Unit 5: Obesity Objectives
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
80 Terms
occurs when there is an increased energy storage resulting from an imbalance between energy intake and energy expenditure overtime.
genetics (contributes to 40-70% of the variance in BMI)
environmental factors (access to food, sedentary lifestyle, high fat foods)
medical conditions (Cushing syndrome, growth hormone deficiency, insulinoma, psychiatric disorders - depression, binge eating, schizophrenia, genetic syndromes)
medications (anticonvulsants, antidepressants, antipsychotics, hormones)
Describe the etiology (causes) of obesity.
involves numerous factors that regulate appetite and energy balance; disturbance of these homeostatic functions results in an imbalance between energy intake and energy expenditure
appetite
the dysregulation of neural network involving hypothalamus, limbic system, brainstem, hippocampus, elements of the cortex and pituitary gland - controls appetite, reward, and energy balance
normal communication between these neural networks breaks down to increased reward-seeking behavior for palatable foods and weakened inhibitory control over eating
many neurotransmitters and neuropeptides have been identified that can stimulate or inhibit brain’s appetite network and thereby affect total caloric intake
Describe the pathophysiology (what goes wrong in our body) of obesity.
HTN
T2DM
CVD
NAFLD or MAFLD/NASH
OA (osteoarthritis)
Cancer
Depression
Identify comorbid disease states that are commonly associated with obesity.
HTN
dyslipidemia
CHD
Type 2 DM
sleep apnea
increased WC (waist circumference)
Identify risk factors that are associated with obesity in the US.
the number of calories your body burns while at rest includes digesting a meal and waking up
includes BMR
Define resting energy expenditure.
the minimum amount of energy required by the body to maintain essential functions as rest, such as breathing, circulation, and cell growth.
portion of RMR
Define basal metabolic rate.
REE:
The minimum amount of energy required to maintain bodily functions at rest, including breathing, circulation, and cell growth.
BMR:
A more specific measurement of REE that is calculated under strict conditions, such as after 12 hours of fasting and 8 hours of sleep
Describe the relationship between resting energy expenditure and basal metabolic rate.
Neurotransmitters
Dopamine - brain (wanting food)
Serotonin - GI tract (anorexigenic (appetite-suppressing) effects, modulating satiety and limiting food intake)
GABA - the main inhibitory neurotransmitter in the CNS and is heavily involved in feeding behavior
Opioids: increase the consumption of highly palatable foods and are involved in the rewarding properties of eating. They are released after palatable food intake and act on opioid receptors in the striatum
Peptide Hormones
Gherlin: Often called the "hunger hormone," ghrelin is the only known circulating gut peptide that stimulates appetite.
produced primarily in the stomach
its levels increase before meals, stimulating the brain's hunger centers.
Leptin: Secreted by adipose (fat) tissue, leptin is a long-term signal of energy sufficiency.
It suppresses appetite by acting on the hypothalamus to decrease the release of hunger-promoting peptides
CCK: short-term satiety peptide released by the small intestine in response to meal intake, especially fat and protein.
It slows gastric emptying, signals satiety, and decreases meal size. Its effects are mediated via the vagus nerve and its receptors in the brain.
GLP-1 RA: anorexigenic (appetite-suppressing) peptide released from the intestine in response to food.
promotes satiety, slows gastric emptying, and enhances glucose-stimulated insulin release. GLP-1 receptor agonists are used as treatments for type 2 diabetes and obesity.
Receptors
Hypothalamic receptors: The arcuate nucleus of the hypothalamus is a crucial site for integrating signals related to hunger and satiety, with many key receptors located here, such as LEPR and GHSR.
Reward system receptors: Dopamine and opioid receptors in the mesolimbic system are involved in the rewarding aspect of food intake.
Gut-brain axis receptors: Receptors on the vagus nerve, such as for CCK and GLP-1, relay signals from the gastrointestinal tract to the brain.
Nutrient-sensing receptors: Taste receptors in the gut and on the tongue can also influence peptide release and food intake.
State neurotransmitters, peptides and receptors associated with food intake.
BMI (body mass index) is a clinical measure of excess body fat that provides an assessment of total body fat better than weight alone
is the practical method of defining obesity
independent predictor of obesity related disease risk
most commonly used index of overweight and obesity
Describe the diagnosis of obesity.
