GI 6 - Bile acids, Small Intestine (+ absorption)
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
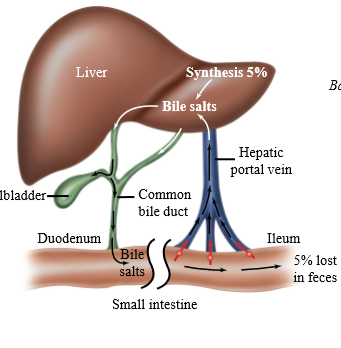
Bile acid recycling
20 to 40g of bile acids are released into the intestine each day. Only 0.5g are lost in feces (95% recovered)
Where does bile acid recycling ocur
Enterohepatic circulation
Movement of bile in GI system
1. Bile acid produced by hepatocytes, and secreted into the canalicular networks (increasing size) until it reaches common bile duct
2. Bile acids are stored in the gall bladder, or secreted into the duodenum
3. Bile acids move through the SI to the ileum
4. Ileum absorbs bile acids, portal vein brings them back to the liver

Why is bile acid reabsorbed and not just completely excrete?
Having a pool ready to secrete allows for a better secretion rate
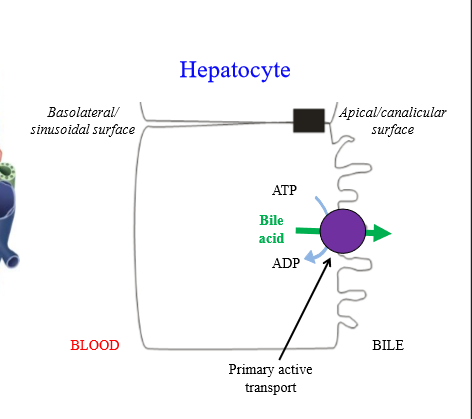
Step 1: Transport of bile acids from hepatocyte to bile
Bile synthesized in hepatocytes, moves across apical surface, and is secreted into canalicular networks, becoming bile ducts. Bile then goes into the SI or is stored in the gall bladder
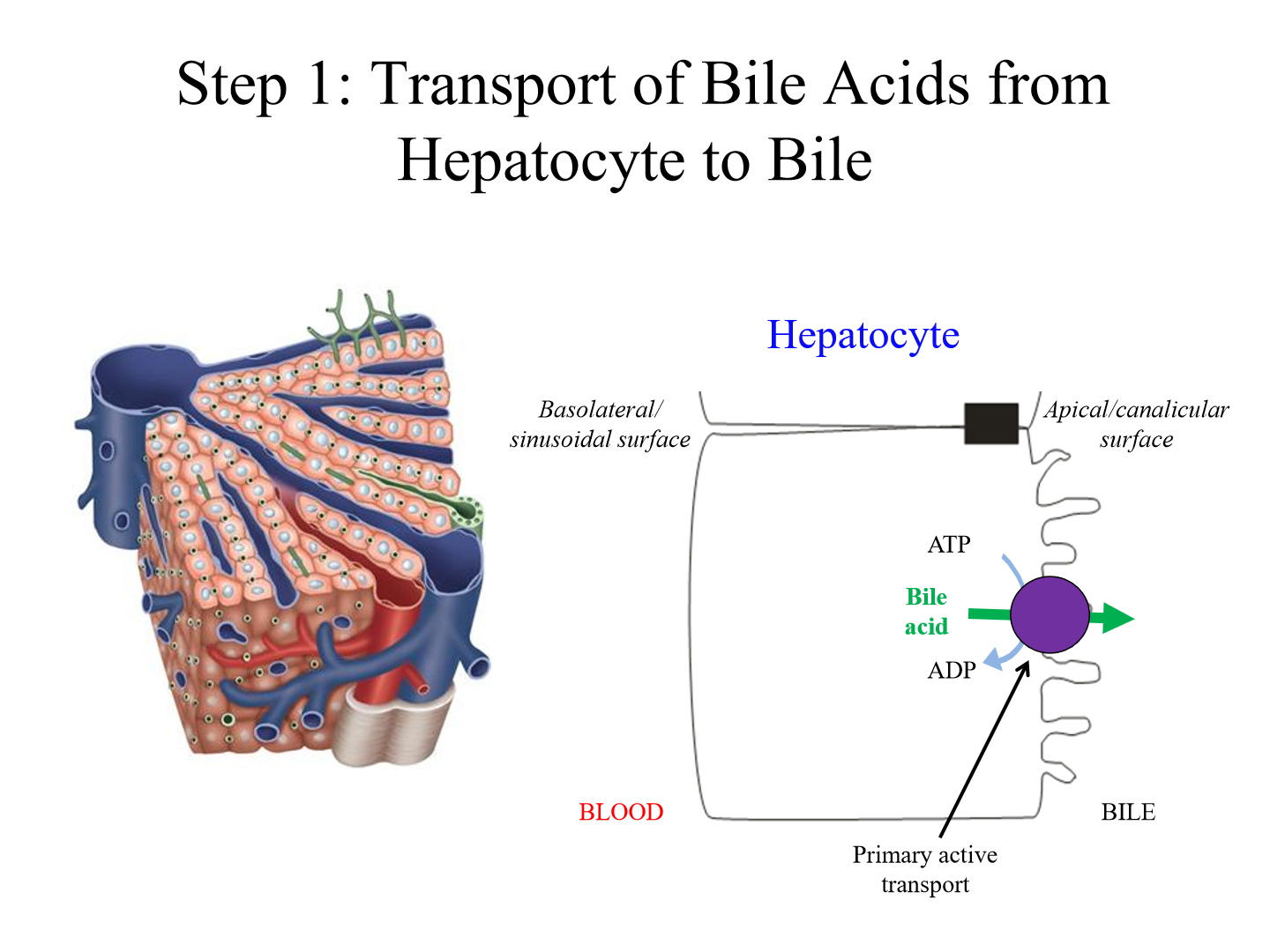
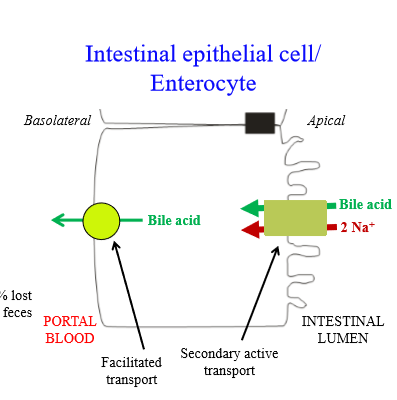
Mechanism of bile acid movement from hepatocytes into canalicular surface
Primary active transporter - ATP hydrolysis allows bile acid to move up concentration gradient. Canalicular networks have a high concentration of bile acid
