Operative - Written Exam 3 (W/O Liners and Bases Lecture - separate quizlet)
1/125
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
126 Terms
why is adhesion important in dentistry
? (6)
• Enables more conservative tooth preparations
• Reduces the need for macromechanical retention
• Minimizes the removal of unsupported enamel compared to amalgam preparations
• Seals the tooth-restoration interface, reducing microleakage
• Prevents recurrent caries by limiting bacterial penetration
• Allows bonding of indirect restorations, posts, orthodontic brackets, and other appliances
what happens when adhesion fails? (5)
• Marginal gaps may form, leading to microleakage and post-operative sensitivity
• Increased risk of recurrent caries
• Loss of restoration retention
• Compromised esthetics due to staining at restoration margins
• Potential fracture or debonding of indirect restorations or bonded posts
How do we reduce adhesion failures?
• Maintain strict moisture control (rubber dam isolation). Avoid contamination (saliva, blood, or water)during the bonding procedure
• Proper technique (etching time, application steps, curing time)
• Ensure proper light-curing (adequate intensity, correct distance and angle, appropriate time)
• Select materials appropriate for the clinical situation and understand their properties, indications,and limitations
the following is the definition of...
attraction force when the molecules are of the same kind
cohesion
the following is the definition of...
attraction force between different molecules
adhesion
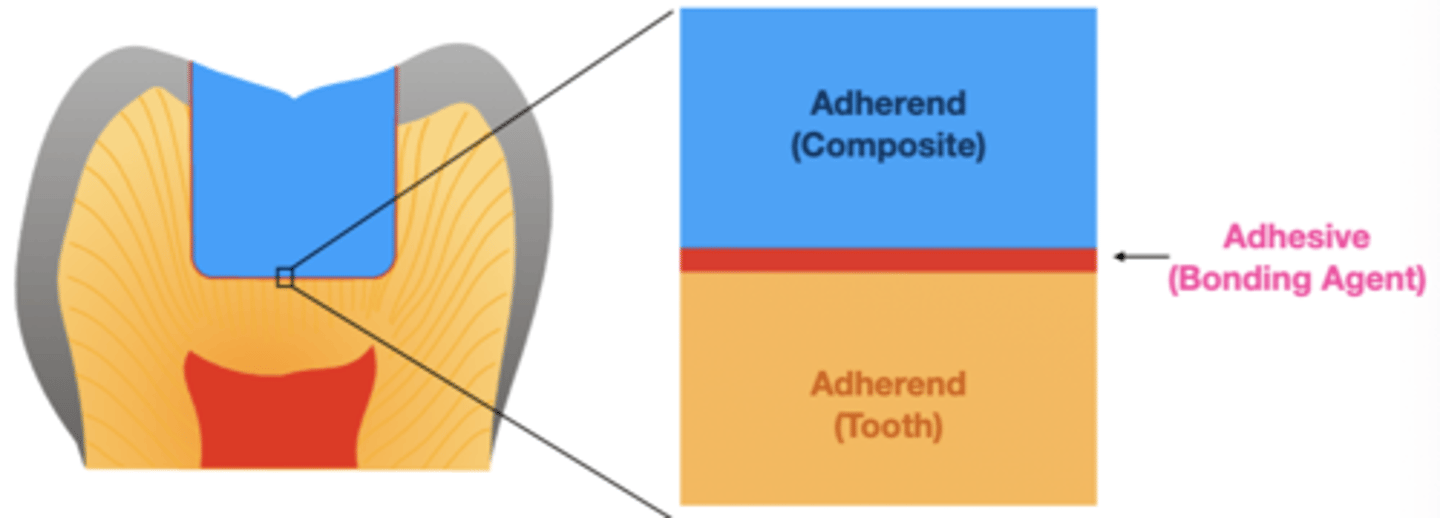
The material that is used to cause adhesion or bonding is known as the...
adhesive
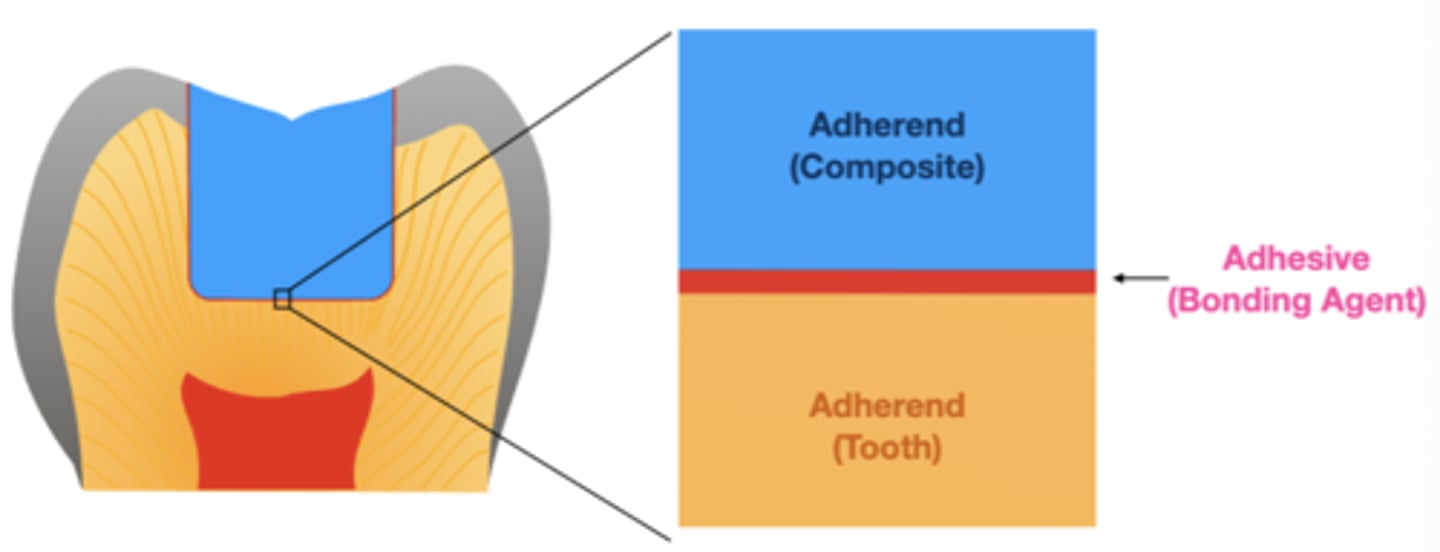
the material to which the adhesive is applied is called the...
