Week 3
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
gum
stimulates vagus nerve. The vagus nerve is a nerve that runs from the brain stem to the abdomen. Stimulating the vagus nerve can help reduce inflammation and improve relaxation.
Why chew gum?
gum helps to stimulate your vagus nerve. The vagus nerve is tasked with helping your body reduce stress and anxiety related to the fight-or-flight response by disengaging this response.
Chewing gum is believed to modulate cortisol to reduce anxiety.
“…recent report proved that long-term chewing gum was effective in reducing stress, anxiety, depression, and improving test scores in school nursing students”
(Luo, Xia & Zhang, 2022)
Map of Disorders covered today
1. Anxiety disorders
Generalized Anxiety Disorder
excessive, persistent worry about various aspects of life (e.g., work, health, finances) lasting 6 months or more.
Restlessness, fatigue, difficulty concentrating, muscle tension, and sleep disturbances.
Panic Disorder
Recurrent unexpected panic attacks, with intense fear or discomfort peaking within minutes.
Heart palpitations, sweating, trembling, shortness of breath, chest pain, dizziness, and fear of dying.
Phobias
Intense, irrational fear of specific objects, situations, or activities that leads to avoidance.
Fear associated with Panic Disorder?
A: Anticipatory anxiety about future attacks and avoidance of situations where attacks might occur.
Examples of common phobias?
Specific phobia: Fear of heights, spiders, or flying.
Social anxiety disorder: Fear of social situations or being judged.
Agoraphobia: Fear of open spaces or being unable to escape.
Map of Disorders covered today
2. Trauma and Stressor related Disorders
Acute stress disorder
A trauma-related condition lasting 3 days to 1 month after exposure to a traumatic event.
Intrusive thoughts, nightmares, dissociation, avoidance, and hyperarousal.
Post traumatic stress disorder
A trauma-related disorder occurring more than 1 month after exposure to a traumatic event.
Conversion Disorder
A condition where psychological stress is converted into neurological symptoms (e.g., paralysis, blindness) without a medical cause.
Map of Disorders covered today
3. Obsessive Compulsive Disorders
A disorder characterized by obsessions (intrusive, unwanted thoughts) and/or compulsions (repetitive behaviors or mental acts to reduce anxiety).
Fear of contamination, doubts (e.g., leaving the stove on), intrusive thoughts of harm.
ie Excessive handwashing, checking, counting, or organizing items.
Q: Key symptoms of PTSD?
Re-experiencing: Flashbacks or intrusive memories.
Avoidance: Avoiding reminders of the trauma.
Hyperarousal: Irritability, difficulty sleeping.
Negative mood: Guilt or emotional numbness.
What is Trichotillomania?
Repeated pulling out of one’s hair, resulting in noticeable hair loss and distress.
Trigers- Stress, anxiety, or boredom.
Trauma inform approaches to care
Principles of Trauma-Informed Approaches:
• Trauma Awareness( treating ppl like everyone comes with trauma to improve trustworthiness and more likely to reach recovery)
• Emphasis on Safety and Trustworthiness ( we are not forcing our decisions on them)
• Opportunity for CHOICE, COLLABORATION, CONNECTION
• Strengths based and Skill building
Overview of Anxiety Disorders
Generalized Anxiety Disorder
A disorder characterized by excessive worry about everyday events or activities for at least 6 months.
Panic Disorder
A disorder involving recurrent, unexpected panic attacks with persistent fear of having more attacks.
Phobias
Intense, irrational fears of specific objects, situations, or activities that cause avoidance and distress.
Epidemiology
Anxiety disorders are
are one of the most common form of psychiatric disorders in Canada (11.6% of those over the age of 18 years)
Increasing prevalence in children and youth with the highest increase in prevalence for those aged 5–10 years.
why: social media, COVID- 19(in formidable yrs had a change in social interactions and are still feeling the effects of social anxiety
Comorbidity
Frequently co-occur with other psychiatric problems like depression anxiety, substance abuse disorders
Frequently co-occurring with depressive disorders
- treatments for both disorders are similar due to shared neurobiology, symptom similarities, and abnormalities of emotional processing
CBT
Cognitive Behavioral Therapy is a goal-oriented, structured psychotherapy that focuses on identifying and changing negative thought patterns and behaviors.
Cognitive Restructuring: Identifying and challenging distorted thoughts.
Behavioral Activation: Engaging in activities to improve mood.
Problem-Solving: Developing strategies to tackle stressors.
Skills Training: Teaching coping mechanisms like relaxation techniques.
Q: What techniques are used in CBT?
Thought Records: Writing down automatic thoughts to evaluate their accuracy.
Exposure Therapy: Gradual exposure to feared situations to reduce anxiety.
Behavioral Experiments: Testing the validity of negative beliefs through action.
