biochem carbohydrate metabolism II
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
what are the 3 energy generating fuels stored in a 70kg human body
1. carbs (in the form of glycogen; muscle and liver) = <1%
2. fat (triglcerides; in adipose tissue) = 85%
3. protein (muscle protein) = 15%
what is the order of preference fuel usage by tissues in normal physiological conditions
1. carbs
2. fats
3. proteins
why are carbs the most preferred energy source?
- all tissues receive blood; blood contains glucose
- all tissues can metabolize glucose (either aerobically or anerobically)
- more importantly, RBC and brain are dependent on glucose
therefore, glucose is more preferred for energy generation and maintaining basal levels of blood glucose
fats (3)
- can be stored in large amounts in small volume
- fatty acids (energy providing component of fats) can NOT be converted to glucose
- can NOT be metabolized aerobically
proteins (1)
needed for cellular and structural functions
what is the percentage of tissue weight of liver glycogen
5.0 - 10.0
what is the tissue weight of liver glycogen
1.8 kg
what is the body content of liver glycogen
100-150 g
what is the percentage of tissue weight of muscle glycogen
1.0-2.0
what is the tissue weight of muscle glycogen
35 kg
what is the body content of muscle glycogen
250-400 g
what is the percentage of tissue weight of extracellular glucose
0.1
what is the tissue weight of extracellular glucose
10 L
what is the body content of extracellular glycose
10 g
how will the amounts of stored glycogen be altered