BMI = body weight (kg) divided by the height of (in meters squared)
Calculate BMI
1. Calculate ideal body weight and adjusted body weight. (1c)
Men less than or equal to 40 inches waist circumference - increased risk of obesity
Women 35 inches waist circumference - increased risk of obesity
Men greater than 40 inches is considered abdominal obesity - high risk
Women greater than 35 inches is considered abdominal obesity - high risk
Interpret waist circumference.
pulmonary disease (sleep apnea, abnormal function, hypoventilation)
liver disease (steatosis, steatohepatitis, cirrhosis)
gall bladder disease
osteoarthritis
cataracts
stroke, heart disease
cancer (breast, colon, kidney, prostate, uterus, esophagus, cervix, pancreas)
diabetes, pancreatitis, gout
death (1 in 5 deaths linked to being overweight or obese)
Describe common complications of obesity.
Lifestyle modifications
5% - 10% reduction in initial body weight over 3-6 months is a common goal
weight loss medications
orlistat (Alli, Xenical) - leads to about 10% body weight loss after 1 year
Phentermine-Topiramate (Qsymia) - approximately >10% of their body weight after 1 year
GLP-1 RA
Semaglutide (Wegovy) - 15%
Tirzepatide (Zepbound) - up to a 15.7% weight reduction
bariatric surgery - patients maintain an average loss of 50% or more of their excess body weight
Identify three general treatment modalities for obesity and the general weight loss anticipated with each treatment option.
Set appropriate goals of therapy in treating an obese patient.
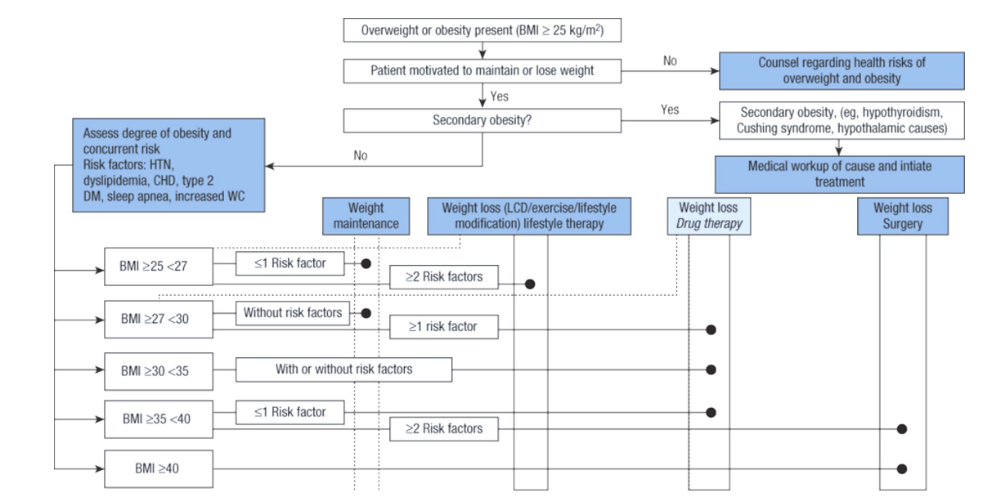
Given a patient with obesity in a case, determine the best general treatment modality.
nonpharmacological therapy - (recommended as first line therapy)
reduced caloric intake
increased physical activity
behavioral modification
Describe the lifestyle modifications for obesity.
glucagon-like peptide-1 (GLP-1) receptor agonists
semaglutide (Wegovy), liraglutide (Saxenda)
glucose-dependent insulinotropic polypeptide (GIP)/glucagon-like peptide (GLP-1) receptor agonist
tirzepatide (Zepbound)
opioid antagonist/dopamine and norepinephrine reuptake inhibitor
naltrexone/bupropion ER (Contrave)
lipase inhibitor
orlistat (Alli - OTC; Xenical - RX)
sympathomimetic
phentermine (Adipex-P; Lomaira)
sympathomimetic/antiepileptic
phentermine/topiramate ER (Qsymia)
Name the drug classes utilized in the treatment of obesity.
Describe the relationship between the mechanism of action of all obesity drug classes and the pathophysiology of the disease.
Identify common adverse drug effects of each of the obesity class of medications.
Determine how the mechanism of action for the drug classes utilized in obesity contributes to the efficacy and safety of the classes.