Relaxation Training: Techniques such as deep breathing or mindfulness.
Etiology of
Anxiety
Disorders
•Biological factors (genetic, neurobiological theories)
the younger the person diagnosed with ansiety the more its linked to genetics and parents may have it too
•Social factors (ie., traumatic life events, overprotective parents)
•Psychological factors (psychodynamic, learning theories)
•Environmental factors (ie., prenatal toxic exposure, adverse childhood events) ie children exposed to smoke had higher lvls of anxiety
•Sociocultural factors (ie., culture bound syndromes)
jumping Frenchman of maine
a rare and unusual neurological disorder characterized by an extreme startle reaction. It was first identified in the late 19th century in a group of French-Canadian lumberjacks in Maine.
Psychological Theories
Psychodynamic theories
Sigmund Freud
Focus: Unconscious mind, childhood experiences, internal conflicts.
Key Concepts:
Id, Ego, Superego.
Psychosexual stages of development.
Defense mechanisms (e.g., repression, denial).
Goal: Resolve unconscious conflicts to improve mental health
Harry Stack Sullivan
Focus: Interpersonal relationships and social interactions.
Key Concepts:
Anxiety stems from unsatisfactory interpersonal relationships.
Personality develops based on interactions with others.
Emphasized therapeutic alliances in treatment.
Goal: Improve relationships to alleviate mental health issues.
Behaviour theories
Focus: Observable behaviors and how they’re learned.
Key Theorists: Pavlov, Skinner, Watson.
Key Concepts:
Classical Conditioning (Pavlov): Learning through associations.
Operant Conditioning (Skinner): Behavior shaped by rewards/punishments.
Goal: Modify maladaptive behaviors through reinforcement or desensitization.
Cognitive theories
Focus: Thought processes and their impact on emotions and behavior.
Key Theorists: Beck, Ellis.
Key Concepts:
Cognitive Distortions: Negative thought patterns that influence emotions.
Cognitive Behavioral Therapy (CBT): Combines changing thoughts and behaviors.
Goal: Restructure negative thoughts to improve mental health.
Cultural considerations
Focus: The role of culture in shaping behavior, beliefs, and mental health.
Key Points:
Cultural norms influence symptom expression and coping strategies.
