Complex Health: Exam 1
1/259
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
260 Terms
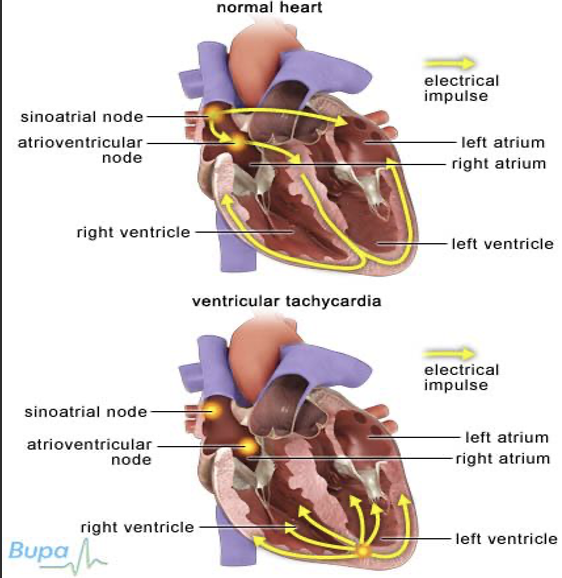
Cardiac Electrical Activity
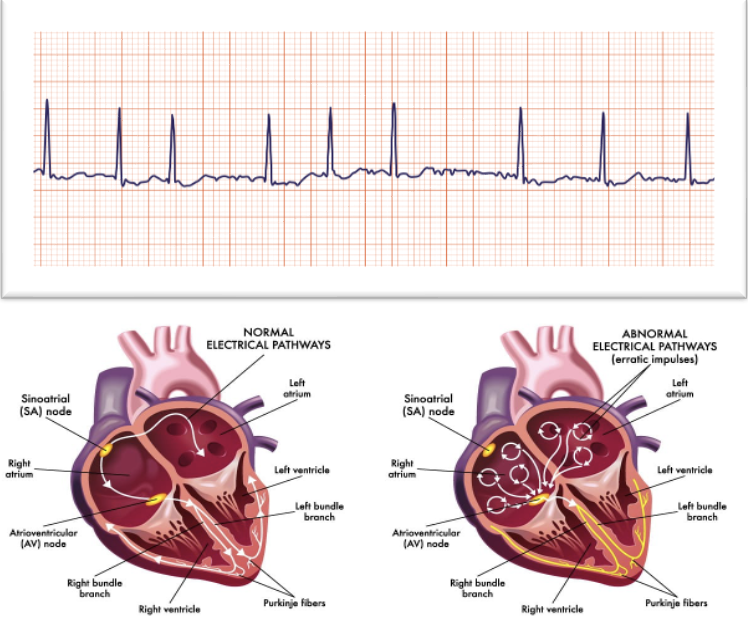
All cardiac cells have the potential to generate electrical impulses.
Ectopy: Stimuli generated outside of the normal conduction pathway.
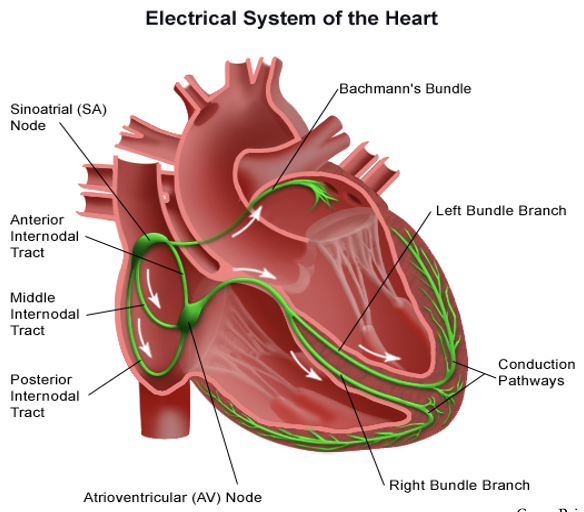
SA Node Intrinsic Rate is…
60 to 100 bpm
AV Node Intrinsic Rate is…
40 to 60 bpm
Bundle Branches Intrinsic Rate is…
25 to 40 bpm
Cardiac Cycle (picture)
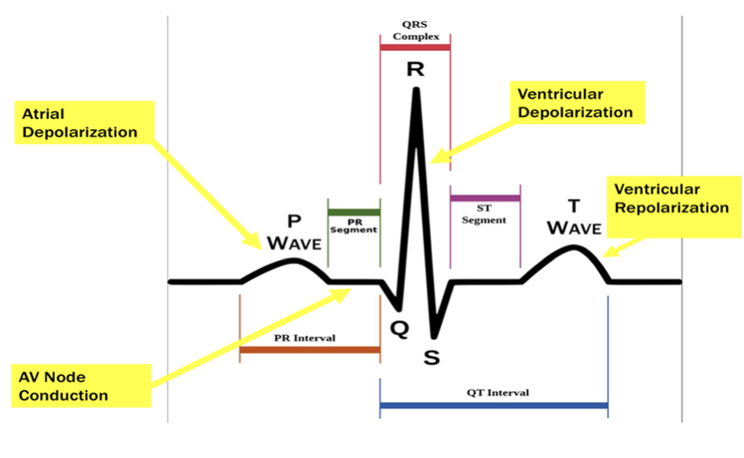
Understanding ECG Graph Paper
Mechanics:
Used to standardize tracings.
Vertical boxes measure voltage/amplitude (T wave/ST elevation)
Sizing:
1 small box = 0.04 seconds
1 large box = 0.20 seconds = 5 small boxes
5 large boxes = 1 second
30 large boxes = 6 seconds
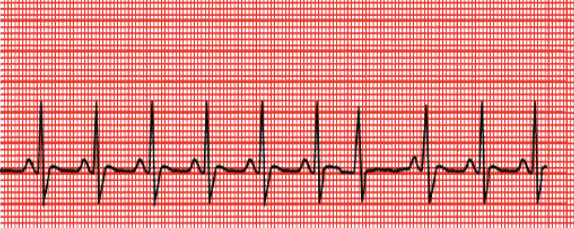
Interpretation of Rhythms
Steps of Rhythm:
Rhythm — Is it regular or irregular?
Heart Rate — Is it fast or slow?
Evaluate the P wave
Measure the PR interval
Evaluate/measure the QRS (including the QT segment)
Evaluate the ST segment — Is it at baseline?
Evaluate the T wave — Upright? Peaked or flattened?
Sinus Rhythms
Originate from Sinus Node:
Normal Sinus
Sinus Bradycardia
Sinus Tachycardia
Sinus Arrhythmia
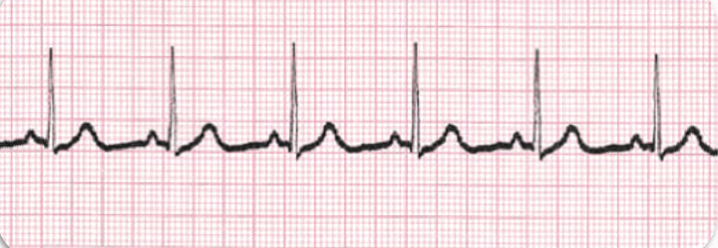
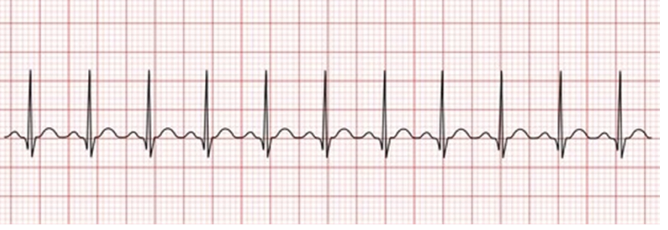
Normal Sinus Rhythm (NSR): Criteria
Rate: 60 to 100 (ventricular and atrial)
Rhythm: Regular
P waves: Uniform and upright
P to QRS Ratio: 1:1
PR Interval: 0.12 to 0.20 seconds
QRS Complex: Less than 0.12 seconds
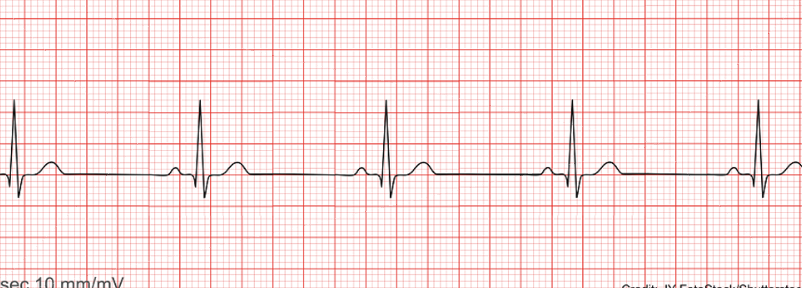
Sinus Bradycardia: Criteria
Rate: Less than 60 bpm in the adult (ventricular and atrial)
Rhythm: Regular
P waves: Normal and consistent, in front of the QRS
P to QRS Ratio: 1:1
PR Interval: Consistent, between 0.12 and 0.20 seconds
QRS Complex: Less than 0.12 seconds
Sinus Bradycardia: Causes
Lower Metabolic Needs:
Sleep
Athletic training
Hypothermia
Vagal Stimulation:
Vomiting
Suctioning
Bowel movements
Medications:
Calcium channel blockers
Beta-blockers
Other:
Increased intracranial pressure
Coronary artery disease
Inferior wall MI
Decompensated heart failure
Electrolyte deficiencies
Sinus Bradycardia: Clinical Manifestations & Diagnostics
Clinical Manifestations:
Lightheadedness or dizziness (especially with exertion)
Easy fatiguability
Syncope (fainting) or near-syncope
Dyspnea (shortness of breath)
Chest pain or discomfort
Confusion
Diagnostics:
Vital signs
12-lead ECG
Chief complaint/complete history and physical examination
Lab work
Echocardiogram (ultrasound of the heart)
Sinus Bradycardia: Treatments
Treatment:
Fix the problem/correct the cause.
