Spine Disorders
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
19 Terms
What are the potential risk factors for lower back pain?
While general health risk factors like age, male gender, and unhealthy habits like obesity and smoking can contribute to back pain, there are a few less known factors
1) Psychosocial Factors
→ depression, anxiety, childhood abuse
→ causes you to perceive pain as being worse
2) Occupation
→ Physical labor such as repetitive heavy lifting
Does acute back pain often resolve?
Acute lower back pain resolves most of the time in 6-12 weeks with about half resolving in a week
→ however, lower back pain can often recur or become chronic
What Muscle Injuries can cause Back Pain?
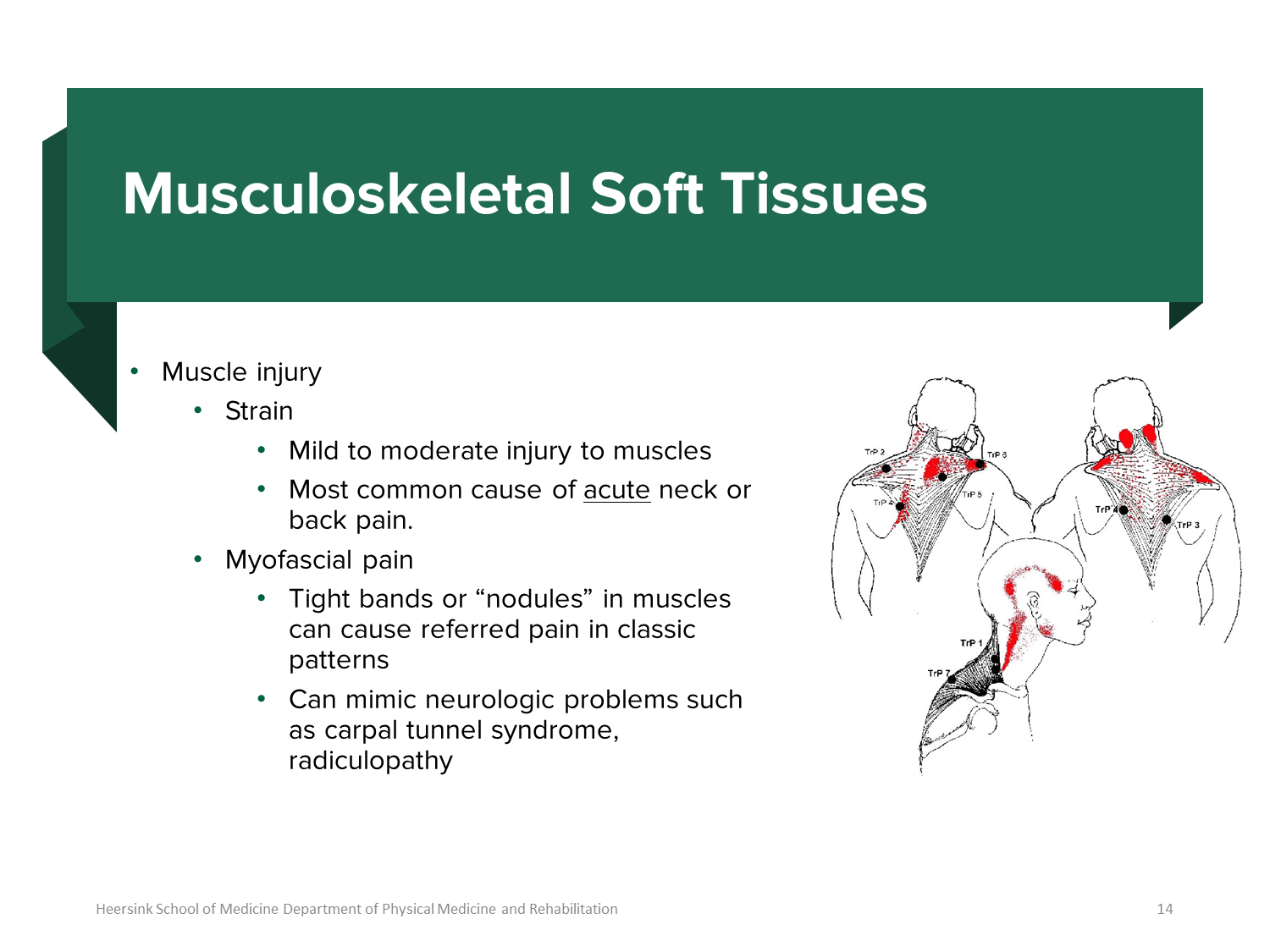
Muscle Injury to the back can be subdivided into strain and myofascial pain.
1) Strain
→ Strain is a mild to moderate injury of the muscles and is the most common cause of acute neck or back pain
2) Myofascial Pain
→ Tight bands or nodules in muscles can cause referred pain in a classic pattern
→ Myofascial pain can mimic neurologic problems like carpal tunnel syndrome or radicular pain
What are lumbar sprains
Ligament Injuries include stretching or tearing a ligament that connects the bones
1) Lumbar Sprain
→ can occur with muscle strain and is often a result of picking heavy things with your back bent
→ Ligament injuries can cause instability in area with joints such as out Sacroiliac joint
What is a cervical sprain or strain?
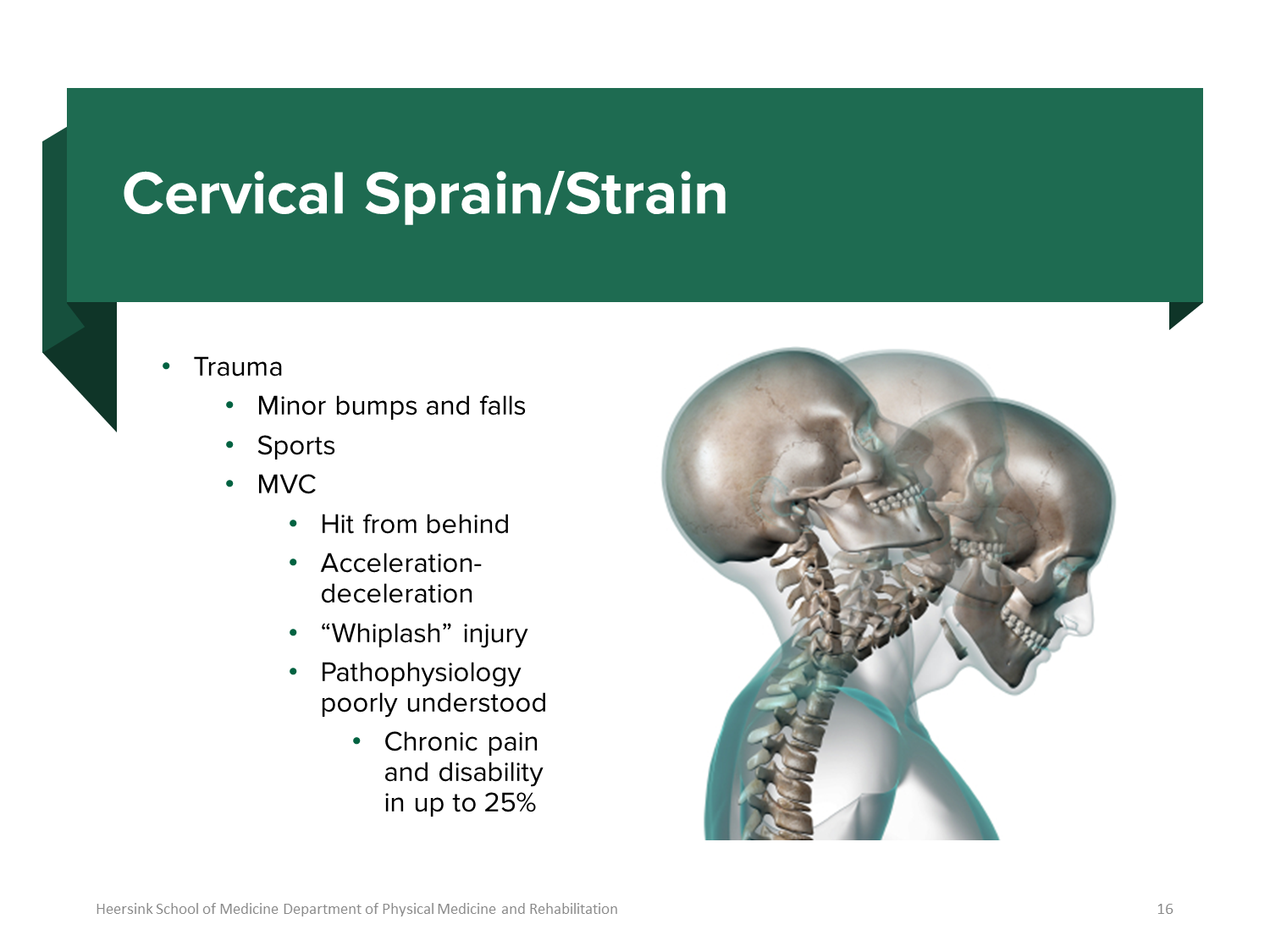
Cervical Sprains and Strains
→ classic whiplash motion that occur in sports, car crashes, or minor bumps/falls
→ pathophysiology is poorly understood and can cause chronic pain and disability in some patients
What are the treatments for muscular causes of back pain?