Awareness of cultural differences is essential for effective therapy.
Therapists should address language barriers, cultural stigmas, and traditional practices.
Goal: Provide culturally sensitive care that respects diverse values and practices.
What is Stress?
An appropriate reaction that is proportionate to the actual threat
The energy generated from the … can be used constructively to meet the challenge, solve the problem or overcome the threat
Examples? financial, work, abt the future
Selye’s General Adaptation Syndrome
Alarm; stimulates adrenaline and norepinephrine & organs to prepare fuel
Resistance; body prepares for fight, flight, or freeze behaviours
Exhaustion; continual arousal and little reserve capacity
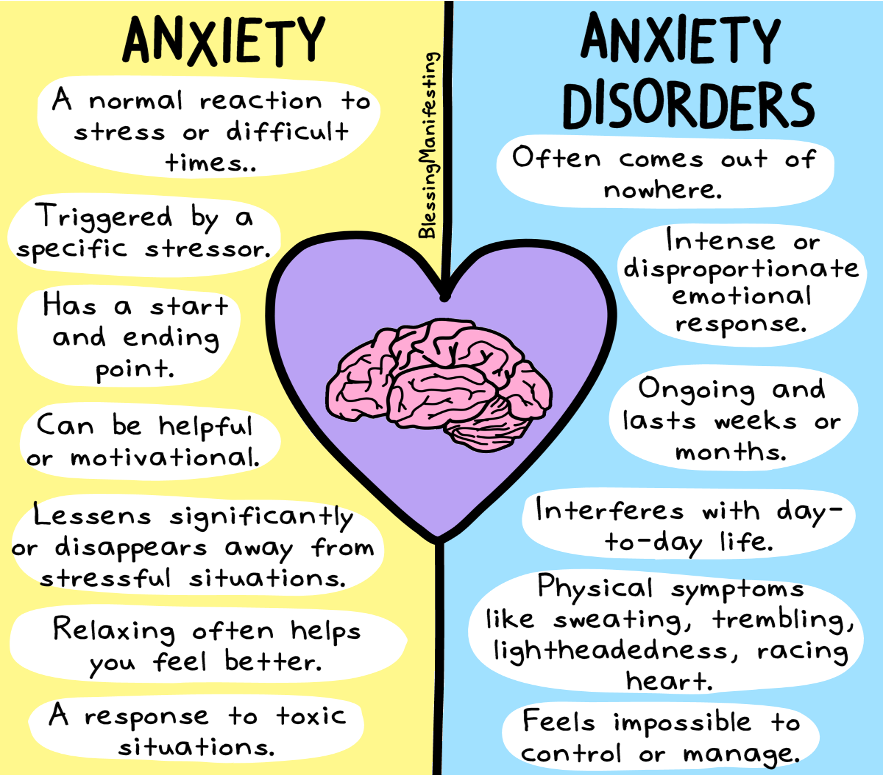
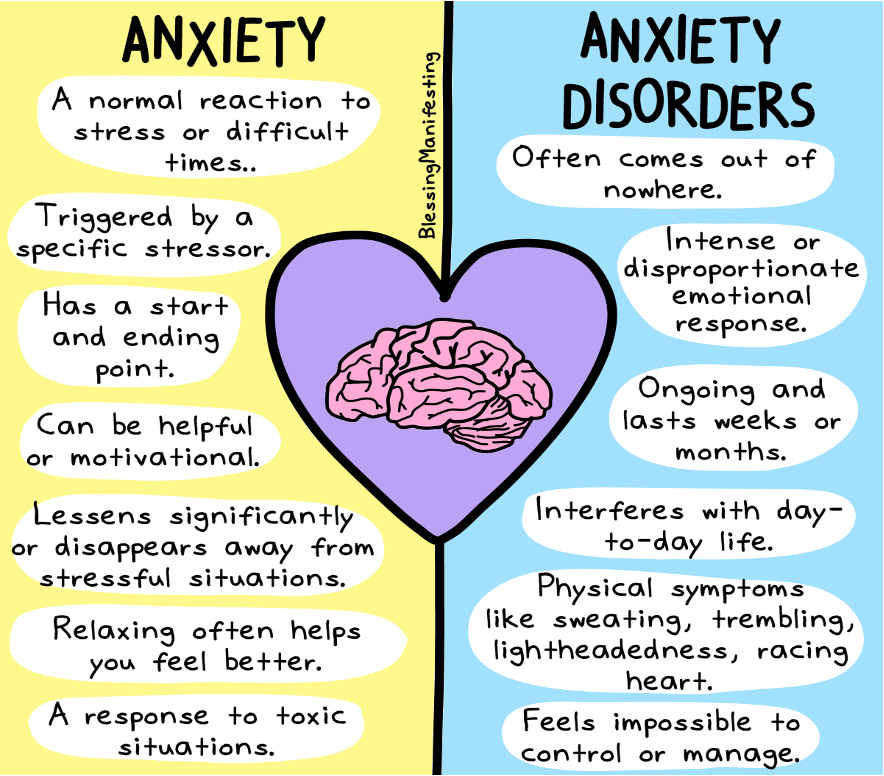
What are Anxiety & Anxiety Disorders?
not everyone with anxiety receives anxiety disorder
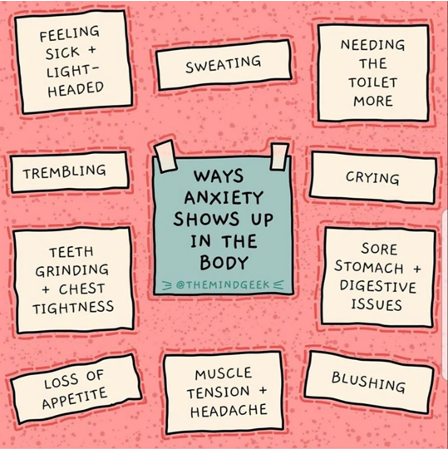
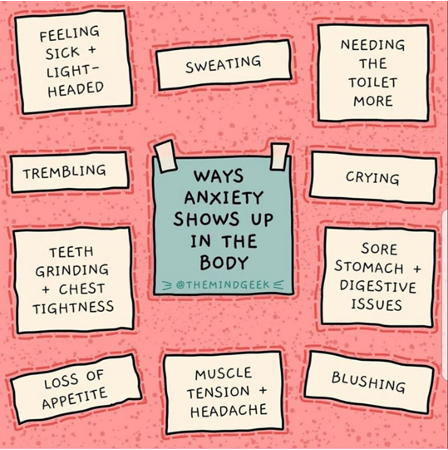
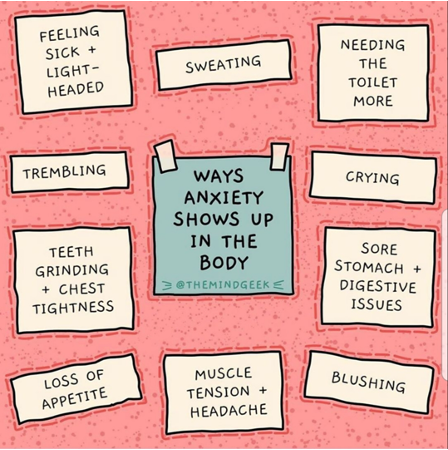
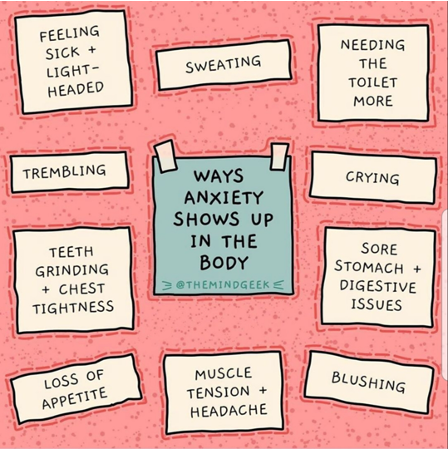
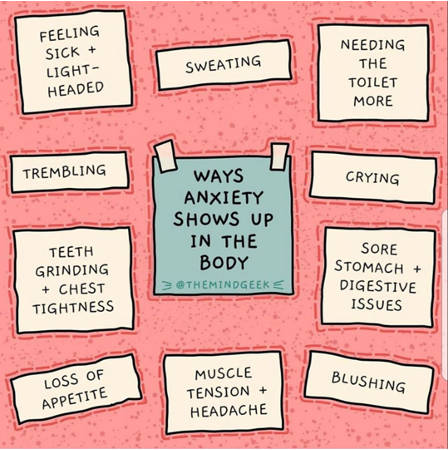
Manifestations/ Responses to Anxiety
Physiological
Cardiovascular (HR increase, BP up )
Respiratory ( increase resp, increases o2 demand, longterm effects- exacerbates conditions u already have ie asthma attacks)
Gastrointestinal ( increases peristalsis, nausea, diahrea, long term effects- increase stress on GI tract like stress ulcer and increased problems with IBS)
Neuromuscular (short term- tightening(ie hunching shoulders), stress headaches, longeterm, increases tension headahces and increase tension in shoulders)
Urinary tract (increases frequency how???, longterm UTI
Skin (sweating, acne, picking at skin, hives, exce,a flareups)
Manifestations/ Responses to Anxiety
Behavioral
Restless
Rapid speech
Inhibition
Hypervigilance (always on guard and waiting for the needle to drop)
Lack of co-ordination
Manifestations/ Responses to Anxiety
Cognitive
Impaired attention
Blocking of thoughts
Loss of objectivity (emotions, biases, or personal involvement cloud one’s judgment, making it difficult to assess situations rationally or make fair decisions.)
Flashbacks
Preoccupation (being excessively focused on a particular thought, idea, or concern, often to the detriment of other aspects of life.)
Manifestations/ Responses to Anxiety
