Fielding Chapter 23: Blood and Blood Product Transfusions in Horses
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
What is the function of a blood transfusion in blood loss?
Serves to restore blood volume as well as oxygen-carrying capacity
Clinical Signs that May Indicate Need for a Blood Transfusion
Pale mucous membranes, tachycardia, tachypnea, sweating, colic, and lethargy may indicate a need for blood transfusion, especially when blood loss is estimated to be greater than 30% of blood volume
Acute blood loss can result in hypovolemic shock in addition to loss of red cell mass so findings may also include cold extremities, hypotension, and increased blood lactate concentrations
PCV in Severe, Acute Hemorrhage
PCV can still be normal during severe, acute hemorrhage
PCV and TP will decrease as fluid redistributes from the interstitial to the intravascular space over the first 12 hours after hemorrhage
If IVF are given for resuscitation, the PCV and TP will decrease more rapidly
TP will decrease before PCV decreases substantially, since splenic contraction initially increases the PCV
Blood transfusion is likely needed if the PCV drops below 20-25% during an acute bleeding episode
Loss of what % of blood generally requires transfusion?
More than 30% of blood volume
Stage I Shock % Blood Loss
Up to 15%
Stage I Shock Heart Rate
Normal to minimal increase
Stage I Shock Respiratory Rate
Normal
Stage I Shock Capillary Refill Time
Normal
Stage I Shock Blood Pressure
Normal
Stage I Shock Urine Output
Normal
Stage I Shock Other Physical Exam Findings
Possible mild anxiety
Stage II Shock % Blood Loss
15-30%
Stage II Shock Heart Rate
Increased
Stage II Shock Respiratory Rate
Increased
Stage II Shock Capillary Refill Time
Mildly prolonged
Stage II Shock Blood Pressure
Normal
Stage II Shock Urine Output
Mildly decreased
Stage II Shock Other Physical Exam Findings
Mild anxiety
Stage III Shock % Blood Loss
30-40%
Stage III Shock Heart Rate
Moderate to Severely Increased
Stage III Shock Respiratory Rate
Increased
Stage III Shock Capillary Refill Time
Prolonged
Stage III Shock Blood Pressure
Decreased
Stage III Shock Urine Output
Decreased
Stage III Shock Other Physical Exam Findings
Altered mentation; cool extremities
Stage IV Shock % Blood Loss
>40%
Stage IV Shock Heart Rate
Severely increased
Stage IV Shock Respiratory Rate
Increased
Stage IV Shock Capillary Refill Time
Absent, very pale mucous membranes
Stage IV Shock Blood Pressure
Severe Hypotension
Stage IV Shock Urine Output
Negligible
Stage IV Shock Other Physical Exam Findings
Obtunded; cool extremities
Indications of Blood Loss in Anesthetized Horses
In anesthetized horses, heart rate and PCV may be very stable so pale MM with prolonged CRT, decreasing TP, hypotension, and hypoxemia are better indicators of blood loss in horses
Oxygenation Status to Determine the Need for Blood Transfusion
Oxygenation status can help to determine the need for blood transfusion in cases of both acute hemorrhage and chronic anemia
Lactate to Determine the Need for a Blood Transfusion
A rise in blood lactate concentration despite volume replacement with crystalloid or colloid fluids may indicated continued tissue hypoxia and a need for blood transfusion
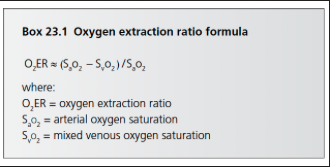
What oxygen extraction ratio in the context of blood loss may indicate the need for blood transfusion?