adherend
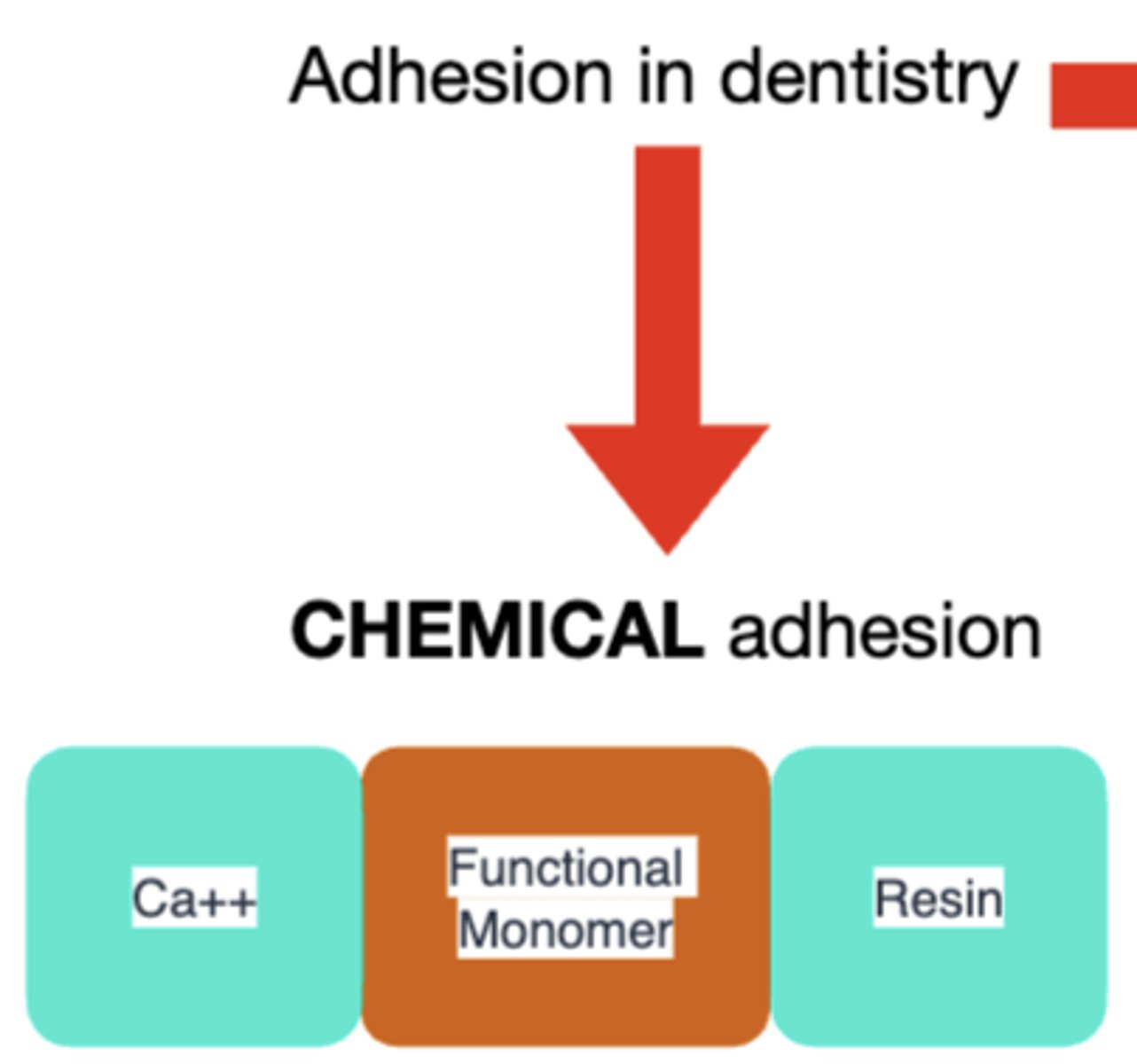
special monomers containing functional groups (e.g., 10-MDP), such as phosphate or carboxyl groups, that interact with calcium and phosphate ions on the tooth surface to create chemical bonds is known as...
chemical adhesion
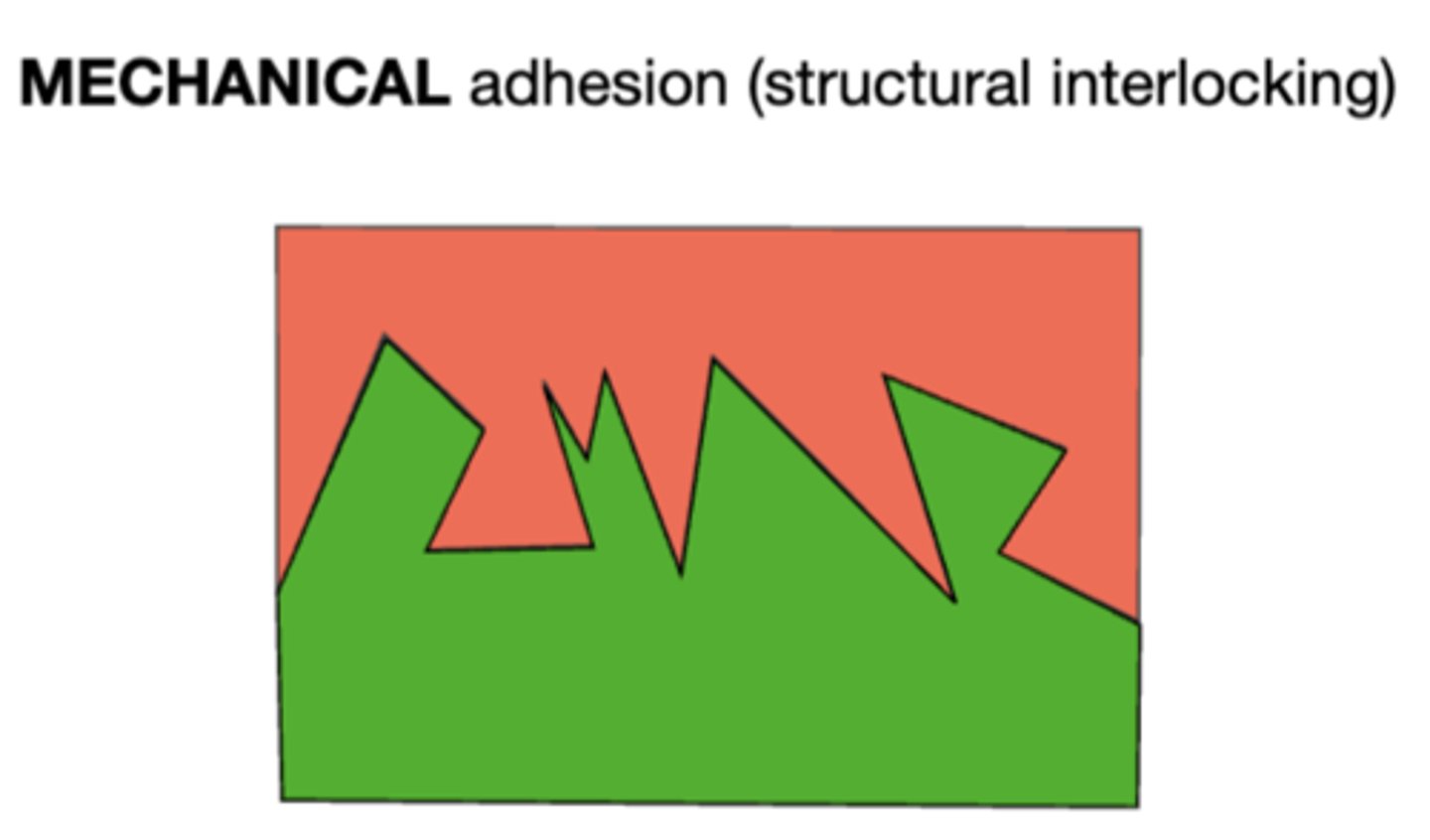
structural interlocking is known as what type of adhesion...
mechanical adhesion
what are the 3 kinds of adhesions in dentistry?
chemical
mechanical
combination of both of the above
a dental bonding system serves 3 key purposes:
1. Resistance to separation: ensures the substrate (enamel, dentin) stays securely attached to the restorative material.
2. Distributes stress across the bonded surfaces.
3. Seals the interface to enhance resistance to microleakage, reducing the likelihood of postoperative sensitivity, marginal staining, and secondary caries
what is meant by wettability?
