Alterations in Mobility or Musculoskeletal Disorders
1/31
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Bone Health
Diet strong in vitamin D, calcium, and protein.
School-aged children need 1,000 mg of calcium (about 4 cups of milk a day).
Adolescents need 1,300 mg of calcium a day.
Encourage weight-bearing exercises; this increases bone density.
Avoid carbonated beverages.
Educate: Carbonated beverages decrease the bone’s ability to absorb calcium.

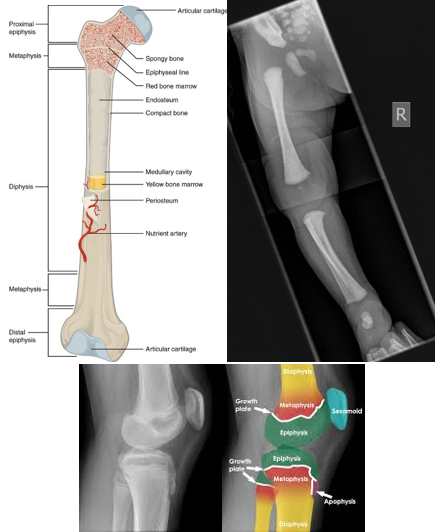
Pediatric Bone Anatomy
Infant skeleton is not fully ossified at birth.
Thick, strong periosteum—outermost lining of the bone—(better shock absorber!)
Pediatric bones can bend up to ~45 degrees before breaking.
Due to this, sometimes children can have more of an incomplete fracture than one an adult would have.
Bone ossification (cartilage to bone) is complete by adolescence.
The growth plate at the end of long bones is composed of the epiphysis and physis (epiphyseal growth plate).
The growth plate is the most vulnerable part of the bone.
Bone growth occurs here.
**The growth plate must be protected at all costs! If it is damaged, it can interrupt blood supply and cause growth failure**
Fractures in Children
Fractures are a common injury in children:
Rare in infants.
They aren’t very active or mobile yet; not doing any hazardous behaviors to themselves.
When they’re born, they may have a clavicular fracture, if they had some shoulder dystocia coming through the birth canal.
Ex: Mom is going down the stairs with her baby in her arms and slips. An infant arm, leg, and skull fracture is possible.
The clavicle is the most frequently broken bone in childhood, especially in those under 10 years old.
When describing a fracture as a nurse:
Name the bone affected.
Note if it is open (bone breaks through skin) or closed (skin is intact, the bone did not break through).
Note if it is distal or proximal.
Specify the part of the bone injured: epiphysis, metaphysis, diaphysis, or physis (Salter-Harris Classification)
Note if it is displaced or nondisplaced.
Displaced = ends do not line up; the patient tends to have a pretty significant amount muscle of spasms and their pain is worse.
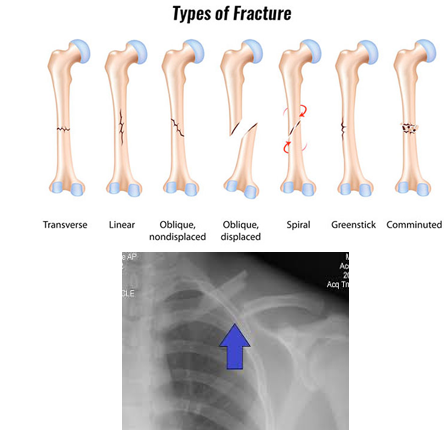
Describe the type: transverse, oblique, spiral, or depressed.
Common Pediatric Fractures
Greenstick
Buckle
Compound or Open
Stress Fracture
Spiral Fracture
Greenstick Fracture
Incomplete fracture
That thick periosteum comes into play!

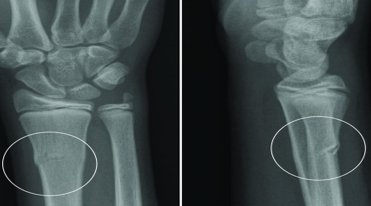
Buckle Fracture
Raised or bulging projection at the site
Seen in the wrist, typically from a fall on an outstretched hand (FOOSH).
Compound or Open Fracture
Fractured bone protrudes through the skin
It can be just a little bit or a lot.
Patient is at a huge risk for infection of the bone and their body.

Stress Fracture
Tiny cracks in a bone
Seen in athletes.

