PHGY 209 - Midterm
1/361
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
362 Terms
physiology
the study of normal functional activities in healthy living organisms
homeostasis
state of dynamic constancy
fundamental principle of physiology
at all levels of organization the functional activities are directed at maintaining optimal and relatively constant internal conditions
Milieu Interieur
“internal environment”
environment surrounding individual cells is vastly different from outside environment
internal conditions remain relatively constant under conditions of health
aspects of body fluids
volume, distribution, characteristics, functions
average amount of water in bodies
45% to 75%
what is body water the medium for
solutes dissolving
where metabolic reactions occur
what are functions of body water
regulating body temp
moistening tissues
lubricating joints
protecting organs/tissue
preventing constipation
helps liver and kidney by removing waste
dissolve minerals so body can use them
carries O2 to cells
what causes difference in the amount of water in individuals
adipose tissue
% of water in various tissue
skin = 70%
muscle = 75%
heart, liver, brain, kidney = 70-80%
bone = 25%
fat = 10%
what happens to % of body water as fat increases
as fat increases water decreases
factors that affect body water
age, sex, weight
standard body water for male, white, 70 kg, 21
60%
variations in body water due to age and sex
infant = ~75% - little fat
18-40 = ~50% (female) - estrogen = deposition of fat in breasts ~60% (male)
elderly = ~45% (female) ~50% (male) - decrease in muscle tissue which is replaced by connective tissue which is drier and increase in adipose tissue
MAJOR TREND = same bw for men and women until puberty when women have less bw and then trend stays the same with ~10% bw for women until death
how to calculate body water in L
weight x bw% / 100 = volume (L)
why is it important to know body water percentage
dosing for water-soluble medication
dosage = 10mg/7kg
is body water a dynamic steady state
yes bc body water remains constant in health
does water input and output have to be the same
yes
obligatory losses
required losses (~1.5 L a day)
insensible - lungs and skin
sensible - urine and stool
facultative losses
vary with intake (necessary to maintain balance)
urine (*kidney)
what kind of loss is sweat
neither facultative or obligatory b/c if you drink more water you wont sweat more
insensible perspiration vs sweating
insensible perspiration:
water
passive evaporation (affected by temp/humidity)
entire skin surface
continuous and obligatory
sweating:
electrolyte
active secretion (energy dependent)
sweat glands
activated by heavy work/temp
water turn over in adult vs baby
adult = 3-4% of body weight in 24 hours
baby = 10% of body weight
why is babies water turnover so high
kidneys less developed
no water drank to maintain electrolyte balance
more loss bc of high surface area to volume ratio
what does body water volume help regulate
normal solute concentrations
normal blood volume and pressure
negative water balance
reduced intake
excessive loss from gut
excessive sweating
loss in expired air (dry air at high altitudes)
loss in urine
water intoxication
excessive intake - causes cells to swell
renal system failure
are body water compartments and sub compartments rigidly isolated
no, water can exchange freely between them
two major body water compartments
intracellular fluid 2/3 - inside cells bound by cell membrane - 28 L
extracellular fluid 1/3 - surrounds cells - 14 L
total body water = 42 L
ECF divided into…
2 major = plasma 5% and interstitial fluid 15%
2 minor = lymph 1-2% and transcellular fluid
plasma
fluid medium in which blood cells are suspended
different parts of blood
plasma, buffy layer (WBC, platelets), red blood cells (RBC, erythrocytes)
hematocrit
percentage of blood volume that is occupied by RBC