The bonding must form intimate contact with the surface
compare the composition between bonding agents and composite resin
bonding agent:
- less filler, more solvent
composite resin:
- more filler, no solvent
compare the viscosity between bonding agents and composite resin
bonding agents:
- low viscosity
composite resin:
- high viscosity
general composition of bonding agents:
- Monomers
- Solvents
- Initiators
- Inhibitors
- Fillers
what are monors commonly found in bonding agents?
- BIS-GMA
- HEMA
- MDP
- 4-META
function of bonding agents:
form polymers that create mechanical and chemical adhesion
what are solvents commonly found in bonding agents?
- ethanol
- acetone
- water
function of solvents
◦ Dilutes monomers, initiators, inhibitors, and fillers for an even distribution.
◦ Facilitate the infiltration of monomers into the tooth structure.
◦ Assist in the removal of water
what are initiators commonly found in bonding agents?
- Camphorquinone
- TPO-Lucirin
function of initiators
trigger the polymerization reaction
what are fillers commonly found in bonding agents?
- Silica particles
- zirconia
function of fillers
◦ Reinforce the adhesive and improve its mechanical properties.
◦ Adjust viscosity
what is a thin film of debris formed on the surface of dental hard tissues (enamel or dentin) as a result of cutting or preparing the tooth with hand or rotary instruments?
smear layer
what is the smear layer composed of?
a mixture of organic and inorganic particles—such as denatured collagen and hydroxyapatite
T or F: the smear layer is restricted to the outer layer of enamel
FALSE
- and may extend into the dentinal tubules as smear plugs.
what are the the percentages of each material that makes up the enamel?
- 88% mineral
- 10% water
- 2% organic
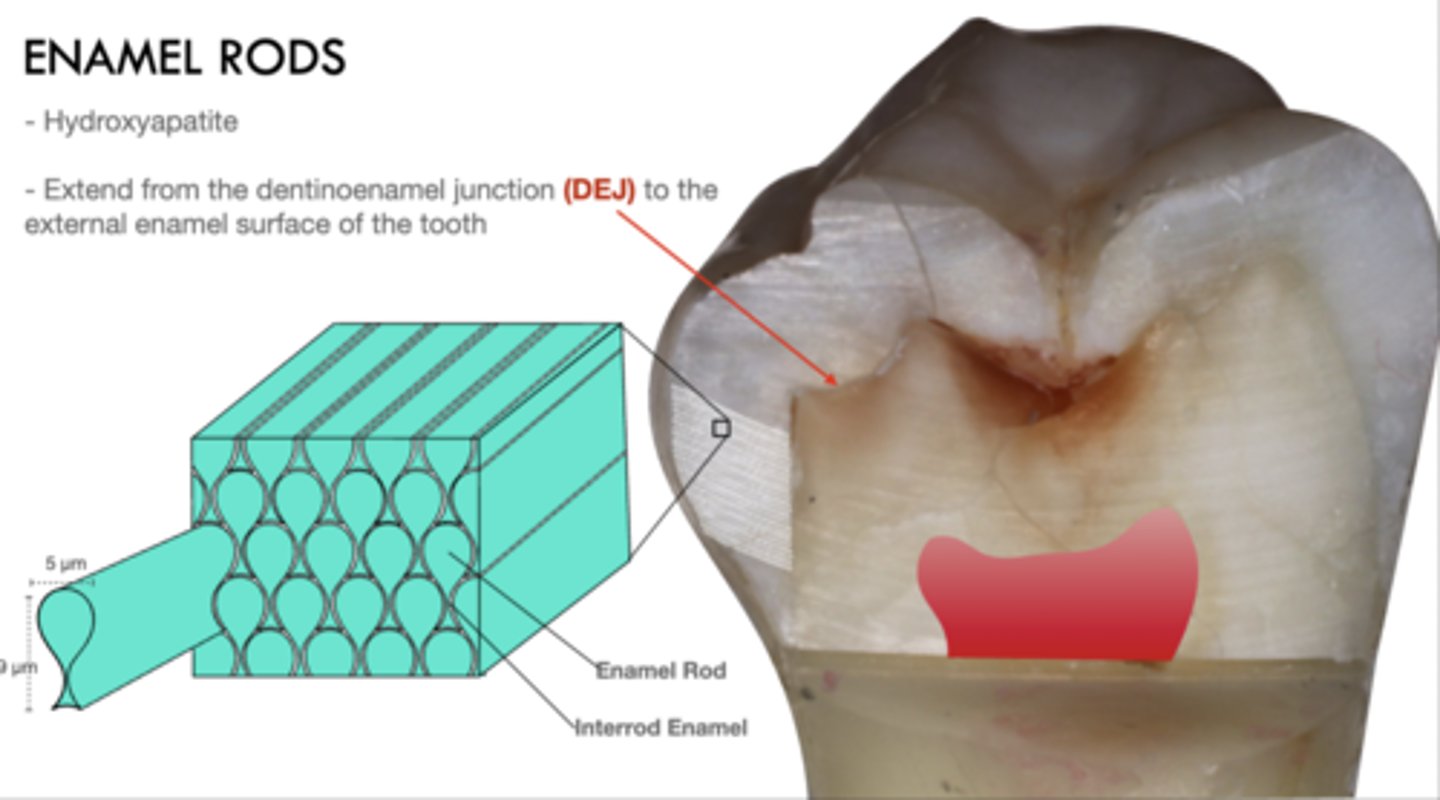
enamel rods are composed of?
hydroxyapatite
enamel rods extend from where to where?
Extend from the dentinoenamel junction (DEJ) to the external enamel surface of the tooth
when and by who was enamel etching introduced?
Buonocore in 1955
when using scotchbond universal plus, what is the etching time?
15 seconds
generally what is enamel etching time?