Affective/Emotional
Edginess
Impatience
Terror
Guilt
helplessness
Social
Increasing isolation

Levels of Anxiety (Ch.14 – Table 14.1)
Anticipation and Mild Anxiety
associated with the tensions of daily living, person alert, perceptual field increased.
Motivates learning, growth, creativity, problem solving
S/S:
- restlessness, difficulty sleeping, irritability, impatience, relieving behaviour such as finger tapping, fidgeting (automatisms)


Levels of Anxiety (Ch.14 – Table 14.1)
Moderate Anxiety
Person focuses on immediate concerns, narrowing of perceptual field
Person hears, sees, grasps less
S/S:
voice tremors, difficulty concentrating, pacing, increased VS, urinary frequency, headache, muscle tension, dry mouth
focus on CBT therpy and how they ca develop coping scoping skils


Levels of Anxiety (Ch.14 – Table 14.1)
Severe Anxiety
Significant reduction in perceptual field
Person focuses on specific detail and not anything else (very focused on self and always think something bad will happen)
All activity directed to relieving anxiety, much direction needed to focus on another area, requires supervision
Purposelessness activities happen like continuously cry
Focused on self, environment blocked out, sense of dread
S/S:
inability to process info & make decisions, purposeless activity, crying, tachycardia, nausea/vomiting
this severe anxiety is treated with medication and CBT therapy (8-10 sessions)


Levels of Anxiety (Ch.14 – Table 14.1)
Panic
Associated with sense of terror
Person unable to do things even with direction
Disorganized personality, loss of rational thought
Distorted perception, emotionally paralyzed
Unable to communicate and function
S/S:
terror, dilated pupils, pallor, speaks unintelligibly or is mute, severe tremors, hallucinations, extreme withdrawal or out of control agitation, hypertension
Fight, flight, or freeze
this rewures therapy and meds if expeireincy=ing panic attacks


Nursing Mental Health Assessment: Anxiety
•How is the person behaving?
•Can you determine the cause? - not everyone will know the exact cause
•Assess level of anxiety – review recent history, psychiatric illness, drugs (how long you’ve been experiencing this or uv experiences any support for anxiety or psychiatric disorders)
•How does the person perceive the threat?