1) Treatment for back pain associated with muscles and ligaments involves RICE
→ Relative Rest - do not completely rest, but rest less than what you would usually do: stay active
→ Ice
→ Compression
→ Elevation
2) NSAIDs, acetaminophen, or muscle relaxants may also be used
→ Trigger point injections (lidocaine and bupivacaine) injections to the area
3) Acupuncture
4) Physical Therapy
→ the most important part - educated about stretching and ergonomic modification
What are the intervertebral discs?
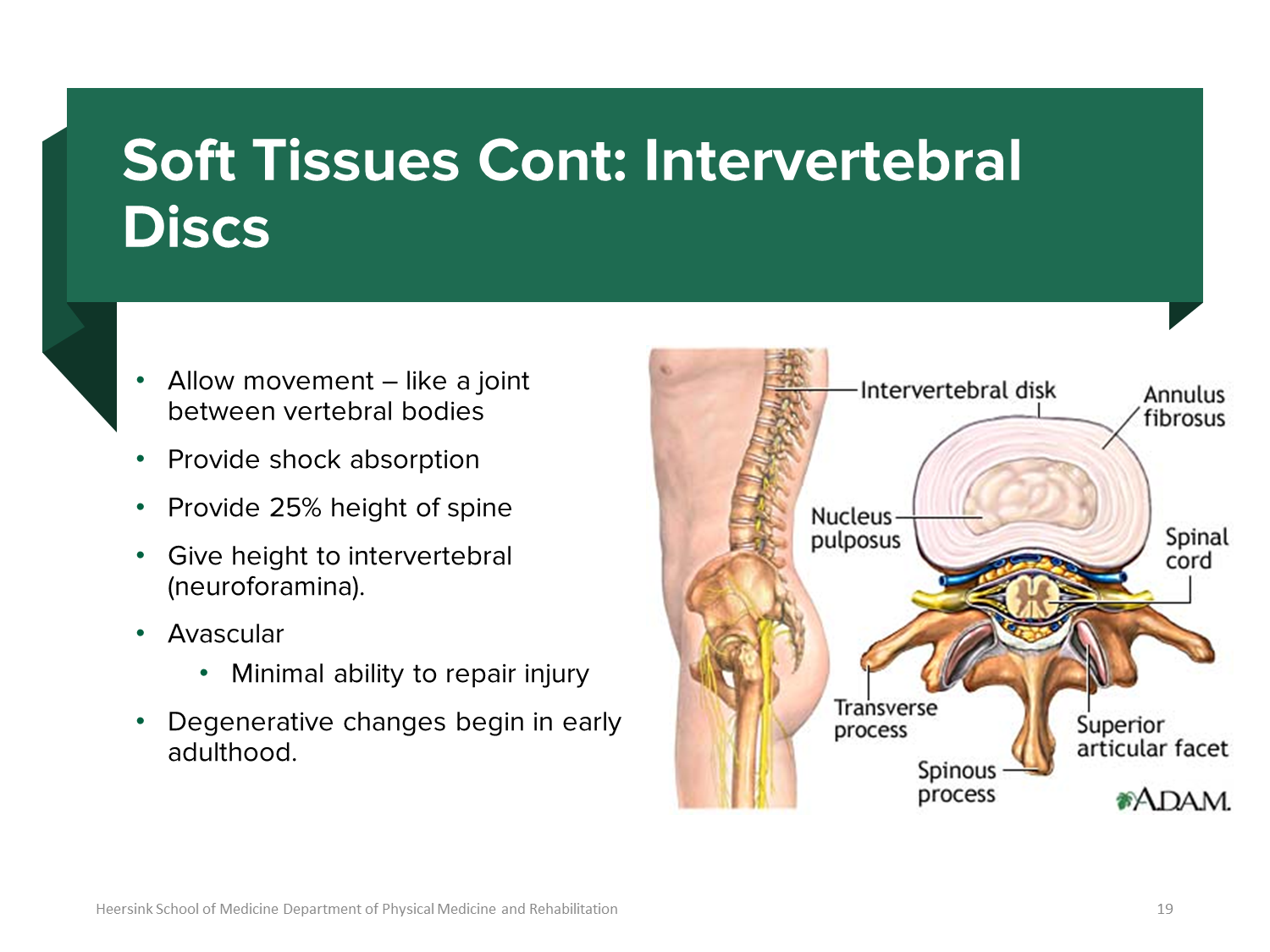
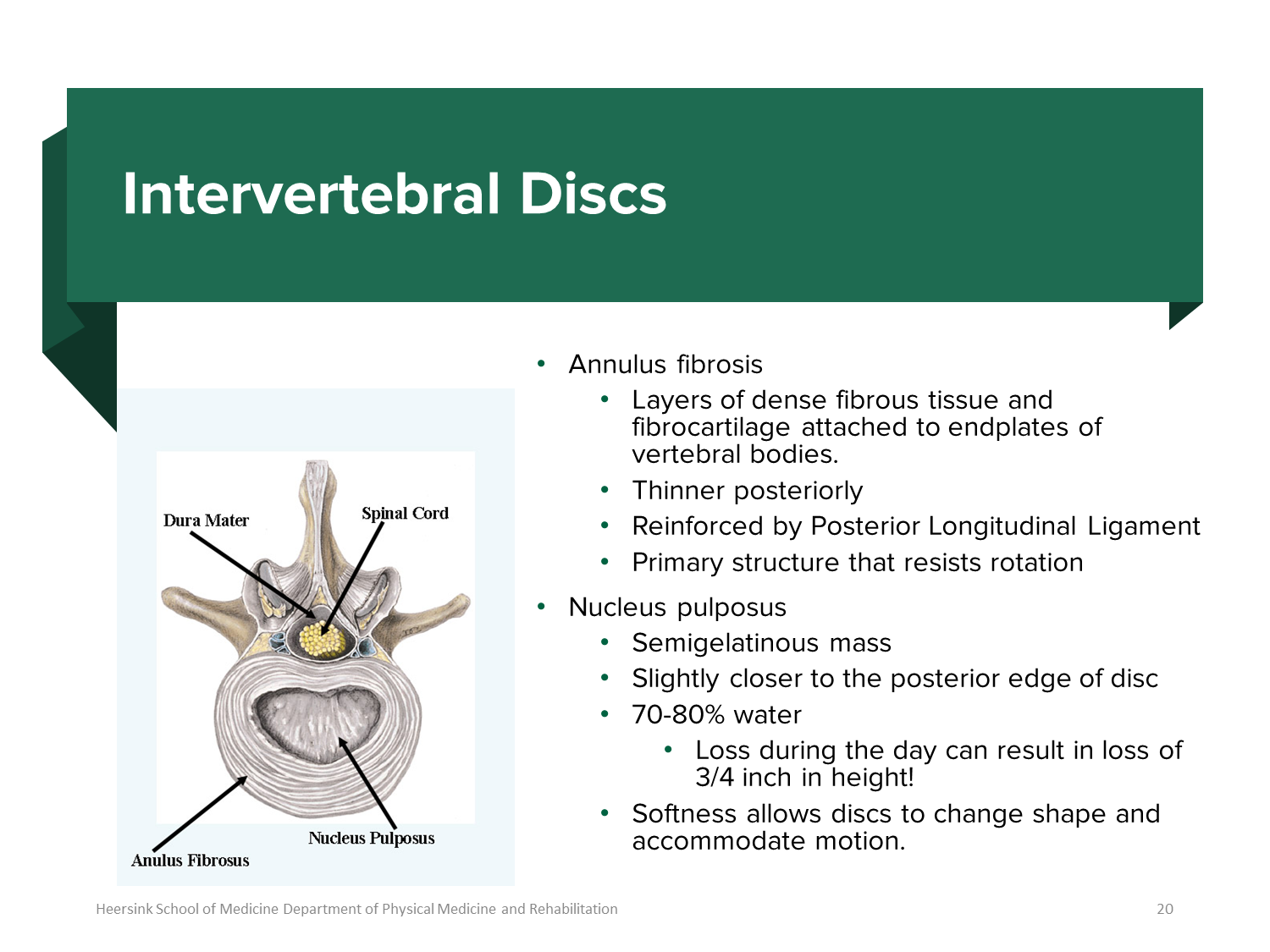
Intervertebral Discs are cushion like pads in between the vertebrae that function as shock absorbers. There are two main parts
1) Annulus Fibrosis
→ layers of dense fibrous tissue and fibrocartilage that surrounds the nucleus pulposus and are used to rest rotation
→ the annulus fibrosus is thinner posteriorly so herniations will typically occur posteriorly into the spinal cord
2) Nucleus Pulposus
→ semigelatinous mass inside the intervertebral disc
→ loss of height occurs during the day due to loss of water
What is Degenerative Disc Diseases?