form glycogen storage disorders
what is the difference between the storage of glycogen in the muscle and liver
- muscle glycogen is readily available source of glucose for glycolysis within the muscle (ONLY useful for muscles)
liver glycogen stores increase in fed state
- 12-18 hrs of fasting causes complete depletion of liver glycogen
- liver glycogen function is to release glucose in fasting state (between meals) to maintain blood glucose levels to support basal function of tissues
what is the purpose of the extensive branches of glycogen (3)
1. enhances solubility
2. acceleration of synthesis
3. increased sites for degradation
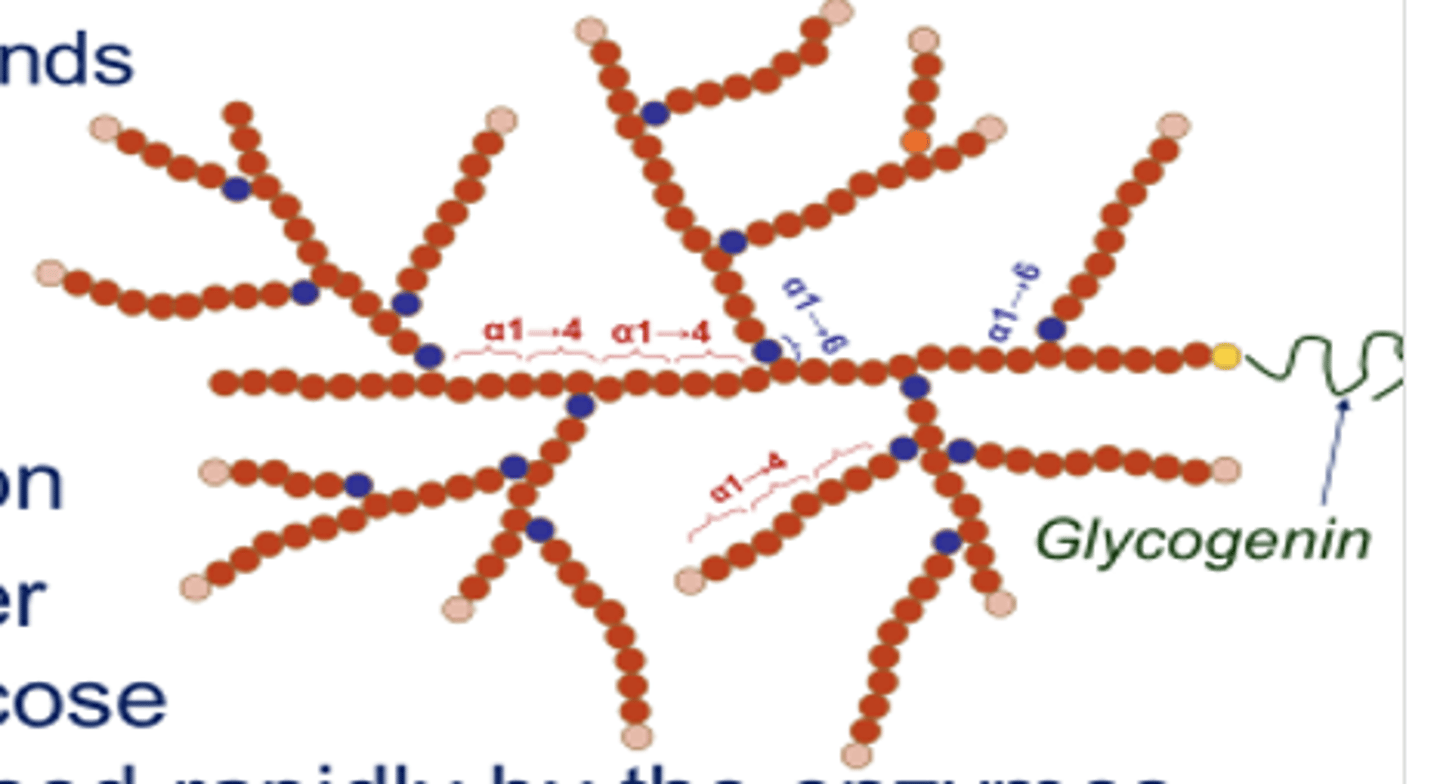
how does branching work and what does it help with
it increases the number of non-reducing sites