•Monitor physical responses
•Identify coping skills used in the past and their reaction to stress
open ended questions*

Anxiety Disorders:
Incidence and etiology?
Who is affected?
Most common mental disorder
More common in women, people <45 y/o, divorced/separated, lower SES
Anxiety Disorders:
Incidence and etiology?
Etiology
Genetics: family history
Brain Chemistry: abnormal levels of certain neurotransmitters
Environmental Factors: trauma, stressful events, use and withdrawal from addictive substances
Generalized Anxiety Disorder (GAD)
Worry that is excessive, persistent and pervasive for more days then not for a period of 6 months
“generalized” -focused on various events/activities
Key assessment components:
amount of time spent worrying
degree of control over one’s worrying
impact on personal, social, and occupational functioning(decrease in social interactions with persons with GAD and cant drive themselves in a car, will stop. attending in class, work etc)
Treatment:
- Cognitive behavioural therapy (CBT) and other psychotherapy
- Awareness of stressors, deep breathing, relaxation(music, meditation)
- Benzodiazepines(ie adavam bc travelling and scaard of flying MD will prescibe adavam), SSRIs, SSNRIs
MSE findings for GAD
•History
•Appearance(fidgeting, postural changes and muscular tension when they walk in) & Behaviour (rapid speech, decreased eye, stuttering, leg bouncing)
Speech & Language
•Mood( look for them using words like this that also means theu expereince anxiety:) frustrated, nervous, apprehensive, feels unease) and Affect( hypervigilence: checking for cameras and obsesively looking around, increased startle response)
•Thought Process(losing focus, hyperfixated on one topic, catostrophic thinking(worst will happen in everything they will go through) & Content
•Assessment of harm to self/others
Sensorium & Intellectual Process
Sensory perception alterations (Impaired concentration)
Judgement & Insight ( poor jundent and incsight and may know this isnt normal to feel that way and this may drive them to seek help, short term memroy can occur
Self-concept(is poor)
Roles & Relationships(role changes ie employee pulls back and leaves early and cant do same task, slef care affected, parent no longer parents properly)
Physiologic & Self-care considerations
Panic Disorder
Pannic attacks
15-30 min
Rapid, intense and escalating anxiety
Recurrent (≥1 per month)
Unexpected and often no antecedent (trigger)
Can cause ‘agoraphobia’- fearing and avoiding places or situations that might cause panic and feelings of being trapped, helpless or embarrassed. You may fear an actual or upcoming situation.
Symptoms (dx= ≥4):
palpitations, sweating , trembling, SOB, chest pain, sensation of choking, nausea, dizziness, depersonalization, derealization, fear of “going crazy” or death, paraesthesia, chills/hot flashes
How will you nurse someone struggling with a panic attack?
Stay Calm: Speak calmly and reassure the patient.
Ensure Safety: Move to a quiet, safe space.
Reassure: Let them know they are safe and the attack will pass.
Guide Breathing: Encourage slow, deep breaths (4-4-4 technique).
Grounding: Focus on surroundings (e.g., "Name 5 things you can see").
Stay With Them: Don't leave until the attack ends.
Post-Attack Care: Offer emotional support and discuss coping strategies.
Reminder: Monitor vitals and document the episode.
Panic Disorder (cont.)
treatments
Cognitive behavioral techniques:
Deep breathing, relaxation
Medications:
Benzodiazepines, SSRIs, tricyclic antidepressants
Education (CBT, medication, how to put yourself in safe situations, educating loved ones on how to support them through it)
Evaluation:
- Client satisfaction with quality of life
MSE findings for Panic Disorder
•History ( how many uve had, environment and if aware of it, are u diagnosed)
•Appearance & Behaviour(hyperventilation, tense, fidgeting)
•Speech & Language
•Mood(feeling of dread or impending doom indicating panic attack and Affect( can be flat, tearfulness or can see anxiety on face)
•Thought Process(losing train of thought, not listening when being calmed down) & Content
•Assessment of harm to self/others
Sensorium & Intellectual Process (irrational, hard to control and challenging- large outburst that can occur)
Sensory perception alterations
Judgement & Insight
Self-concept
Roles & Relationships
Physiologic & Self-care considerations
Panic Disorder:
NSG interventions
During panic attack
-Promote safety, privacy
-Decrease environmental stimulation(lights and loud nioses)
-Remain with client
-Soothing, calm voice
-Reassure client is safe, this will pass
-Therapeutic communication
Panic Disorder:
NSG interventions
Following panic attack:
-Therapeutic communication- open ended questions and discussion
-Education re: Managing anxiety
-Deep breathing, guided imagery(ie imagin wave rushing over u) progressive relaxation
-Education re: client & family
-Combined psychotherapy & meds
-Manage vs cure goal (not. something we can just cure its normal its how we manage it so its not paralyzing or severly affecting dayto day life)
-Benefits of exercise
benzo- used as emergency drugs and used as PRN
Panic Disorder: Nursing Evaluation
Reassess behaviours both psychological and physiological
Does patient have any insight into their problem?