Stop the meds, warm the patient, and stop nausea/vomiting.
If Symptomatic:
Atropine 1 mg IV bolus, repeated every 3 to 5 minutes until a maximum dose of 3 mg.
An order is typically needed, except for emergencies; Have to be ACLS trained.
How do you know when to stop giving the atropine?—You have reached your max dose or you patient is now stable (Pulses, HR, BP, etc.)
If ineffective, apply pacing pads to the skin for transcutaneous pacing. (a little more invasive)
Provide medication/sedation prior—it shocks!
If that is ineffective, administer epinephrine and/or dopamine.

Sinus Tachycardia: Criteria
Rate: Greater than 100 bpm in the adult (ventricular and atrial)
Rhythm: Regular
P Waves: Normal and consistent, in front of the QRS
P to QRS Ratio: 1:1
PR Interval: Consistent, between 0.12 and 0.20 seconds
QRS Complex: Less than 0.12 seconds
Sinus Tachycardia: Causes
Physiologic:
Acute blood loss
Anemia
Severe dehydration
Shock
Hypovolemia
Heart failure
Pain
Hypermetabolic states
Fever
Exercise
Psychological Stress:
Anxiety
Medications:
Cold meds — pseudoephedrine
Bronchodilators — albuterol
ADHD — Ritalin and Adderall
Antidepressants — Cymbalta
Thyroid meds — Synthroid
Other Stimulants:
Caffeine, nicotine
Amphetamines, cocaine, ecstasy
Autonomic Dysfunction:
Postural Orthostatic Tachycardia Syndrome (POTS) — Tachycardia with position changes but with an adequate change in BP to perfuse the brain.
Sinus Tachycardia: Clinical Manifestations & Diagnostics
Clinical Manifestations:
Drop in blood pressure upon standing (orthostatic hypotension)
Palpitations
Fatigue
Exercise intolerance
Blurred vision
Dizziness
Chest pain
Fainting
Lightheadedness
Shortness of breath
Sweating
Weakness
Diagnostics:
Vital signs
12-lead ECG
Chief complaint/complete history and physical examination
Lab work
Echocardiogram (ultrasound of the heart)
Sinus Tachycardia: Treatment (treat the problem!)
Physiologic:
Acute blood loss, anemia — Find the source, replace the loss.
Dehydration — Fluids/eliminate the cause; provide fluid replacement.
Fever — Use antipyretics.
Pain — Use pharmacological and non-pharmacological pain relief.
Shock — Identify the type and treat the cause.
Psychological Stress:
Make lifestyle changes.
Seek mental health treatment.
Medications:
Change or avoid certain medications. (amphetamines, cold medicine, etc.)
Use beta-blockers (e.g., Metoprolol, Lopressor, etc.)
Use calcium channel blockers (e.g., Amlodipine, Diltiazem, etc.)
Other Stimulants:
Eliminate the source (caffeine, alcohol, smoking, drugs, etc.)
If Unresponsive to Other Treatments:
Possible cardiac ablation therapy.
Atrial Rhythms
Originate from Foci within the Atria:
Premature Atrial Complexes (PACs)
Atrial Fibrillation (A-Fib)
Atrial Flutter (A-Flutter)
Premature Atrial Contractions (PACs)
Signs/Symptoms:
The patient may say, “My heart skipped a beat.”
Possible pulse deficit (difference between apical and radial pulse rate).
Causes:
Caffeine, alcohol, nicotine
Stretched atrial myocardium (e.g., as in hypervolemia)
Stress/anxiety
Electrolyte imbalances
Atrial ischemia, injury, or infarction
Treatment:
Treat the underlying cause:
Replace electrolytes
Reduce stress/anxiety
Dietary changes
Asymptomatic = no treatment
Symptomatic = Amiodarone and beta-blockers

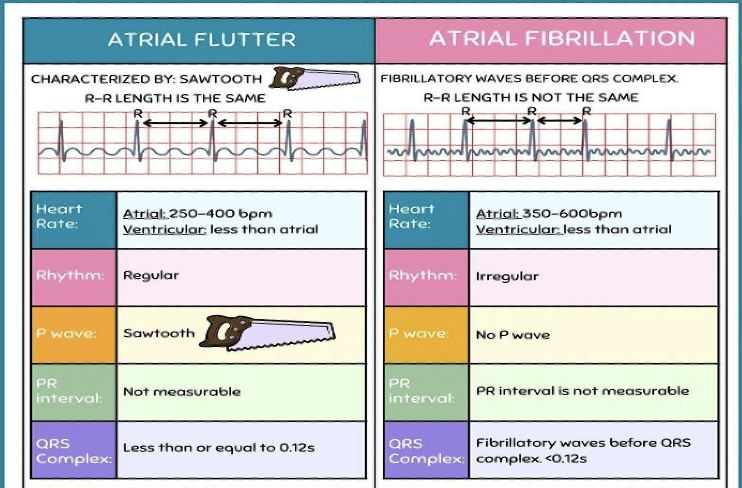
Atrial Fibrillation (A-Fib): Criteria
Rate: Atrial — 300 to 600 bpm; Ventricular — Variable, but between 60 to 100 bpm
Rhythm: Highly irregular
P Waves: No discernible P waves; irregular, undulating waves are referred to as fibrillatory or f waves
P to QRS Ratio: Not discernible
PR Interval: Absent; unmeasurable due to lack of P waves
QRS Complex: Usually normal
A-Fib: Risk Factors
Increasing Age
Hypertension
Diabetes
Obesity
Valvular heart disease
Heart failure
Obstructive sleep apnea
Alcohol abuse
Hyperthyroidism
Myocardial infarction
Smoking
Exercise
Cardiothoracic surgery
Increased pulse pressure
European ancestry
Family history
A-Fib with RVR (Rapid Ventricular Response): Criteria
Rate: Atrial — 300 to 600 bpm; Ventricular — Variable, between 100 to 200 bpm
Rhythm: Highly irregular
P Waves: No discernible P waves; irregular, undulating waves (fibrillatory or f waves)
P to QRS Ratio: Many:1
PR Interval: Absent; unmeasurable due to lack of P waves
QRS Complex: Usually normal
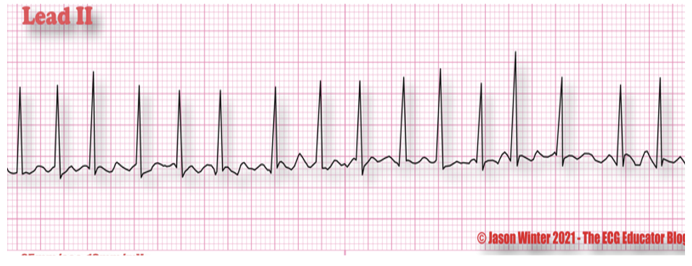
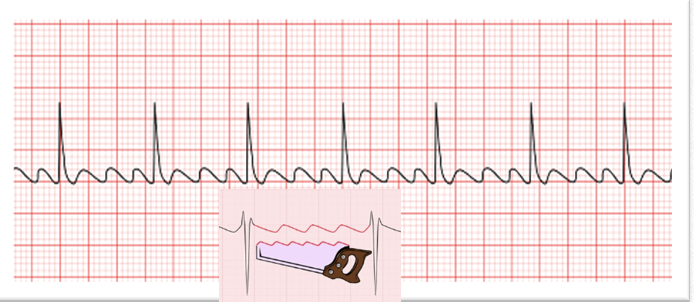
Atrial Flutter (A-Flutter): Criteria
Rate: Atrial — 250 to 400 bpm; Ventricular — 75 to 150 bpm
Rhythm: Atrial regular; Ventricular usually regular but may be irregular due to changes in AV conduction
P Waves: Saw-toothed, referred to as F waves
P to QRS Ratio: 2:1, 3:1, or 4:1
PR Interval: Multiple F waves make determination difficult
QRS Complex: Usually normal
A-Flutter/A-Fib Comparison Chart + Interventions
A-Flutter:
Unstable patients: Prepare for cardioversion.
Administer medication: Anticoagulant
A-Fib:
Unstable patients: Prepare for cardioversion.
O2 therapy
Anticoagulants: To prevent emboli.
Administer cardiac medications (beta-blockers, calcium channel blockers, digoxin)
A-Fib/A-Flutter: Clinical Manifestations
Signs:
Irregular pulse
"Pulse deficit"
Variable heart sounds
May present with a murmur or pulmonary edema
Symptoms:
Palpitations
Shortness of breath
Dizziness/lightheadedness
Chest pain
Fatigue
Dyspnea on exertion
Important to Know:
May be asymptomatic
Patients are 5 times more likely to suffer a stroke (approximately 15% are caused by A-fib)!!
A-Fib/A-Flutter: Management
Prevention: Anticoagulants:
Warfarin (Coumadin)—1st line; frequent lab monitoring—PT/PTT/INR
Factor Xa inhibitors (Pradaxa, Xarelto, Eliquis)—DOAC $$$
Non-Invasive Treatments:
Rate control medications:
Calcium channel blockers: Diltiazem, etc.