- new glucose residues can be added or released rapidly by the enzymes during synthesis and breakdown respectively
where does the synthesis of glycogen (glycogenesis) occur
cytosol
what is needed for the initiation of glycogenesis
preexisting piece of glycogen / primer (also known as a glycogenin)
- a protein with autocatalytic activity that is capable of synthesizing a piece of glycogen
what is the 1st step of glycogenesis
glucose to glucose 6-PO4 to glucose 1-PO4
what catalyzes the reaction of glucose to glucose 6-PO4 (in the liver and in muscle)
liver = glucokinase
muscle = hexokinase
what catalyzes the reaction of glucose 6-PO4 to glucose 1-PO4 (in the liver and in muscle)
phosphoglucomutase
what is the 2nd step of glycogenesis
formation of UDP-glucose
what catalyzes the formation of UDP glucose form glucose 1-PO4
UDP-glucose pyrophosphorylase (UTP ->PPi)
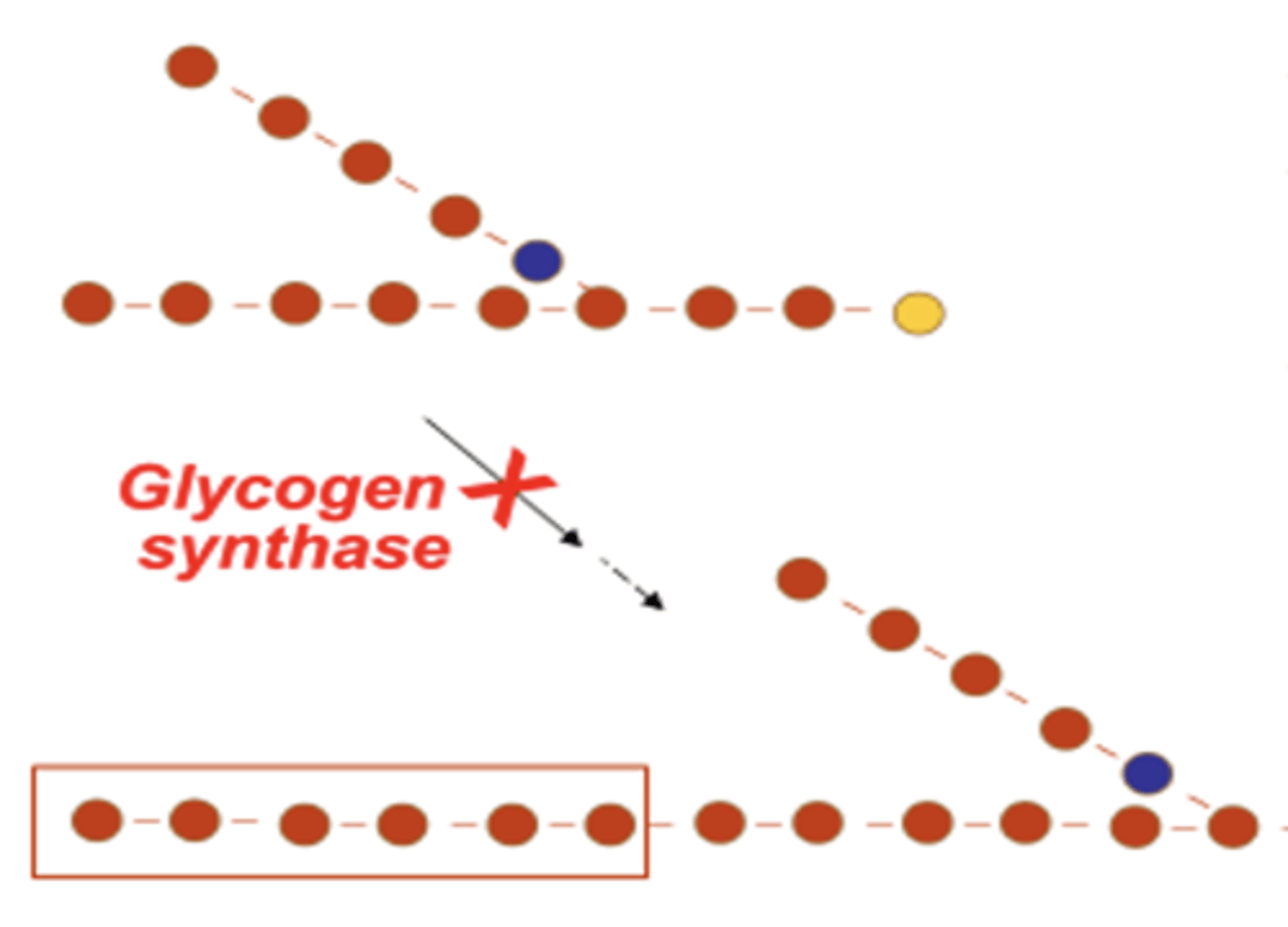
what is the 3rd step of glycogenesis
addition of glucoses for glycogen chain elongation by glycogen synthase (makes alpha 1 -> 4 linkages)
- forms an alpha 1 -> 4 glycosidic bond between UDP glucose and another glucose residue present in preexisting glycogen primer of glycogenin
*glycogen is elongated at non-reducing end by the addition of 8-10 glucoses
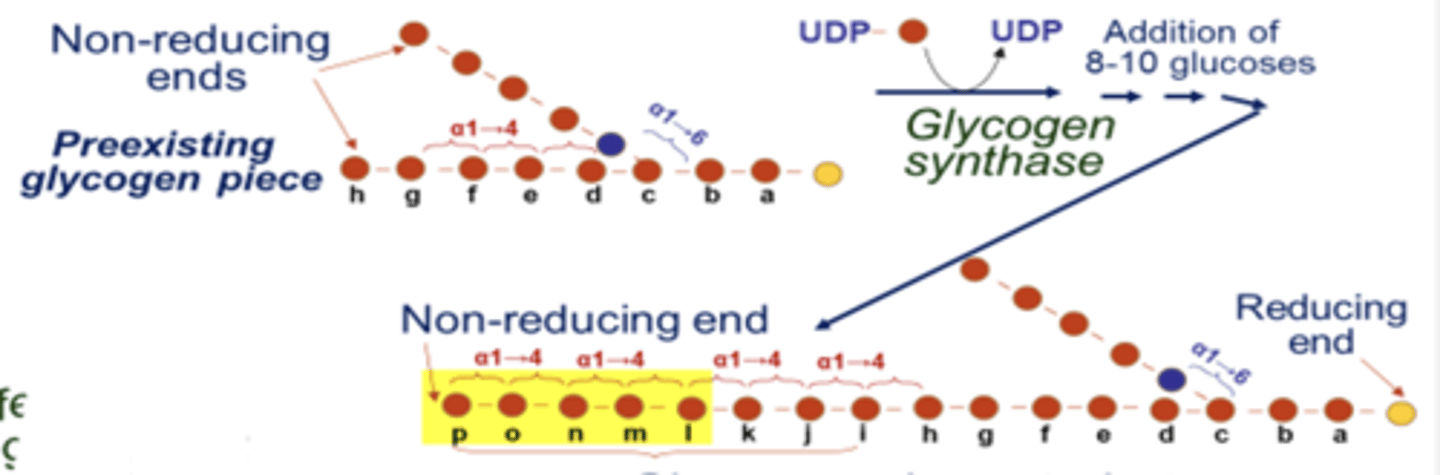
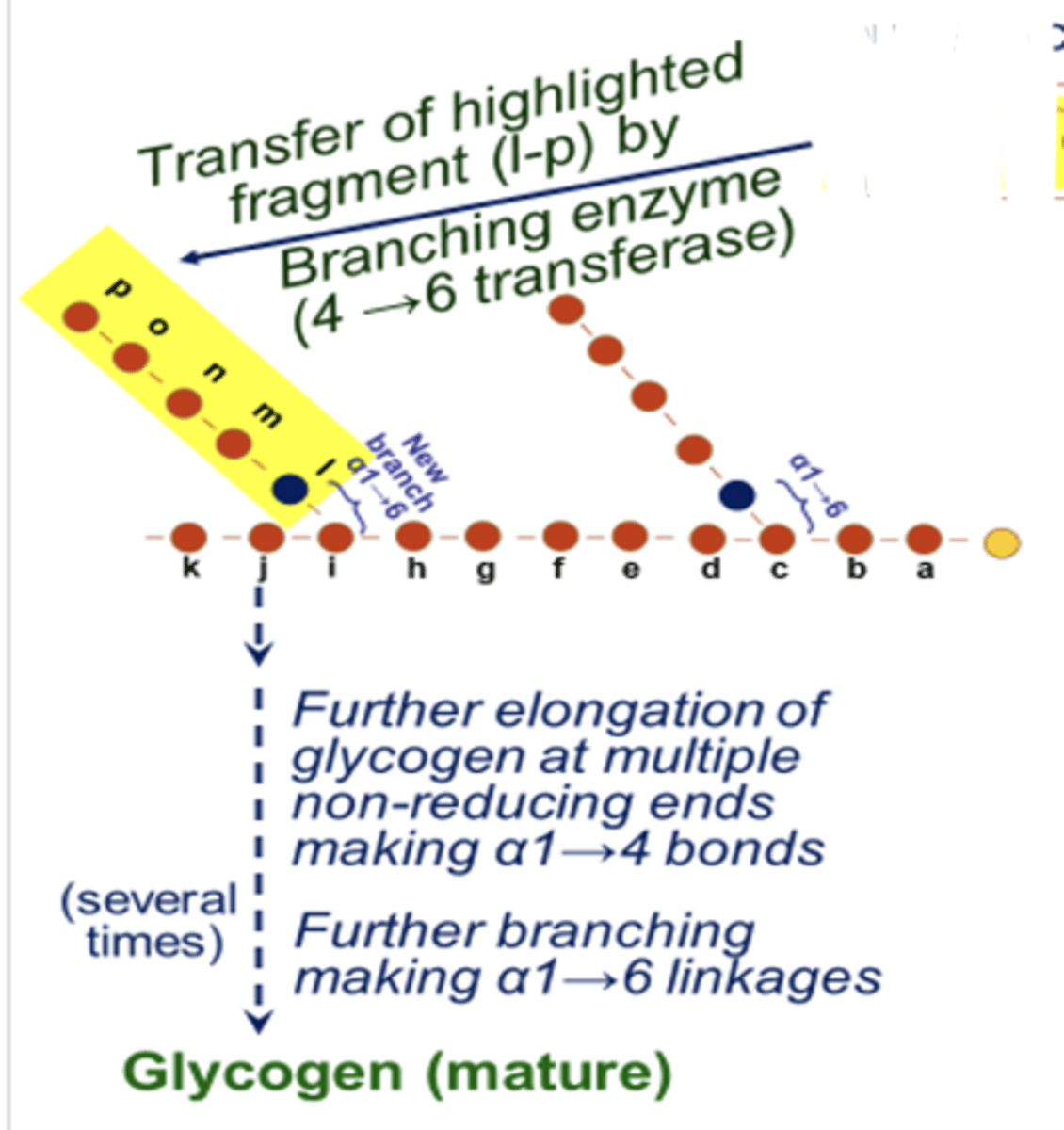
what is the 4th step of glycogenesis
formation of branches to extend glycogen structure by branching enzyme 4 -> 6 transferase (makes alpha 1 -> 6 linkages)
