Lec 01: Intro to pain
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Pain Theories
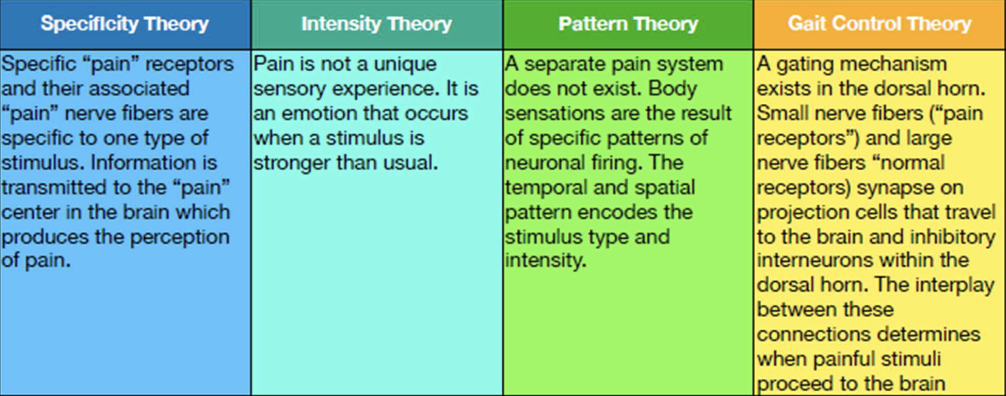
what is specificity theory?
specific “pain” receptors and their associated “pain” nerve fibers are specific to one type of stimulus. Information is transmitted to the “pain” center in the brain which produces the perception of pain
what is intensity theory?
pain is not a unique sensory experience. it is an emotion that occurs when a stimulus is stronger than usual
what is pattern theory?
a separate pain system does not exist. body sensations are the result of specific patterns of neuronal firing. the temporal and spatial pattern encodes the stimulus type and intensity
what is gait control theory?
a gaiting mechanism exists in the dorsal horn. small nerve fibers (“pain receptors”) and large nerve fibers “normalreceptors) synapse on projection cells that travel to the brain and inhibitory interneurons within the dorsal horn. the interplay between these connections determines when painful stimuli proceed to the brain.

what is gate control theory?
1. When no input comes in, the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed).
2. Normal somatosensory input (large-fiber stimulation). Both the inhibitory neuron and the projection neuron are stimulated, but the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed).
3. Nociception input (small-fiber stimulation). Inactivates the inhibitory neuron, and the projection neuron sends signals to the brain (gate is open)
what is step 1 of Gate Control Theory?
When no input comes in, the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed)
what is step 2 of Gate Control Theory?
Normal somatosensory input (large-fiber stimulation). Both the inhibitory neuron and the
projection neuron are stimulated, but the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed).
what is step 3 of Gate Control Theory?
Nociception input (small-fiber stimulation). Inactivates the inhibitory neuron, and the projection neuron sends signals to the brain (gate is open).