Beta-blockers: Metoprolol, etc.
Digoxin
Cardioversion: Often preceded by a transesophageal echocardiogram (TEE)
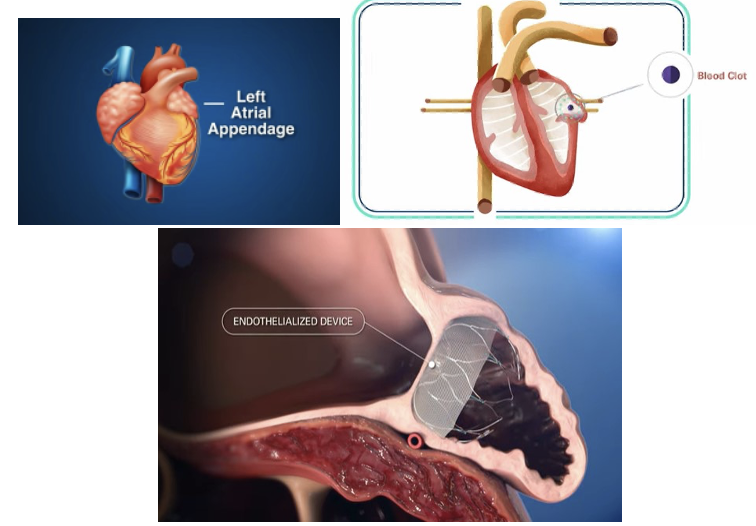
Invasive Procedures:
Ablation/Maze Procedure: Small transmural incisions are made in the atria, resulting in scar formation.
Left Atrial Appendage Occlusion (LAAO)/WATCHMAN: Reduces the risk of blood clots from entering the bloodstream and causing a stroke.
Acute + Symptomatic (unstable): Cardioversion → baseline
Acute + Asymptomatic (stable): IV Amiodarone drip is first-line treatment:
Given an IV bolus dose of 150 mg over 10 minutes → Infusion/drip: 1 mg/min over 6 hours → 0.5 mg/min over 18 hours → transitioned to PO.
Chronic: rate control (b/c they have already attempted to correct when first diagnosed, but efforts have failed)—BBs & CCBs
Left Atrial Appendage (LAA) Occlusion (WATCHMAN)
90% of clots are formed by a-fib that originate in the LAA.
An endothelialized device is placed inside of that area and keeps/catches clots from getting out into the heart and the rest of the body.
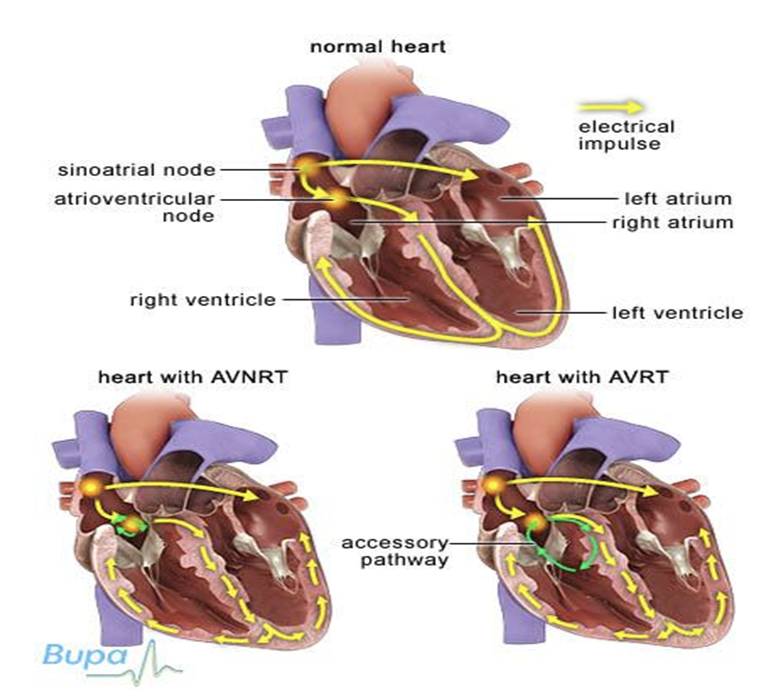
Junction Arrhythmias
Originate within AV Nodal Tissue:
Premature Junctional Complexes (PJCs)
Junctional Rhythms
Junctional Tachycardia
Atrioventricular Nodal Reentry Tachycardia (AVNRT)
SVT (Supraventricular Tachycardia)
PVST (Paroxysmal Supraventricular Tachycardia)
PAT (Paroxysmal Atrial Tachycardia)
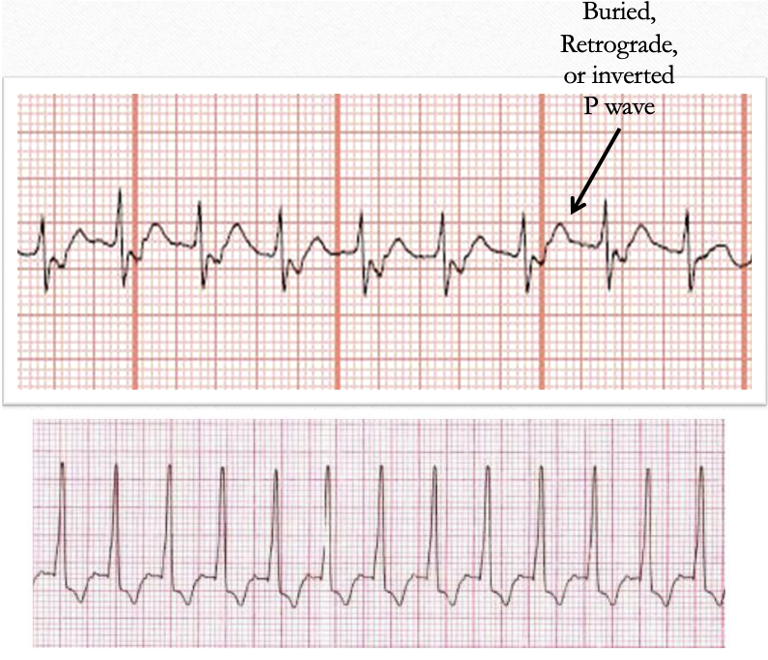
Junctional Rhythms: Criteria
Rate: Atrial — 40 to 60 bpm (if there is retrograde conduction); Ventricular — 40 to 60 bpm
Rhythm: Regular
P Waves: May be absent, may be inverted
P to QRS Ratio: 1:1 or 0:1
PR Interval: If the P wave is in front of the QRS, the PR interval is less than 0.12 seconds
QRS Complex: Usually normal

Junctional Rhythms: Causes, S/Sx, & Treatments
Causes:
Hypokalemia and side effects of medications
Myocardial infarction (MI)
Cardiac surgery
Digitalis (Digoxin) toxicity
Sinus node dysfunction
Post AV node ablation
Signs & Symptoms: (collapsed)
Chest pain
Oxygen deficiency
Low blood pressure (BP)
Lethargy
Anxiety
Palpitations
Shortness of breath
Elevated ventricular rate or heart rate
Dizziness or syncope (fainting)
Lightheadedness
Activity intolerance
Weakness
Treatments:
Same as for sinus bradycardia — treat the underlying cause(s)!
Lifestyle changes
Medication changes
Permanent pacemaker
Premature Junctional Complexes (PJCs)
Signs & Symptoms:
Usually the same as PACs
The patient may say, “My heart skipped a beat.”
Possible pulse deficit (difference between the apical & radial pulse rates)
Rarely produces significant symptoms
Causes:
Digitalis (Digoxin) toxicity
Heart failure
Coronary artery disease
Treatment:
Same for PACs — treat the underlying cause
Change the medications and/or make lifestyle changes
Permanent pacemaker
Junctional Tachycardia: Criteria
Rate: Atrial — 70 to 120 bpm (if P waves are discernible); Ventricular — 70 to 120 bpm
Rhythm: Regular
P Waves: May be absent, after the QRS, or before the QRS; may be inverted
P to QRS Ratio: 1:1 or 0:1
PR Interval: If the P wave is in front of the QRS, the PR interval is less than 0.12 seconds
QRS Complex: Usually normal, may be widened
Junctional Tachycardia: Causes, S/Sx, & Tachycardia
Causes:
Digoxin toxicity is the cause of 60% of cases
Inferior myocardial infarction
Hypokalemia
Open-heart surgery
Signs & Symptoms:
Will depend on the precipitating cause
Treatment:
Eliminate or treat the underlying cause (e.g., Digoxin toxicity)
Antiarrhythmic drugs
Permanent pacemaker
Atrioventricular Nodal Reentry Tachycardia (AVNRT)
AVNRT is a common arrhythmia that occurs when an impulse is conducted to an area in the AV node, causing the impulse to be routed back into the same area repeatedly at a very fast rate.
Each time the impulse is conducted through the area, it is also conducted down into the ventricles, resulting in a fast ventricular rate.