- transfer of elongated chain and establishment of new branch point by branching enzyme
- branching involves detachment of a fragment (of 5-6 glucoses) by branching enzyme form non-reducing end of the elongated alpha 1 -> 4 chain and link it to another glucose in the chain or to a neighboring chain by an alpha 1-> 6 linkage
what is glycogenolysis
glycogen degradation to generate glucose
where does glycogenolysis occur
cytosol
what are the primary end products of glycogenolysis (2)
- glucose 1- PO4
- some free glucose released (from each end of an alpha 1-> 6 glucose linkage; the non-reducing end)
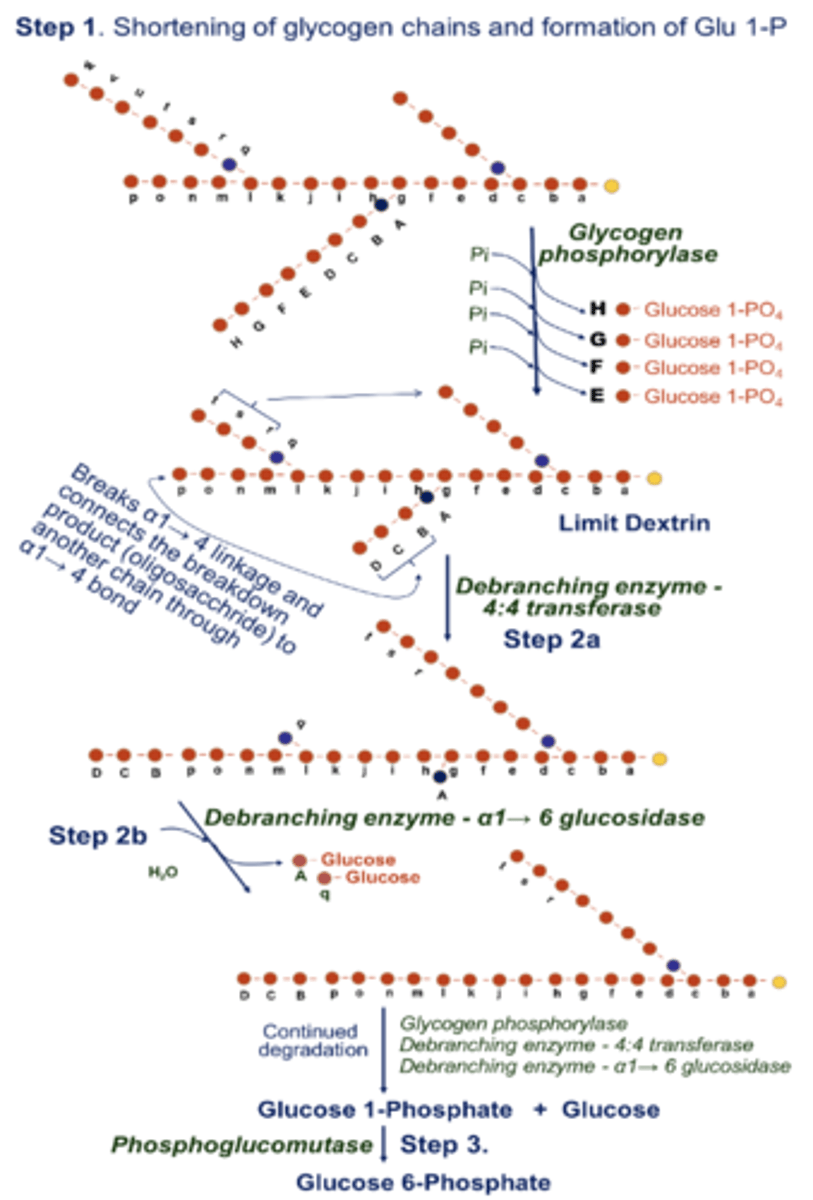
what is step 1 of glycogenolysis
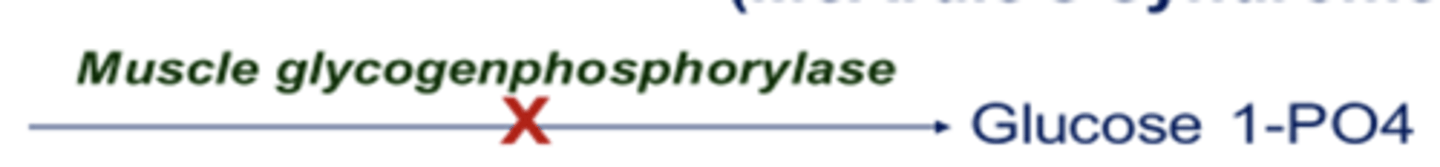
shortening of glycogen chains and release of glucose 1-PO4 via glycogen phosphorylase