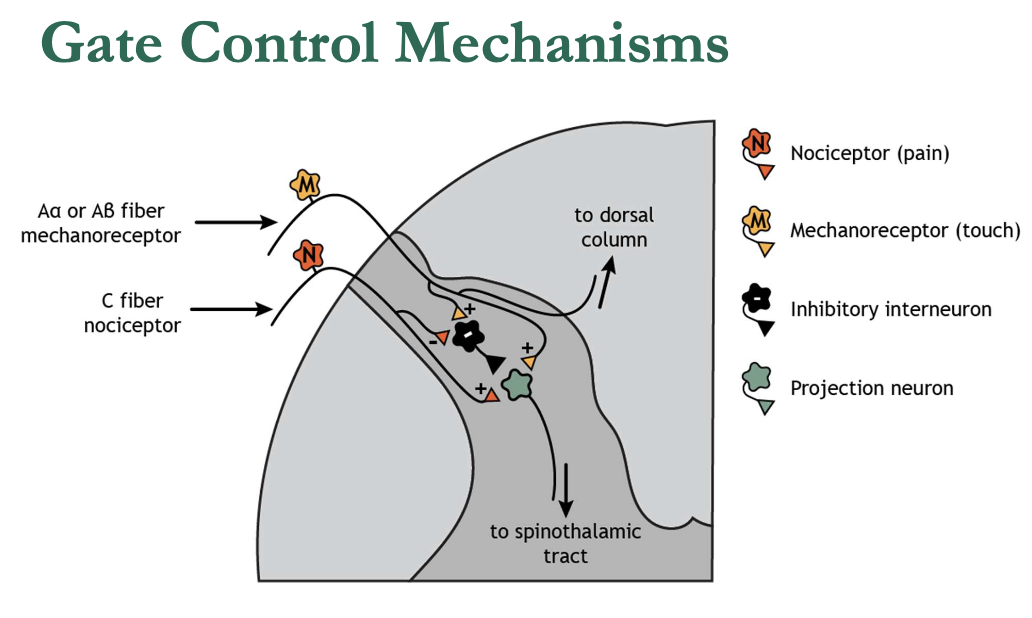
gate control mechanisms
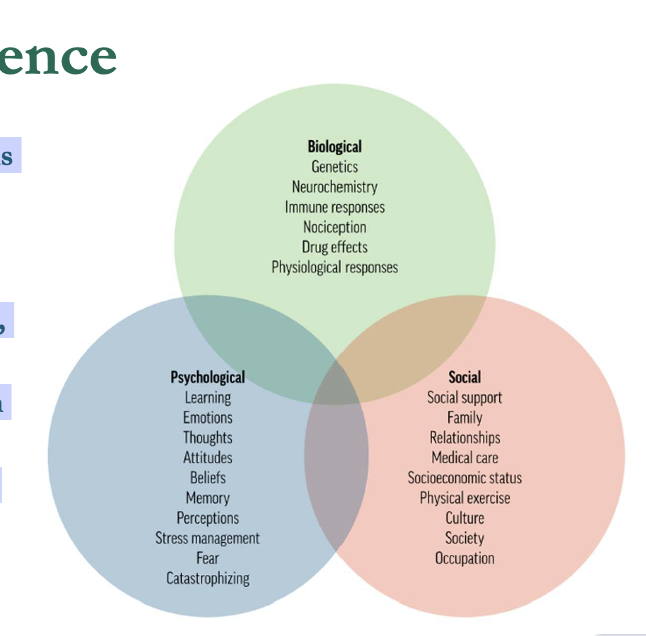
• Developed in response to limitations of the biomedical model
• Recognizes pain as a multidimensional experience
• Integrates biological, psychological, and social factors
• Emphasizes individual variability in pain perception
• Supports interdisciplinary care and patient-centered approaches
modern pain science
what is definition of pain?
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”
Pain is always a personal experience
- Influenced to varying degrees by biological, psychological, and social factors.
Pain and nociception are different phenomena
Pain cannot be inferred solely from activity in sensory neurons.
Individuals learn the concept of pain through life experiences
Pain is shaped by personal history and context.
A person’s report of pain should be respected
Pain is subjective and valid regardless of objective findings.
Pain usually serves an adaptive role
But it may have adverse effects on function and social/psychological well-being.
Verbal description is only one way to express pain
Inability to communicate does not negate the possibility of experiencing pain (applies to humans and nonhuman animals)
6 Key Points (IASP)
what is Pain is always a personal experience?
Influenced to varying degrees by biological, psychological, and social factors
what is Pain and nociception are different phenomena?
Pain cannot be inferred solely from activity in sensory neurons.
what is Individuals learn the concept of pain through life experiences?
Pain is shaped by personal history and context.
what is A person’s report of pain should be respected?
Pain is subjective and valid regardless of objective findings.
what is Pain usually serves an adaptive role?
But it may have adverse effects on function and social/psychological well-being.
what is Verbal description is only one way to express pain?
Inability to communicate does not negate the possibility of experiencing pain (applies to humans and nonhuman animals).