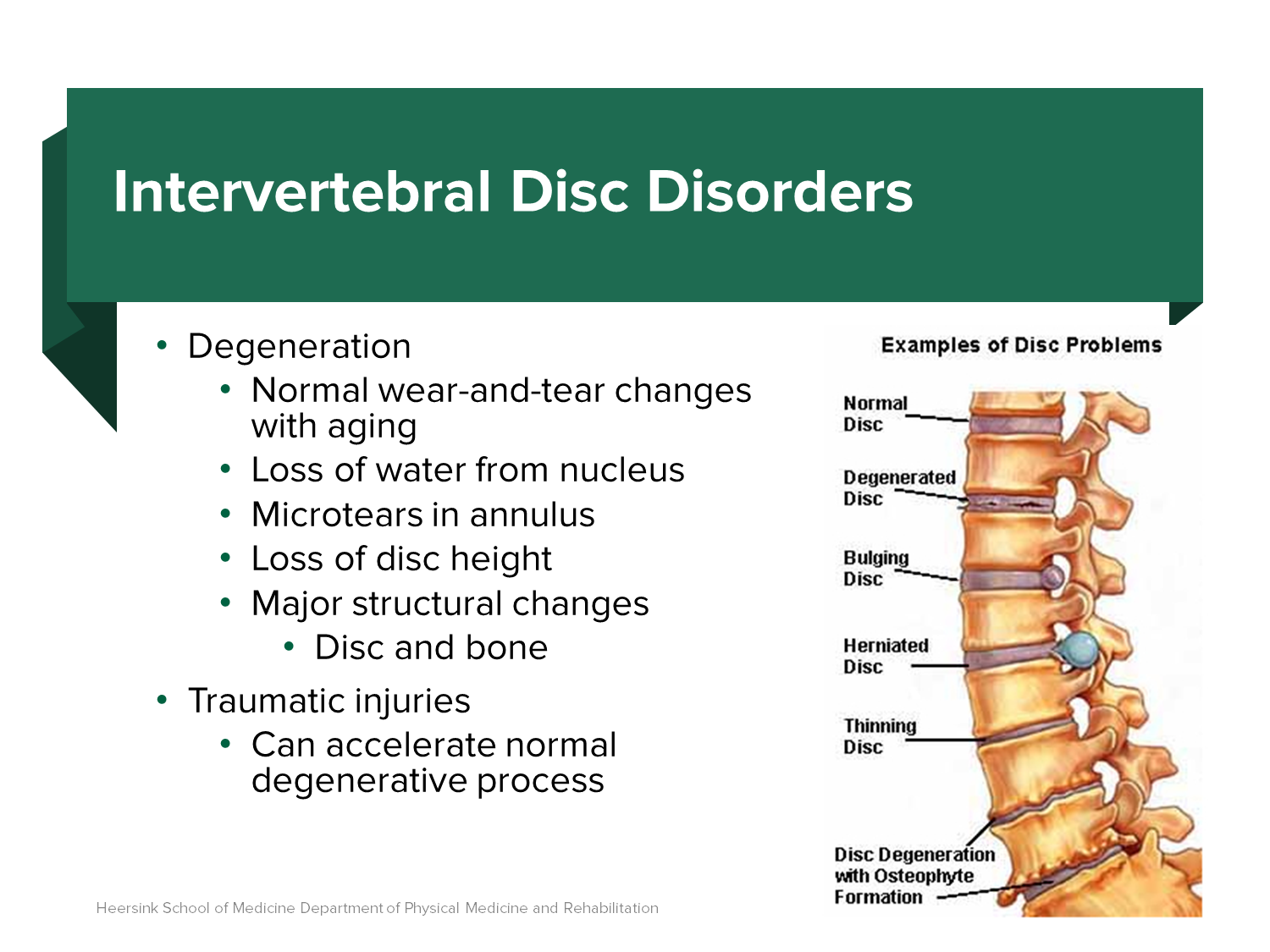
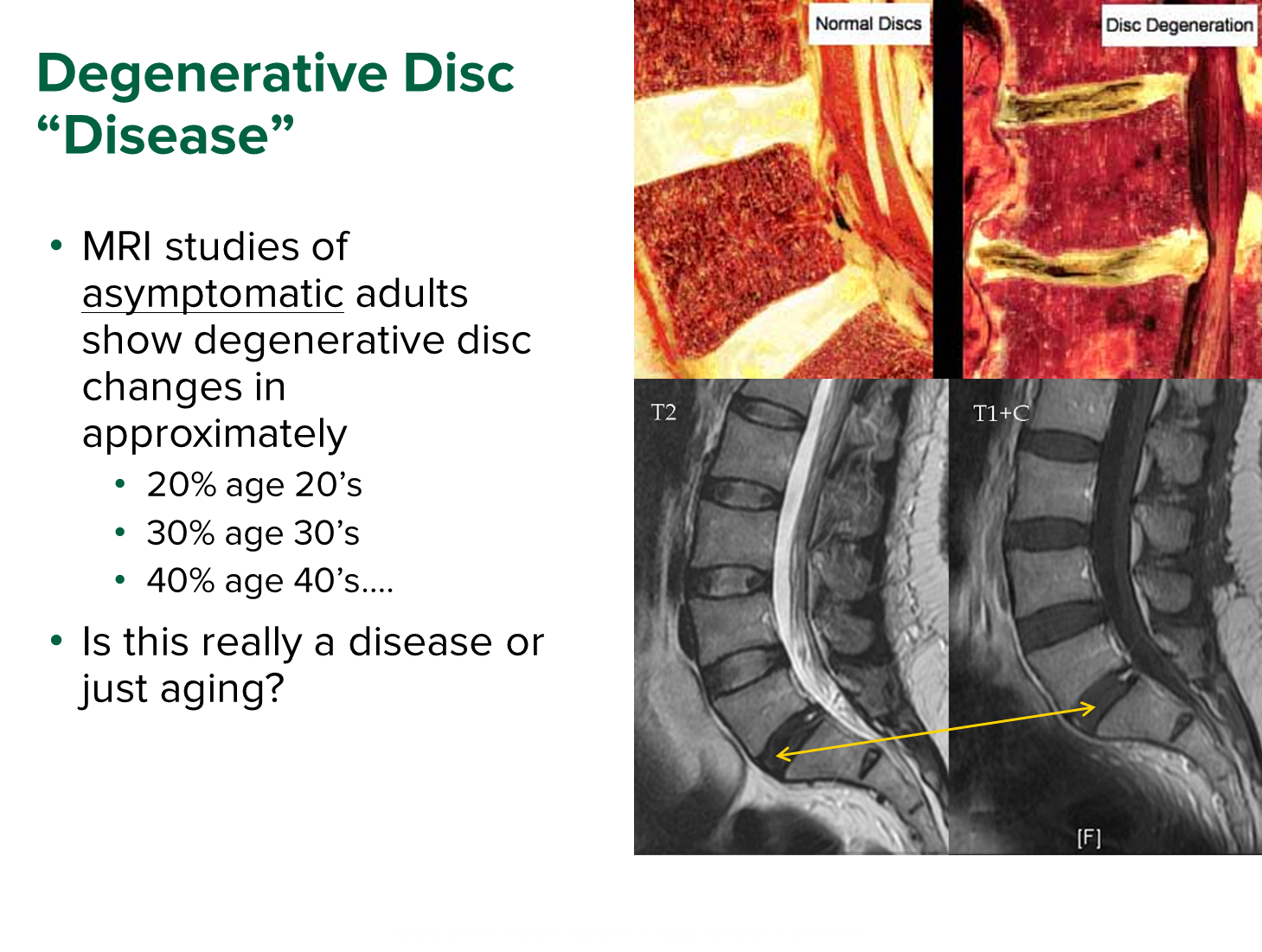
Degenerative Disc Disease is a result of normal wear and tear changes with age resulting in the breakdown of the intervertebral discs
→ it is not a true disease but a normal age-related process
→ slowly the discs show loss of hydration and disc height as well as tears or cracks in the annulus fibrosis especially near the bottom of the vertebral column
→ can present with degenerative disc even without pain
1) Degenerative Disc Disease is associated with
→ increased loads on the disk
→ obesity and sedentary lifestyle
→ poor physical fitness
→ smoking
What can happen when there is damage to the annulus fibrosis?