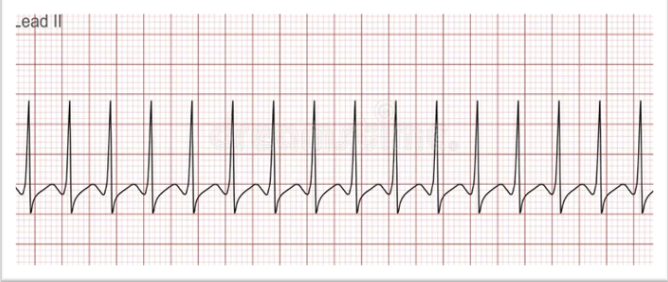
Supraventricular Tachycardia (PSVT or SVT): Criteria
Rate: 150 to 250 bpm
Rhythm: Regular, with sudden onset and termination
P Waves: Difficult to discern
P to QRS Ratio: 1:1
PR Interval: If the P wave is visible, the PR interval is less than 0.12 seconds
QRS Complex: Usually normal, may be slightly widened
PSVT: coming and going
SVT: typically sustainable, constant
Supraventricular Tachycardia (PSVT or SVT): Causes, S/Sx, & Diagnostics
Causes:
Caffeine
Nicotine
Hypoxemia
Stress
Not associated with underlying structural heart disease
Signs & Symptoms (due to decreased cardiac output):
Dizziness/Syncope
Palpitations
Restlessness
Chest pain
Shortness of breath
Pallor
Hypotension
Diagnostics:
Clinical picture / History & Physical (H&P)
ECG (basic and 12-lead)
Blood work
Echocardiogram
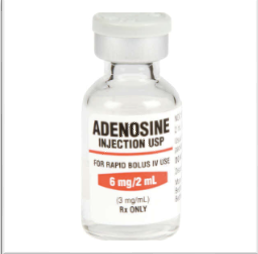
SVT: Treatments
Stable:
Vagal maneuvers (the first thing you want to do is get the pt. to bear down, cough, suction)
Adenosine: 6 mg → 12 mg → 12 mg IV, rapid push
Done in a controlled environment (ACLS nurse + provider @ bedside w/ crash cart and respiratory team)
Done in a sequence of doses until the pt’s HR goes down. (not all doses are necessarily used)
Consider synchronized cardioversion
IV calcium channel blocker or IV beta-blocker
Unstable:
Immediate synchronized cardioversion
Long-Term:
Ablation therapy
Treatment:
Correct the underlying causes
Administer fluids, blood products, and pain medications
Reduce anxiety
Discontinue medications or stimulants causing the issue
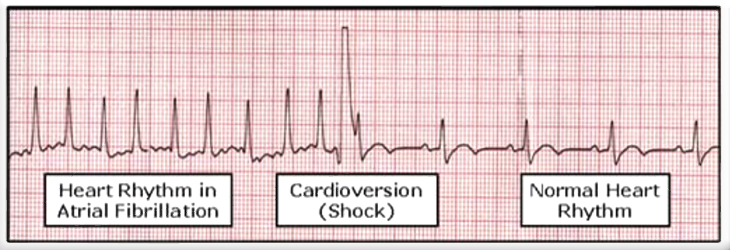
Defibrillation vs. Cardioversion
Defibrillation:
Emergency procedure—used only for cardiac arrest.
Not synchronized with the cardiac cycle
Used for Ventricular Fibrillation (V-Fib) or pulseless Ventricular Tachycardia (V-Tach)
No cardiac output
Begin with 200 Joules, may increase up to 360 Joules
Client is unconscious—Not used for patients who are conscious or have a pulse.
Continuous ECG monitoring
Cardioversion:
Elective procedure
For tachydysrhythmias (unstable)
Client is awake and often sedated
Synchronized with the QRS complex
Energy level: 50 to 200 Joules
Consent form required
Continuous ECG monitoring
**Switch to cardioversion sync mode!!*
Oh, Say It Isn’t So!—Preparing for Cardioversion
O – Oxygen monitoring
S – Suction equipment
I – IV access
I – Intubation supplies
S – Sedation and analgesics
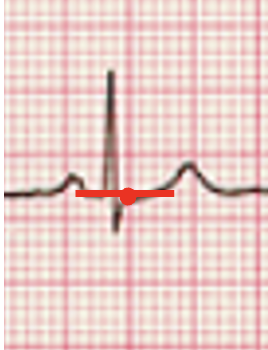
Synchronized Cardioversion at Work
Shock delivered on the R wave at ventricular depolarization.
Ventricular Dysrhythmias
Originate from Irritable Foci within the Ventricles:
Premature Ventricular Complexes (PVCs)
Ventricular Tachycardia (V-Tach)
Polymorphic Ventricular Tachycardia (Torsades de Pointes)
Ventricular Fibrillation (V-Fib)
Ventricular Asystole
Pulseless Electrical Activity (PEA)
Premature Ventricular Complexes (PVCs)
Causes:
Cardiac ischemia or infarction, tissue hypoxia
Anxiety, stress
Caffeine, nicotine, alcohol
Increased cardiac workload
Electrolyte imbalances
Signs & Symptoms:
“My heart skipped a beat”
Often patients are asymptomatic (at first)
Treatments:
Correct the cause
Medications (antidysrhythmics)
Lifestyle changes
Ablation
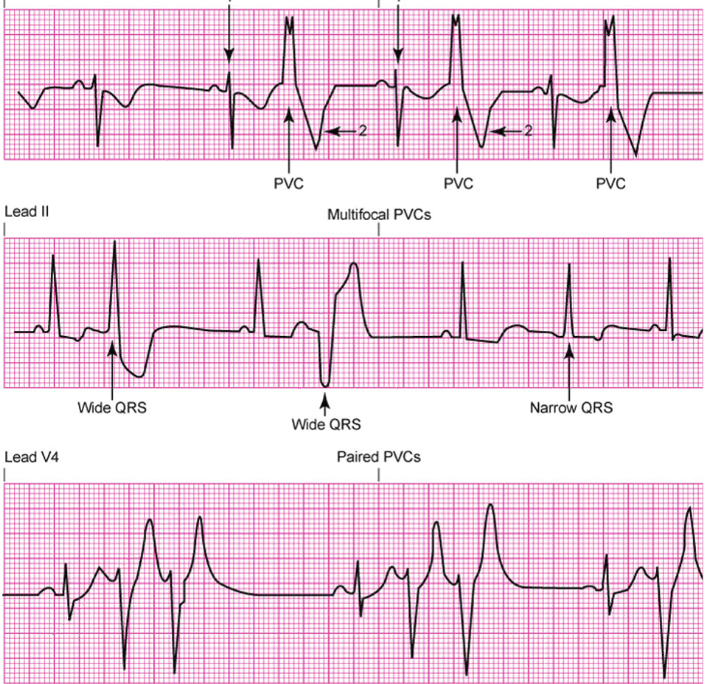
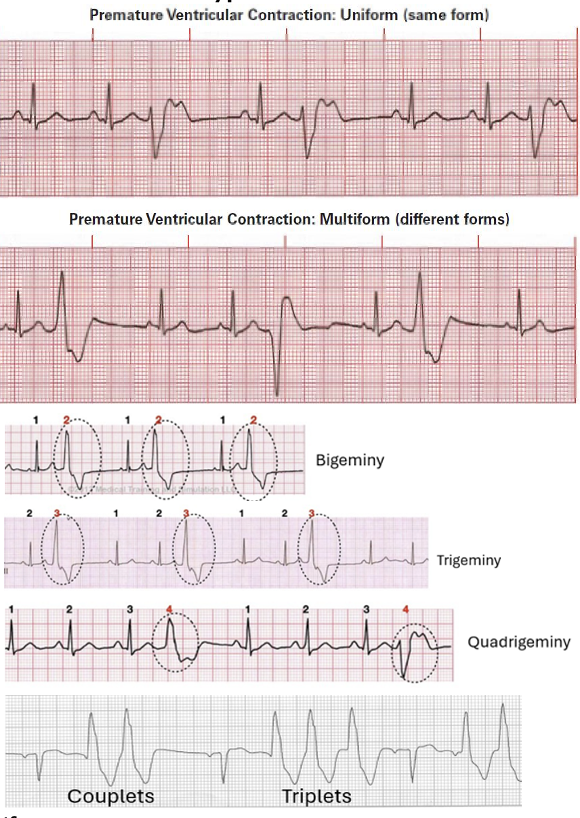
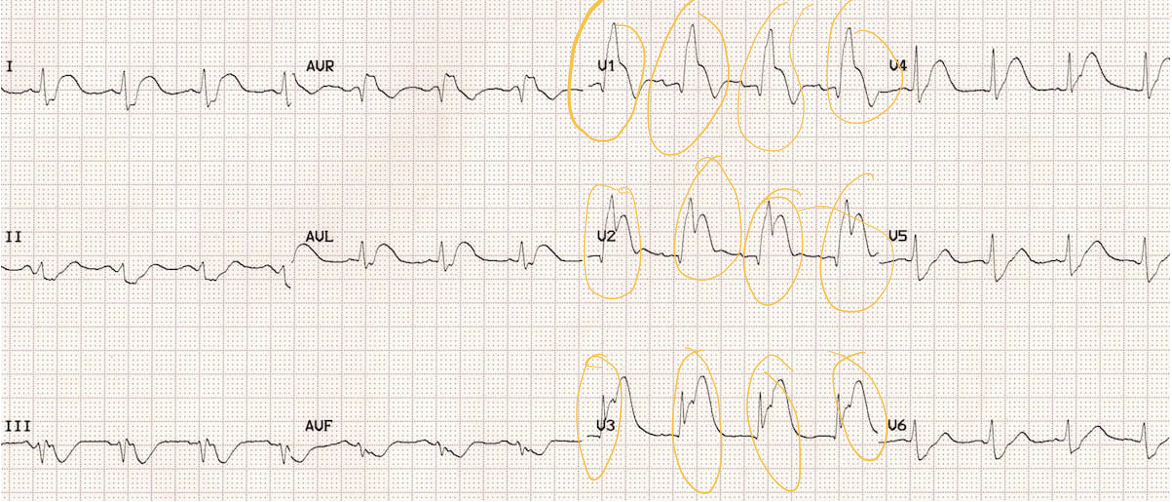
Characteristics and Subtypes of PVCs
Uniform
Multiform
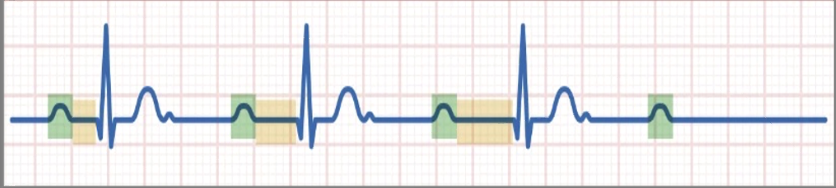
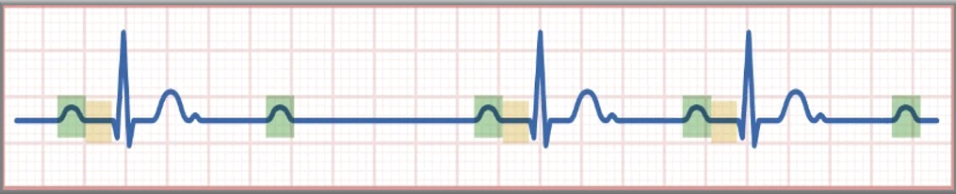
Bigeminy (1, 2; 1, 2; 1, 2)
Trigeminy (1, 2, 3; 1, 2, 3)
Quadrigeminy (1, 2, 3, 4; 1, 2, 3, 4)
Couplets
Triplets
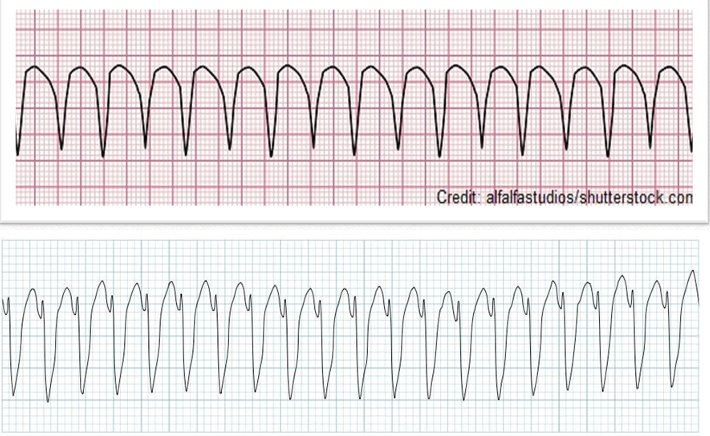
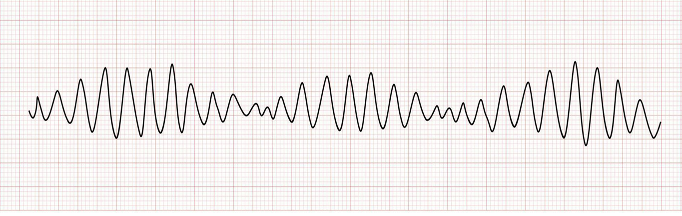
Ventricular Tachycardia (V-Tach): Criteria
