electrolyte 1 - hypokalemia (↓K+)
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
normal sodium (Na+) range
135-145 mEq/L
normal chloride (Cl-) range
98-107 mEq/L
normal potassium (K+) range
3.5 - 5.0 mEq/L
normal phosphorus (PO4-) range
2.7-4.5 mg/dL
normal calcium (Ca2+) range
8.4-10.2 mg/dL
normal magnesium (Mg2+) range
1.6-2.4 mg/dL
total body water (TBW)
distributed primarily into 2 compartments:
the intracellular compartment (ICF; 60% of TBW)
the extracellular compartment or extracellular fluid (ECF; 40% of TBW)
intracellular compartment (ICF)
ICF osmolality is primarily determined by the concentration of potassium and its accompanying anions (mostly organic and inorganic phosphates)
extracellular compartment/extracellualr fluid (ECF)
sodium and its accompanying anions (chloride and bicarbonate) comprise more than 90% of the total osmolality of the ECF
describe the compartmentalization of potassium
potassium is the most abundant cation in the body, with estimated total-body stores of 3,000 to 4,000 mEq (3,000 to 4,000 mmol)
the sodium-potassium-adenosine triphosphatase (Na+-K+-ATPase) pump located int eh cell membrane is responsible for the compartmentalization of potassium
this pump is an active transport system that maintains increased intracellular stores of potassium by transporting sodium out of the cell and potassium into the cell at a ration of 3:2
which drugs cause hypokalemia through intracellular shift?
beta receptor agonists and catecholamines:
epinephrine, albuterol, terbutaline, pseudoephedrine
insulin
alkalosis — sodium bicarbonate*
(also causes hypokalemia through renal loss)
which drugs cause hypokalemia through renal loss?
thiazides
loop diuretics
penicillin
alkalosis — sodium bicarbonate*
(also causes hypokalemia through intracellular shift)
which drugs cause hypokalemia through GI loss
laxatives
sorbitol, sodium polystyrene sulfonate
functions of potassium
cellular metabolism & growth
protein & glycogen synthesis
regulation electoral gradient across myocardium
cardiac conduction
symptoms associated with mild hypokalemia
3.1 - 3.49 mEq/L
may be asymptomatic
N/V
muscle weakness
symptoms associated with moderate and severe hypokalemia
mild = 2.5 - 3.0 mEq/L
severe = < 2.5 mEq/L
paralysis
respiratory compromise
EKG changes
cardiac arrhythmias
death
underlying causes of hypokalemia
refeeding syndrome:
can occur when severely malnourished pts (ie nutrition depleted for 7-10 days) receive aggressive nutritional supplementation —> causes severe/rapid:
↓ serum phosphate
↓ serum potassium
↓ serum magnesium
medications
metabolic alkalosis (pH ↑, K+↓)
for every 0.1 ↑ in pH, [K+] ↓ by < 0.4
hemodialysis
magnesium deficiency
renal outer medullar potassium (ROMK) channel
hypokalemia management if pt needs to be on diuretic therapy
consider using a potassium sparing diuretic:
aldosterone antagonists:
spironolactone
eplerenone
sodium channel blockers:
amiloride
triamterene
potassium sparing diuretics MOA
in the collecting duct and distal tubule:
aldosterone antagonism (spironolactone and eplerenone)
inhibits aldosterone —> ↓ Na+ reabsorption and ↑ K+ sparing
inhibition of aldosterone sensitive sodium channels (amiloride and triamterene)
non-pharmacologic treatment for hypokalemia
diet — high potassium content foods
consensus guidelines on pharmacological treatment of hypokalemia
usual dose to prevent hypokalemia = 20 mEq/day
usual dose to treat hypokalemia = 40-100 mEq
K+ repletion therapy is best administered orally in divided doses over several days to achieve full repletion
K+ repletion therapy is recommended for pts who are:
sodium-senstive
hypertensive
subject to vomiting or diarrhea
taking diuretics
subject to laxative abuse
potassium repletion in pts with renal dysfunction
caution in repleting potassium in patients with renal dysfunction
reduce by ~50% in renal insufficiency
when is PO preferred and when is IV preferred?
oral route is preferred if patient can tolerate PO and is asymptomatic
if pt has severe hypokalemia, might need both PO and iV
if pt is in the ICU, IV may be preferred
if pt is NPO, IV route is preferred
which do you replete first if the pt has concomitant hypomagnesemia and hypokalemia?