Have they learned ways of dealing with it that are constructive? (how we know is by teach back method, if not what components we need to work on and document it)
Do they recognize the triggers? (if pt doesn’t know ask :what was going on in the environment before panic struck
Coping: what is working and what is not working? (ie with a journal they should write down their thoughts before, during and after)

Phobias
Intense illogical persistent fears about a specific object or situation
Categories:
agoraphobia;
specific phobia;
social phobia (social anxiety disorder)
Categories of specific phobia:
natural environment;
blood-injection;
situation;
animal;
other types

Phobias (cont.)
Treatment
Cognitive behavioral therapy:
positive reframing; (Help the individual view feared situations or objects in a more positive light.)
assertiveness training; (Empower individuals to express their feelings, needs, and boundaries confidently)
systematic desensitization; (Gradually expose the person to the feared object or situation in a controlled way to reduce anxiety over time)
flooding (Expose the person to the feared object or situation at full intensity, with the idea that prolonged exposure will lead to a decrease in fear.)
Medications
Antidepressants (SSRIs/SNRIs): Help reduce anxiety and depression linked to phobias.
Benzodiazepines: Sometimes prescribed for short-term relief of acute anxiety, but not recommended for long-term use due to dependency risks.
Beta-blockers: Can reduce physical symptoms of anxiety (e.g., rapid heartbeat) in certain situations
Trauma
and
Stress Disorders
Acute Stress Disorder
Occurs within 3 days to 1 month after trauma. Symptoms include flashbacks, nightmares, and hyperarousal. Treatment: CBT, trauma-focused therapy, medications.
Post Traumatic Stress Disorder
Lasts more than 1 month after trauma. Symptoms include reliving the trauma, avoidance, and hypervigilance. Treatment: CBT, EMDR, medications.
Conversion Disorder
Neurological symptoms (e.g., paralysis, seizures) with no medical cause, often triggered by stress. Treatment: CBT, physical therapy, stress management, medications.
Acute Stress Disorder
Onset/duration:
Occurs immediately after a traumatic event
lasting ≤ 4 weeks
Symptoms:
Re-experiencing
Avoidance
Negative cognition
Hyper-arousal (being on-guard)
Agitation
Includes:
dissociative symptoms (ex. Depersonalization(Feeling like you're observing yourself from outside your body) and derealization(dreamlike state, Feeling like the world is unreal)
Post-traumatic Stress Disorder
Onset/Duration:
Occurs ≥ 3 months following traumatic event
Symptoms:
Same as ASD
Includes:
Dissociative symptoms
MSE findings for Phobias
History: Fear of specific objects/situations, often triggered by traumatic events or learned experiences.
Appearance & Behavior: May appear anxious, restless, or agitated; often avoidant of feared objects.
Speech & Language: Speech may be rapid or pressured when discussing the feared object, but generally coherent.
Mood & Affect: Mood may be anxious or fearful; affect congruent with anxiety symptoms.
Thought Process & Content: Thoughts focus on avoiding or escaping the feared situation; may exhibit irrational or distorted thinking.
Assessment of Harm to Self/Others: Low risk of harm unless phobia involves dangerous behavior; no intent to harm others.
Sensorium & Intellectual Process: Intact sensorium, intellectual functioning unaffected, although anxiety can impair focus.
Sensory Perception Alterations: Rare, though hypervigilance may lead to misperception of threats.
Judgement & Insight: Judgment may be impaired during a panic attack, but insight into the phobia is often intact.
Self-Concept: May have low self-esteem or feel inadequate in managing anxiety.
Roles & Relationships: Phobia may impact social relationships, work, or daily activities.
Physiologic & Self-care Considerations: May experience physical symptoms (e.g., sweating, rapid heartbeat); may neglect self-care during anxiety episodes.
ASD & PTSD Treatment
•Psychosocial Treatments:
•Cognitive behaviour therapy
Teach coping skills to improve functioning
Anxiety management
Exposure therapy (repeated exposure to memories and emotions of the event to diminish their impact)
ASD & PTSD Treatment
•Medications:
Antidepressants: SSRIs (e.g., sertraline, fluoxetine) help reduce anxiety and depressive symptoms.
Antipsychotics: May be used for severe symptoms like dissociation or agitation.
Mood Stabilizers: Used if mood swings or irritability are significant.
Other Treatments:
Stress Management: Mindfulness, relaxation techniques, and grounding exercises.