A ratio of 40%
Oxygen Extraction Ratio Equation
PCV and TP to Determine Need for a Blood Transfusion in Chronic and Hemolytic Anemias
PCV and TP can be more useful indicators of the need for blood transfusion in chronic and hemolytic anemias
In chronic anemia cases, a PCV of less than 12-15%, especially with physical examination findings such as pale mucous membranes, tachycardia, tachypnea, and lethargy, represents an indication for blood transfusion
Transfusions may need to be given to patients with a higher PCV if they have concurrent disease such as respiratory conditions or sepsis
Hemoglobin-Based Oxygen Carriers (HBOCs)
Blood substitutes consisting of polymerized hemoglobin that are given to increase oxygen-carrying capacity in patients with moderate to severe anemia
Oxyglobin - HBOC produced with hemoglobin of bovine origin
Indications for Plasma Product Transfusion
Plasma transfusion is indicated for the treatment of clotting factor deficiency, hypoalbuminemia, decreased colloid osmotic pressure, and failure of transfer of passive immunity
Can be used for colloid support when the TP is less than 4.0 g/dL, serum albumin concentration is less than 2.0 g/dL, or colloid oncotic pressure is less than 14 mmHg acutely
If clotting factors and albumin are not needed, synthetic colloids such as hydroxyethyl starch may be preferred for colloid support
Commercially available hyperimmune plasma has very high IgG concentrations (1500-2500 mg/dL), plasma from local donor horses may provide better protection against specific local pathogens
For animals with von Willebrand disease, cryoprecipitate may be used since it contain more concentrated von Willebrand factor (as well as factor VIII, fibrinogen, factor XIII, and fibronectin
Typically administered to a patient with known deficiency that needs to undergo a surgical procedure or is having life-threatening bleeding associated with primary hemostatic dysfunction
Equine cryoprecipitate is not a commercially available product
What do fresh and fresh frozen plasma contain?
Fresh and fresh frozen plasma (FFP) contain immunoglobulins, coagulation factors (fibrinogen and factors II, VII, IX, X, XI, and XII) and cofactors (factors V and VIII) as well as the anticoagulant proteins antithrombin, protein C, and protein S
Indications for Platelet Transfusion
Indicated for patients with severe thrombocytopenia and life-threatening hemorrhage or a need for surgical intervention
Platelet transfusion should be considered with a platelet count of less than 20,000/uL in the presence of risk factors for bleeding
May be less beneficial for patients with immune-mediated thrombocytopenia since the transfused platelets will be rapidly destroyed so are reserved for use as a stop-gap measure in extreme circumstances
Fresh whole blood can also provide platelets and may be the ideal choice for patients that require RBCs and platelets
Will not generally provide platelet concentrations high enough to treat severe thrombocytopenia and may provide excess RBCs for patients that require chronic platelet therapy
For patients with primary thrombocytopenia or thrombocytopathia, platelet concentrates can be given
Can be obtained by plateletpheresis or centrifugation using a slow-spin technique
How many equine blood groups and factors are there?
8 recognized equine blood groups and 30 different factors identified within 7 of these groups
Is there a universal blood donor for horses?
No
Ideal Blood Donor
Healthy young gelding weighing at least 500 kg
Disease Testing for Blood Donors
Donors should be up to date on vaccinations and tested annually for EIA
Donors that are used for USDA-licensed plasma products must also be tested for piroplasmosis, dourine, glanders, and brucellosis
What are the most immunogenic RBC antigens?
RBC antigens Aa and Qa are the most immunogenic and have been commonly associated with neonatal isoerythrolysis so the ideal donor should lack the Aa and Qa alloantigens
What horses are not suitable as blood donors?
Horses that have received blood or plasma transfusions and mares that have had foals are not suitable as donors because they have a higher risk of carrying RBC alloantibodies
Donkeys or mules should not be used as donors for horses because they have a RBC antigen known as "donkey factor" which isn't present in horses, transfused horses can develop anti-donkey factor antibodies
What must be done in order to use the mare of a foal with NI as a blood donor?
For foals with NI, the mare can be used as a blood donor, but the RBCs must be washed prior to transfusion
Life Span of Transfused Autologous RBCs vs Allogenic Blood
Life span of transfused autologous RBCs after 28 days of storage is approximately 30 days, compared to a 20 day half life for fresh, crossmatched, blood-typed, allogenic blood
How soon do horses develop alloantibodies to RBCs?
Horses can develop alloantibodies within 1 week of transfusion so blood typing and crossmatching are recommended before a second transfusion is performed
A second blood transfusion may be performed safely within 2-3 days of the first transfusion without a blood crossmatch
Blood Typing
Blood typing involves the use of antisera to detect specific RBC antibodies
Blood typing is time consuming and laboratories performing blood typing are very limited this is not often a practical method of donor selection
More important for horses for which subsequent blood transfusions are anticipated and for broodmares that may produce foals with NI if sensitized to other blood group factors
Antibody Screening
Donor animals should ideally be screened for alloantibodies yearly
Naturally occurring anti-Aa and anti-Ac antibodies can be found in horses and are usually agglutinin antibodies; Mares that have been previously sensitized may have anti-Aa hemolysins as well
Antibody screens are routinely performed in mares that may be at risk of having anti-RBC antibodies to the foal's blood type and therefore at risk of causing NI
What type of reactions does hemagglutination crossmatch test for?