replete magnesium first if it is low
oral treatment for hypokalemia
most to least % of potassium:
Potassium Chloride
Rx
both PO and IV
Potassium Bicarbonate
OTC/Rx
PO
Potassium Citrate
OTC/Rx
PO
Potassium Gluconate
OTC
PO
Potassium Phosphate
Rx
both PO and IV
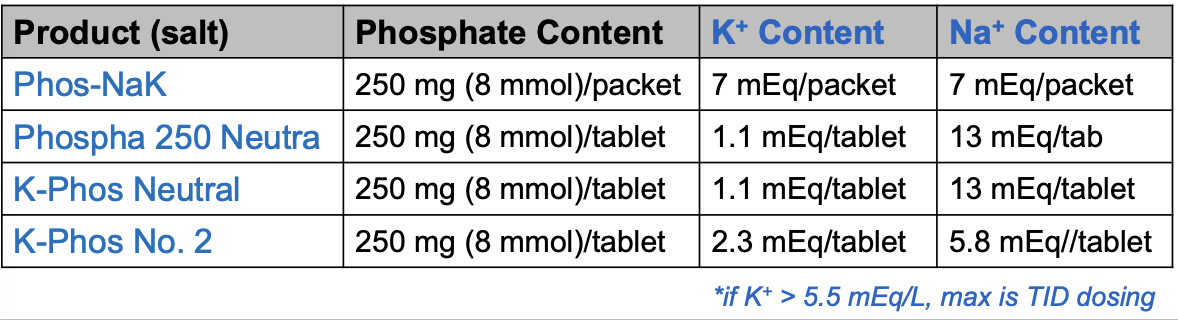
K-Phos products
used for pts with BOTH hypophosphatemia AND hypokalemia
different products contain SAME amount of phosphorus and VARIABLE amounts of potassium (and sodium)
to minimize GI damage, dissolve tablets in 6-8 oz water for at least 2-5 min (can crush tablet particles that remained undissolved. stir vigorously)
most to least K+ content:
Phos-NaK (*max is TID dosing)
K-Phos No. 2
Phospha 250 Neutra
K-Phos Neutral
oral K+ products ADEs
common:
GI side effects (e.g. N/V, diarrhea, flatulence)
if dose > 40 mEq, it should be give in divided dose
ex. if the pt needs 60 mEq, give 30 mEq PO BID
serious:
abdominal pain, GI ulcer
cardiac arrest, arrhythmias
hyperkalemia
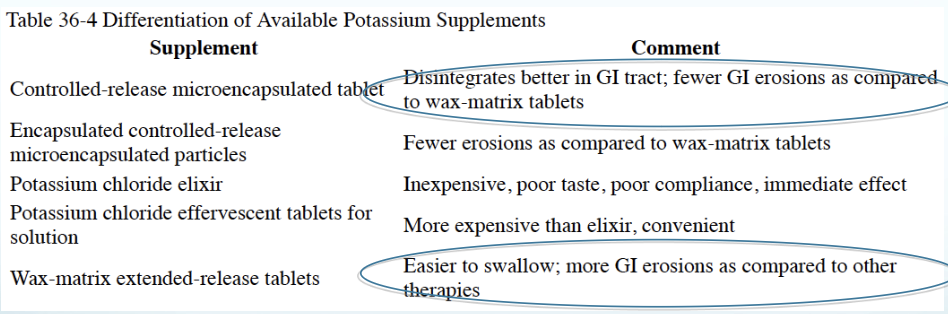
compare the different formulations of potassium supplements
IV K+ products
potassium chloride — most common, most efficient (i.e., raises serum [K+] at a faster rate)
for every ~10 mEq of K+ administered, serum K+ will ↑ by 0.1 mEq/L
potassium phosphate — use if pt also has hypophosphatemia
potassium acetate — use if pt has metabolic acidosis
IV K+ products ADEs
common:
phlebitis (inflammation of the vein)
injection site pain (burning)
extravasation (can lead to tissue necrosis)
serious:
cardiac arrest, arrhythmias
hyperkalemia
IV potassium administration
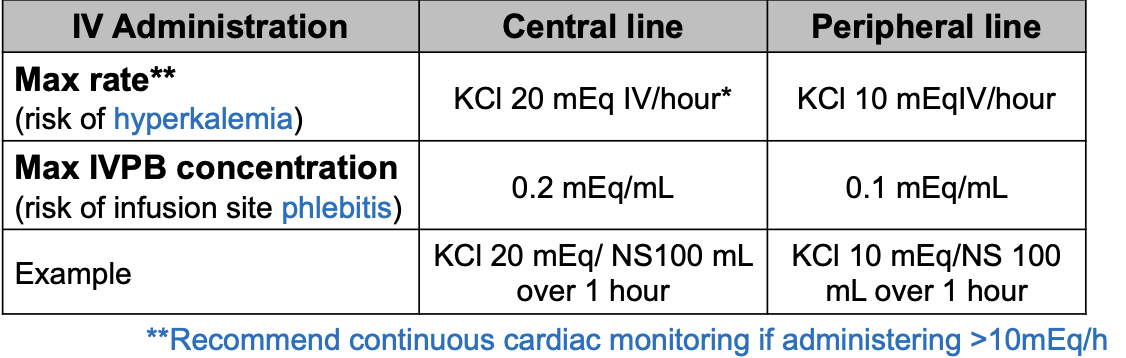
IV potassium monitoring
cardiac function (tele monitoring, ECGs)
K+ levels
within 2-8 hours after replacement (sooner if symptomatic)
daily with morning labs
signs of phlebitis, extravasation
IV push vs IV piggyback (IVPB)
IV piggyback (IVPB) = administered as an infusion
IV push = administered via syringe
NEVER give K+ as an IV push —> will cause cardiac arrest
compartmentalizationof potassium (concept map)
the normal concentration range for potassium is 3.5-5 mEq/L
the intracellular potassium concentration is usually approximately 150 mEq/L
the Na+-K+-ATPase is responsible for the compartmentalization
different formulations of potassium supplement GI intolerance (concept map)
wax-matrix extended-release tablets > controlled release micro-encapsulated tabletsrimp
primary causes of hypokalemia (concept map)
loop and thiazide diuretic administration
excessive loss of potasisum-rich GI fluid as a result of diarrhea and/or vomiting
drug induced hypokalemia
beta2 agonsits
insulin overdose
high dose of penicillins