15-30 seconds
enamel etching is made of...
phosphoric acid (35-37%)
rinsing time after acid etching:
10-15 seconds
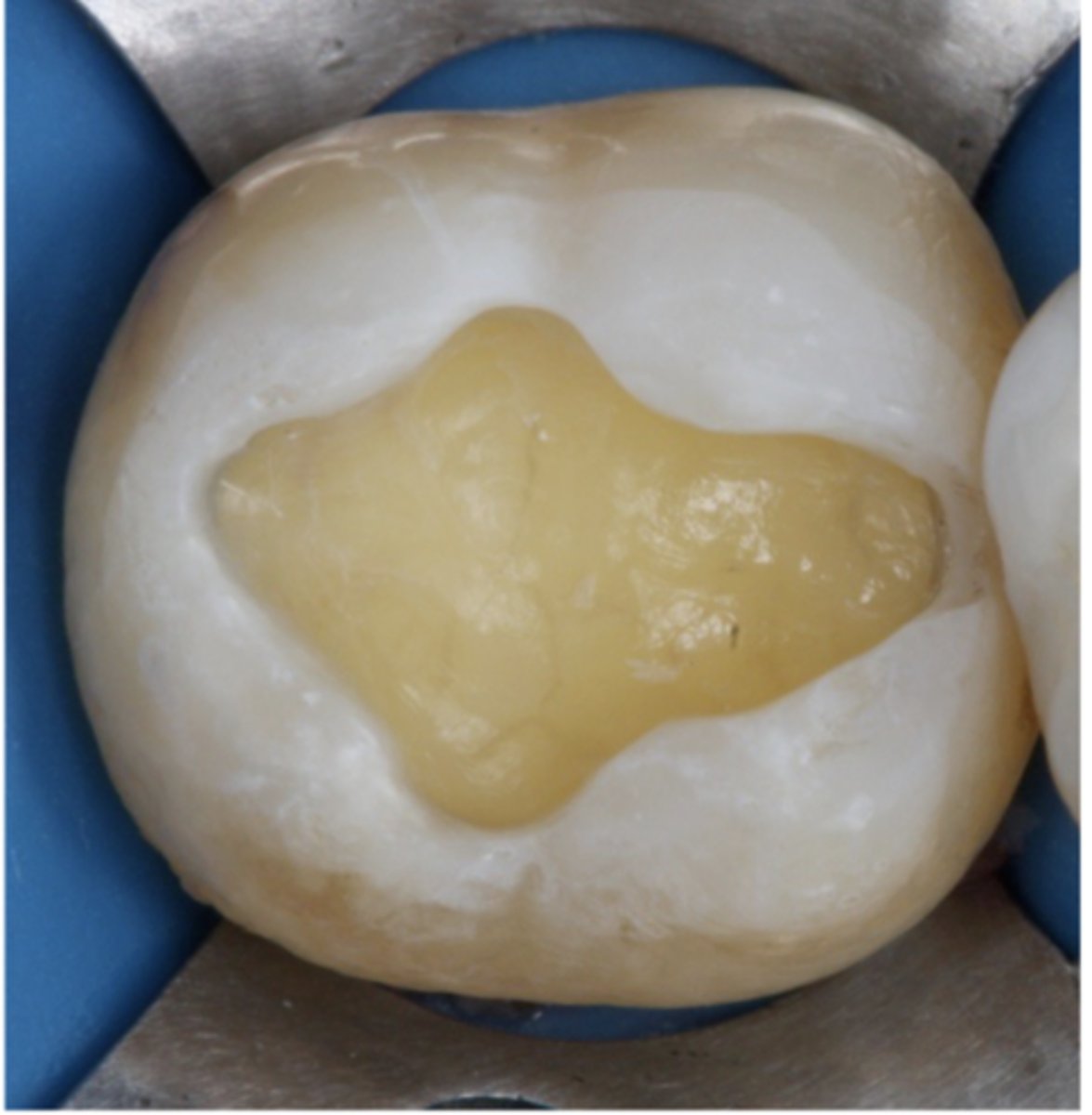
What visual sign indicates that enamel has been properly etched?
Properly etched enamel will appear frosty or chalky white when air-dried
the following is a description of what process?
transforms the smooth enamel into an irregular surface and increases its surface-free energy.
acid etching
When the bonding agent is applied to the irregular etched surface, what does it do?
it penetrates into the surface, aided by capillary action
what is the fundamental mechanism of adhesion on enamel?
formation of resin MICROTAGS
material becomes interlocked with the enamel surface when...?
monomers in the material polymerize
describe the composition of dentin
50% - mineral
25% organic
25% water
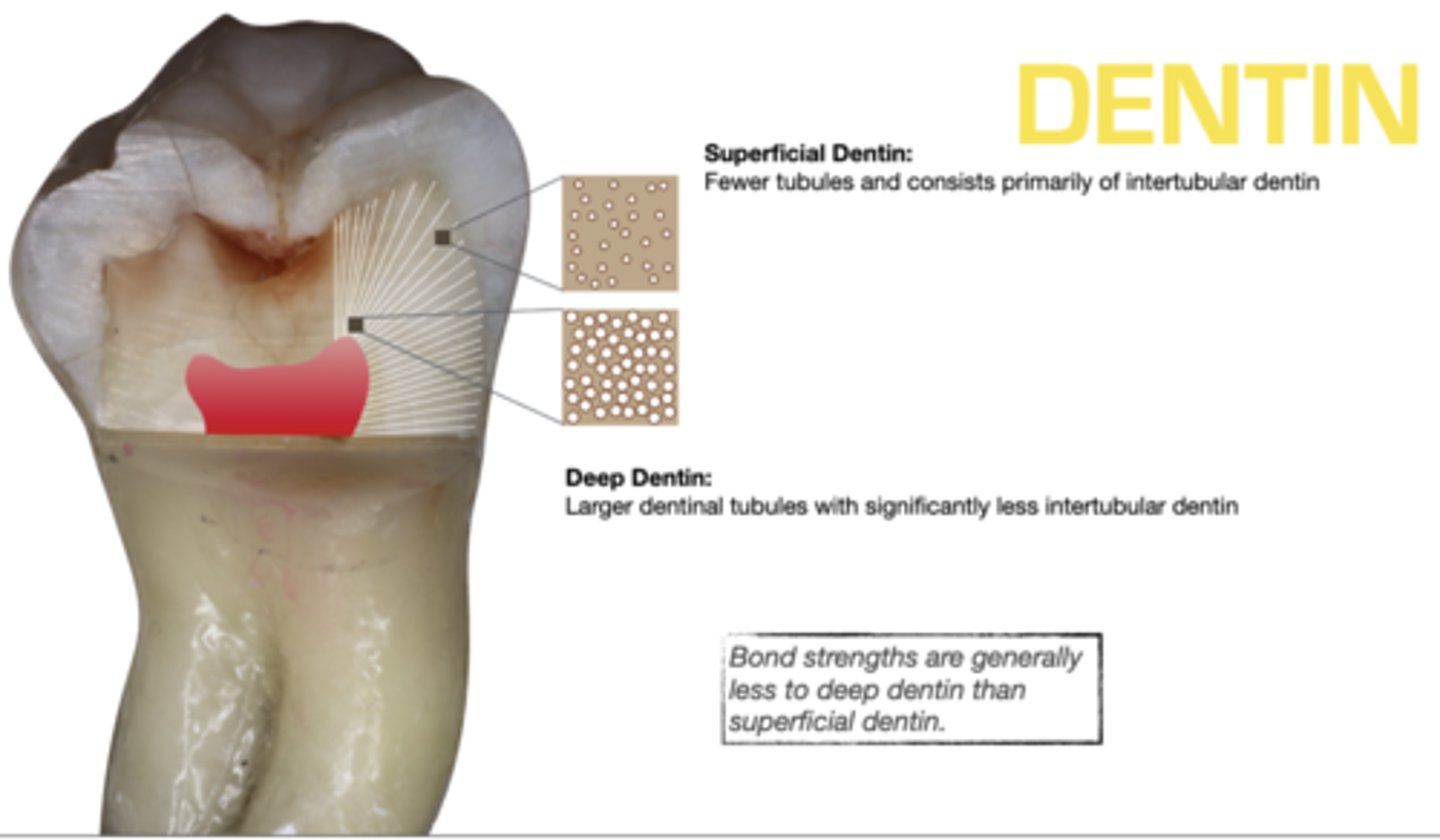
compare bond strengths between deep dentin and superficial dentin
Bond strengths are generally less to deep dentin than superficial dentin
compare dentin tubule amounts and intertubular dentin amounts between superficial and deep dentin
superficial:
- fewer tubules, primarily intertubular dentin
deep:
- larger dentinal tubules, significantly less intertubular dentin
"total-etch" was introduced by who and in what year?