Spiral Fracture
Spiral appearance of fracture
Always investigate spiral fractures in children when the mechanism of injury does not match the fracture type, especially in a non-ambulatory child!
It takes a great force to cause this injury.

Epiphyseal Injuries
The weakest point of long bones is the cartilage growth plate (epiphyseal plate).
It is a frequent site of damage during trauma.
Injury may affect future bone growth.
Treatment may include open reduction and internal fixation to prevent growth disturbances.
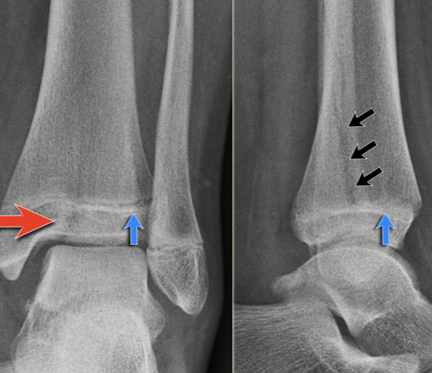
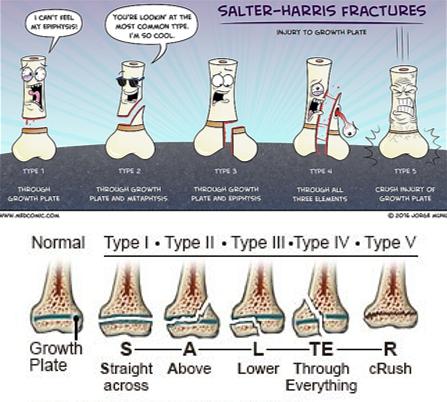
Salter-Harris Fractures
The Salter-Harris Classification system is used to describe fractures involving the epiphyseal growth plate.
These injuries have a higher likelihood of healing difficulties.
The most common concern is:
Growth arrest with the potential for deformity and limb length discrepancy.
Salter-Harris I and II fractures can be treated with closed reduction, casting, or splinting.
Salter-Harris III, IV and V will require surgery—open reduction.
Salter-Harris V fracture diagnosis may be delayed unless there is a high degree of clinical suspicion, and often the diagnosis is not made at the initial presentation.
May see in a follow-up examination as the patient starts to have some healing.
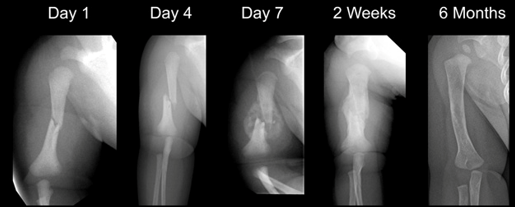
Bone Healing and Remodeling
Stages of Bone Healing
Inflammatory Phase:
Duration: hours to days
A hematoma forms, then begins forming a primary callus.
Reparative Phase:
Duration: days to weeks
A thick mass of callus forms around the bone ends.
New bone is formed from bone-forming cells.
Remodeling Phase:
Duration: months to years
The callus becomes smoother and is calcified.
Assessment of Musculoskeletal Injuries
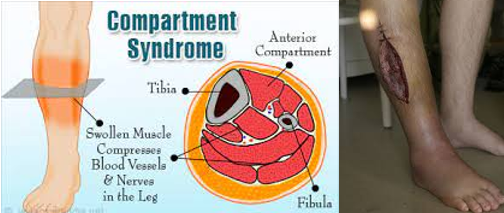
Assess for the 5 Ps to rule out complications of compartment syndrome:
Pain (increased and out of proportion)
Pulselessness
Pallor
Paresthesia
Paralysis
Also assess the 5 Ps before and after immobilization, as well as any time the patient reports a change in sensation.
Displaced fractures may require reduction:
Open Reduction: requires surgery.
Closed Reduction: patient is sedated; performed outpatient.

Casts and Splints
Immobilizes the fracture to ensure alignment.
Promotes healing, comfort, and provides protection.
Splinting:
Immobilizes the injury while allowing swelling to decrease.
The splint will be worn for approximately 1 week.
Like to start off with this.
Cast:
Provides hard immobilization of fractures.
Made of fiberglass or plaster.
Nursing Measures:
Assess the injury and determine if an open fracture is present.
Splinting or casting material is not placed over open fractures.
Open fractures require IV antibiotics and sometimes surgery.
Perform peripheral vascular checks during the initial assessment and before and after immobilization and/or reductions.
Pain management.
Apply the splint and ensure proper placement of splint padding and splint.
Educate the patient and family regarding warning signs of compartment syndrome and care of the cast or splint.