Identify monitoring parameters for the drug classes utilized in obesity management based on their mechanism of action.
Using the obesity-focused history, determine appropriate questions for interviewing a patient with obesity to gather subjective information.
Given a role play scenario, gather a detailed eating history in a patient who is overweight/obese.
men less than or equal to 40 inches - increased risk
women 35 inches - increased risk
men greater than 40 inches - high risk
women greater than 35 inches - high risk
Define what is considered high risk for the waist circumference
Define the waist-to-hip ratio that is considered at-risk
reduced caloric intake
increased physical activity
behavioral modification
Describe the lifestyle modifications for obesity
Discuss recommended goals for weight loss to aid in improvement in overall health and comorbid conditions
Review dietary recommendations that aid in weight reduction
men: 1500-1800 per day
women: 1200-1500 per day
Distinguish between daily caloric recommendations for men and women
decrease calories by 500-750 calories / day (30%)
Identify the daily caloric deficit that should be targeted to aid in weight reduction
8% after 6 months
identify the appropriate rate of weight loss
to help augment or maintain weight loss you need 200-300 min/wk of moderate intensity physical activity plus muscle strengthening at least 2 days/wk
minimize weight gain after a year
to stay healthy you need 150 min/wk of moderate intensity physical activity plus muscle strengthening at least 2 days/wk
with 10 minute intervals for heart health
Goal is 30 minutes/day for most days of the week
Discuss recommended physical activity goals for weight reduction and cardiovascular health
Increase aerobic activity
Goal is greater than or equal to 150 min/week of moderate intensity or 75 min/wk of vigorous intensity
Need to do in at least 10 min intervals for heart health
PLUS muscle strengthening activities at least 2 days/week
Increase activity to 200-300 min/week
Help augment or maintain weight loss
Minimize weight regain (> 1 year)
PLUS muscle strengthening activities at least 2 days/week
Goal: 30 minutes/day, most days of the week
Describe the weekly recommended amount of physical activity
Moderate intensity and vigorous intensity
Moderate intensity
aerobic activity at least 150 minutes a week and at least 2 days/week of muscle strength training
vigorous intensity
Describe the intensity of physical activity that is recommended
BMI = weight (kg)/height (m squared) or [weight (lbs)/height (inches squared)] x 703
BMI less than 18.5 - underweight
BMI 18.5 - 24.9 - normal
BMI 25 - 29.9 - overweight
BMI 30 - 34.9 - Class I Obesity
BMI 35 - 39.9 - Class II Obesity
BMI greater than or equal to 40 - Class III Obesity
calculate and interpret a BMI
Identify when a patient is adherent or non-adherent to therapy using subjective and/or objective information
1. Describe how evidence-based techniques lead to a determination of patient understanding (52, 142)
Physical consequences
cardiovascular disease
Type 2 diabetes
Musculoskeletal disorders
Respiratory problems
Kidney/Gallbladder disease
Mental consequences
depression/anxiety
cognitive decline
Other
increased healthcare cost
reduced life expectancy
Given a patient scenario with an increased weight, elevated BMI, and high waist circumference, counsel a patient regarding two consequences of obesity. (
reducing caloric intake
increasing physical activity
managing behavioral situations (managing stress/depression & improve sleep)
Given a patient with obesity, counsel a patient regarding three lifestyle modifications they should utilize to help with weight management
healthy weight loss is 5-10% over 6 months
1-2 pounds per week
1. Given a patient with obesity, counsel a patient regarding what healthy weight loss is. (98)
checks for understanding by asking person to repeat back key information (dosing regimen, adverse effects, what to do about missed doses)
1. Demonstrate teach-back method for assessing patient understanding. (142)
first person strengths: nonjudgmental, unbiased, caring, free from stigma; places an emphasis on the person as an individual instead of the disease
she has diabetes, she has obesity
strengths based language: improves communication and motivation; fosters hope and collaboration
increased BMI (fat), weight management (excess fat), unhealthy weight (large size), carrying higher weight (obese), eating habits (diet), physical activity (exercise)
Given examples of communication with a person carrying extra weight, identify examples of words and language that either violate or are consistent with person-first or strengths-based language.