Rate: Atrial: Depends on the underlying rhythm; Ventricular: 100 to 200 bpm
Rhythm: Usually regular
P Waves: N/A
P to QRS Ratio: N/A
PR Interval: N/A
QRS Complex: Greater than 0.12 seconds; wild, bizarre, and abnormal
**all are uniform
V-Tach: S/Sx & Causes
Signs & Symptoms:
May or may not have a pulse —SO ASSESS FOR A PULSE FIRST! #1
Hypotension
Dizziness/lightheadedness
Causes:
Ischemic heart disease/coronary artery disease (#1 cause)
Hypoxemia
Acid-base imbalance
Cardiomyopathy
Electrolyte imbalances
Valvular disease
Genetic abnormalities
QT prolongation
V-Tach: Treatments
Stable:
Patient is alert with a pulse.
Obtain a 12-lead ECG
Determine if sustained (> 3 seconds) or non-sustained.
Try a vagal maneuver—to try and kick them back into a normal rhythm.
If unresponsive to amiodarone, alternative drugs include procainamide, metoprolol, or sotalol.
First-line for wide complex V-tach:
Amiodarone 150 mg IV over 10 minutes.
Then 1 mg/min for the first 6 hours.
Followed by 0.5 mg/min for the next 18 hours.
Consider Life Vest, AICD (automatic internal cardiac-defibrillator), or synchronized cardioversion (shock).
**Adenosine may be considered only if the rhythm is regular and monomorphic**
Unstable:
Patient has lost consciousness and has no pulse.
Call a code and begin CPR.
Use an AED/defibrillator to deliver a shock immediately when available.
VT is a shockable rhythm and may not resolve spontaneously.
**If that AED/Defibrillator is readily available, the first choice is shock. If not, then CPR until you can get it**
***Follow ACLS (Advanced Cardiovascular Life Support) guidelines for medication administration during a code.
Polymorphic V-Tach or Torsades de Pointes: Criteria
Rate: Ventricular — 100 to 200 bpm
Rhythm: Looks like twisting points or peaks on the ECG
P Waves: N/A
P to QRS Ratio: N/A
PR Interval: N/A
QRS Complex: Bizarre, with fluctuations in amplitude
“Twisting of Pointes”
Torsades de Pointes: Causes & Common Treatments
Causes:
Similar to V-Tach and V-Fib
Usually associated with low magnesium levels**
Prolonged QT intervals (e.g., from amiodarone/procainamide)**
Common Treatments:
Correct the underlying issue(s)
IV magnesium sulfate 1 to 2 grams (first-line treatment)
Isoproterenol, Mexiletine
Atrial pacing (helps shorten QT interval)
Antiarrhythmics can be considered, but they are often ineffective or harmful
If stable: Implantable cardioverter defibrillator (ICD)
Prepare for cardioversion
If pulseless: CPR and defibrillation
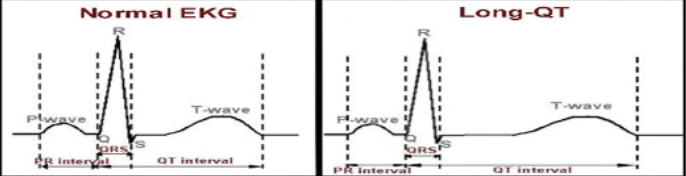
Long QT Syndrome (LQTS)
Normal QT Interval:
0.35 to 0.45 seconds
Genetic/Inherited Causes:
QT > 0.50 seconds
A common cause of cardiac arrest among young people
Often underdiagnosed
Genetic testing is available
Acquired Causes:
Drug-induced: Over 75 drugs can prolong the QT interval
Possible Contributors to Prolonged QT:
Electrolyte imbalance
Hypothermia
Structural heart disease
Female gender
Abnormal thyroid function
Signs & Symptoms:
Syncope
Seizures
Sudden death
Treatment:
Eliminate medications that may contribute
Potassium supplements
Implantable Cardiac Defibrillator (ICD)
Mexiletine (oral analog to Lidocaine)
Beta-blockers (Shorten the QT interval)
Ventricular Fibrillation (V-Fib): Criteria, Causes, & Symptoms
Criteria:
Rate: Chaotic
Rhythm: Chaotic
P Waves: Absent
P to QRS Ratio: Absent
PR Interval: Absent
QRS Complex: Absent
PULSELESS — ALWAYS
Causes:
Coronary Artery Disease (CAD) → Myocardial Infarction (MI)
Untreated or unsuccessfully treated V-Tach
Cardiomyopathy
Valvular heart disease
Acid-base and electrolyte abnormalities
Electrical shock
Symptoms:
Always pulseless!
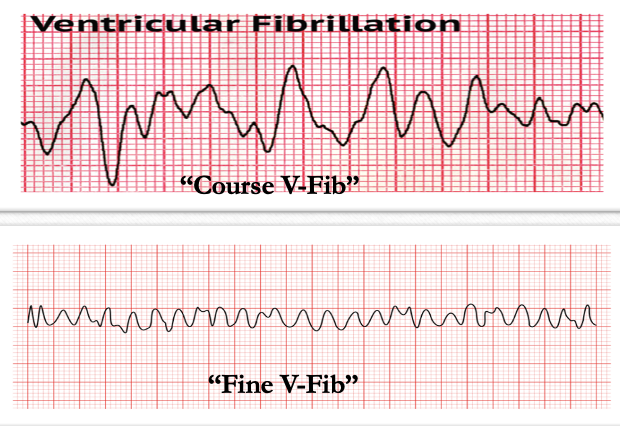
V-Fib: Treatments
Immediate Interventions:
No pulse / No respirations → Call a CODE!!!