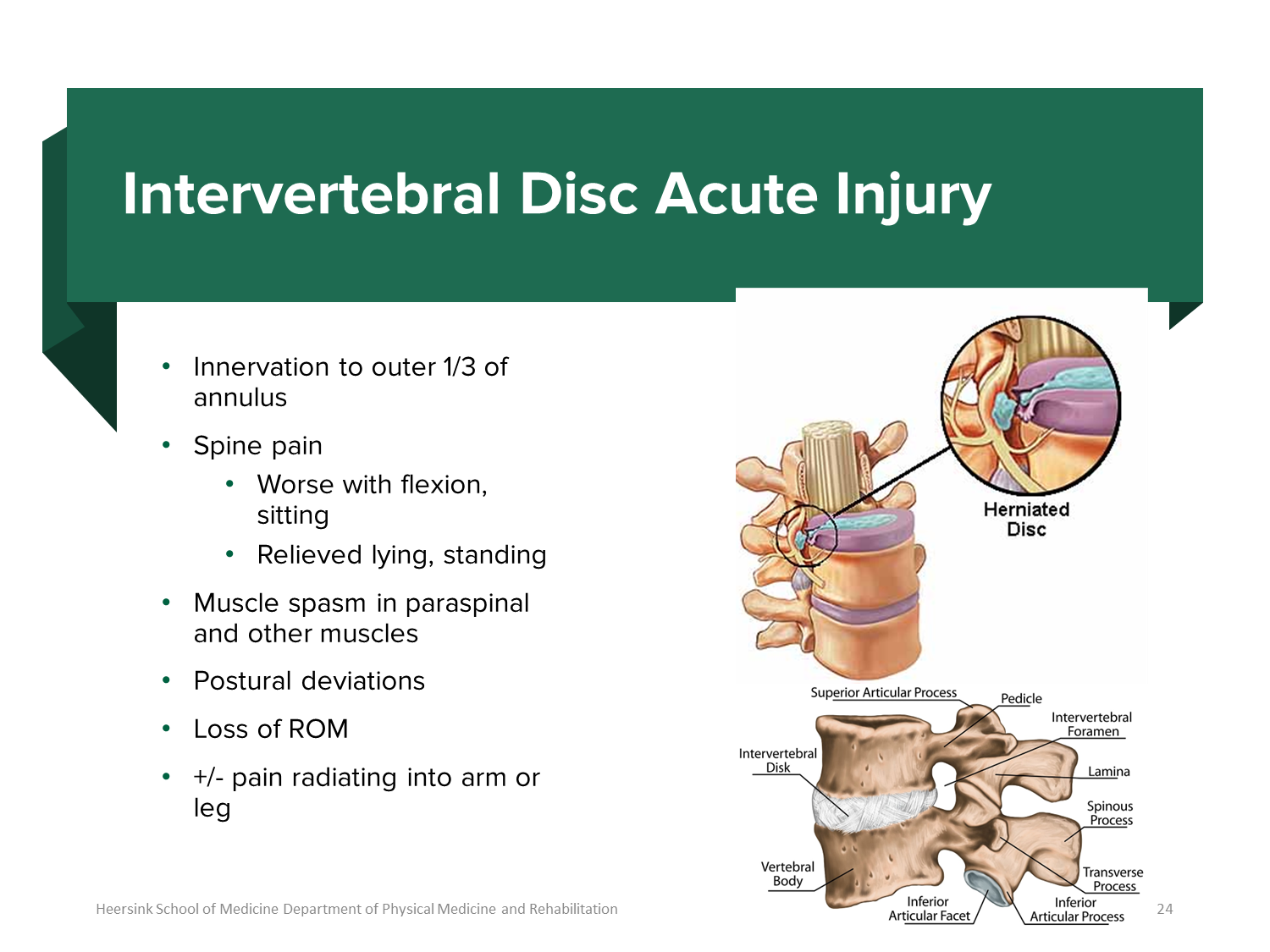
1) The outer 1/3 of the annulus fibrosis is innervated, meaning it has nociceptive nerve fibers
→ tears to this area can lead to spinal pain that gets worse when the spine is flexed or you are sitting
2) Pain to the area can lead to muscle spasm of paraspinal muscles as well as a loss of range of motion
→ can lead to radiating pain
What is the difference between radiculopathy and myelopathy?
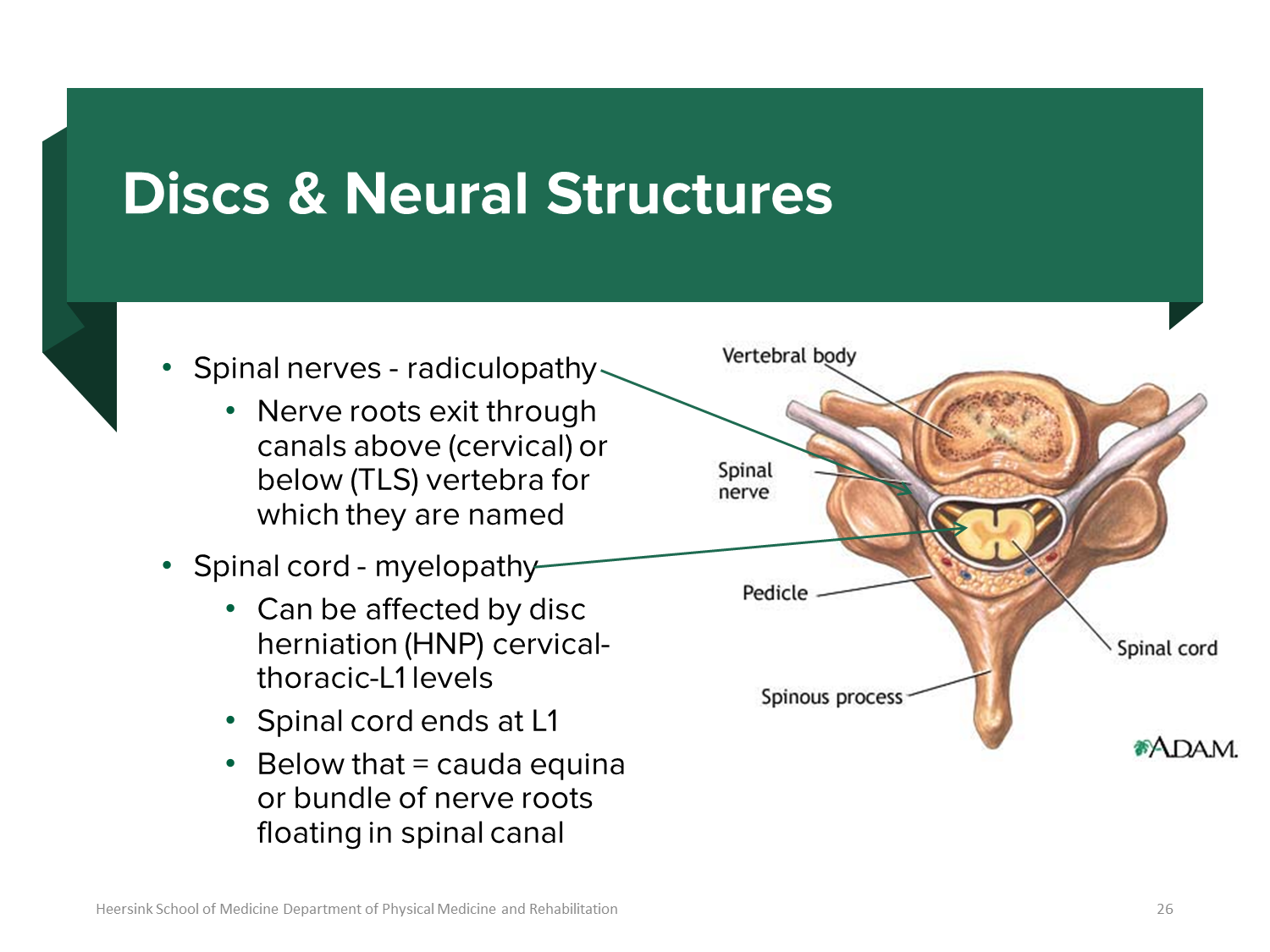
1) Radiculopathy affects the nerve roots (compression of nerve roots)
→ typically occurs as a result of a herniated disc leading to radicular pain shooting down the arm or leg
→ most herniations will occur at the L5-S1 or the L4-L5 area, leading to compression of the lower nerve
→ L5 pain is the top of the foot and S1 pain is the bottom of the foot
→ leads to peripheral nerve symptoms
2) Myelopathy affects the spinal cord
→ caused by a variety of issues such as central canal stenosis and leads to upper motor neuron findings
What is Cauda Equina Syndrome?