the extent to which a person’s behavior - taking medications, following a diet, and/or executing lifestyle changes - corresponds with agreed recommendations from a healthcare provider
1. Define adherence. (40, 41)
primary non-adherence
not filling a new RX
30% of newly prescribed medications are never picked up at the pharmacy
partial non-adherence
missing 20% or less of prescribed doses
repeat non-adherence
consistently missing >20% of prescribed doses
persistence
duration of time from start of therapy until discontinuation
1. Differentiate between types of nonadherence. (40, 41)
compliance: following instructions (making a recipe one time); patients are passive or obedient participants in the decision to take medications
adherence: active and engaged decision to follow plan (making recipe over and over again)
80% is considered “adherence” in many research studies; 95% is critical for HIV
1. Differentiate between the terms adherence and compliance. (40, 41)
subjective vs objective measures
subjective: self reported (patient diaries), structured questionnaires, patient interview
objective: pill counts, refill records, insurance claims, electronic monitoring devices
direct vs indirect measures
direct measures: blood serum levels, ingestible sensors, observation
1. Differentiate objective and self-reported measures of adherence. (40)
look at glucose monitoring records
proportion of days covered (PDC) from claims
assess patient self reporting
1. Given a patient with diabetes mellitus, identify at least one method to measure adherence. (40, 19)
questionnaires/patient diaries
pill counts, electronic monitoring, tracking behavioral goals
1. Given a patient with obesity, identify at least one method to measure adherence. (19, 40)
health system/HCT factors: long wait times, lack of time with patients, lack of community support, patient-provider relationship
condition related factors: severity of symptoms, level of disability, comorbidities
patient related factors: forgetfulness, lack of understanding, low literacy
social/economic factors: poverty, low level of education, lack of transportation
therapy-related factors: complexity of regimen, duration of treatment, adverse effects
1. In a patient scenario with diabetes, evaluate barriers to adherence. (40, 41)
1. In a patient scenario with obesity, evaluate barriers to adherence. (40, 41)
educational: provide clear information, tailor to patient’s situation
behavioral: pill boxes, calendars, email reminders
administrative support: tailoring of medications regimens, recommend change in therapy if adverse effects are a problem, automated refills, 90 say supplies, medication reconciliation
List interventions available to improve adherence with treatments for diabetes and obesity.
leads to poor blood sugar control
increased risks of complications
higher hospitalization rates
early mortality
Explain why non-adherence is a medication-related problem for a patient with type 1 or 2 diabetes mellitus.
worsening health outcomes
exacerbate the chronic nature of obesity
higher health care costs/hospitalizations
1. Explain why non-adherence is a medication-related problem for a patient with obesity. (25)
leptin and insulin resistance: Hormones like leptin (from fat cells) and insulin (from the pancreas) signal to the hypothalamus to suppress appetite.
In obesity, a state of resistance develops, meaning the brain does not properly receive or respond to these satiety signals, leading to persistent feelings of hunger.
gherlin dysregulation: the "hunger hormone" ghrelin, secreted by the stomach, is elevated before meals.
In obesity, its signaling to the mesolimbic reward system may be altered, further stimulating appetite.
What hormones regulate homeostasis for monitoring the body’s energy status and controlling basic sensations of hunger and fullness (satiety)?
brain region composed of several distinct nuclei, involved in coordinating the GI and nervous systems to the endocrine system,
major structure controlling appetite
hypothalamus
causing appetite suppression
anorexigenic
causing increased appetite
orexigenic
pertaining to the cessation of hunger
satiation
the sensation of being full
satiety
specialized endocrine cells of the GI tract and pancreas
enteroendocrine cells
any gut hormone (GLP-1 and GIP) released in response to eating and stimulate the pancreas to release insulin which helps lower blood sugar levels
regulate appetite
slow digestion
reduced the amount of sugar released by the liver
aid in weight loss and provide cardiovascular protection
Incretin
several hormones released from the gut in response to food intake exert anorexigenic (appetite-suppressing) responses in the brain, particularly in the hypothalamus
What are anorexigenic hormones?