Early and immediate defibrillation
Do not delay defibrillation
Perform high-quality CPR (30:2)
Medical/Pharmacological Management: ACLS meds
Epinephrine 1 mg IV push every 3 to 5 minutes
Amiodarone 300 mg initial IV bolus, followed by 150 mg (may substitute Lidocaine)
Post-Resuscitation Management:
Amiodarone or Lidocaine drip (follow-up)
Identify and treat reversible/underlying causes
Asystole: Criteria
Rate: No pulse
Rhythm: No rhythm (flatline)
P Waves: Absent
PR Interval: Not applicable
QRS Complex: Absent
Key Feature: NO PULSE! – Cardiac Arrest
**non-shockable rhythm

Pulseless Electrical Activity (PEA): Criteria
Rate: Varies
Rhythm: Varies
P Waves: Varies
P to QRS Ratio: Varies
PR Interval: Varies
QRS Complex: Varies
Key Feature: Electrical activity present, but no pulse!
**Looks like sinus rhythm on the monitor, but the patient has no pulse.
**Usually seen after coding a pt. for a while. (post-code)

Medical Management of Pulseless Cardiac Arrest: Mind Your H’s and T’s
H’s:
Hypovolemia
Hypoxia
Hydrogen ion (acidosis)
Hypo/Hyperkalemia
Hypothermia
T’s:
Tension pneumothorax
Tamponade, cardiac
Thrombosis (coronary)
Thrombosis (pulmonary)
**Treating the underlying causes
Conduction Defects
Left and Right Bundle Branch Blocks
First-Degree AV Block
Second-Degree AV Block, Mobitz Type 1 (Wenckebach)
Second-Degree AV Block, Mobitz Type 2
Third-Degree (Complete)
Bundle Branch Blocks
What is Happening:
First division of the ventricular conduction after the bundle of His.
A delay or blockage of the electrical impulses, resulting in the heart pumping blood less efficiently.
Cause:
LBBB—MI, HTN, myocarditis, cardiomyopathy
RBBB—PE, MI, congenital heart defects, pulmonary HTN, myocarditis
Signs & Symptoms:
Usually asymptomatic
Dizziness, syncope
Treatment:
Usually not needed if asymptomatic
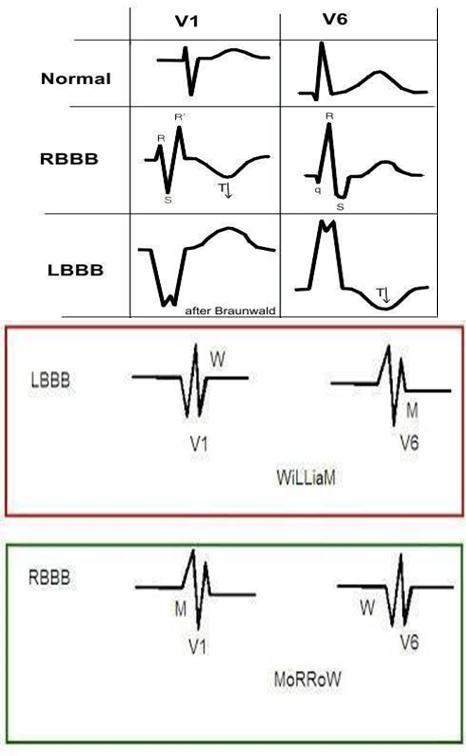
Mnemonic: WilliaM MorroW—You need a 12 lead ECG looking at lead V1 and V6!
LBBB: V1 = W; V6 = M—90% are this!
RBBB: V1 = M; V6 = W
**William has L and Morrow has R
Atrioventricular (AV) Blocks
The SIGNAL is DELAYED or BLOCKED WHEN MOVING from the ARTIA to the VENTRICLES.
Caused by:
Lev’s disease
Ischemic heart disease
Cardiomyopathy
Myocarditis
Three types:
1st degree
2nd degree
3rd degree
First Degree AV Block: Criteria
Looks like NSR except with a prolonged PR interval: greater than 0.20 seconds.
Constant PR interval for each beat.
Usually asymptomatic and only needs monitoring.
If symptomatic, treat with atropine.

Second Degree AV Block—Mobitz Type 1 (Wenckeback): Criteria + Treatment
PR Interval: Steady lengthening (slowly gets further from the QRS complex until the QRS complex disappears).
QRS Complex: Dropped or blocked.
PP Interval: Regular.
RR Interval: Irregular.
QRS: Normal.
Decreased cardiac output may occur.
Treatment: If symptomatic, treat with atropine.
Second Degree AV Block—Mobitz Type II: Criteria + Treatment
PR Interval: Fixed.
PP Interval: Fixed.
Occasional P wave not followed by QRS.
Essentially, the PR interval is constant, and then the QRS is dropped.
Typically unstable and needs treatment.
Treatment: Atropine or pacing.
Third-Degree AV Block (Complete Heart Block): Criteria + Treatment
Atria and ventricles beat independently of each other.
P waves are not associated with QRS complexes.
Treatment:
Atropine can be given but is usually ineffective.
Transcutaneous, transvenous, or implanted permanent pacemaker.

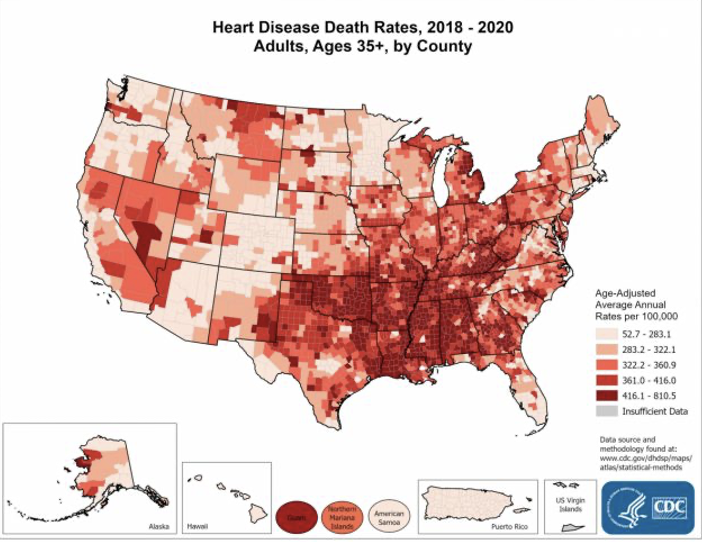
ACS/MI: Prevalence
Per the CDC:
Approximately 695,000 people died from cardiac disease in 2021 (1 in 5 deaths).
Over 800,000 people had heart attacks (1 attack every 40 seconds).
CAD cost in the U.S. is about $239.9 billion in healthcare costs, services, and lost wages.
About 1 in 5 (20%) of all heart attacks are “silent.”
Risk Factors for CAD
Smoking**
Hypertension
Diabetes
Hyperlipidemia
Obesity
Inactivity
Family history
In-patients are highly susceptible to cardiac events. Why do you think this is?
High concentration of high-risk populations.
Metabolic syndrome (hyperlipidemia, hypertension, diabetes, and obesity)
Physical/emotional stress
Increased bed rest/immobility
Medication changes
ACS Cascade
Ischemia → Injury → Necrosis
Stable Angina
Character of Pain: Exertional pain
Pattern: Crescendo-Decrescendo
Relievers: Responds to NTG
Enzymes: Normal
ECG: Often Normal
Unstable Angina
Character of Pain: Rest pain
Pattern: Crescendo
Relievers: No NTG effect
Enzymes: Normal
ECG: Often ST depression
NSTEMI
Character of Pain: Rest pain
Pattern: Crescendo
Relievers: No NTG effect
Enzymes: Elevated
ECG: No ST segment elevation
STEMI
Character of Pain: Rest pain
Pattern: Crescendo
Relievers: No NTG effect
Enzymes: Elevated
ECG: ST segment elevation
30 minutes
How long does it take to progress from the onset of ischemia to irreversible cardiac tissue necrosis?
Typical MI Symptoms
Chest pain (crushing, squeezing, pressure, heaviness)
Pain that radiates to jaw, shoulders, or back.
Shortness of breath
Atypical MI Symptoms (silent MIs)
Dizziness/lightheadedness/syncope
Nausea/vomiting
Diaphoresis/pallor
Sudden weakness/tiredness
women, elderly, diabetics
20% of MIs do NOT present with typical symptoms, particularly in _____, _______, and _________. Treat it like an MI until proven otherwise.