Step 2: Bile acid reabsorption from the Ileum
Bile acids secreted into duodenum, digest fats, then move to ileum. The ileum reabsorbs bile acids into portal circulation by enterocytes
Mechanism of bile acid movement from lumen to enterocytes
Bile acid enters enterocytes via a secondary active transporter. Reabsorption is coupled to sodium movement into enterocyte
Mechanism of bile acid movement from the enterocyte into portal blood
Facilitated transport
Step 3: Transport of bile acids from blood into hepatocyte
Bile acids move in portal blood, and return to the hepatocytes. The bile acid secretion cycle can begin again
Mechanism of bile acid movement from portal blood into hepatocyte
Bile acid enters hepatocytes via a secondary active transporter. Movement is coupled to sodium movement into enterocyte
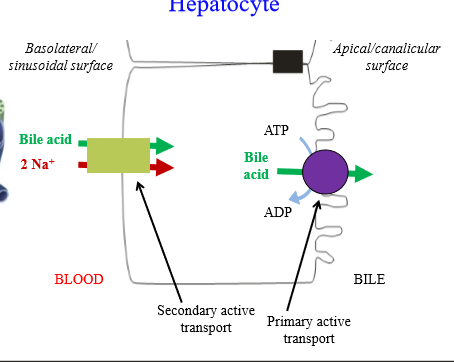
Summary of bile acid recycling (photo)
Role of dietary fiber
Sequesters bile acids, preventing them from cycling back to the liver (lost through feces). More bile acids have to be synthesized, lowering cholesterol levels in the blood
What would be the use if a drug entered the enterohepatic circulation?
Drug that effects enzyme would work well, as the whole dose is concentrated to the enterohepatic circulation
How is hepatobiliary secretion regulated during the intestinal phase?