Glucagon-like peptide-1 receptor agonist (GLP-1 RA) - slows stomach emptying and increasing feelings of fullness to lower blood sugar and reduce appetite
cholecystokinin (CCK) - stimulates contraction of gallbladder to release bile, triggers pancreas to secrete digestive enzymes, promotes satiety, and regulates appetite
peptide tyrosine tyrosine (PYY) - appetite regulating hormone produced in the gut which is released after feeding to reduce hunger and promote satiety
pancreatic polypeptide (PP)
oxyntomodulin (OXM or OXY)
Leptin- hormone produced by fat cells that signals the brain that there are sufficient fat stores, suppressing appetite and promoting satiety
Insulin - suppresses appetite by crossing the blood-brain barrier to stimulate hypothalamus (inhibit neurons that promote hunger and activate neurons that promote satiety)
Name some anorexigenic hormones.
a hormone made by fat cells that decreases your appetite
lower when you are thin and higher when you’re obese
in obesity, people develop a resistance to the appetite- suppressing effects of leptin
What is leptin?
a hormone that increases appetite and also plays a role in body weight
from the stomach
“hunger hormone”
What is ghrelin?
Underweight: BMI of less than 18.5
Normal range: BMI of 18.5 - 24.9
Overweight: BMI of 25 - 29.9
Obesity: BMI of more than 30
Class I Obesity: 30 - 34.9
Class II Obesity: 35 - 39.9
Extreme obesity: BMI over 40 (Class III)
Interpret body mass index (BMI) - what do the values mean?
Ghrelin (reduce satiety)
Leptin
GLP-1
Insulin
Which of the following hormones induces satiety?
Gastrin (stimulates the secretion of HCl in the stomach to aid in digestion in preparation for food) - makes you feel hungry
Which hormone has an impact on the hypothalamus and controls satiety and is secreted from the stomach?
enhances satiety in the brain
reduces GI motility
makes me feel full
How do GLP-1 agonist make you lose weight?
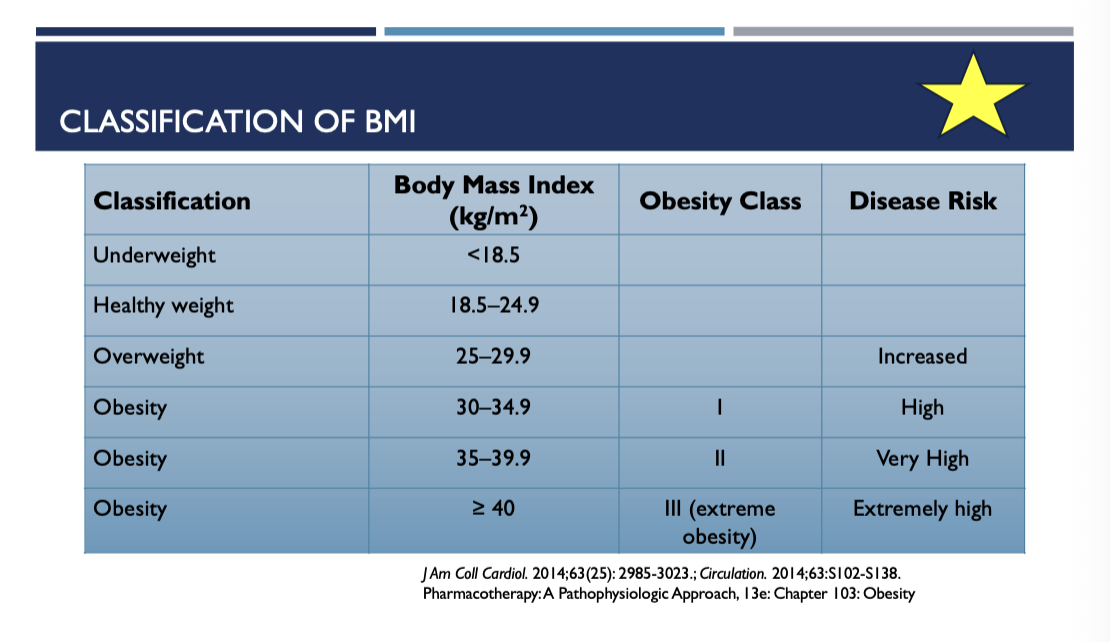
Classification of BMI chart
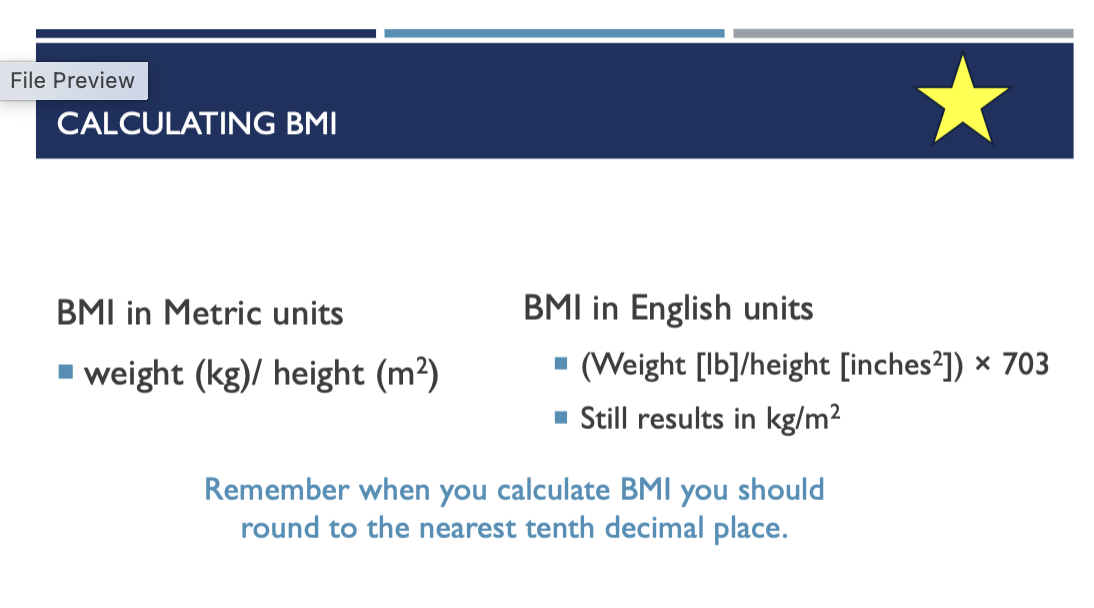
Calculate BMI (round to nearest tenth decimal place)
39.37 inches
How many inches in one meter?
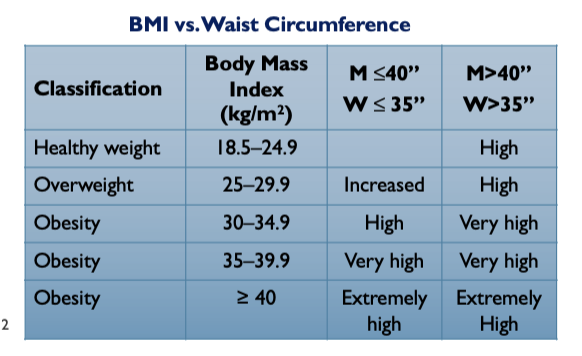
BMI and Waist Circumference Chart
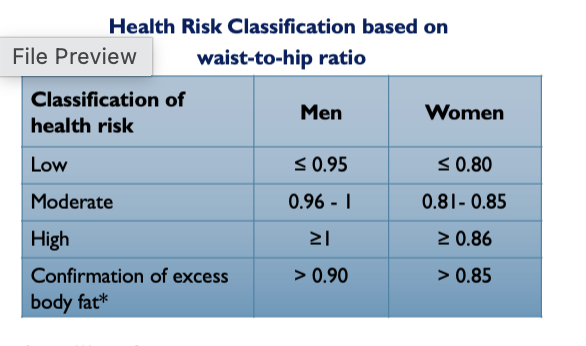
Health Risk Classification based on waist-to-hip ratio
5-10%
What is the goal weight loss for all therapies?
