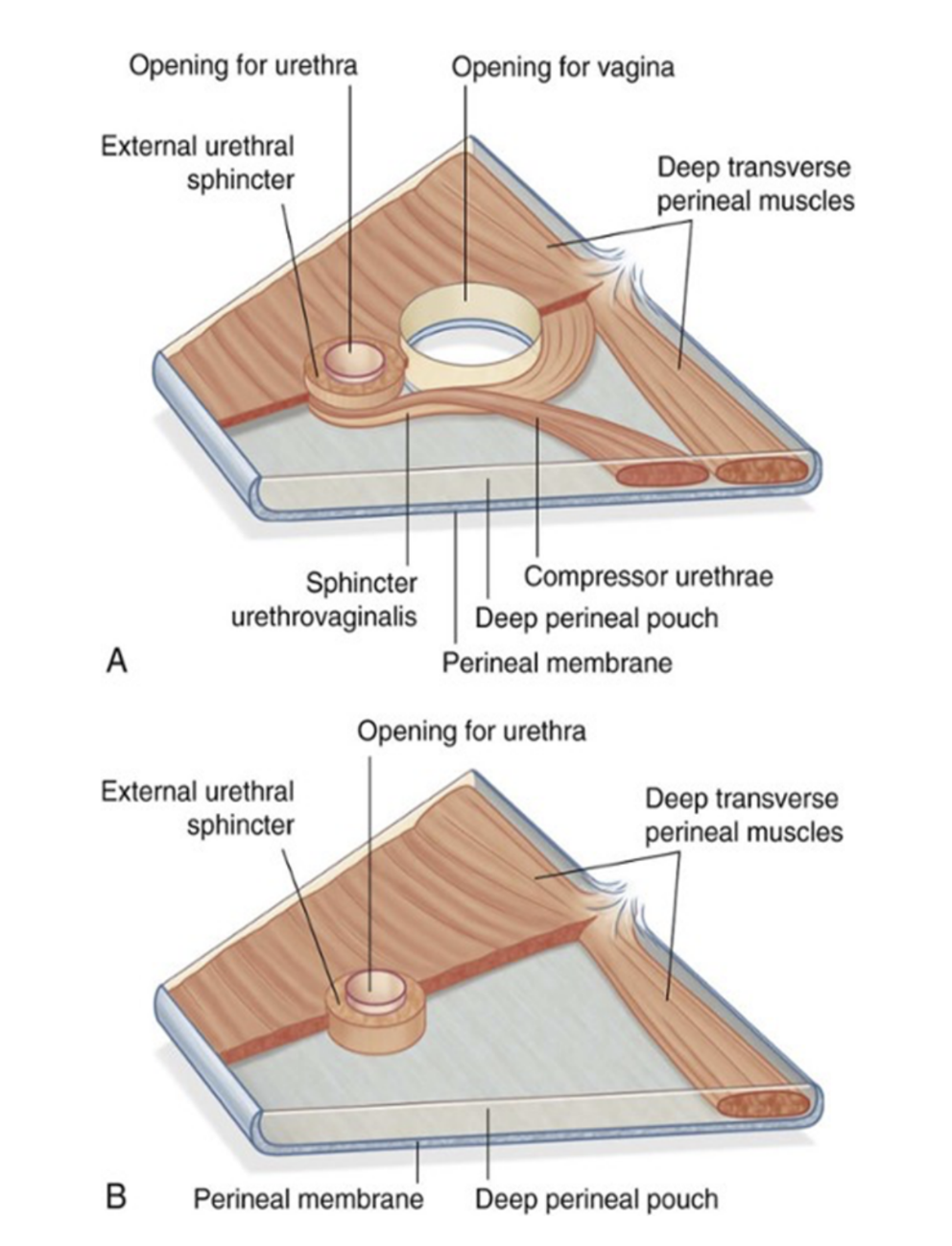
Deep perineal pouch
Potential space between deep fascia of pelvic floor (superiorly) and perineal membrane (inferiorly)
In both sexes, contains —
Part of urethra, centrally
Inferior part of external urethral sphincter muscle, above the center of the perineal membrane, surrounding the urethra
Anterior extensions of ischio-anal fat bodies
In males, contains —
Intermediate part (narrowest) of male urethra
Deep transverse perineal muscles, immediately superior to the perineal membrane (on its superior surface), running transversely along its posterior aspect
Bulbo-urethral glands embedded in the deep perineal musculature
Dorsal neurovascular structures of the penis
In females, contains —
Proximal part of the urethra
Mass of smooth muscle in the place of deep transverse perineal muscles on the posterior edge of the perineal membrane, associated with the perineal body
Dorsal neurovasculature of the clitoris
Muscles of the perineum — overall
External urethral sphincter
Formed in the deep perineal pouch, distal to the internal urethral sphincter
Its skeletal muscle fibers arise from the ischial rami, inferior pubic rami, & adjacent fasica, extending to surround the middle-lower membranous part of the urethra
In men its circular muscle fibers surround the intermediate/membranous part of male urethra, forming an annular sphincter
Has same structure in both sexes — skeletal muscle under voluntary control — however, in males the external sphincteric mechanism is quite complex, as it correlates with fibers of the rectourethralis & levator ani muscles
Origin — inferior ramus of pubis on each side & adjacent walls of deep perineal pouch
Insertion. — surrounds membranous part of urethra
Innervation — perineal branches of pudendal nerve (S2-S4)
Function — compresses membranous urethra, relaxes during micturition (urinating)
Compressor urethrea muscle
Only found in women — second part of urogenital sphincter (others are urogenital sphincter proper & urethrovaginalsphincter) — bilateral extension from innermost part