Fusayama in 1979
- phosphoric acid (35-37%), dentin etch time (15 sec.), and rinse time (10-15 sec) are all the same as standard protocol for etching
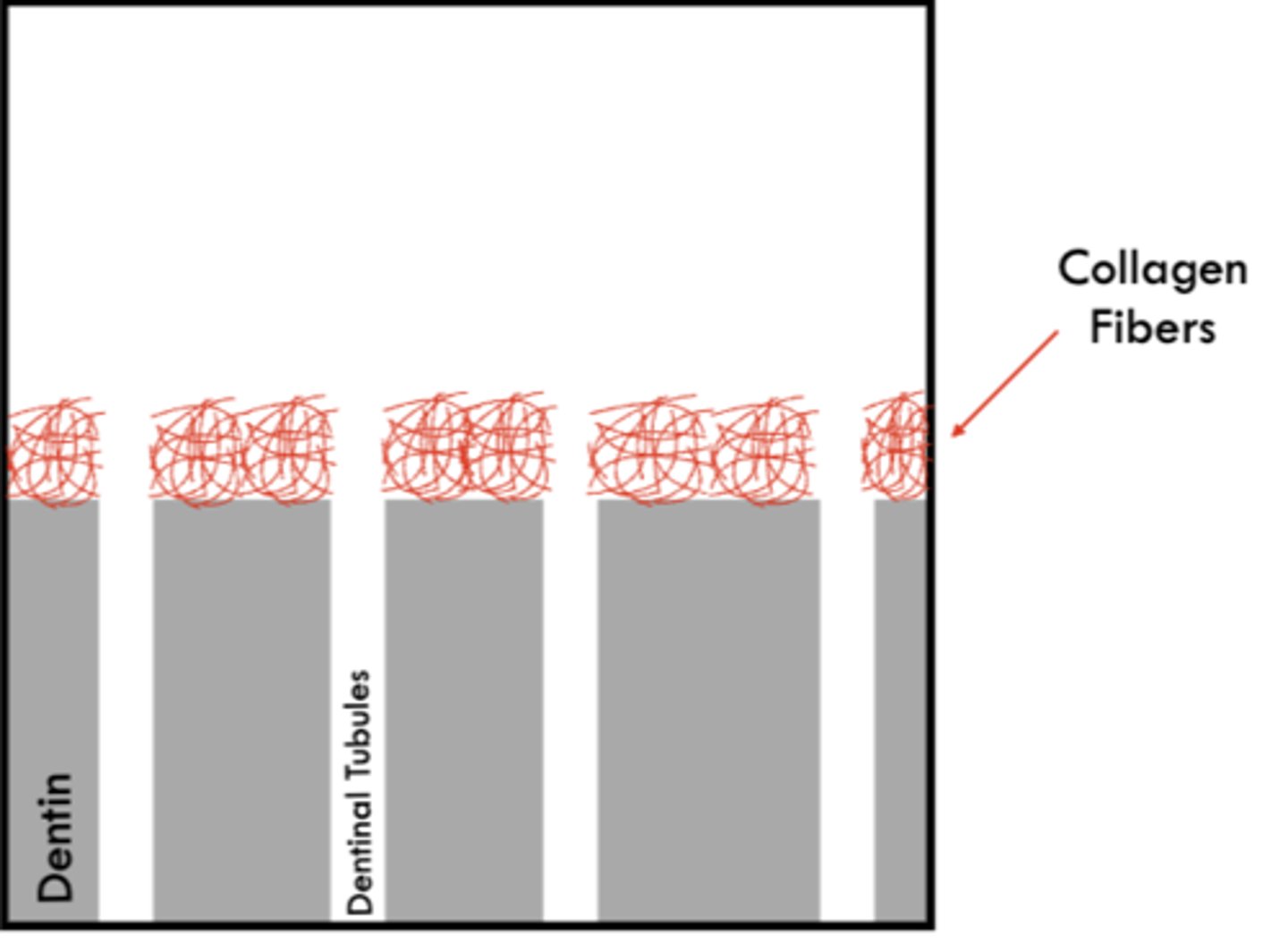
what does dentin etching do?
• Removes the smear layer and opens the dentinal tubules
• Partially demineralizes the dentin, exposing collagen fibrils
• Increases surface energy and porosity, allowing adhesive infiltration
• Creates a substrate for micromechanical retention via formation of the hybrid layer
• Requires careful moisture control to maintain the ideal moist dentin state for bonding
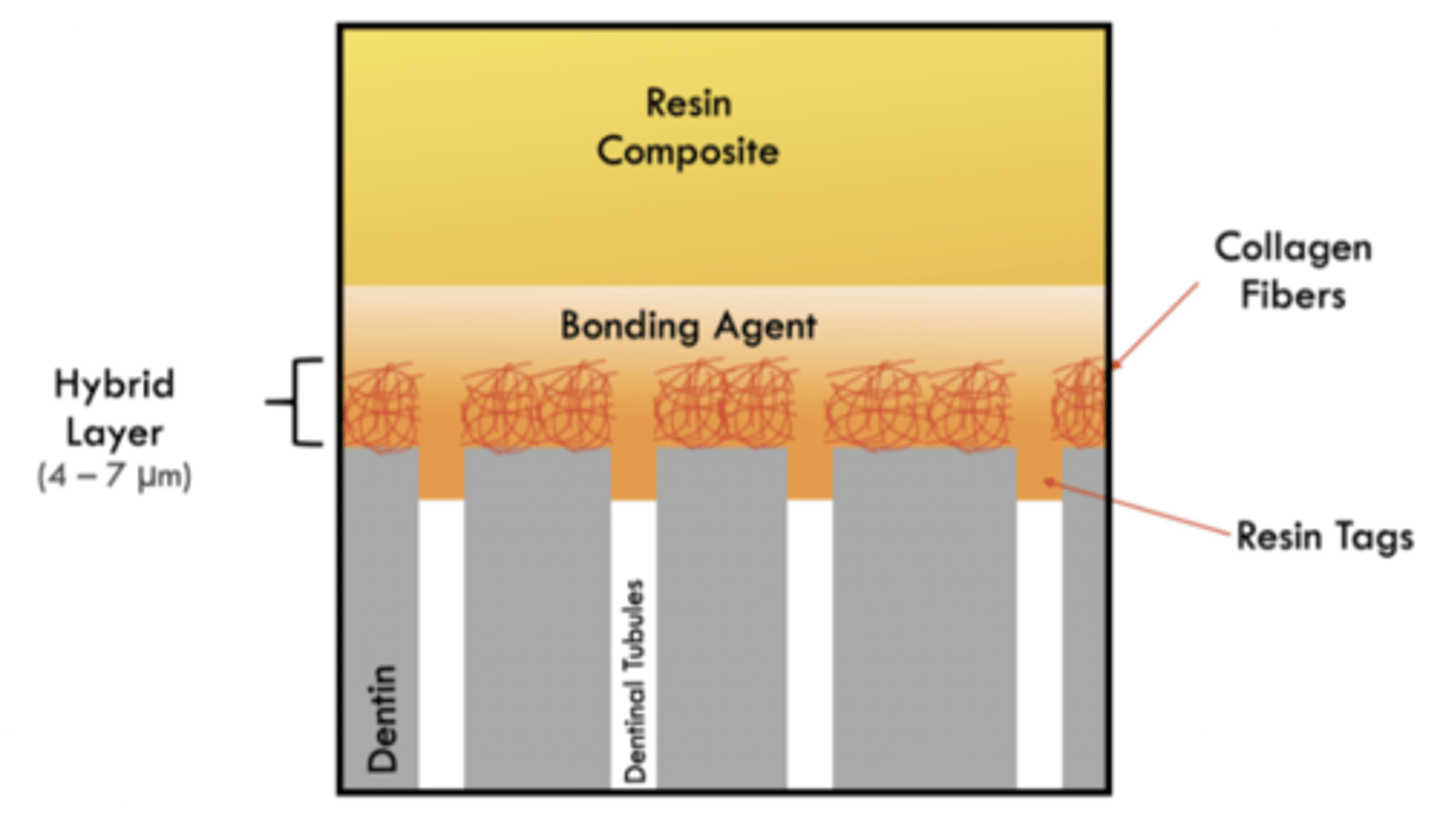
An intermediate layer of resin, collagen, and dentin that is produced by acid etching of dentin and infiltration of resin into the conditioned dentin describes what?