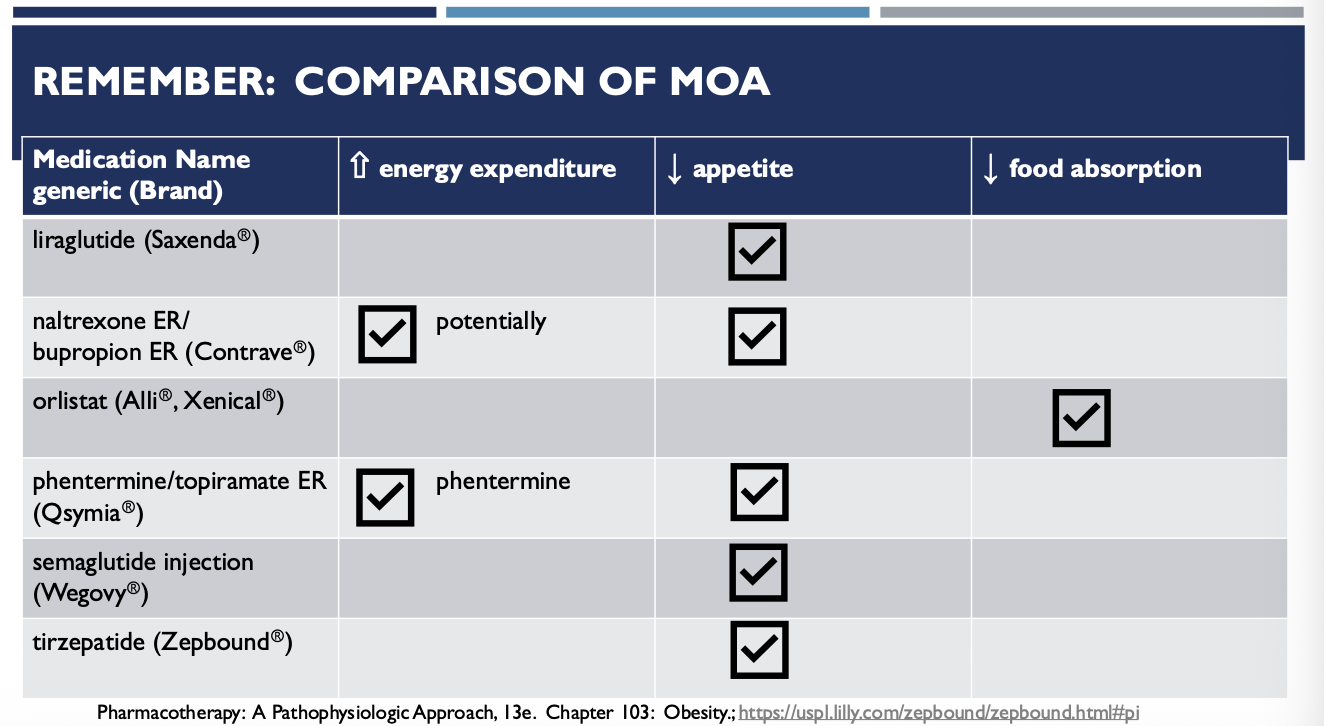
Which medications increase energy expenditure?
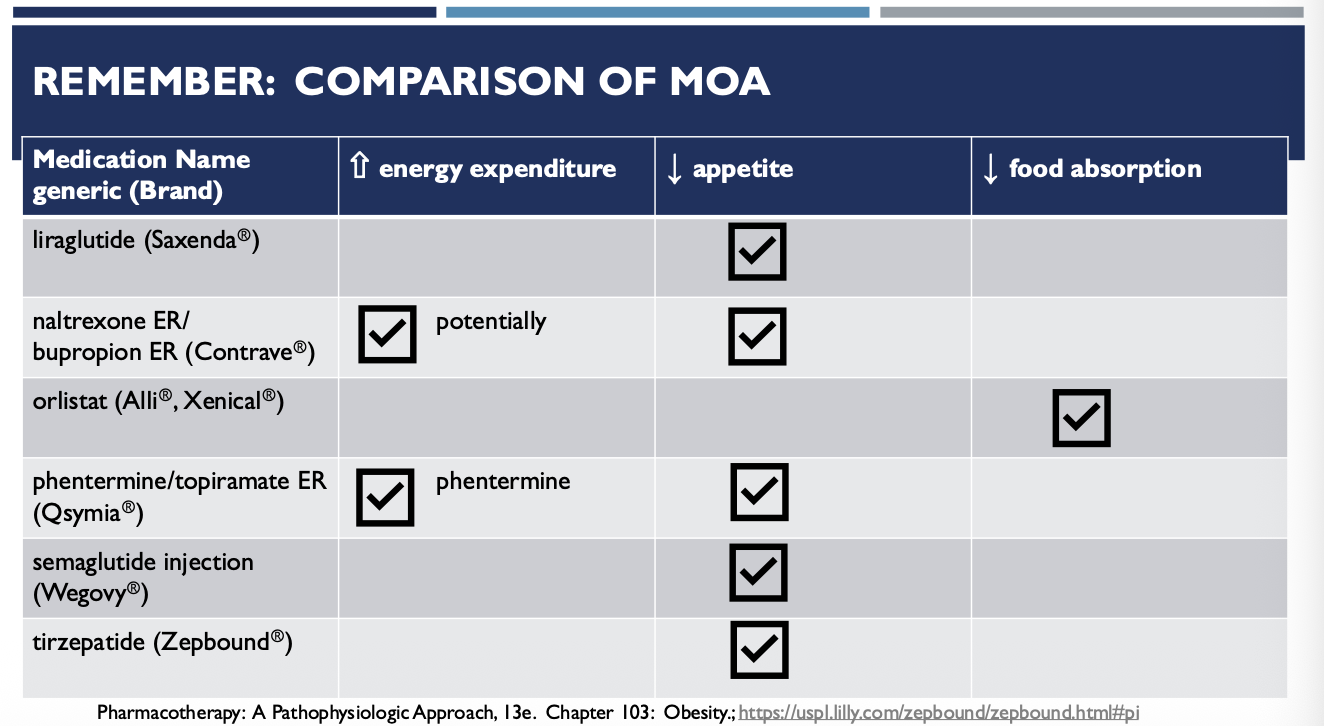
Which medication decreases food absorption?