normal value is 45%
interstitial fluid
fluid that percolates between individual cells (through capillaries and cells)
lymph
one way finger like projections
converge to form larger vessels which converge to form lymphatic ducts
drain into large veins in chest
transcellular fluid
aggregate of small fluid volumes secreted by specific epithelial cells that line body cavities
do not contribute overall to water exchanges
percentages and groups of total water
ICF = 40%
ECF = 20%
ISF = 15%
plasma = 5%
methods to determine compartment volumes
direct (mathematically measure volume)
indicator dilution method
indicator dilution method
know total quantity of test substance introduced (through vein)
allow time to equilibrate
remove volume of blood and centrifuge to obtain plasma
concentration of plasma and volume of fluid after dispersion
use V = Q/C
factors of indicator
non toxic
diffuse readily and evenly
induce no changes in distribution of water between compartments
easy to measure its concentration
radioactive
ECF compartment measurement
needs to cross capillary wall not cell membrane ~14 L
plasma volume measurements
cannot cross capillary wall ~3.5L
ICF of ISF volume measurements
total body water - ECF = ICF
what element is ICF high in
K+ (and Mg++) low in Na+ and Cl-
what element is ECF high in
Na+ and Cl- and low in K+
good for IV drips
physiological saline measurements
0.9% NaCl
barriers to transport between ICF and external environment
cell membrane - barrier between ICF and ECF
capillary wall - barrier between ECF and plasma, and between plasma and the external environment
permeability of cell membrane
highly permeable to: H2O, Lipid-soluble substances, Dissolved Gases (O2, CO2), Small uncharged molecules
Less Permeable to: Larger molecules, Charged particles
Impermeable to : Very Large molecules
what makes up the cell membrane
phospholipids - hydrophilic heads and hydrophobic tails
cholesterol
proteins - integral and peripheral
glycocalyx
cholesterol in cell membrane
buffer to prevent low temps from inhibiting fluidity and high temps from increasing fluidity
formation of vesicles that pinch off cell membrane
lipid rafts (signalling)
proteins in cell membrane
integral - cross the membrane, close to phospholipids
peripheral - sides of plasma membrane
glycocalyx in cell membrane
formed from glycans, glycoproteins, glycolipids
cell-cell recognition, communication, adhesion, protection
fluid mosaic model
dynamic, fluid structure
phospholipid bilayer = solvent for embedded proteins creating mosaic of molecules that move laterally
selective transport - proteins
channels and transporters
enzyme - proteins
amino acid transport, Na-K pump
cell surface receptor - proteins
G - protein receptor, insulin receptor
cell surface identity marker - proteins
CD4 T Lymphocytes
CD45 Leucocytes
CD68 Monocytes
cell adhesion - proteins
CAMS, cadherins, integrins
attachment to cytoskeleton
actin. microtubules, septins
two transmembrane pathways
phospholipid bilayer
interaction with transmembrane protein
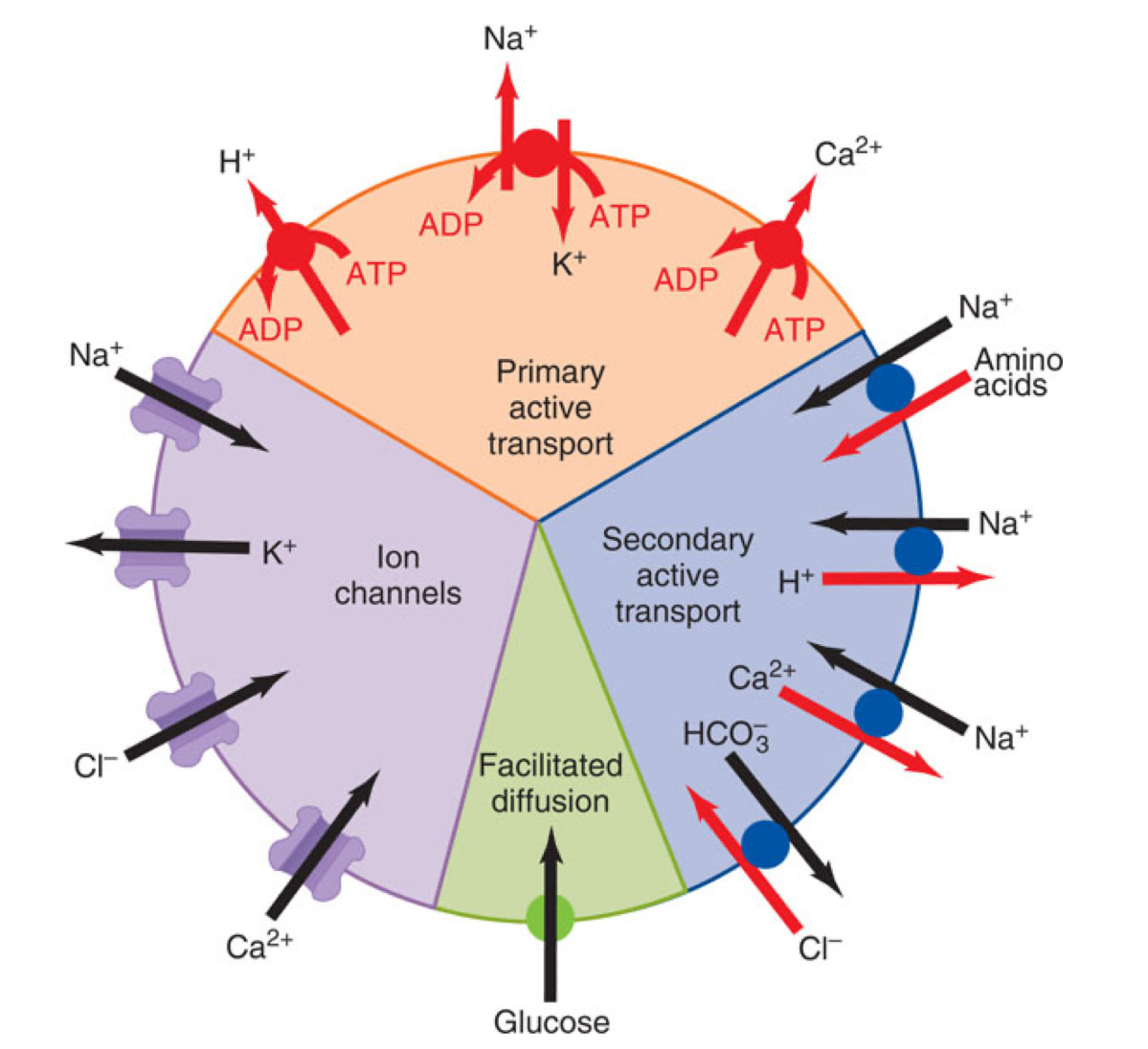
passive transport types
diffusion
facilitated diffusion
osmosis
active transport types
active: primary and secondary
pino/phagocytosis
diffusion
movement molecules from one location to another as a result of random thermal motion
flux
amount of solute crossing surface area per unit time
one way flux
unidirectional rate of movement of solute
net flux
overall rate of movement of solute
what is diffusion driven by
concentration gradient
when is net flux zero
at equilibrium
intracellular and extracellular concentration both starting at zero
time 0 = concentration zero for both when molecule is added to extracellular solution (Co). Co remains constant because the number of molecules required to increase Ci is small bc the intracellular cell volume is small relative to the extracellular volume.