By bile salts, secretin, and CCK
How does bile salts regulate hepatobiliary secretion?
As more bile salts are absorbed from ileum and return to liver, more will be secreted back into the bile. Bile salt synthesis is reduced when enterohepatic circulation is working well
How does secretin regulate hepatobiliary secretion?
Secretin is produced and released in duodenum S cells in response to acid. Secretin increases HCO3- secretion by bile duct cells (and the pancreas)
How does CCK regulate hepatobiliary secretion?
Fats and proteins in upper small intestine stimulate CCK release by I cell. CKKs increases gallbladder contraction and relaxes the sphincter of Oddi (hepatopancreatic sphincter), allowing for bile release into the duodenum
What are gallstones caused by
Excess cholesterol
How do gallstones form
Cholesterol is water insoluble - only kept in solution by micelles with bile acids and PLs
- If [cholesterol] > [bile acids], cholesterol precipitates out to form stone
What does cholesterol require to become a gallstone
A nucleating agent (protein, bacteria)
Pigment stones
Stones caused by excessive hemolysis, increasing bile pigment concentration in bile. Pigments precipitate with Ca2+
Consequences of gallstones
Depends on location - can cause obstruction, infection of gall bladder, liver pancreas.
Clinical manifestations of gallstones
Pain, nausea, jaundice, malabsorption of fats and fat-soluble vitamins
Treatment of gallstones
- Cholecystectomy (remove gall bladder): requires a reduction of fat in diet
- Removal of gallstones
- Drugs to dissolve gallstones
Location of small intestine
Between the stomach and large intestine
Shape of small intestine
Tube of 2.4 cm in diameter, 3m in length
Why does the SI increase in size in autopsy
Loss of muscle tone
Sections of the small intestine
Duodenum (30cm), Jejunum (1m), Ileum (1.7m)
Functions of the duodenum
- Mixes pancreatic digestive enzymes and bile with food
- Absorption of nutrients, iron, calcium
- Release of endocrine hormones secretin and CCK
Functions of the jejunum
digestion and absorption. Most of the chyme entering SI is digested and absorbed within first 25% of intestine
Functions of the ileum
Digestion and absorption - absorbs bile acids (secondary transporter) and vitamin B12
Pyloric sphincter
Controls passage of food from stomach to small intestine

How is SA increased in small intestine