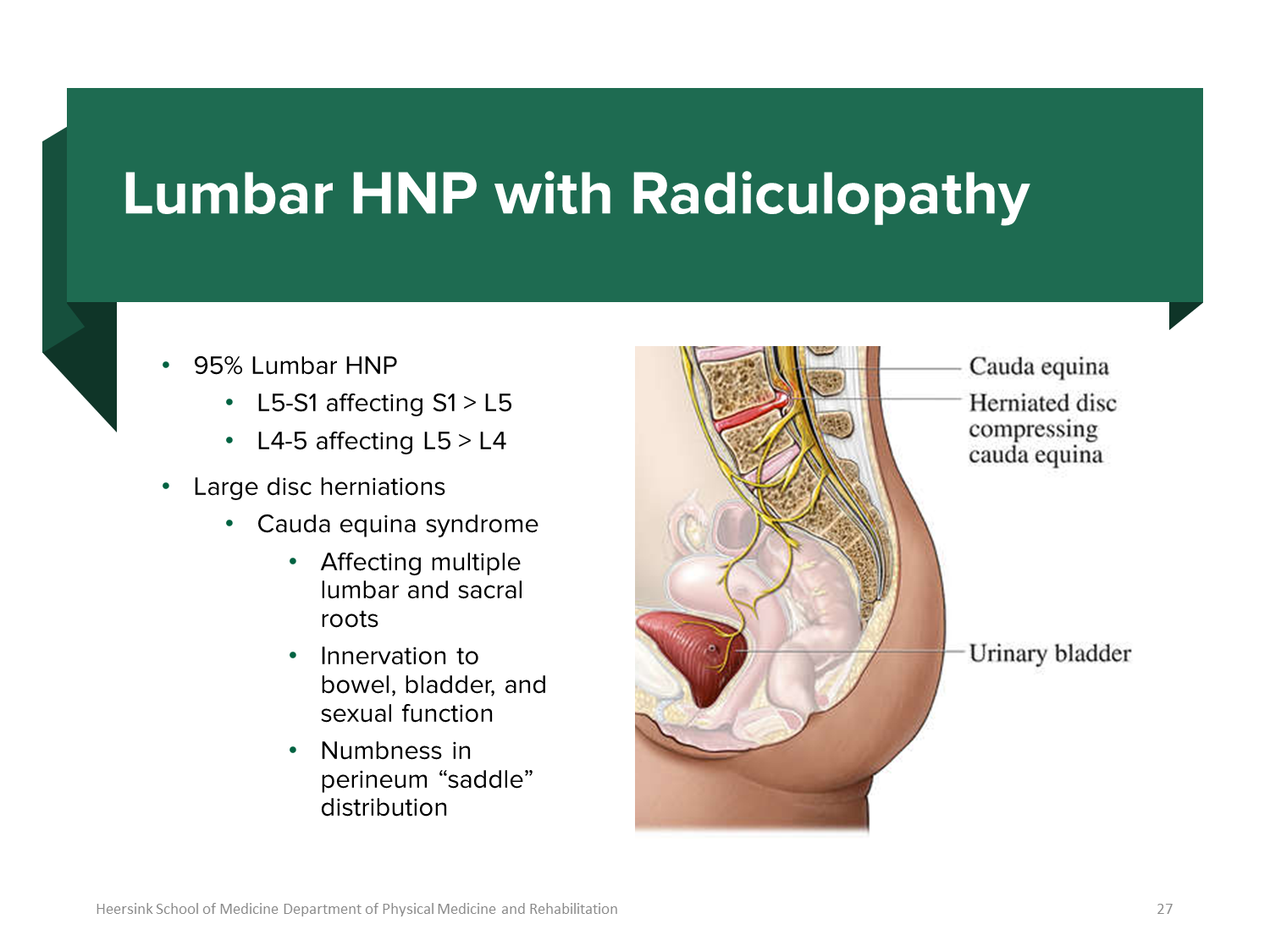
Cauda Equina Syndrome is a medical emergency due to compression of the cauda equina, the bundle of spinal nerve roots at the end of the spinal cord (L1-L2). It is a severe radiculopathy
1) causes a classic saddle anesthesia with loss of sensation in the groin, thighs and butt
→ bladder and bowel dysfunction
→ sexual dysfunction
→ and severe low back pain radiating to both legs
→ causes lower motor neuron signs like hyporeflexia
What is Schmorl’s Nodes?
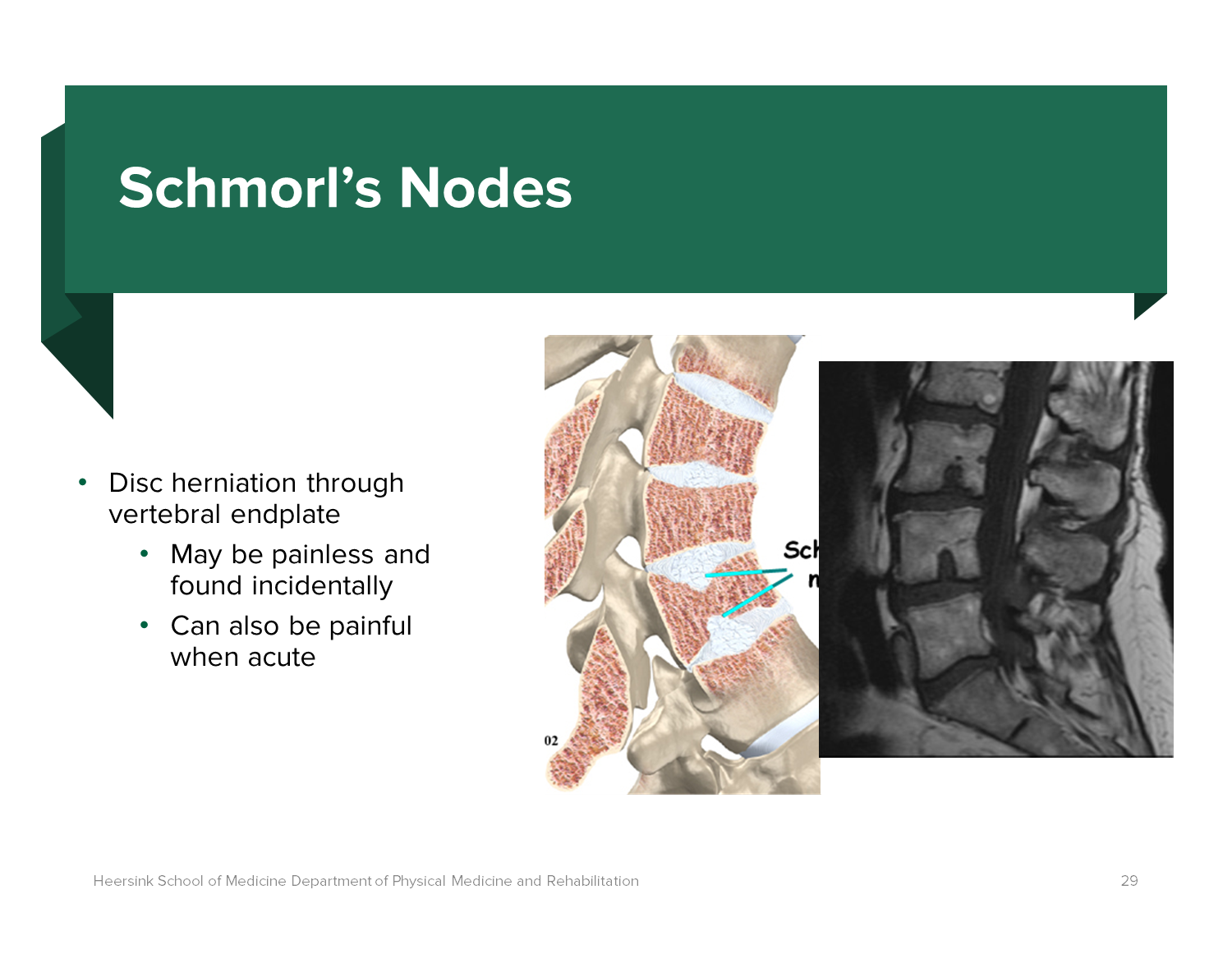
Schmorl’s Nodes are disc herniation upward or a disc herniation into the vertebral endplate
→ often painless but can also be painful when occurring acutely
What are the treatments for lumbar radiculopathy?