hybrid layer
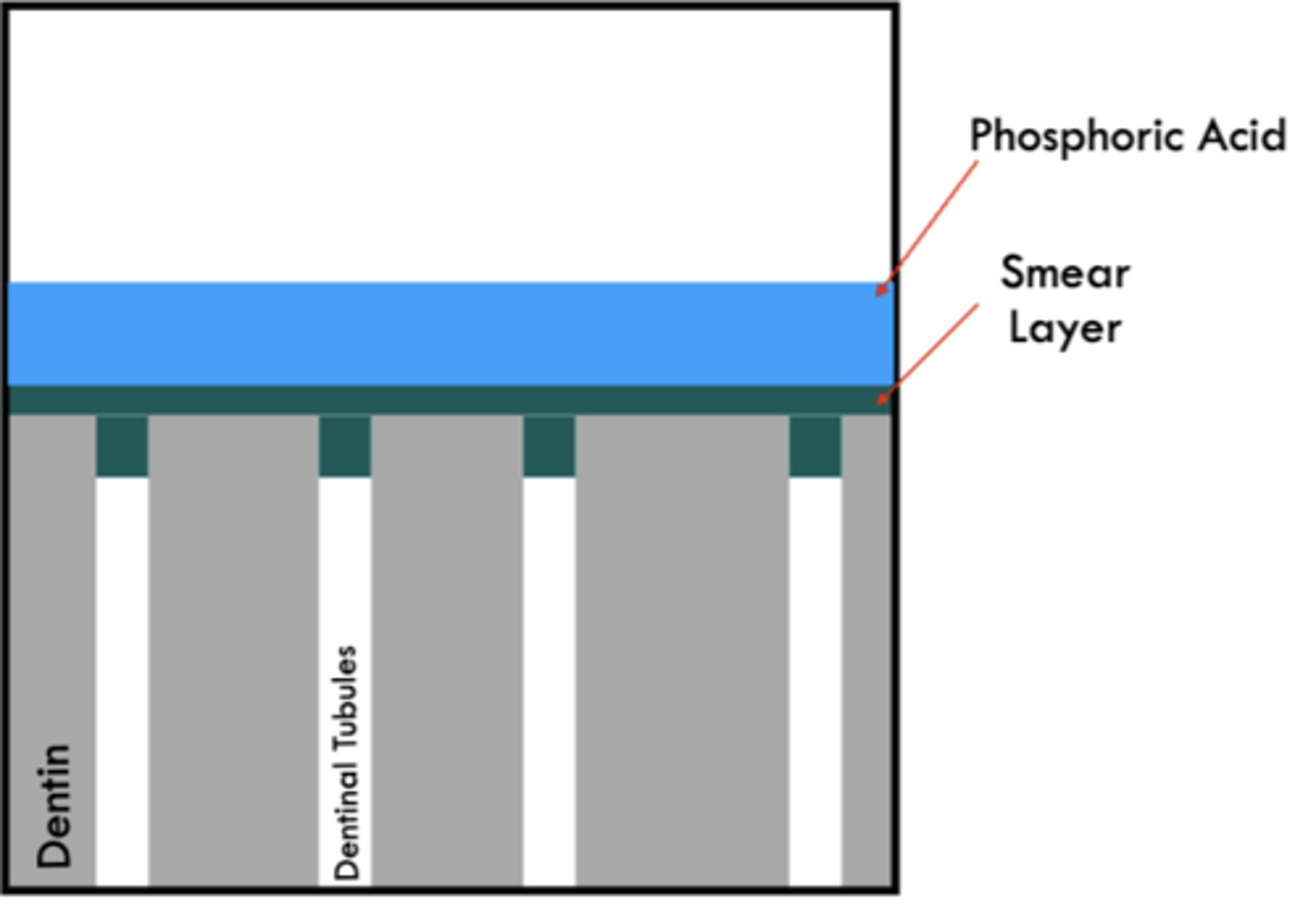
goals of phosphoric acid:
• Removes the smear layer and opens the dentinal tubules
• Partially demineralizes the intertubular dentin, exposing collagen fibrils
Which one is more reliable:
dentin adhesion or enamel adhesion?
Enamel
what relies primarily on the penetration of adhesive monomers into the network of collagen fibrils left exposed by acid etching?
dental adhesion
why is dental adhesion more challenging than enamel adhesion?
due to the following characteristics of dentin:
• Less mineralized
• Complex structure
• Intrinsically hydrated
between enamel adhesion and dentin adhesion, which is more challenging?
dentin adhesion
what is the main goal of the etch-and-rinse adhesion strategy?
to remove the smear layer
what is the main goal of the self-etch adhesion strategy?
transform the smear layer
compare the goals of each adhesion strategy:
- self-etch
- etch-and-rinse
- self-etch: transform smear layer
- etch-and-rinse: remove smear layer
what steps do you perform in the self-etch adhesion strategy?