SI has circular folds - layers of intestine that fold on itself. The circular folds are covered in villi: projection of tissue into the lumen.
- SI also has crypts, whcih increases surface area
- Villi covered in epithelial cells with microvilli projections for increased SA
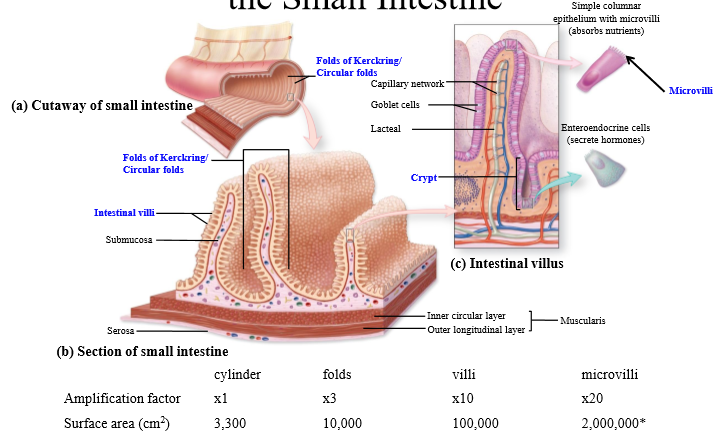
Total surface are of small intestine
Around 1-2 million cm^2
Structure of the villus
- Apical layer consists of brush-border epithelial cells
- Crypts are invaginations of the epithelium - stem cells in crypts divide into epithelial cells, allowing top layer of cells to slough off
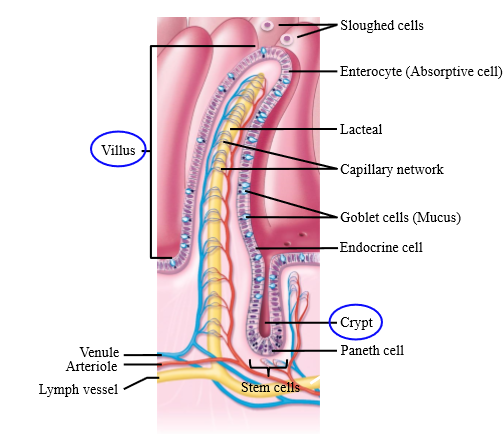
Cells that arise from small intestine crypts
Enterocytes, Goblet cells, enteroendocrine cell, paneth cell
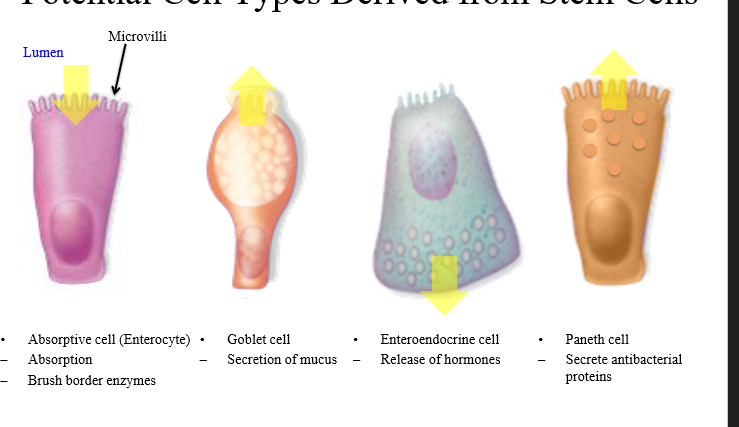
Enterocyte function
Absorptive cell - contains microvilli on lumen (brush border with brush border enzymes)
Goblet cell function
Secretes mucus for food lubrication, and acts as buffer for amount of acid entering SI from stomach
Enteroendocrine cell function
Reease secretin and CCK - are either S or I cells (respectively)
Paneth cells function
Secrete antibacterial proteins to protect GI tract from bad bacteria
Brush border
small projections (microvilli) of epithelial cells covering the villi of the small intestine; major absorptive surface of the small intestine
Brush border enzyme
Enzyme anchored to the brush b order with catalytic activity in the lumen - used to break down carbs and peptides into sugars and amino acids prior to transport across the enterocyte
Initial breakdown of starch
Starch (amylose and amylopectin) are broken down into maltose, maltotriose, a-limit dextrin by salivary and pancreatic amylases. Need further digestion to monosaccharides for absorption
Small intestine breakdown of starch
Brush border enzymes break down maltose, maltotriose, and a-limit dextrin into glucose
Brush border enzymes that break down polysaccharides
Maltase, Sucrase, a-dextrinase
What enzyme(s) breaks down maltose or maltotriose
Either maltase, sucrase, or a-dextrinase break them down to glucose, cleaving the alpha 1-4 bond
What enzyme breaks down a-dextrin
a-dextrinase breaks it down to glucose, cleaving the alpha 1-6 bond
Other sugars in diet other than starch
Sucrose (table sugar), lactose
Enzyme to break down sucrose
Sucrase breaks sucrose into glucose and fructose (brush border enzyme)
Enzyme to break down lactose
Lactase breaks lactose into glucose and galactose (brush border enzyme)