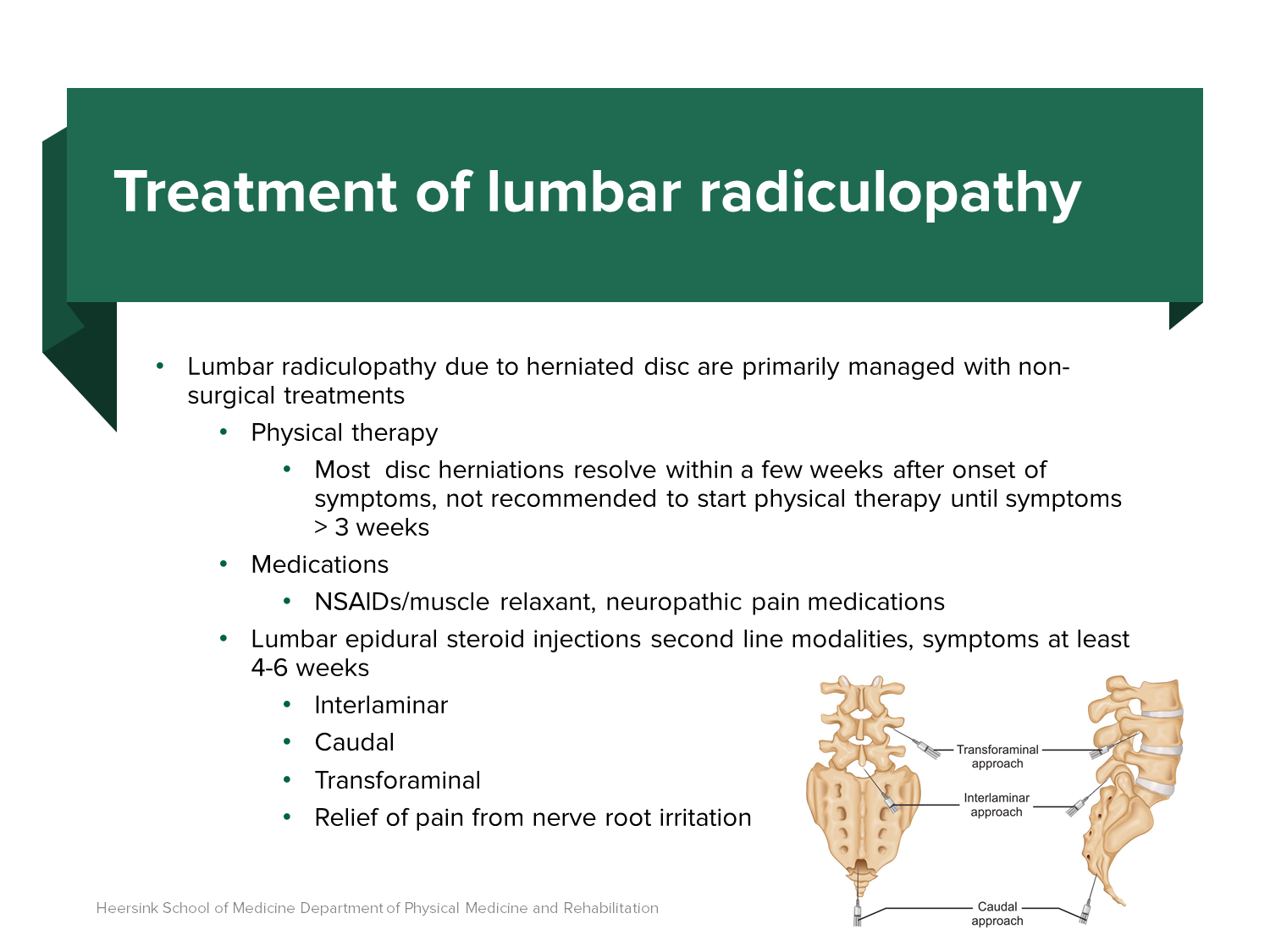
Lumbar Radiculopathy can be treated with:
1) Physical Therapy
→ most disc herniations will spontaneously resolve within a few weeks after onset
→ physical therapy is not recommended until symptoms persist for longer than 3 weeks
2) Medications
→ NSAIDs/Muscle Relaxant
3) Lumbar epidural steroid injections for quick relief
→ Interlaminar - shotgun approach for a broader area, targeting the epidural space between the vertebral lamina
→ Transforaminal - sniper approach for a single area, targeting a single nerve root through the exit foramen
3) Surgeries
→ better for radiculopathy rather than mechanical back pain
→ works better in younger, normal sized, non-smoking patients
What is Spondylosis? What are the subsets?
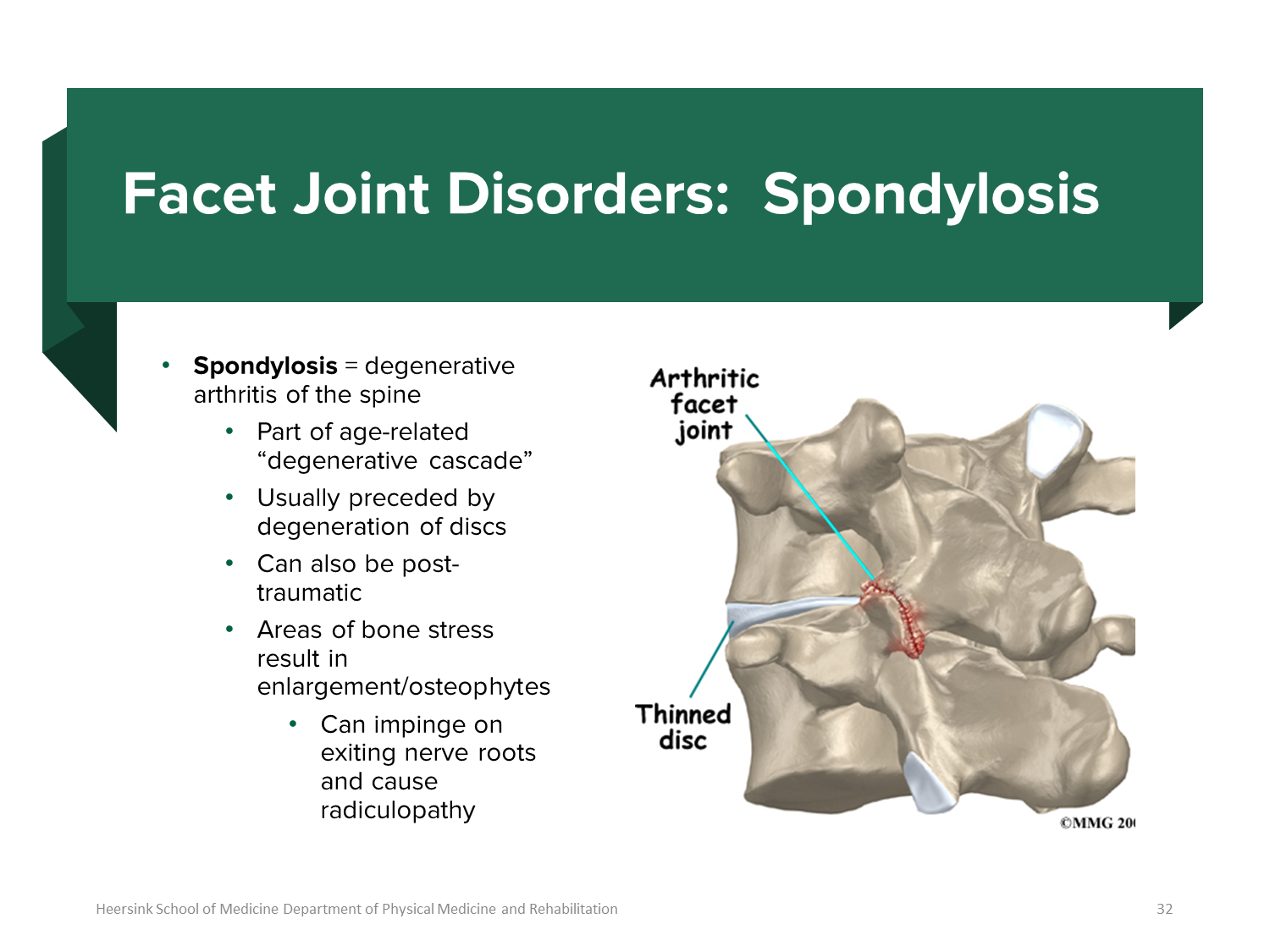
Spondylosis is degenerative arthritis of the spine usually as a result of age-related wear and tear int he spine
→ can cause the growth of osteophytes or bone spurs in areas of stress that can impinge nerves
1) Spondylosis can lead to Facet Syndrome
→ if spondylosis occurs at the facet join/zygapophyseal joints where the articular processes of the vertebrae join
→ results in pain
What is Spinal Stenosis?