Cast Saw
When removing a cast, a cast saw is used.
This cast saw cuts through the cast using vibration.
If the cast saw stays against bare skin for more than a couple of seconds, it can cause a burn.

Complications for Splints or Casts
Compartment Syndrome:
Occurs when there is increased pressure in an enclosed space, such as a cast.
This results in decreased blood flow.
The patient will typically report sudden increased pain (this is due to tissue dying).
Ischemia occurs, followed by necrosis of tissue.
An emergency fasciotomy must be performed to save the tissue and extremity.
These patients will require a skin graft sometime in the future.
Pressure Sore:
Develops from improper cast or splint application.
Skin grafts will also be needed for recovery.
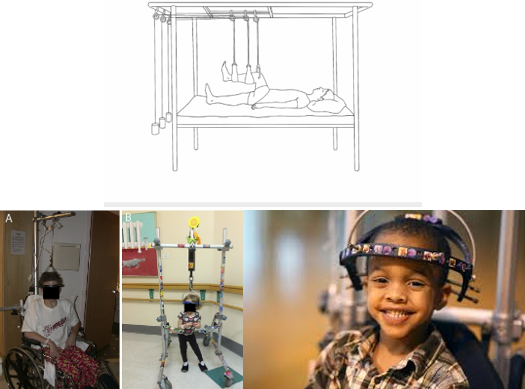
Traction
Uses:
Reduce and/or immobilize a fracture
Align an injured extremity
Allow the extremity to be restored to its normal length
May also reduce pain by decreasing the incidence of muscle spasms.
Extension by a pulling force may be used.
The type of traction used depends on the child’s age, the condition of the soft tissue, and the type and degree of displacement of the fracture:
Manual Traction:
Applied to the body part by hand, placed distally to the fracture site.
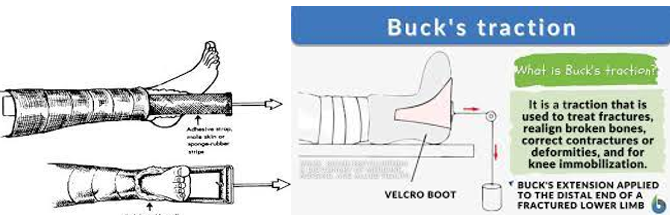
Skin Traction:
Pulling mechanisms are attached to the skin with adhesive material or elastic bandage.
Skin must be intact!
Skeletal Traction:
Applied directly to the skeletal structure by a pin, wire, or tongs inserted into or through the diameter of bone distal to the fracture.

Skin Traction
Buck’s Traction:
Reduces femur fractures.
Also used for contractures of the hip or knee.
Force is delivered through a traction boot or skin traction in a straight line.
**Skin must be intact!
Skeletal Traction
90-90 Traction:
Reduces femur fractures.
Pins are placed through the distal femur; traction is applied through pins only.
Huge risk for infection and pressure sores.
Nursing Considerations:
Regular pin care per policy.
Diversional activities
Frequent assessment of the peripheral neurovascular system.
Encourage patients to use their unaffected extremities.
Monitor U/O & BM.
Ensure adequate nutrition and hydration.
Encourage incentive spirometry use.
Halo Traction:
Used for fractures or injuries of the cervical spine.
First step in correcting severe scoliosis, kyphosis, and other spinal deformities.
A ring surrounds the head, and pins are attached to the outer portion of the skull.
Nursing Care of a Patient in Traction
Assessment of the 5 Ps
Maintain traction and alignment
Monitor weights and ropes:
All weights should hang freely; they should not rest on the ground or the bed.
Nurses do not adjust the weights.
Prevent skin breakdown using proper padding
Prevent complications
Provide pain management and comfort measures
Exercise unaffected extremities
Encourage deep breathing
Monitor for constipation or urinary stasis
Provide distraction
Enlist Child Life Services (CLS)