why can diffusion only occur over small distances
Diffusion time increases in proportion to the square of the distance travelled by the solute molecules
diffusion across lipid bilayer
Non-polar molecules and gases
Mass of the molecule
Concentration gradient
Lipid Solubility
diffusion through ion channels
concentration gradient
electrical gradient
ion species (Na, K, Ca, Cl)
ion channels
transmembrane proteins that show ion selectivity
what determines the movement through ion channels
opposing electrochemical forces
electrical potential difference across membrane
concentration gradient of that ion across membrane
ion channel gating types
ligand - open when molecule binds to it
voltage - change in membrane potential
mechanical - stretch or pressure
what does current flow through ion channel depend on
channel conductance
channel open time
frequency of channel opening
concentration gradient
membrane potential
mediated transport
movement of ions and other larger molecules by integral membrane proteins called transporters, carrriers, exchangers (slower than ion channels)
facilitated, active transport
factors that determine mediated transport
solute concentration
affinity of transporter for solute
number of transporters
rate of transporter conformational change
characteristics of mediated transport
a. specificity - transporter likes one molecule
b. saturation - rate reaches max when all binding sites on all transporters are occupied
c. competition - similar structured molecules compete for same binding site
facilitated diffusion
presence of transporter or carrier which enables solute to move better than simple diffusion
solute binds to transporter
conformational change
solute on other side of membrane
conformation change to og conformation
NO ENERGY and HIGH TO LOW CONCENTRATION
active transport
transporter mediated
supply of chemical energy (hydrolysis of ATP)
susceptible to metabolic inhibitors
against concentration gradient
primary active transport
hydrolysis of ATP by transporter
phosphorylation of transporter changes the conformation of the transported and solute binding affinity
sodium potassium pump
2 potassium in, 3 sodium out
phosphorylation to bring Na in and dephosphorylation to bring K out
Ca - ATPase
maintain low intracellular Ca levels
H - ATPase
maintain low lysosomal pH
H/K - ATPase
acidification of stomach
secondary active transport
movement of Na down concentration gradient is coupled with transport of another solute molecule against concentration gradient - uses energy stored in the electrochemical gradient which comes from primary
sodium transporter
high concentration of sodium outside cell
Na binds to transported allowing glucose/aa to bind to same carrier
conformational change delivers Na and substance inside cell
reverts back and Na is pushed outside cell by Na/K - ATPase
secondary active transport mechanisms
symport/cotransport = solute transported in same direction as Na
antiport/countertransport/exchange = opposite direction as Na
examples of symport
Na+ with HCO3/aa/glucose cotransporters
examples of antiport
Na+ with H+/Ca++ exchangers
summary of transport mechanisms
endocytosis
cell membrane invaginates and pinches off to form vesicle
exocytosis
an intracellular vesicle fuses with the cell membrane and its contents are released into ECF
types of exocytosis
constitutive - non regulated
replaces plasma membrane
deliver proteins to cell membrane
secrete collagen/other materials
regulated
triggered by extracellular signals, increase of cytosolic Ca++
secretion of hormones, digestive enzymes, neurotransmitters
types of endocytosis
pinocytosis
engulfs extracellular fluid including solutes present
non specific
when in cytoplasm fuse with other vesicles like endosomes and lysosomes
phagocytosis
specific and triggered
extensions of cell membrane called pseudopodia fuse to form large vesicles that pinch off the membrane
sometimes fuse with lysosomes where contents are degraded
defends against infection
receptor-mediated endocytosis
molecules in ECF bind with high affinity to specific protein receptors on the plasma membrane
clathrin dependent receptor mediated endocytosis
ligand binds to receptor → conformational change and clathrin is recruited to plasma membrane
adaptor proteins link with ligand-receptor to the clathrin
forms cage like structure which invaginates leading to clathrin coated vesicle
sheds clathrin coat and fuses with endosome and lysosome
or fuse with membrane on other side of cell
clathrin and receptors recycled
LDL (low density lipoproteins)
cholesterol is transported in the blood as lipid protein particles known as LDL
differences between LDL and endocytized vesicles
endo - fuse with early endosomes where LDL dissociates from receptor protein
LDL - continues to late endosome andlysosome where cholesterol is released