Spinal Stenosis is narrowing of the spaces within the spinal canal or neuroforamina which can lead to compression of the spinal cords or nerve roots
→ if the neuroforamina are narrowed there is compression of the nerve roots (radiculopathy)
→ if the spinal canal shrinks then you can have myelopathy
What is the three-column model and what are the kinds of back fractures?
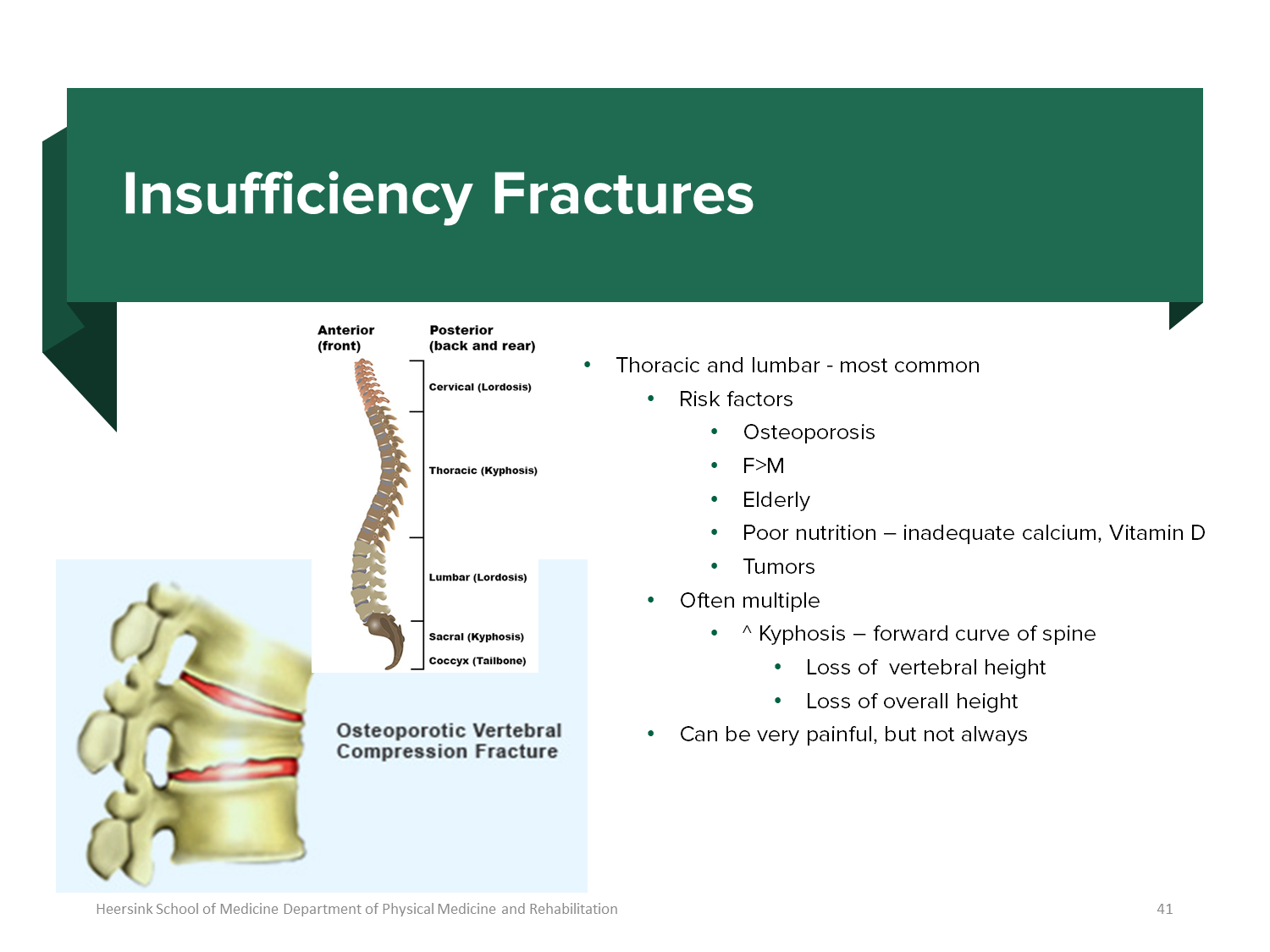
The three-column concept divides the back into an anterior, middle and posterior column and allows us to determine if a spinal fracture is stable or unstable
→ you would only treat when 2 or more columns are injured (instability)
There are 2 kinds of fractures
1) Traumatic Fractures
→ trauma to the spine, with the majority not affecting neurologic function
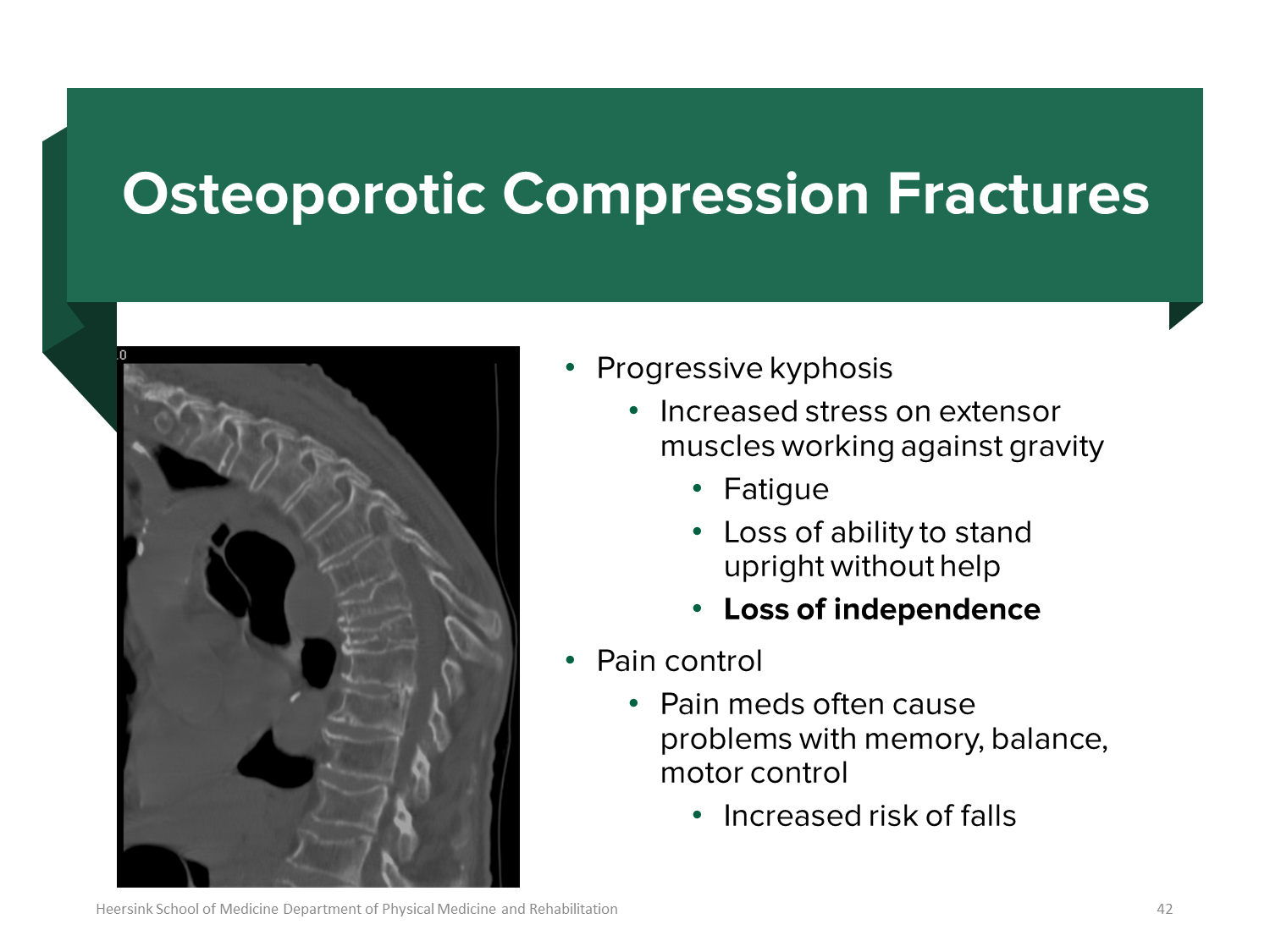
2) Insufficiency Fractures
→ stress fracture applied to an abnormally weak bone such as an older person with osteoporosis
→ more common in the thoracic and lumbar area
→ leads to kyphosis or hunch back
What is Spondylolysis?