- NO etching of the dentin with phosphoric acid
- NO removal of the smear layer
- smear layer is modified and incorporated into the adhesive surface
- selectively enamel with phosphoric acid to improve bonding enamel
what is unique to the self-etch adhesion strategy?
the smear layer is NOT removed (with etch), instead smear layer is modified and incorporated into the adhesive surface and the enamel is selectively etched
between the etch-and-rinse and self-etch adhesion strategies, which is more technique sensitive?
the etch-and-rinse
- risk of over-etching, which can be detrimental to bond strength and increases the likelihood of post-operative sensitivity
what is a risk of using the etch-and-rinse adhesion strategy?
risk of over-etching, which can be detrimental to bond strength and increases the likelihood of post-operative sensitivity
T or F: enamel etching is not recommended in the self-etch adhesion strategy
FALSE
- Selective Enamel Etching is recommended. (Self-etch systems do not etch enamel as well as phosphoric acid)
what type of bonding can be used in both the etch-and-rinse and self-etch adhesion strategies?
universal bonding agent
is universal bonding agent performance dependent on the degree of dentin moisture?
NO it is independent
why are universal bonding agents rubbed? (2)
- enhances penetration of the adhesive
- improves solvent evaporation
why is solvent evaporation important?
• It is essential to remove water and/or solvents (e.g., ethanol, acetone) from the adhesive layer
• Incomplete evaporation can dilute the adhesive and interfere with polymerization
• Solvent retention may lead to decreased bond strength and increased nanoleakage
use gentle air-drying for at least 5-10 seconds or high-speed suction
what is a tooth-colored restorative material available in various shades and translucencies to mimic the natural appearance of tooth structure?
composite resin
what is composed of a resin matrix, inorganic filler particles, and a coupling agent (silane) that chemically binds the fillers to the resin?
composite resin
Composite resins hardens through what method, which is typically initiated by light (light-cure), chemicals (self-cure), or a combination of both (dual-cure) systems.?
polymerization reaction
what are the components of composite resin?
resin matrix, inorganic filler, coupling agent (silane), pigments, polymerization initiators
the following is a function of what component of composite resin?
Organic phase (e.g., Bis-GMA, UDMA, TEGDMA) thatforms the plastic network after curing.
resin matrix
the following is a function of what component of composite resin?
Glass, Silica, zirconia, or prepolymerized particles that improve strength, wear resistance, and reduce shrinkage. Reduce water sorption; control of viscosity;provide radiopacity. Typically ~75% by weight
inorganic fillers
the following is a function of what component of composite resin?
Bond chemically the fillers to the resin matrix, ensuring structural integrity
coupling agent (silane)
the following is a function of what component of composite resin?
Usually Camphorquinone. Absorbs blue light to start polymerization.
initiator
how are composite resins classified?
By Viscosity and Handling
By Placement Technique
By Polymerization Reaction (curing method)
By Filler Particle Size
what are the 3 curing methods?
- Light-Cured
- Self-Cured
- Dual-Cured
what is the most common light curing method in direct restorations?
light-cure with blue light
what light curing methods are used in core build-ups and cementation of indirect restorations?
self-cured
- chemical
- limited working time
dual-cured
- light and chemical
smaller filler particles means what for polishibility and strength?
HIGH polishability
LOW strength
higher filler content means what for polishibility and strength?
GREATER strength
LOW polishability
when are flowable composites indicated? (2)
• 0.5 mm-thick liner under large restorations
• Ultra-conservative class I restorations
compared to conventional composite, does flowable composite experience more or less shrinkage?
more in flowable
compare filler content in flowable and conventional composite
Lower filler content in flowable compared to conventional composites: 35% to 65% by weight
what are some characteristics of bulk-fill composites
• High filler loading for strength and reduced shrinkage
• Higher translucency to allow deeper light penetration
• Lower elastic modulus (not as stiff as conventional composites)
• Special monomers
how is bulk-fill composite is placed
in up to 4-5mm layers
what materials contain functional monomers capable of etching and bonding directly to tooth structure, eliminating the need for separate etching and bonding steps?
self-adhesive composites
what materials release beneficial ions (e.g., fluoride, calcium) to promote tooth remineralization?
Studies are needed to evaluate their long-term performance
bioactive composites
what composites are designed with agents that inhibit bacterial growth (quaternary ammonium compounds, bioactive fillers, or metal ions such as silver or zinc)?
Studies are needed to evaluate their long-term performance
antibacterial composites
what composites use advanced blending technology to match a wide range of tooth shades with one materia
single-shade composites
most modern composites experience how much polymerization shrinkage?
2.4% - 2.8%
if not manages corrected polymerization shrinkage can cause...
gaps, microleakage, cusp deflection, postoperative sensitivity, and increased risk of recurrent caries.
Polymerization shrinkage of composite resin generates what
internal stress
what is the consequence of internal stress generated by polymerization shrinkage?
This stress may concentrate at the adhesive interface, risking gap formation and marginal breakdown, or transmit to the surrounding tooth structure, potentially causing cusp deflection
how to minimize complication due to composite shrinkage:
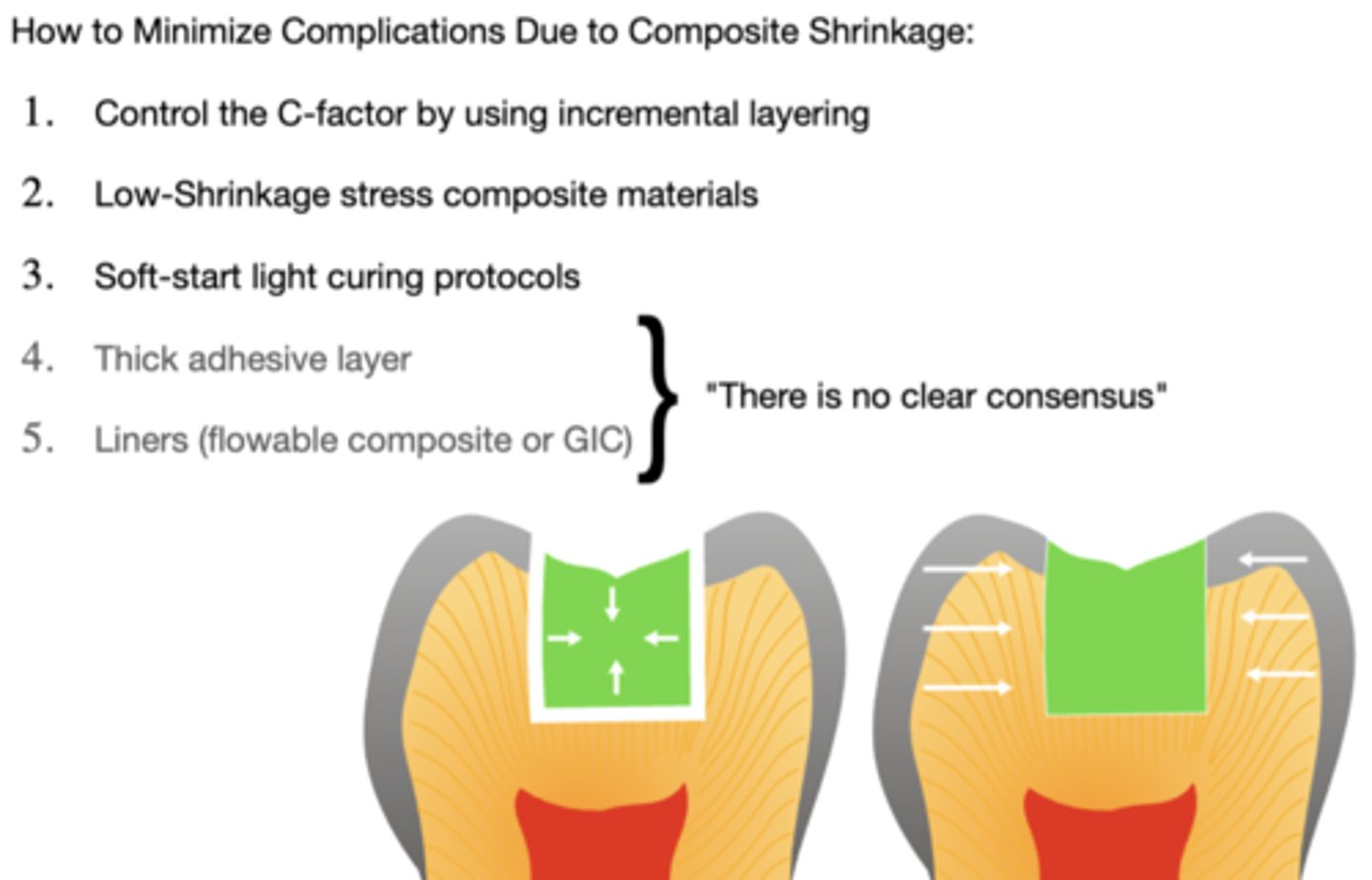
what is the c-factor?