What causes lactose intolerance
Lower amount of lactase enzymes in small intestine
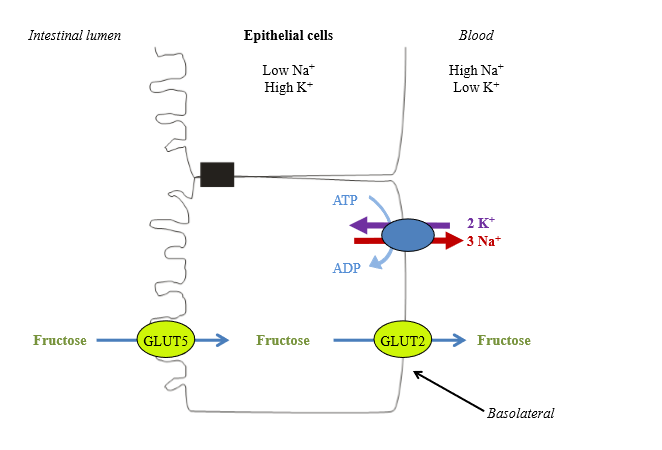
How does the small intestine absorb glucose/galactose
- Carried into enterocyte by sodium dependent glucose transporter (SGLT)
- Secondary active transport pathway - uses sodium gradient to drive glucose absorption
- Sodium gradient facilitated by Na+/K+ ATPase
- Sodium moves into basolateral surface by GLUT transporter
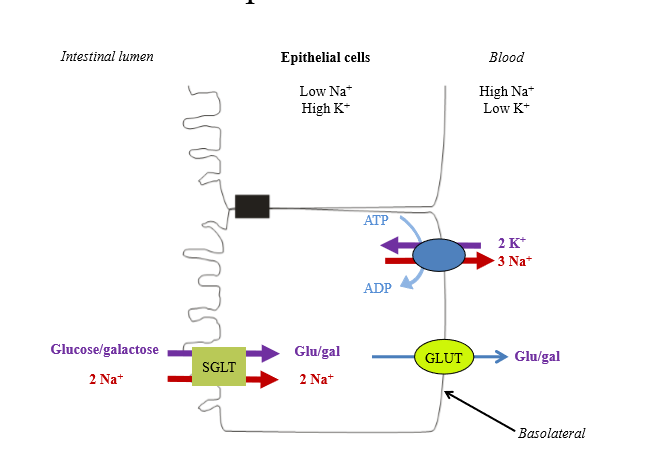
How does the small intestine absorb fructose
- Enter cell via facilitated carrier GLUT5
- At basolateral surface, leave via facilitated carrier GLUT2
- Enters blood
Full overview of carbohydrate absorption
• Pancreatic amylase breaks down polysaccharides into 3 products (maltose, maltotriose, a-limit dextrins)
• Brush border enzymes break down polysaccharides down into glucose, fructose, galactose
○ Fructose carried by GLUT
○ Glucose and galactose carried by SGLT transporter (secondary active transport)
• Move through basolateral membrane of enterocyte by GLUT transporter

Initial digestion of proteins in stomach
Proteins are broken into peptides by stomach. They are further broken down into amino acids by pancreatic proteases
What enzymes break down peptides to amino acids?
- Carboxypeptidase (pancreatic protease)
- Aminopeptidase (brush border enzyme)
- Other brash border enzymes
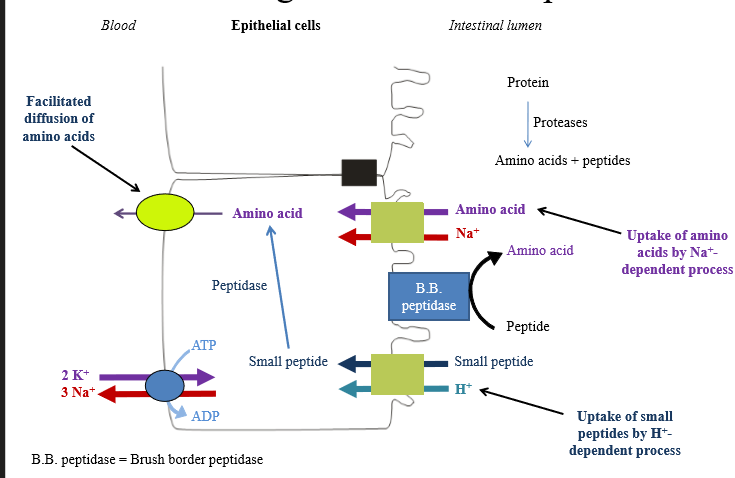
How are free amino acids absorbed into enterocytes
Secondary active transport coupled to Na+ (multiple transport prtoeins)
Peptide absorption into enterocytes
Small peptides are absorbed by different secondary active transport proteins coupled to H+. Peptidases intracellularly will break down product
General pathway of protein digestion and absorption
• Pepsin in stomach starts acting on proteins
○ Pepsinogen released by chief cells, activated by acidic environment
• Pancreatic proteases continues to break down peptides into amino acids and peptides
• Brush border peptidases cleave peptides into AA's
• AA's can be taken up into enterocytes via Secondary active transport coupled to sodium
• Alternatively - small peptides are taken into cell via secondary active transport coupled to protons
○ Small peptides are cleaved by intracellular peptidases into amino acids
• Amino acids leave enterocyte via facilitated diffusion into interstitial space for bloodstream absorption