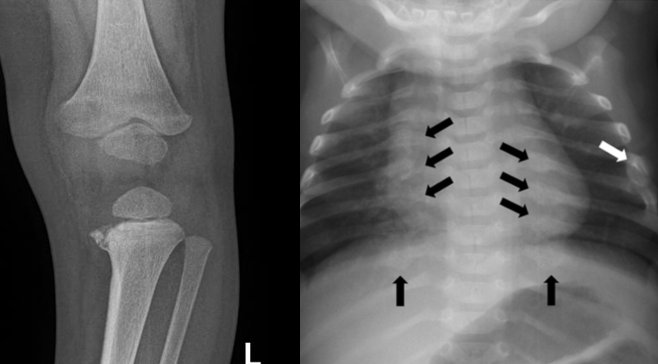
Child Abuse (Non-Accidental Trauma—NAT) Fractures
Occurs most often in children under 3 years of age.
Median age is 7 months.
Common Fractures in NAT (Non-Accidental Trauma):
Femur, humerus, and skull fractures are the most common sites.
Clavicular fractures and spiral fractures of long bones in non-ambulatory children.
Bucket Handle Fracture:
Occurs when an adult grabs, twists, or shakes a child’s limb in frustration.
Shaking the child, causing the limbs to move back and forth, can also cause a bucket-handle fracture.
It is difficult to sustain this injury from accidental causes, such as a fall.
Posterior rib fractures (due to compressive squeezing).
Multiple fractures, especially if they are in different stages of healing.
Be suspicious of any injury that does not fit the stated cause of injury.
Delay in seeking treatment.**
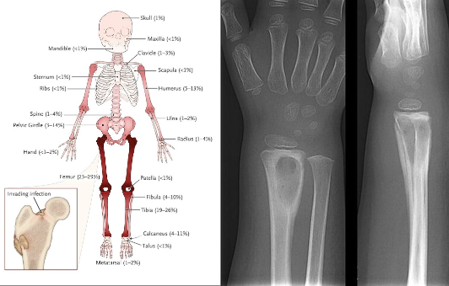
Osteomyelitis
Defined as an infectious process in the bone that can occur at any age, but is most commonly seen in children 10 years and younger.
Causes:
Direct inoculation (break in the skin → pathogen enters)
Abscess
Dead bone
Clinical Symptoms:
Malaise, low-grade fever
Irritability (especially in infants and non-verbal children)
Edema
Erythema
Joint tenderness
Decreased use
Limp
Refusal to walk (woke up not wanting to walk)
Fever
Children may c/o their knee hurting when its actually their hip and vice versa.
Diagnosis:
Bloodwork:
For acute: Elevated ESR and CRP
WBC count may be non-specific (acute = elevated; chronic = may be normal)
Imaging:
Deep tissue swelling, periosteal elevation, lytic sclerosis.
Bone biopsy may be necessary.
Nursing Management:
Administer IV antibiotics. (for a long time)
Provide pain medications as needed.
Enforce activity restrictions and immobilization.
Provide post-op care after surgical debridement. (5 Ps)
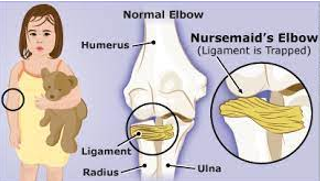
Radial Head Subluxation “Nursemaid’s Elbow”
Cause:
Caused by a pulling motion on the arm that stretches or tears the annular ligament surrounding the radial head, displacing the radial head.
Typically occurs in children under 5 years of age.
Injury Reduction Technique:
The elbow is flexed to 90 degrees, and then the forearm is fully and firmly supinated.
Clinical Manifestations:
Holds the affected arm close to the body.
Pain with forearm supination is always present.
No obvious deformity, PNV (peripheral neurovascular) compromise, bony tenderness, or swelling.
History of the arm being pulled.
The ligament becomes entrapped within the joint, preventing spontaneous reduction.
Nursing Measures:
Provide education and reassurance for the child and parents.
May need to assist with the reduction.
Administer pain medication as needed.
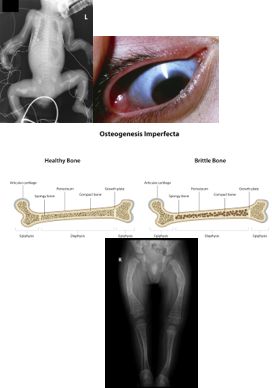
Osteogenesis Imperfecta
Genetic bone disorder with an autosomal dominant inheritance pattern that affects collagen type I production:
Low bone mass
Increased bone fragility
Connective tissue problems; unstable joints.
The estimated incidence is approximately 1 in every 12,000 to 15,000 births.
Occurs equally among males and females, and across races and ethnic groups.
Fractures may persist into adulthood.
Physical Characteristics:
**Blue sclera:
The most common ocular sign.
Caused by thin scleral collagen, allowing the underlying darker choroid vasculature to be seen.
Patients with OI show reduced thickness of corneal and scleral collagen fibers, resulting in low ocular rigidity.
Hearing loss
Frequent fractures
Short stature
Fragile dentition
Treatment:
Goal is to decrease fracture incidence and maintain mobility.
Bisphosphonate administration to promote bone growth.
Zebra lines are evidence of bisphosphonate treatment.
Physical therapy/occupational therapy to prevent contractures and maximize mobility.
Standing with bracing is encouraged.
Severe cases may require surgical insertion of rods into the long bones.
Lightweight splints or braces may allow the child to bear weight earlier.
Developmental Dysplasia of the Hip (DDH)
Formerly called congenital hip dysplasia or congenital dislocation of the hip
Femoral head is displaced from the acetabulum
Risk Factors:
Firstborn
Breech presentation
Female
Family history of DDH
Diagnosis:
Physical examination shows asymmetric thigh or gluteal folds
Barlow Test, Ortolani Test, Galeazzi Test
Ultrasound if < 6 months old
X-ray if > 6 months old
Therapeutic Management:
Goal: maintain hip joint in reduction so the femoral head and acetabulum can develop properly
Pavlik Harness (< 6 months):
Used full-time, do not remove!!
Worn for approximately 3 months if started at a young age
Closed Reduction (> 6 months):
Used for older infants/toddlers
Followed by a spica cast after reduction
Nursing Management:
Educate parents on Pavlik harness care and assess the skin
Provide education and care for surgical reduction