Evaluates for agglutination reactions but not hemolytic reactions
Major Crossmatch
Detects agglutination reactions between the donor’s RBCs and the recipient’s plasma
Minor Crossmatch
Detects agglutination reactions between the donor’s plasma and the recipient’s RBCs
Saline Dispersion Test
May be difficult to determine agglutination because of rouleau
Normal rouleaux should disperse when a small amount of saline is mixed with the blood whereas agglutination will not disperse
Crossmatch Procedure
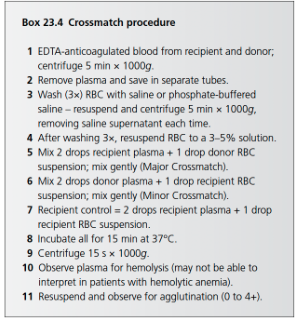
How to test for hemolytic transfusion reactions?
Rabbit complement can be added to the reaction mixture for hemolytic testing but this is not routinely performed
Also does not accurately predict the lifespan of the transfused red cell or the development of antibodies to the transfused RBCs and transfusion reactions have been reported even with a compatible crossmatch
Can a blood transfusion still be performed if the minor crossmatch is incompatible but the major crossmatch is compatible?
Yes, after washing the donor red blood cells and providing packed red blood cells
What should donor PCV be prior to blood donation?
Greater than 35%
What is the maximum amount of blood that can be collected from a horse?
20% of blood volume or approximately 16 ml/kg body weight
What should volume replacement with IV crystalloid fluids be given to blood donor horses?
When 15% or more of the blood donor’s volume is collected
How long after blood donation should blood donor’s vitals normalize?
Within 1 hour of collection
Why are glass bottles not recommended for blood collection?
Glass inactivates platelets and can damage the RBCs
Anticoagulant for when Blood is Collected for Immediate Transfusion
When blood is collected for immediate transfusion, anticoagulation with 32% sodium citrate is adequate (1:9 anticoagulant to blood ratio)
Anticoagulant for when Blood is Stored for Later Transfusion
When blood is stored for later transfusion, optimal pH and support of RBC metabolism are necessary to sustain RBC viability
Citrate-phosphate-dextrose (CPD) or citrate-phosphate-dextrose-adenine (CPDA) should be used
Anitcoagulant for Shed Blood Collected from Cavitary Hemorrhage
When shed blood is collected from cavitary hemorrhage, less anticoagulant is needed since the blood is already defibrinated
Recommend anticoagulant to shed blood range from 1:7 to 1:20
How can you determine if you have the proper blood to anticoagulant ratio?
Weigh the blood bags to ensure adequate fill
How long can WB stored in CPDA-1 bags be stored for?
Suggest that WB stored in CPDA-1 bags may be acceptable for transfusion after 3 weeks of storage
How long can RBC concentrates stored in saline-adenine-glucose-mannitol solution be stored for?
RBC concentrates stored in saline-adenine-glucose-mannitol solution may be suitable for transfusion for up to 35 days after collection
How do you wash RBCs
In order to separate the components, blood is centrifuged at 500 x g for 5 mins
Plasma is transferred to the satellite bag using a plasma extractor, and an additive solution is mixed with the PRBCs
For RBC washing, the RBC component is mixed with saline and centrifuged, supernatant removed, and this process is repeated twice more
How can plasma be prepared?
Plasma can be prepared by gravity sedimentation, centrifugation, or plasmapheresis
When larger volumes of plasma are desired without RBCs, plasmapheresis is the preferred technique as it is more rapid than WB collection and processing and results in plasma with minimal RBCs and leukocytes
How much and how often can plasmapheresis be performed?
4-11L every 30 days
Fresh Plasma
Plasma that is used within 8 hours of collection
Fresh Frozen Plasma
Plasma placed in a freezer within 8 hours of collection
How soon after freezing should FFP be used?
FFP should be used within 1 year of freezing to ensure optimal clotting factor activity
Frozen Plasma
Plasma that is frozen more than 8 hours after collection or is more than 1 year old
What is decreased in frozen plasma compared to fresh frozen plasma?