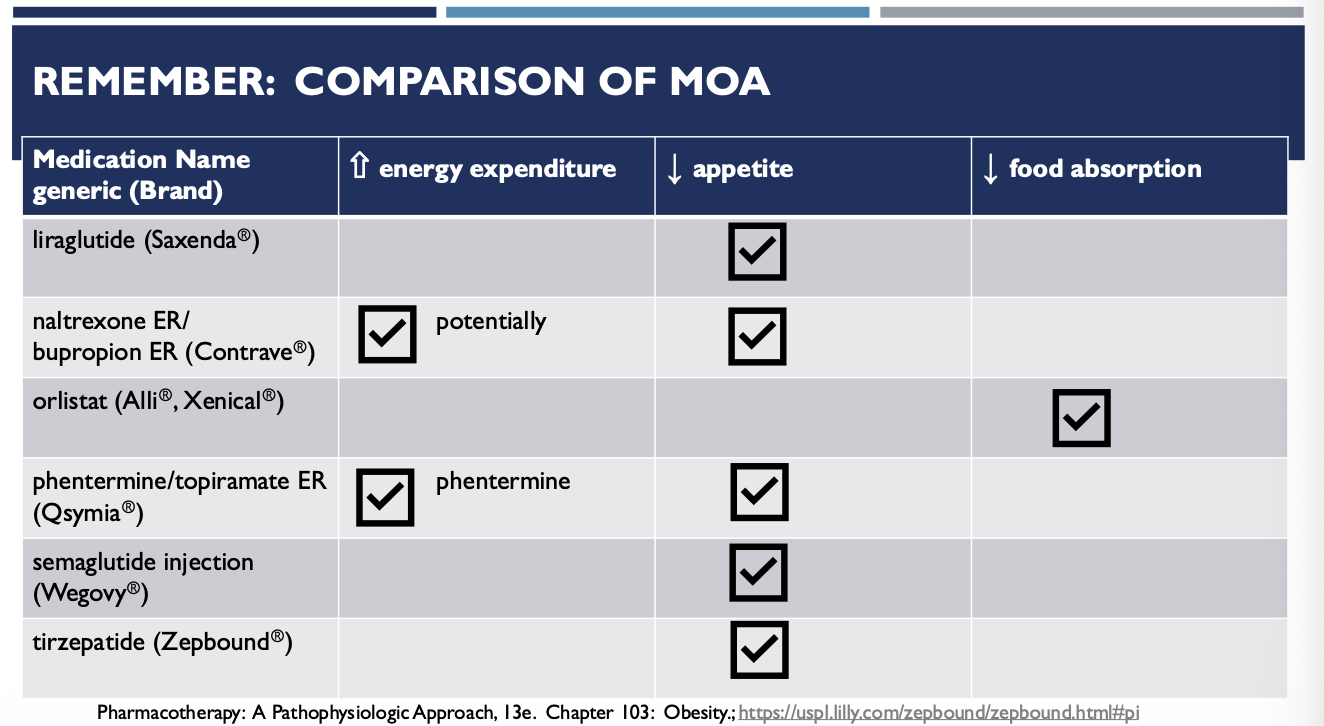
Which medications decrease appetite?
men: 1500-1800 per day
women: 1200-1500 per day
What is the calorie goal for men and women?