Ratio of bonded to unbonded surfaces
The C-factor relates to the...
configuration of the cavity walls
a high C-factor indicates what?
a greater ratio of bonded surfaces to unbonded (free) surfaces.
why does c-factor matter?
Higher C-factor = More bonded walls = Greater polymerization stress (more restriction during shrinkage)
what is the c-factor of a class 1 cavity?
5 bonded walls, 1 free surface → C-factor = 5:1 (High)
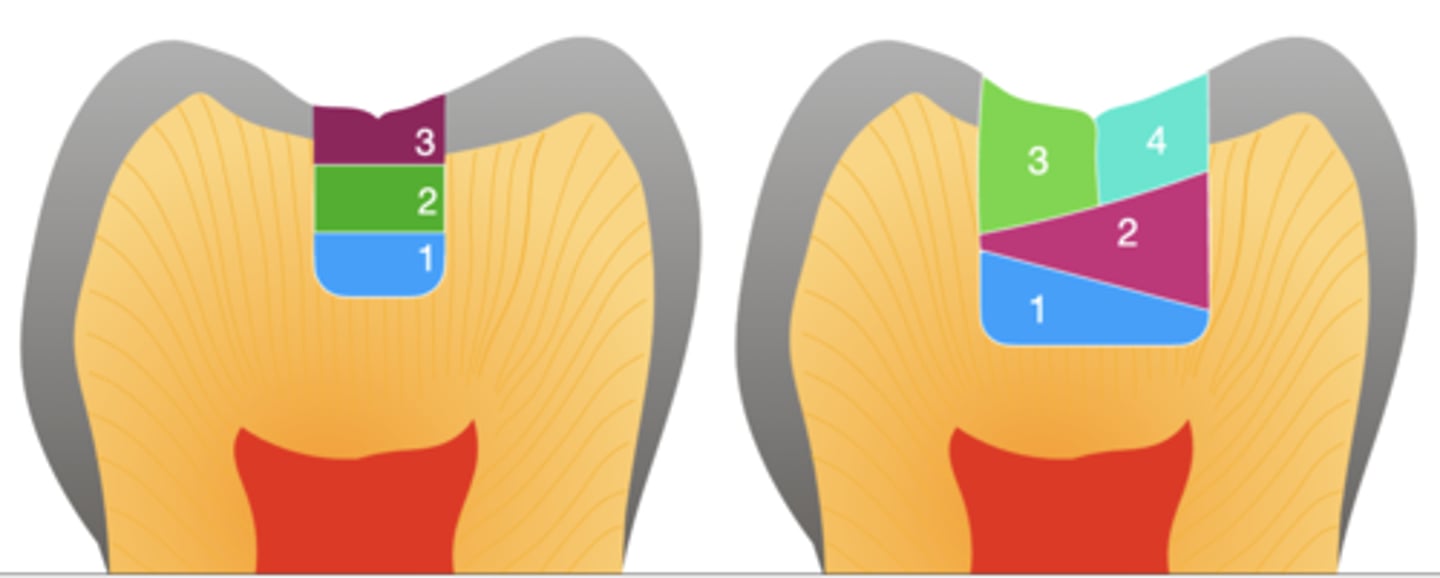
how can c-factor be controled?
incremental layering
- Horizontal layers for small isthmus and oblique layers for larger restorations
how does light curing work on composite?
Photoinitiators in the composite—such as camphorquinone (CQ) and TPO—absorb this light
- When activated, they initiate polymerization, transforming resin monomers into a solid polymer network
most composites use what photo initiator?
camphorquinone (CQ)
Some esthetic or flowable composites may include what photoinitiators for lighter shades?
TPO or PPD
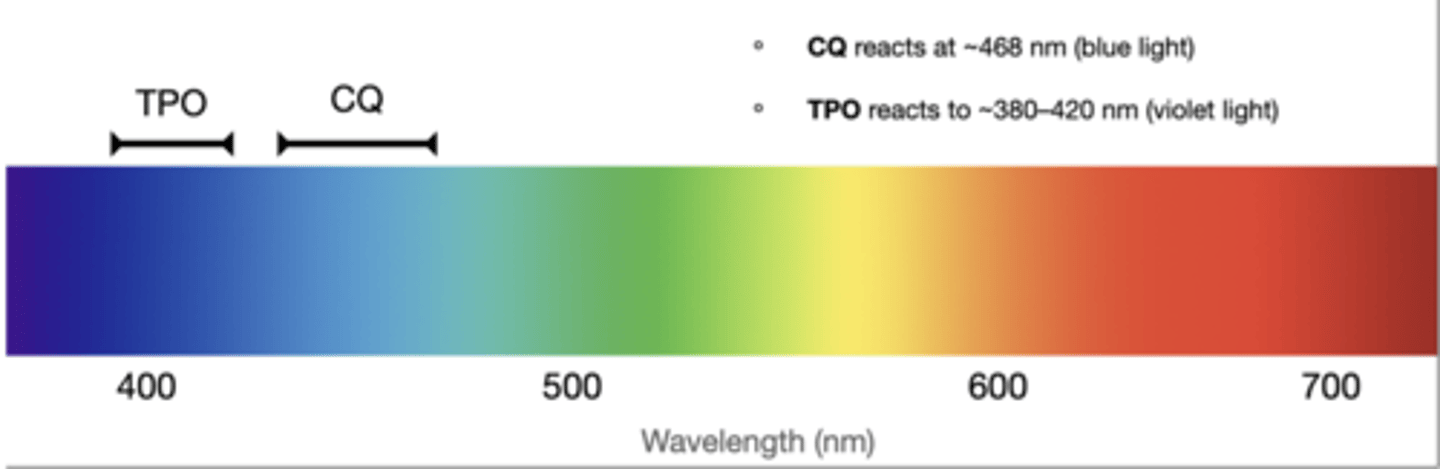
CQ reacts at what wavelength? what about TPO?
CQ - 468 nm (blue light)
TPO - 380-420 (violet)