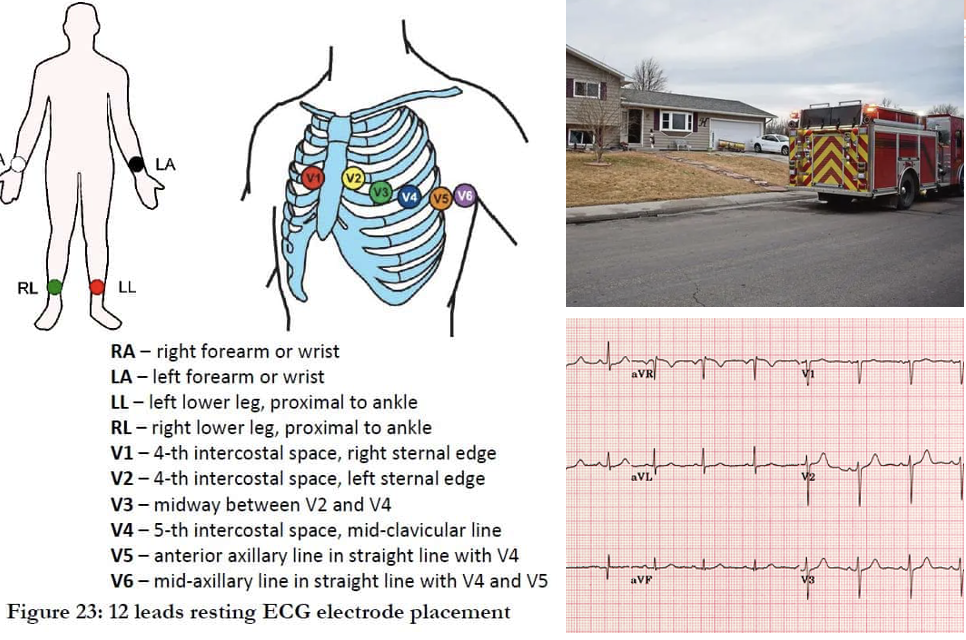
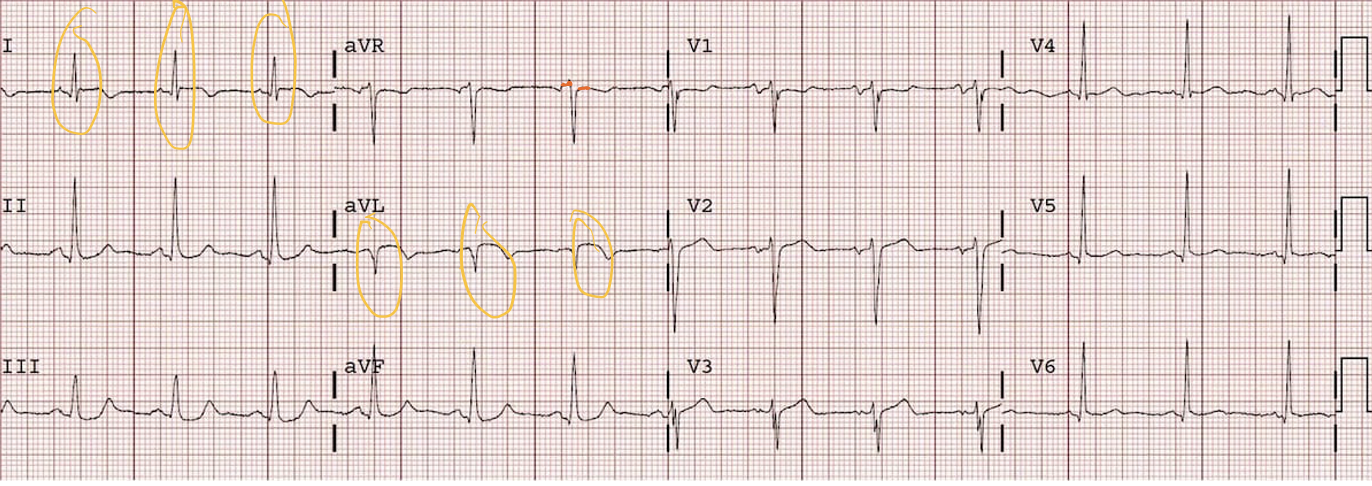
12-Lead ECG
10 leads actually means 12 views.
The views look at the heart’s electrical activity from multiple angles.
Changes must be noted in at least two contiguous leads (looking at the same part of the heart) to be considered clinically significant.
Which Leads Look Where? (picture)
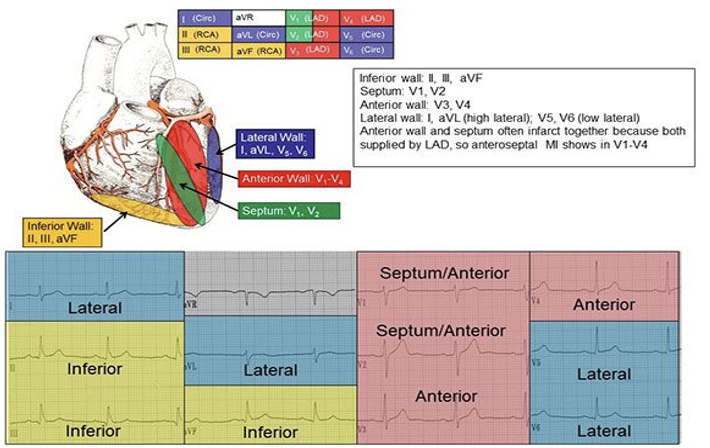
Which leads look at the lateral wall of the heart?
Leads: I, AVL, V5, and V6
Which leads look at the inferior wall of the heart?
Leads: II, III, and AVF
Which leads look at the septum/anterior wall of the heart?
Leads: V1 and V2
Which leads look at the just the anterior wall of the heart?
Leads: V3 and V4
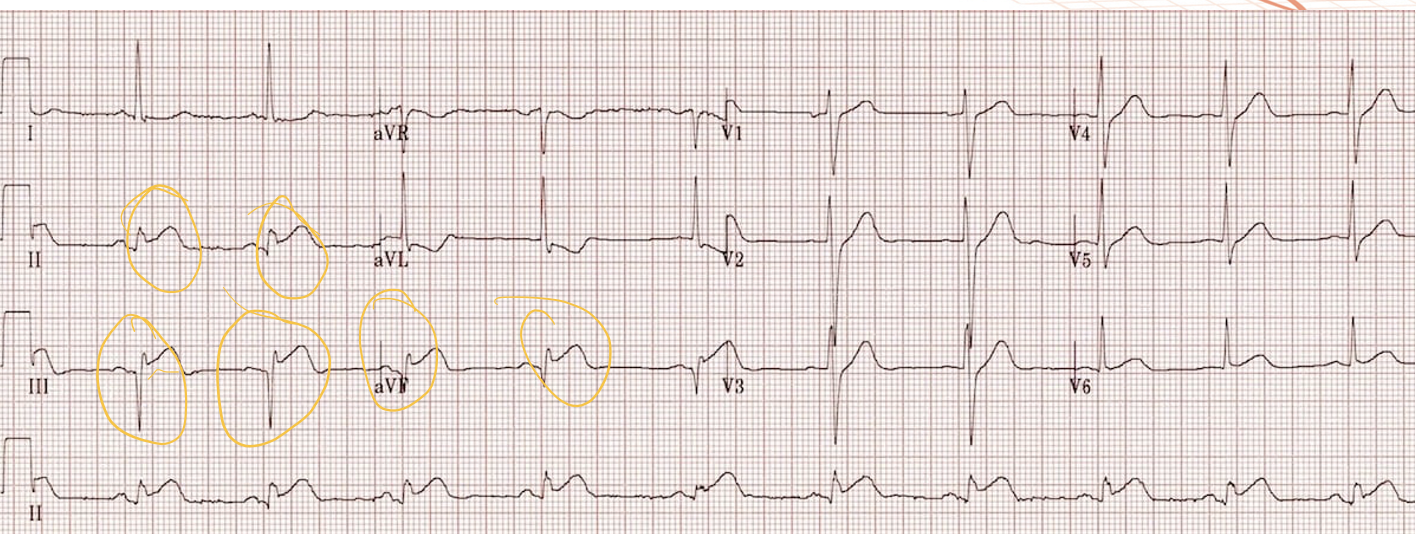
When looking for ST segment elevation, what are the three areas you look at?
PR segment
J point
ST segment
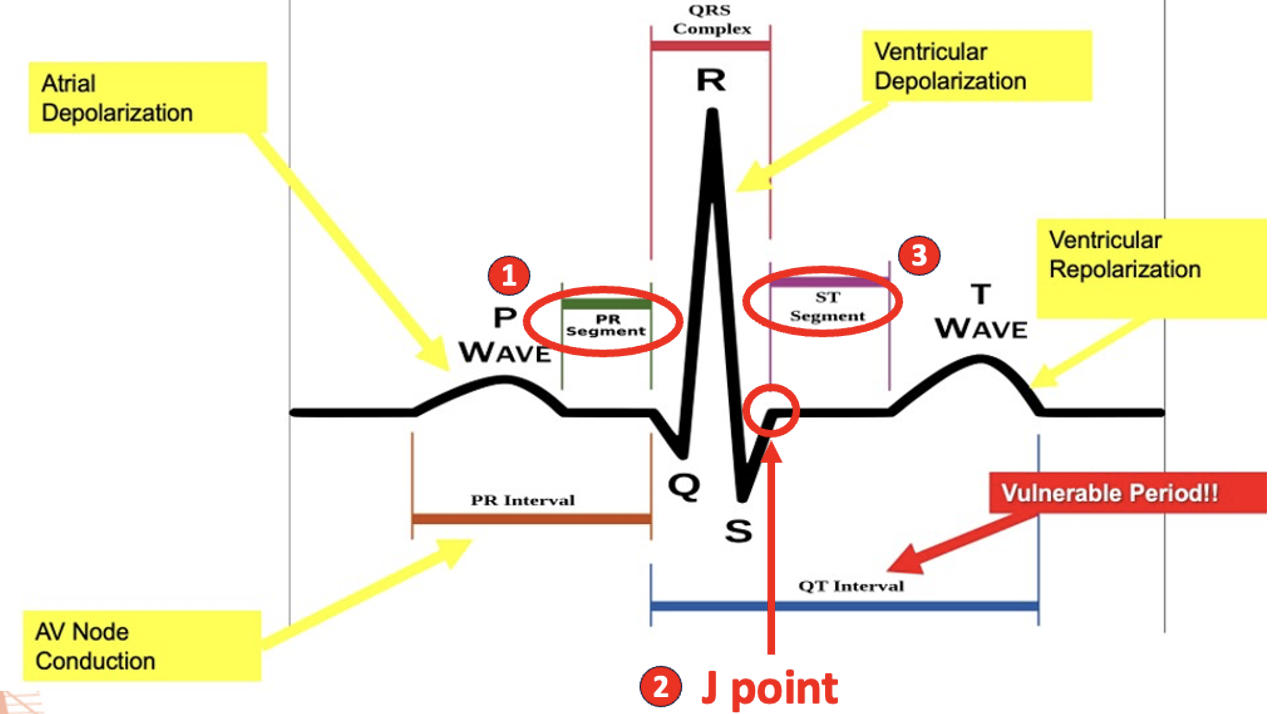
one small square, ABOVE
If the J point falls at least ___ _____ ______ (1mm) _____ your line, then you have ST elevation. If not, then you don’t have ST elevation.