Origin — ischiopubic ramus on each side
Insertion — blends with partner on other side anterior to the urethra
Innervation — perineal branches of pudendal nerve (S2-S4)
Function — accessory sphincter of the urethra
Sphincter urethrovaginalis
Only found in women — broad flat band of fibers passing in a posterior direction to surround both the urethra & vagina as 1 unit — also extending to vestibular bulb
Origin — perineal body
Insertion — passes forward lateral to the vagina to blend with partner on other side, anterior to the urethra
Innervation — perineal branches of pudendal nerve (S2-S4)
Functions — accesory sphincter of urethra (may also facilitate closing of vagina)
Deep transverse perineal muscle
Found in both sexes, parallels free margin of perineal membrane & joins with its partner at the midline
Thought to stabilize the position of the perineal body (midlinje structure along posterior edge of perineal membrane)
Origin — medial aspect of ischial ramus
Insertion — perineal body
Innervation — perineal branches of pudendal nerve (S2-S4)
Function — stabilizes position of perineal body
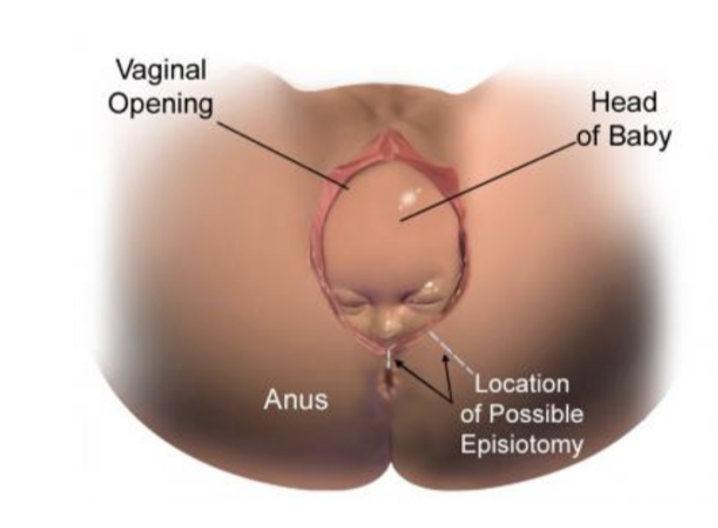
Clinical drop — episiotomy
During childbirth, the perineal body may be stretched & torn — traditionally felt that if a perineal tear is liekly, the obstetrician may proceed with an episiotomy
Procedure in which an incision is made in the perineal body to allow the head of the fetus to pass through the vagina
2 types —
Median episiotomy — cuts through perineal body
Mediolateral episiotomy — incision 45° from midline
Maternal benefits of this procedure are thought to be less traumatic to the perineum, and to result in a decreased pelvic floor dysfunction after childbirth
HOWEVER, recent evidence suggests that an episiotomy should not be performed routinely — review of data has failed to show a decrease in pelvic floor damage with routine use of episiotomies