Pavlik Harness Education
Do not adjust the harness without checking with the physician or nurse practitioner first.
Until your physician or nurse practitioner instructs you to remove the harness for periods during the day, it must be worn continuously (for the first week or sometimes longer).
Change your baby’s diaper while they are in the harness.
Place your baby on their back to sleep.
Check skin folds, especially behind the knees and in the diaper area, for redness, irritation, or breakdown; keep these areas dry and clean.
Once your baby is permitted to be out of the harness for short periods, you may bathe your baby while the harness is off.
Long knee socks and an undershirt are recommended to prevent skin irritation from the brace.
Note the strap markings to ensure proper harness placement.
Wash the harness by hand with mild detergent and air dry. If using a dryer, use the air fluff setting only (no heat).
Call the doctor if:
Your baby’s feet are swollen or bluish.
The harness appears too small.
Skin is raw or there is a severe rash.
Your baby is unable to actively kick their legs.

Congenital Clubfoot—Congenital Talipes Equinovarus
Structural foot deformity present at birth.
Etiology is unknown, but may be associated with certain syndromes or neurogenic disorders.
A congenital anomaly occurring in approximately 1 out of 1,000 live births.
The foot is excessively plantar-flexed, with the forefoot swinging medially and the sole facing inward. It cannot be moved into the normal midline position.
The deformity resembles a golf club head.
Complications:
Rocker-bottom deformity
Awkward gait
Epiphyseal disturbance
Nursing Management:
Cast care for serial casting (in stages)
Post-operative care if surgery is needed
Education and support for the family

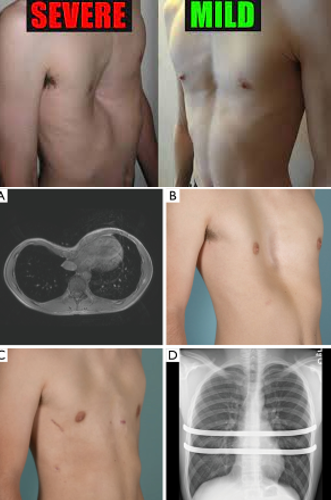
Pectus Excavatum
Funnel-shaped chest:
Depression that sinks inward at the xiphoid process.
Worsens as the child grows.
Cardiac and pulmonary compression can occur in severe cases:
Shortness of breath (SOB)
Exercise intolerance
Surgery may be required if the condition is severe.
Nursing Management:
Perform respiratory assessments.
Provide wound care postoperatively if surgery is done.
Manage pain effectively.
Kyphosis
Lateral convex angulation of the thoracic spine.
Treatment options:
Exercises
Bracing
Physical therapy
Surgical spinal fusion, if indicated