Anteroseptal MI
Lateral MI
Inferior MI
MI Mimics
Example:
Left Bundle Branch Block (most common)
Left Ventricular Hypertrophy (LVH)
Early Repolarization
Right Bundle Branch Block
Changes (ST elevation are usually in all the leads, which gives it away that it’s not an MI.
full thickness
A STEMI indicates ____ _________ (inside and out) damage of the heart muscle (tissue death).
partial thickness
A NSTEMI indicates _______ _________ damage of the heart muscle. Electrical impulses show through the healthy sliver of tissue.
Cardiac Enzyme: Troponin T
More hospital systems have switched to using 5th generation Troponin T tests, which are more sensitive and report results in whole numbers.
If labs are drawn early when a patient shows symptoms of an MI, troponin levels may still be normal because it can take time for the heart tissue to release enough troponin into the bloodstream.
If symptoms just began, the troponin may not yet be detectable and labs may need to be repeated later.
“Normal” Range for Troponin T (5th Gen)
Males: < 15 ng/L
Females: < 10 ng/L
99th Percentile for Troponin T (5th Gen)
Males: 22 ng/L
Females: 14 ng/L
Critical Value for Troponin T (5th Gen)
> 53 ng/L
10 minutes
If a patient starts complaining of chest pain or other symptoms that could indicate a heart attack, you have __ _______ to obtain a 12-lead ECG!
Nursing Interventions: ACS/MI
Obtain 12-lead ECG within 10 minutes at most!:
Leave machine attached.
Call Rapid Response Team (RRT):
Get ECG to interventional cardiologist.
Assess your patient:
Baseline vital signs
Ensure patent IV
If STEMI is confirmed:
Prepare for cath lab:
Place defibrillator pads on patient
Shave groin and wrist sites (femoral/radial)
Administer meds per physician orders
Prepare for transport
If STEMI is ruled out:
Administer meds per physician order.
ACS/MI: MONA—Pharmacological Nursing Interventions
Morphine:
Given for pain, but no mortality benefit.
Oxygen:
Usually only if pt.’s SpO2 is < 90%.
Nitroglycerin:
Still used in presence of persistent ischemia.
Aspirin:
23% mortality reduction.
ACS/MI: Other Phamracological Interventions
Drugs of Choice that Improves Mortality:
Fibrinolytics—if symptoms are <12 hours and prompt PCI is unavailable.
Anticoagulants—anti-platelet.
P2Y12 Inhibitors—prevent further platelet aggregation, preventing clots from getting bigger.
Glycol. IIb/IIa Inhibitors—ONLY if the patient is unable to receive a P2Y12 Inhibitor.
Beta Blockers—lowers HR and reduces workload of heart; be cautious and obtain baseline vitals.
RAAS Inhibitors—lowers systemic vascular resistance/BP.
Statins—given after the fact, to lower cholesterol.
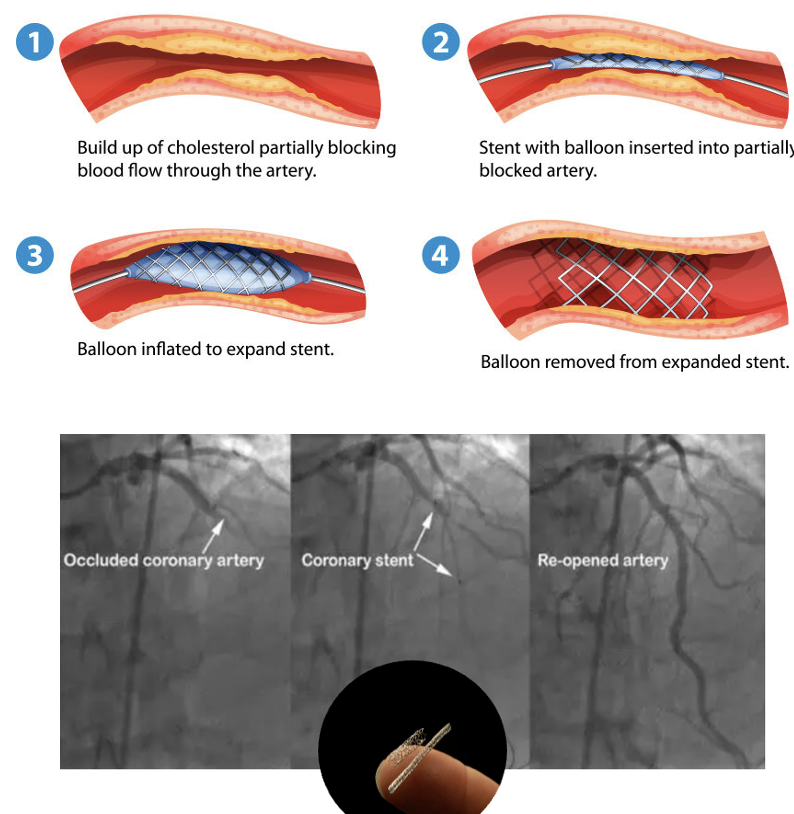
PCI: Stent with Balloon Angioplasty
A procedure that leaves a permanent wire mesh within a coronary artery to restore flow to cardiac tissue.
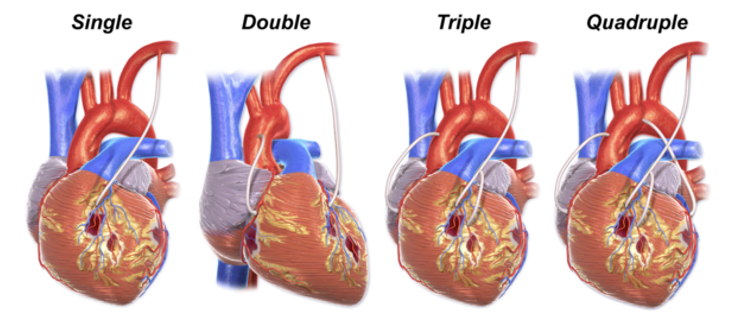
Coronary Artery Bypass Graft (CABG)
When a PCI isn’t possible, blood vessels from other parts of the body can serve as conduits for blood to perfuse the heart.
They include the internal thoracic or mammary artery (ITA or IMA), saphenous vein (SV), and radial artery (RA).
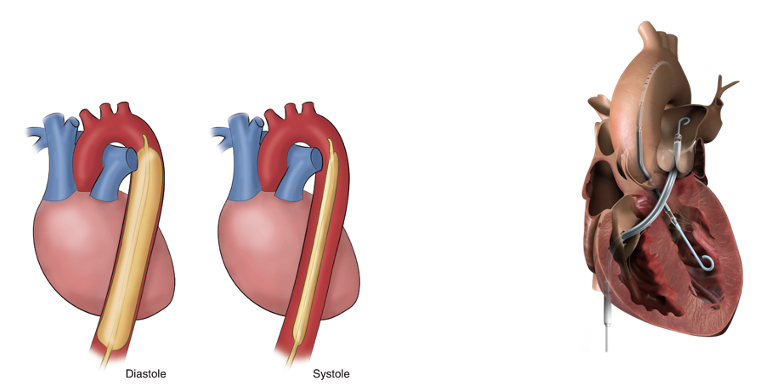
Intra-Aortic Balloon Pump & Impella Pump
These are temporary, in-hospital measures until definitive treatment can be completed. (bridge treatments)
Both of these interventions are in place for less than 30 days.
It buys the patient time until a PCI or CABG can be performed.
Intra-Aortic: it inflates and blocks the aorta during diastole and then during systole when the heart contracts, it deflates to let the blood pass. (improves injection fraction)
Impella: “outdoor motor”—it is fed up into the ventricle and it anchors itself in there. It helps push the blood out with every beat.
Cardiac Rehabilitation
Recovery can generally take anywhere from 4 to 12 weeks.
Cardiac rehab teams usually consist of physicians, nurses, exercise physiologists, dietitians, and clinical psychologists.
Patient gradually increased physical activity over a couple of weeks, starting with several shot walks per day and increasing in length.
Services can include physical exams, exercise sessions, health classes, therapy groups, dietary consults, and even grocery store tours.
ACS/MI: Patient Education
Lifestyle Changes:
Smoking Cessation
Dietary changes (low fat/cholesterol)
Attend cardiac rehab and follow up cardiology appointments
When to call their physician or 9-1-1
Medication Compliance and Potential Side Effects:
Asprin
Antiplatelets
Beta blockers
RAAS Inhibitors (ACE Inhibitors, ARBs, etc.)
Statins
Nitroglycerin (SL spray or tablets)
Keep in a cool, dry, and dark place (sensitive to light).
Only good for 3 to 5 months → replace.
Sit down when taking it because it significantly drops BP.
Take one every 3 to 5 minutes with of max of 3 doses.