Labile clotting factors, factor V and factor VIII
What is the shelf lfie for immunoglobulin efficacy in hyperimmune plasma
2-3 years
What is necessary for platelets to be present in whole blood?
Blood stored at room temperature and transfused within 8 hours
How is platelet rich plasma created?
Plasma is centrifuged in a “soft spin”
How is platelet concentrate created?
Further centrifugation of PRP or by platelet pheresis
How long after collection should platelet concentrate be used?
Must be stored at room temperature and should be used within 5-7 days
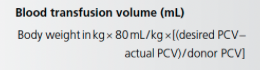
Blood Transfusion Volume Equation
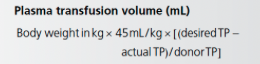
Plasma Transfusion Volume Equation
What % of blood lost should be transfused in acute hemorrhage?
In situations of acute hemorrhage, an estimate of blood loss is based on clinical parameters and between 25 and 50% of the total blood lost should be replaced by transfusion since much of the circulating volume will be replaced by fluid shifts
What are reasons PCV may not increase after transfusion?
PCV may not increase after transfusion in cases of hemorrhagic anemia likely due to endogenous fluid shift, IV fluid resuscitation, and possibly continued hemorrhage
What % of RBCs lost into a body cavity are autotransfused back into circulation within 24-72 hours?
Up to 75%
What is the starting point for treatment of coagulopathy?
A starting point for treatment of coagulopathy is approximately 4-5 ml/kg plasma
Follow up monitoring with hemostatic testing is recommended to help determine the endpoint of treatment
How can you determine the volume of plasma needed in a foal with FPT?
Volume of plasma needed in a foal with FPT can be determined if the IgG concentration of the foal and the plasma are known
A dose of 20 ml/kg of plasma (IgG approximately 1200 mg/dL) will generally raise the foal's IgG concentration by 200-300 mg/dL
How often should the administration filter be changed during blood product transfusion?
Every 2-4 units of blood
Transfusion technique
Refrigerated blood can be transfused directly as warming may cause further deterioration of RBCs
Blood should not be given concurrently with hyper- or hypotonic solutions and should not be given with calcium containing solutions as the citrate anticoagulant will bind calcium in the fluids and no longer be an effective anticoagulant
Blood products should be given slowly for the first 10-20 minutes so the animal can be monitored closely for signs of transfusion reaction and transfusion can be stopped if needed
Give 0.3 ml/kg (over 10-20 min) and the rate can then be increased if needed
Rate of transfusion will depend on the patient's volume status and can be as high as 20-40 ml/kg/h
Not recommended to exceed 2-4 ml/kg/h in patients with significant cardiac disease
Transfusion should be completed within 4 hours to prevent bacterial growth and ensure functional platelets
What is the incidence of adverse reactions with plasma transfusion?
0-10%
What is the incidence for blood transfusion reactions?
16% with 2% having a fatal anaphylactic reaction
Acute Hemolytic Transfusion Reaction
Can appear during the transfusion or within hours of the transfusion
Typically requires pre-existing antibodies and is classified as a cytotoxic (type II) hypersensitivity
Clinical signs include hemoglobinemia, hemoglobinuria, and progressive anemia or lack of increase in PCV
Highly inflammatory nature can lead to signs of systemic inflammatory response, DIC, shock, cardiovascular collapse, and death
Severity of signs is directly related to the volume of transfused blood
AKI may result from hemoglobinuria and IVF is indicated to protect the kidneys
What may you see with a delayed transfusion reaction?
Delayed transfusion reaction may be recognized by an unexpected decline in PCV following transfusion, hyperbilirubinemia, and possibly fever
What transfusion administration errors can lead to RBC destruction?
Improper storge, excessive warming of the blood, administration with hypertonic solutions, and administration using pumps can all lead to RBC destruction
Non-Hemolytic Transfusion Reactions
Non-hemolytic reactions such as fever an allergic reactions are the most common reactions seen
Fever may be related to donor leukocytes and accumulation of pyrogenic cytokines in the blood over time - older units more likely to cause this response
Tranfusion Reactions from Acute Allergic (Type I) Hypersensitivty
Transfusion reactions from acute allergic (type I) hypersensitivity can include muscle fasciculation, urticaria, pruritis, anaphylaxis, sweating, and pyloerection