Lordosis
Lateral inward curve of the cervical or lumbar spine.
Treatment options:
Weight loss
Correction of underlying deformity
Targeted exercises
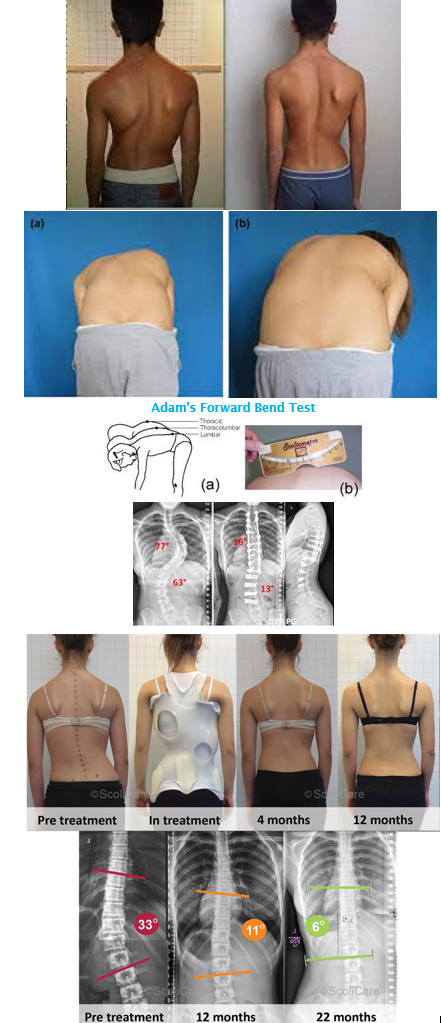
Scoliosis
Lateral curvature of the spine > 10 degrees.
If > 70 degrees, it may cause cardiopulmonary dysfunction due to alterations in the thoracic cage.
Causes:
Idiopathic (infantile, juvenile, adolescent)
Congenital (results from anomalous vertebral development)
Neuromuscular (associated with neuromuscular or muscular diseases such as cerebral palsy, myelomeningocele, spinal cord tumors, spinal muscular atrophy, and muscular dystrophies)
Screening:
Adam’s Forward Bend Test
Diagnosis:
Physical examination and full spine X-rays
Determine underlying cause (idiopathic, congenital, or neuromuscular)
Treatment:
Bracing or Spinal Fusion
Treatment depends on the degree of curvature and skeletal maturity:
If the curve is < 25 degrees, the doctor may observe the curve and repeat X-rays to monitor progression.
If the curve is between 25 and 45 degrees and the child still has growth remaining, bracing may be considered to prevent progression.
If the curve is > 50 degrees, surgery may be recommended.
Post-Operative Care (for spinal fusion > 50 degrees):
Monitor hemodynamic status
Pain management
Early ambulation
Physical therapy
Logrolling
Neurovascular checks
Monitor for infection of surgical hardware
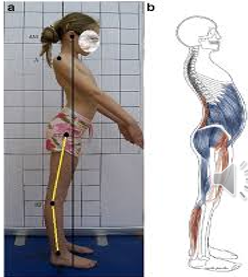
Duchenne Muscular Dystrophy
Inherited progressive myopathic disorder resulting from a defective gene located on the X chromosome that is responsible for the production of dystrophin.
X-linked Recessive
Symptoms:
Muscle Weakness:
Typically occurs at 2 to 3 years of age
Progresses from proximal to distal limb muscles
Affects lower extremities before upper extremities
Children are typically wheelchair-bound by approximately 12 years of age
Decreased endurance; unable to keep up with peers
Toe walking, calf hypertrophy
Muscle cramping
Heart failure and arrhythmias occur late in the disease
Scoliosis—leads to poor pulmonary function
Developmental delays are common
May also present with ADHD, OCD, anxiety, and autism
Diagnosis:
Elevated creatine kinase (CK) levels
Muscle biopsy for definitive diagnosis (shows absence of dystrophin)
**Gower’s Sign (as shown in picture—uses hands to "walk up" the legs when standing from a sitting or lying position)
Treatment:
Administer corticosteroids and calcium/vitamin D supplements
Promote mobility
Assess and maintain cardiopulmonary function
Provide support (chronic, progressive disease)