MSE findings for ASD and PTSD
acute is less than 4 months and ptsd more than 4 months
History: History of trauma or exposure to life-threatening events; in PTSD, symptoms last more than a month, meds, triggers, coexisting comorbidiies, coping strategies, family history
Appearance & Behavior: Appears anxious, hypervigilant, or detached; may avoid reminders of trauma; physical signs of stress (e.g., fidgeting).
Speech & Language: Speech may be pressured or slow, especially when discussing trauma; often coherent but focused on distressing memories.
Mood & Affect: Mood is typically anxious, fearful, or depressed; affect may be flat or incongruent with the situation. will explain fear and horror or anxiety wrds, emotional numbing(ie words like not sure how to feel so affect not corresponding with situation sometimes
Thought Process & Content: Intrusive thoughts, flashbacks, or nightmares related to the trauma; irrational or distorted thinking in response to perceived threats.
Assessment of Harm to Self/Others: Suicidal ideation or self-harm may be present in severe cases; generally no risk to others.
Sensorium & Intellectual Process: Intact orientation, but concentration and memory may be impaired due to anxiety; intellectual functioning generally unaffected.
Sensory Perception Alterations: Flashbacks, hallucinations, or vivid intrusive memories of the trauma; hypervigilance may cause misperception of threats. hyperarousal(always on guard)
Judgment & Insight: Judgment may be impaired during episodes of high anxiety or flashbacks; insight into the disorder is often intact.
Self-Concept: Feelings of guilt, shame, or inadequacy; may experience a loss of identity or self-worth due to trauma.
Roles & Relationships: Strained relationships due to avoidance behaviors or emotional numbing; difficulty trusting others.
Physiologic & Self-Care Considerations: Physical symptoms (e.g., increased heart rate, sweating) related to anxiety; neglect of self-care during episodes of distress or hyperarousal.
Nursing Interventions-
Trauma and stress related disorders
Promote client safety
Safe plan (see template)
Help clients cope with stress and emotions
Grounding
Validating
Reorient to reality (if having disosiative symptomss)
Help promote client’s self-esteem
Promote an empowering self-image
- Establishing social support:
- Identification of emergency services
- Key family/friends
- Connecting with counseling, spiritual resources
Conversion disorder
FND same as conversion disorder(functional … find this disordewordr)
Difficult to diagnose
Characterized by S&S affecting sensory and motor with no neurological disease or medical condition (ex. Paralysis, numbness, blindness, deafness or seizures)
An extreme reaction to stress, anxiety and trauma
Treatment:
Some recover without treatment
CBT
Medications: tricyclic antidepressants, haloperidol
ECT(electric shock therapy to shick brain to receruit brain and prevent it from happening again)
MSE findings for Conversion Disorder
History: Recent stress, trauma, or psychological conflict; sudden onset of neurological symptoms (e.g., paralysis, blindness) without a clear medical cause.
Appearance & Behavior: Appears distressed or anxious; may show physical signs of disability (e.g., tremors, gait disturbances) but with inconsistent or exaggerated symptoms.
Speech & Language: Speech may be normal or impaired depending on symptoms; no physical cause for speech difficulties (e.g., aphonia or dysphagia).
Mood & Affect: Mood may be anxious or depressed, often reflecting the distress of the symptoms; affect may be inconsistent with the severity of physical symptoms.
Thought Process & Content: May express beliefs or fears about the physical symptoms; thinking can be influenced by the severity of symptoms and the underlying psychological stress.
Assessment of Harm to Self/Others: Generally no intent to harm self or others; symptoms are not consciously produced, though there may be underlying psychological distress.
Sensorium & Intellectual Process: Intact sensorium and cognitive functioning; however, concentration may be impaired during episodes of distress.
Sensory Perception Alterations: May report altered or absent sensations (e.g., blindness, numbness) that do not align with medical findings; somatic symptoms are inconsistent with neurological examinations.
Judgment & Insight: Insight is often poor; the individual may believe the symptoms are entirely physical or medically explained, unaware of the psychological origin.
Self-Concept: May have low self-esteem, especially if symptoms interfere with life roles; stress or trauma may be linked to feelings of inadequacy or helplessness.
Roles & Relationships: Symptoms can strain relationships due to the impact on functioning; family or work roles may be affected.
Physiologic & Self-Care Considerations: Physical symptoms (e.g., paralysis, seizures) may impair mobility or self-care; self-care may be neglected or difficult due to the functional disability.
Obsessive Compulsive Disorder
(OCD)
Obsessions
Unwanted, intrusive and persistent thoughts, impulses, or images that cause anxiety and distress.
Compulsions
Behaviours that are performed repetitive, in a ritualistic fashion, with the goal of preventing or relieving anxiety and distress caused by obsessions.
Onset: males more often in childhood, females more often in their 20s
Etiology: environmental experiences in development, heredity, anxiety
DX
OCD consume the client and impair functioning
Obsessive-Compulsive Disorder (OCD) (cont.)