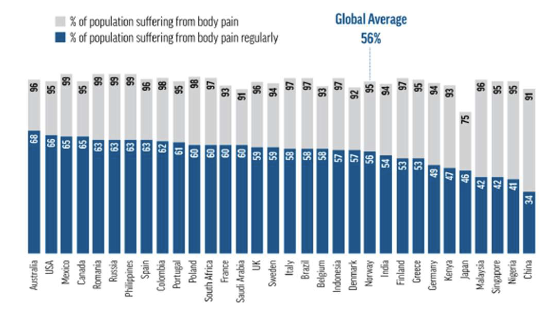
Pain is recognized as a global health crisis by the United Nations and the World Health Organization (WHO).
Approximately 56% of people worldwide suffer from regular body pain on a weekly basis.
Persistent pain affects daily activities, social life, and work productivity across populations
Pain Epidemic – Global Overview
Pain is recognized as a global health crisis by the
United Nations and the World Health Organization (WHO).
The Institute of Medicine (IOM) estimates:
116 million American adults are affected by persistent pain conditions.
126.1 million adults report pain over a 3-month period.
25.3 million suffer from daily persistent pain
The economic burden is staggering:
Estimated $560–$635 billion annually spent on pain management.
$61 billion/year lost in productivity due to common pain conditions.
Pain costs exceed those of heart disease, cancer, and diabetes combined
Americans account for 5% of the worlds population, but consume 80% of the global opioid supply.
In 2012, 259 million prescriptions for opioids were written.
Over 100 deaths per day are attributed to prescription pain medications
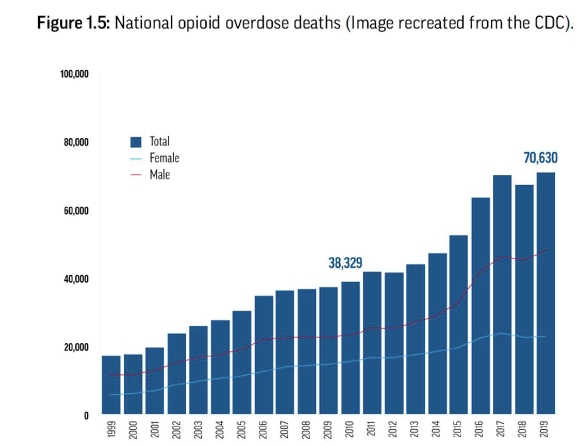
Opioid Epidemic
Four key “must-know”:
misleading origins of the Crisis
High risk of Long term use
early exposure risks
COVID-19 Amplified the Crisis
what is misleading Origins of the Crisis?
– A one-paragraph letter by Porter and Jick (1980) in the New England Journal of Medicine claimed addiction was rare in hospitalized patients receiving narcotics.
– This letter was misinterpreted and misused by pharmaceutical companies
what is high risk of long term use?
– 13.5% of patients who take opioids for 8 consecutive days will still be using them one year later.
– If a patient takes opioids for 31 days or more, the chance of continued use after one year rises to 30%
what is early exposure risks?
– Routine opioid prescriptions for oral health care and musculoskeletal injuries—especially from dentists and emergency departments—can set patients up for long-term use and addiction.
what is COVID-19 amplified the Crisis?
– The COVID-19 pandemic has led to a significant increase in opioid use.
– Factors include increased stress, isolation, reduced access to non-pharmacological care, and disrupted healthcare systems
The U.S. reflects the global struggle with pain but also highlights unique challenges:
– High reliance on pharmacological interventions (e.g., opioids).
– Disparities in pain treatment across age, gender, race, and socioeconomic status.
– Growing need for multidisciplinary and biopsychosocial approaches to pain care.
The global data underscores the importance of?
education, advocacy, and reform in pain management—especially for physical therapists
who play a key role in non-pharmacological interventions.
what is impact on providers?
lack of training
burnout
what is lack of training?
• Physical therapists often lack formal education in modern pain science
• This gap leads to clinical uncertainty, reduced confidence, and emotional exhaustion
what is burnout?
• Treating patients with persistent pain is emotionally and professionally demanding.
• Many clinicians report feeling underprepared to manage chronic pain effectively.
• Outdated pain models and ineffective treatment strategies contribute to frustration and
fatigue.
• Simply withdrawing from clinical work does not reduce burnout—reengaging in meaningful practice is more effective