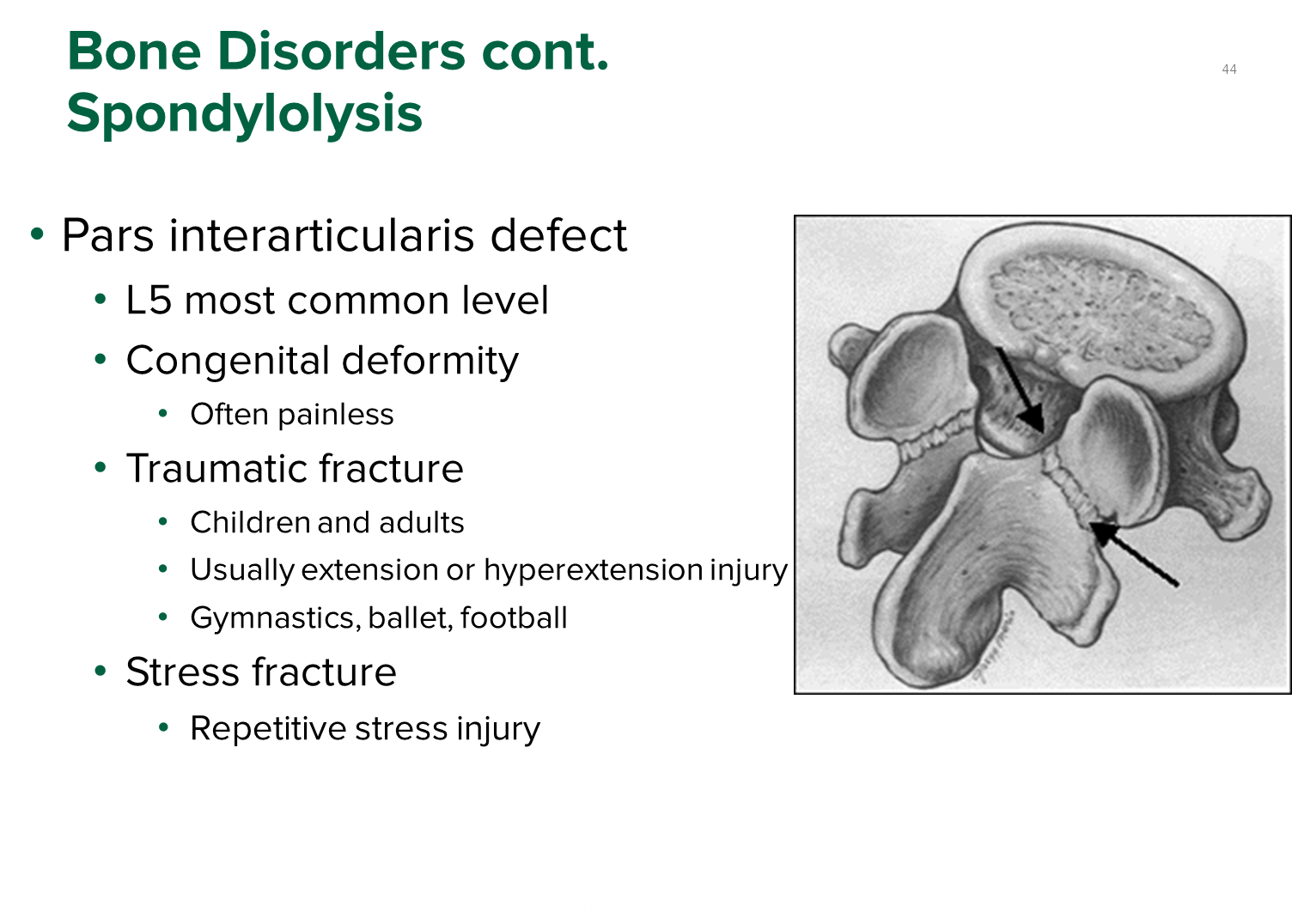
Spondylolysis is a stress fracture in the pars interarticularis of the vertebrae, or the bony bridge connecting the superior and inferior articular processes
1) most common occurs at the L5 level and is seen in people with a traumatic injury involving hyperextension of the back
→ like gymnastics
2) Extension makes the back pain worse and is relieved by flexion
What is Spondylolisthesis?

Spondylolisthesis is a forward slippage of one vertebral body over the one below it
→ the vertebral body will slide forward
1) Seen in patients with spondylolysis that progresses due to continued hyperextension, can progress to having neurologic symptoms
→ older patients may have spondylolisthesis due to degenerative disc
What is Scoliosis?
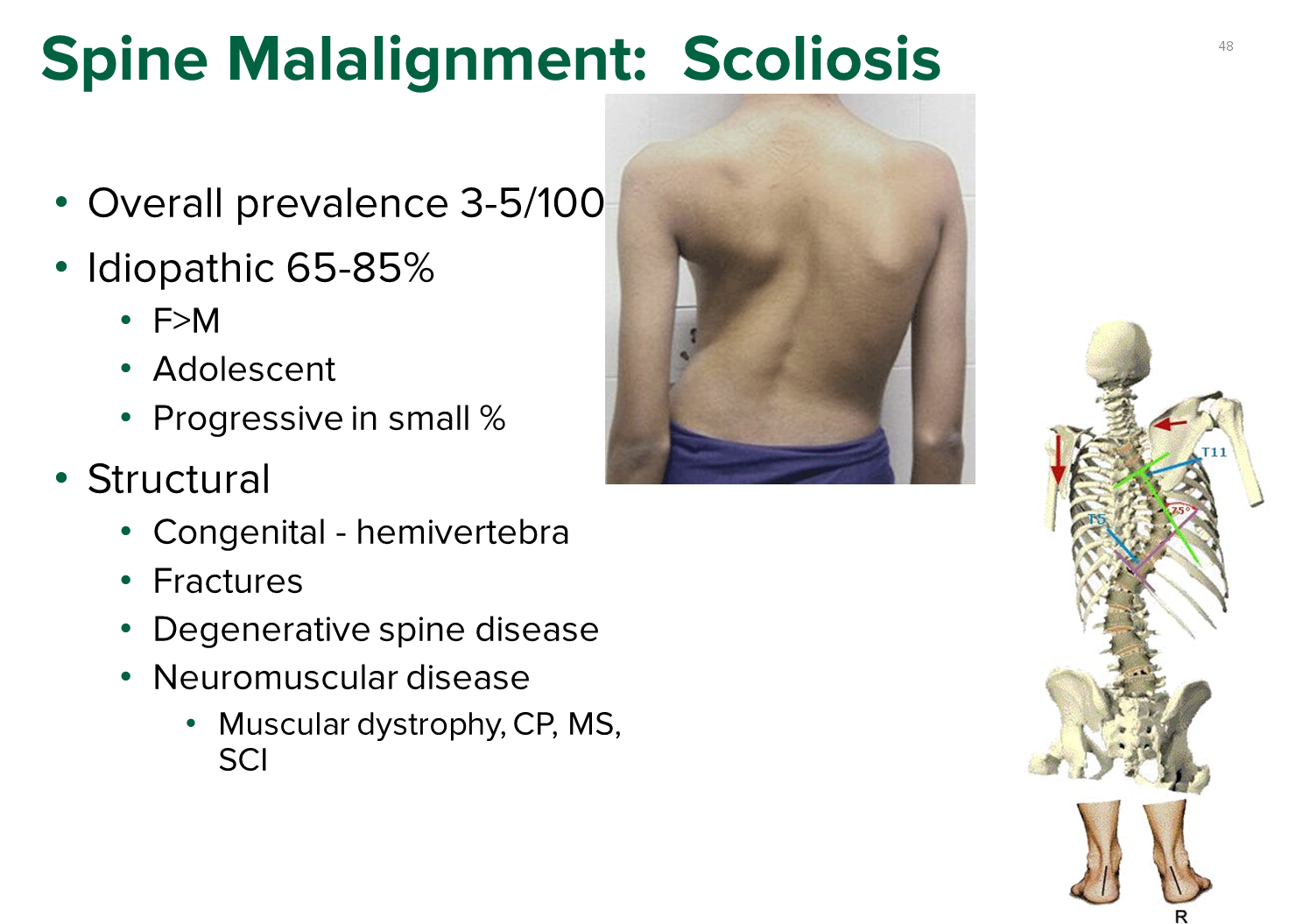
Scoliosis is a lateral curvature of the spine greater than 10 degrees and is often idiopathic
→ most often congenital, but can lead to pain and muscular dystrophy