Treatment
Medications
Cognitive behavior therapy
Response prevention
Exposure
Thought stopping
Recovery is possible!
MSE findings for Obsessive-Compulsive Disorder (OCD)
History: Persistent, intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to reduce anxiety; symptoms interfere with daily functioning.
Appearance & Behavior: May appear anxious or distressed, particularly if unable to perform compulsive rituals; behaviors often time-consuming (e.g., washing, checking, arranging).
Speech & Language: Speech may be normal, though the individual may talk about rituals or obsessions; speech may become more rapid or pressured when discussing obsessions.
Mood & Affect: Mood can be anxious, tense, or frustrated; affect is often incongruent with the situation, particularly when rituals are disrupted.
Thought Process & Content: Thought process is typically logical but dominated by intrusive, unwanted thoughts (obsessions); the content centers on fears of harm, contamination, or orderliness. ruminate(obsess and fixtate on items)
Assessment of Harm to Self/Others: Low risk of harm to others; self-harm may occur (e.g., from repeated rituals) or due to frustration with inability to control compulsions.
Sensorium & Intellectual Process: Intact sensorium; intellectual function is generally unaffected, though concentration may be impaired by obsessive thoughts.
Sensory Perception Alterations: Rarely altered, but distressing thoughts may dominate perception of reality, leading to hyper-focus on certain sensations (e.g., fear of germs or contamination).
Judgment & Insight: Judgment may be impaired in relation to the irrationality of compulsions; insight is often partially intact—patients recognize the compulsions are excessive but feel unable to control them. insights vary, some are aware and some are not
Self-Concept: Self-esteem may be affected, with feelings of guilt, shame, or inadequacy related to obsessions or compulsions; may feel out of control or anxious about not performing rituals correctly.
Roles & Relationships: OCD symptoms can interfere with work, family, and social roles due to time-consuming rituals; relationships may be strained if others don't understand the compulsions.
Physiologic & Self-Care Considerations: Compulsions may cause physical strain (e.g., hand washing leading to skin damage); self-care may be impacted by time spent on rituals; anxiety can also impact sleep and eating habits.
Nursing Interventions-
Obsessive-compulsive disorder
Therapeutic communication:
Offering support and encouragement
Validate their feelings and be clear that you believe they can change
Encourage the client to discuss their thoughts and ritual behaviours
Teach relaxation and behavioural techniques:
Have the client journal about triggering situations, and related thoughts and behaviours.
exposure and response prevention techniques
Completing a daily routine
Develop an agreed upon plan regarding completion of daily routines (time allotment - ie u spend 6hrs getting ready for work thats unreasonalbble so we should talk them through it that it should take shorter time)
Common Defense Mechanisms
… are behaviors people use to separate themselves from unpleasant events, actions, or thoughts. These psychological strategies may help people put distance between themselves and threats or unwanted feelings, such as anxiety, guilt or shame.
…. are a normal, natural part of psychological development. Identifying which type you, your loved ones, even your co-workers use can help you in future conversations and encounters.
Common Defense Mechanisms (cont)
Dissociation
not connected to the reality they are experiencing
Common Defense Mechanisms (cont)
Repression
unconsciously blocking from awareness that which is threatening or painful
may have lapses in mmemore bc associated with so much fear not able to remeber it
Common Defense Mechanisms (cont)
Conversion
Transforming anxiety into physical symptoms
Constructive Coping Strategies for Anxiety
•Finding comfort in social network (friends, etc.)
•Relying on self-discipline (making sure u are following through with strategies ie half hr walk everyday ice it makes me feel good)
•Express your feelings
•Avoidance and withdrawal (aviod anxiety-provoking situations if possible)
•Talking it out
•Privately thinking it through (ie self reflection)
•Engaging in self-healing practices-mind body practices
Building Skills for Stress Management
1. Exercise.
2. Relaxation Techniques.
Meditation/ prayer, guided imagery, progressive relaxation, abdominal breathing, yoga, massage.
3. Lifestyle Change
Eat well(certain foods spike anxiety; alcohol, caffeiene), sleep, satisfying relationships, seek help and support, schedule me-time.
4. Reframing
Glass half empty? Glass half full?
changing the way you look at a situation to view it in a more positive or helpful light. Glass half empty: Focusing on what’s missing or negative. Glass half full: Focusing on what’s there or positive.
5. Set realistic goals and expectations for yourself.
Summary
Stress- wear and tear of life on the body
Anxiety- part of life and response to stress
Levels from mild-panic
Unique psychological and physical responses at each level
Nursing interventions specific to each level
Anxiety disorders (chronic anxiety impairing functioning)
Review MSE and nursing interventions for all
study how to do MSE
watch video about MSE