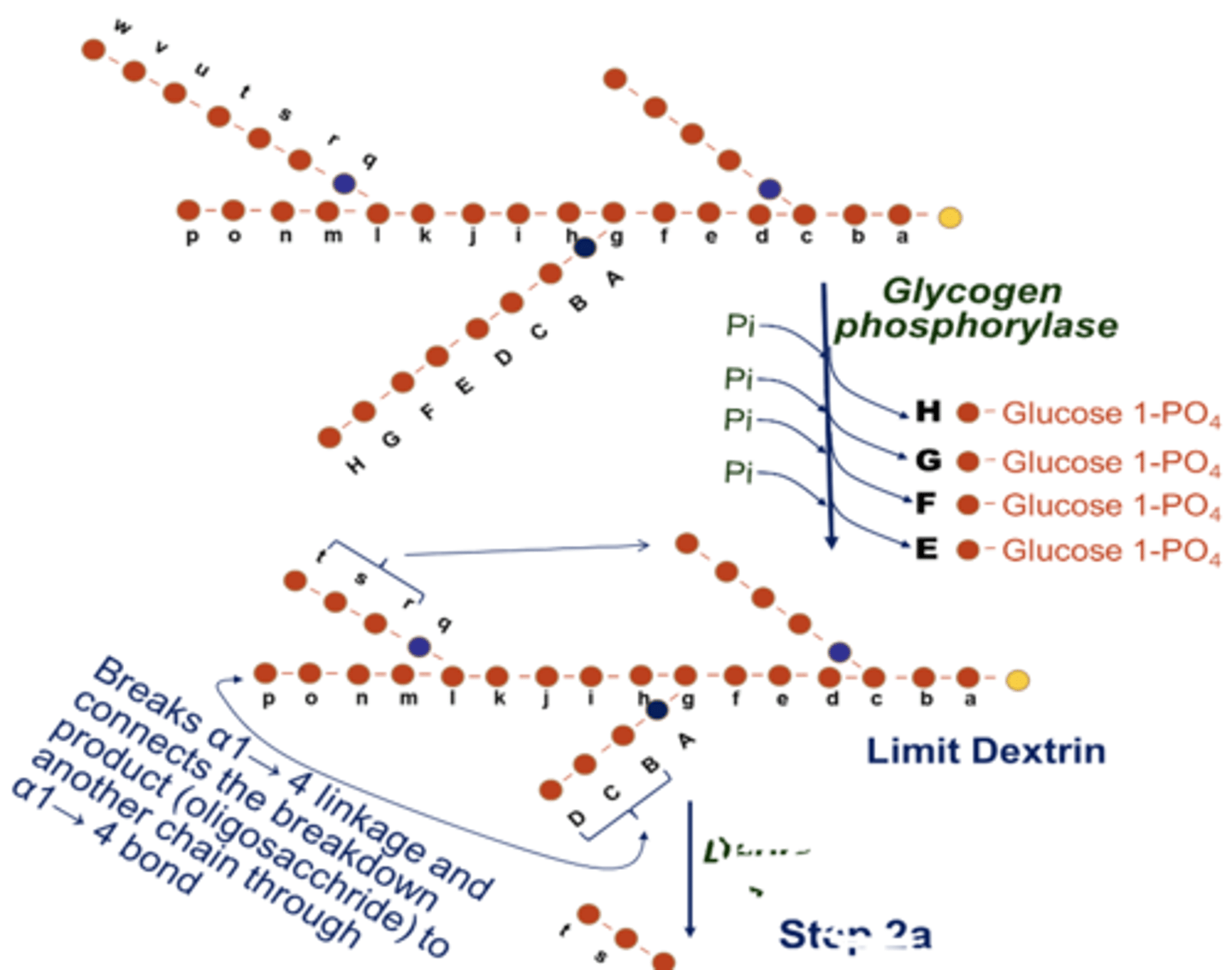
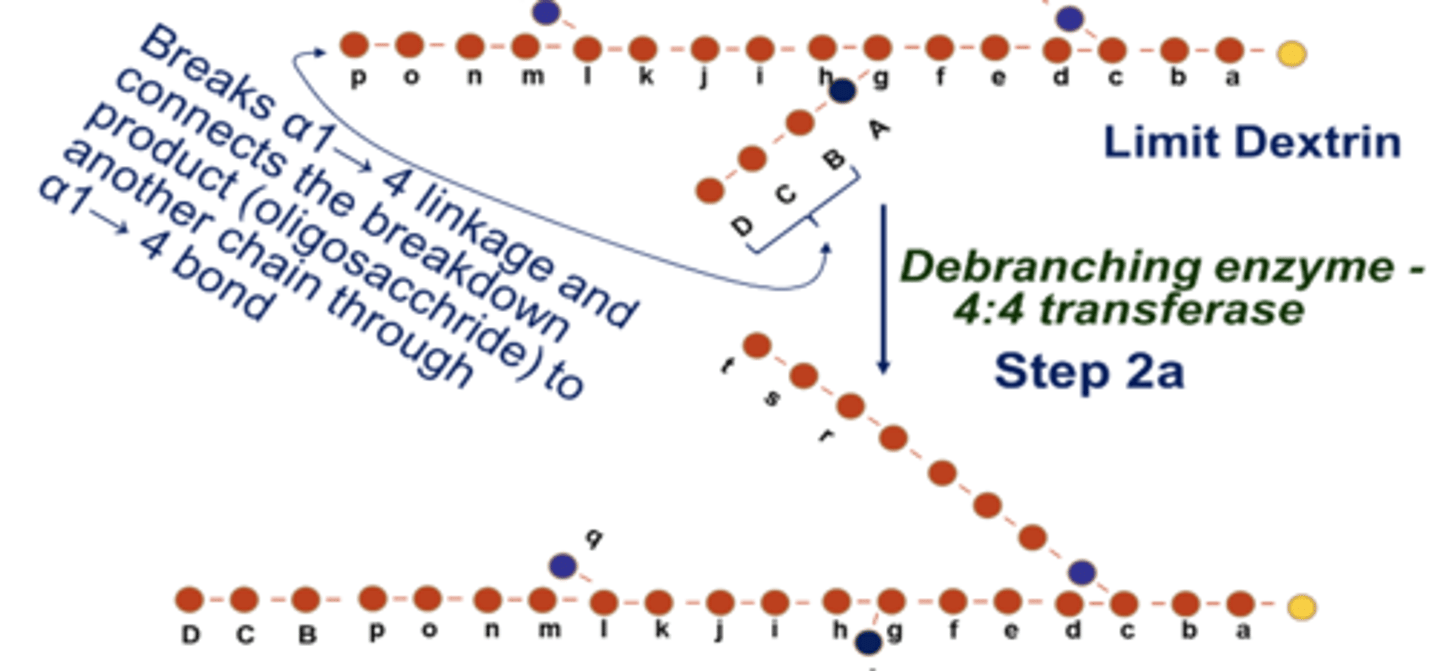
what is step 2a of glycogenolysis
removal of branches
- removal and transfer of branches by debranching enzyme (4:4 transferase from limit dextrin)
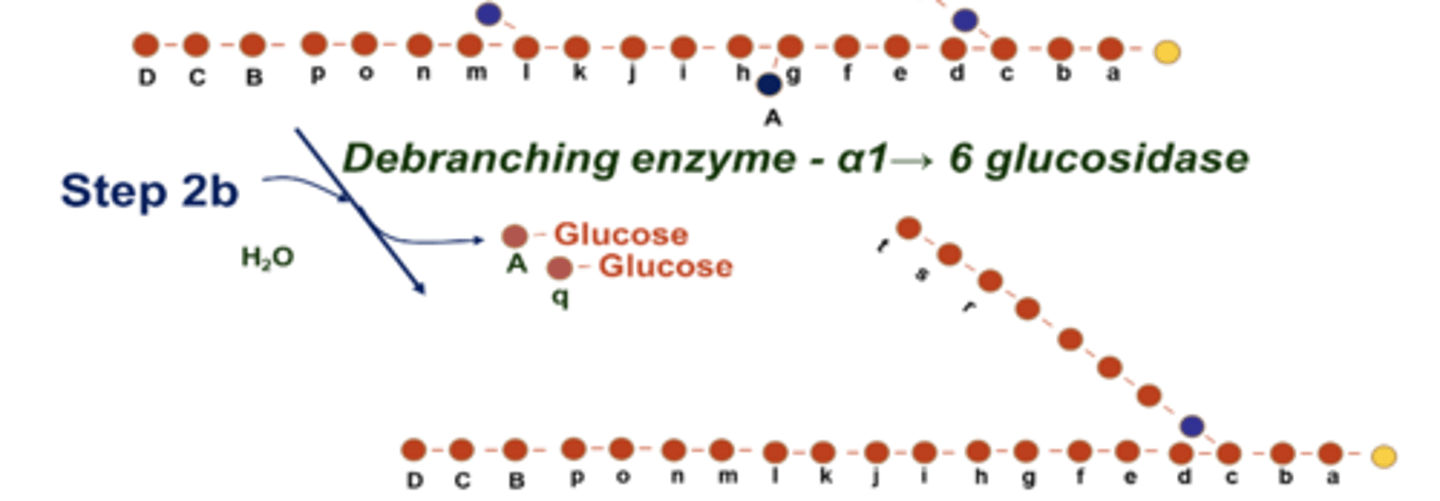
what is step 2b of glycogenolysis
removal of branches
- hydrolysis of alpha 1 ->6 linkages by debranching enzyme alpha 1 -> 6 glucosidase
what is step 3 of glycogenolysis
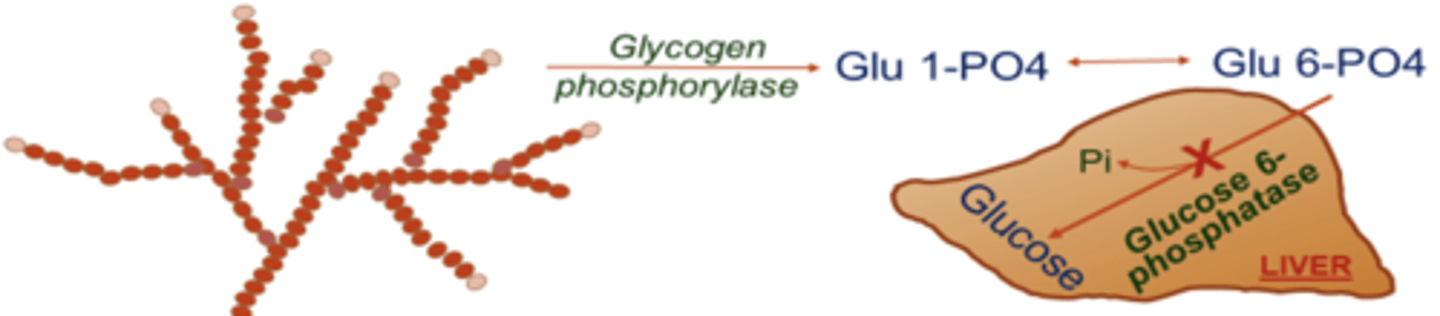
conversion of glucose 1-PO4 to glucose 6-PO4 by phosphoglycomutase

here is the whole picture
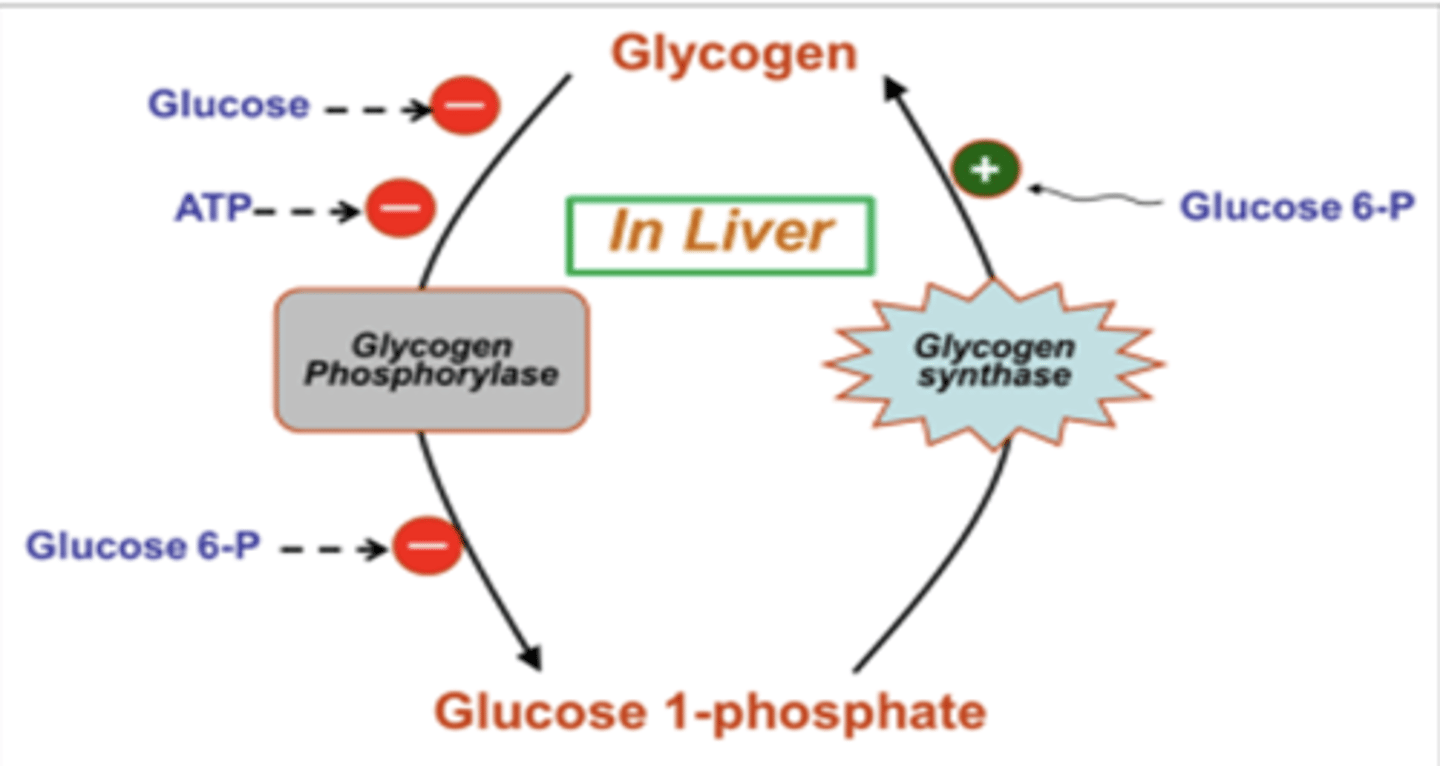
what does the liver do to glycogen in the fed state
stores it
what does the liver do to glycogen in the fasting state
liver glycogen is broken down and glucose released is useful to maintain blood glucose at basal level
is the glucose released from muscle glycogen useful to meet energy needs of the muscle?
yes
is the glucose released from muscle glycogen able to contribute to blood glucose levels?
no
why can't muscle glucose enter the blood to maintain blood glucose at the basal level during fasting
muscle tissue lacks the enzyme glucose-6 phosphotase that is necessary for the conversion of glucose-6 PO4 to glucose
what are the negative allosteric regulators of glycogen metabolism in the liver (3)
1. glucose
2. ATP
3. glucose 6-PO4

what are the positive allosteric regulators of glycogen metabolism in the liver (1)
glucose 6-phosphate
what are the negative allosteric regulators of glycogen metabolism in muscle (2)
1. glucose 6-PO4
2. ATP
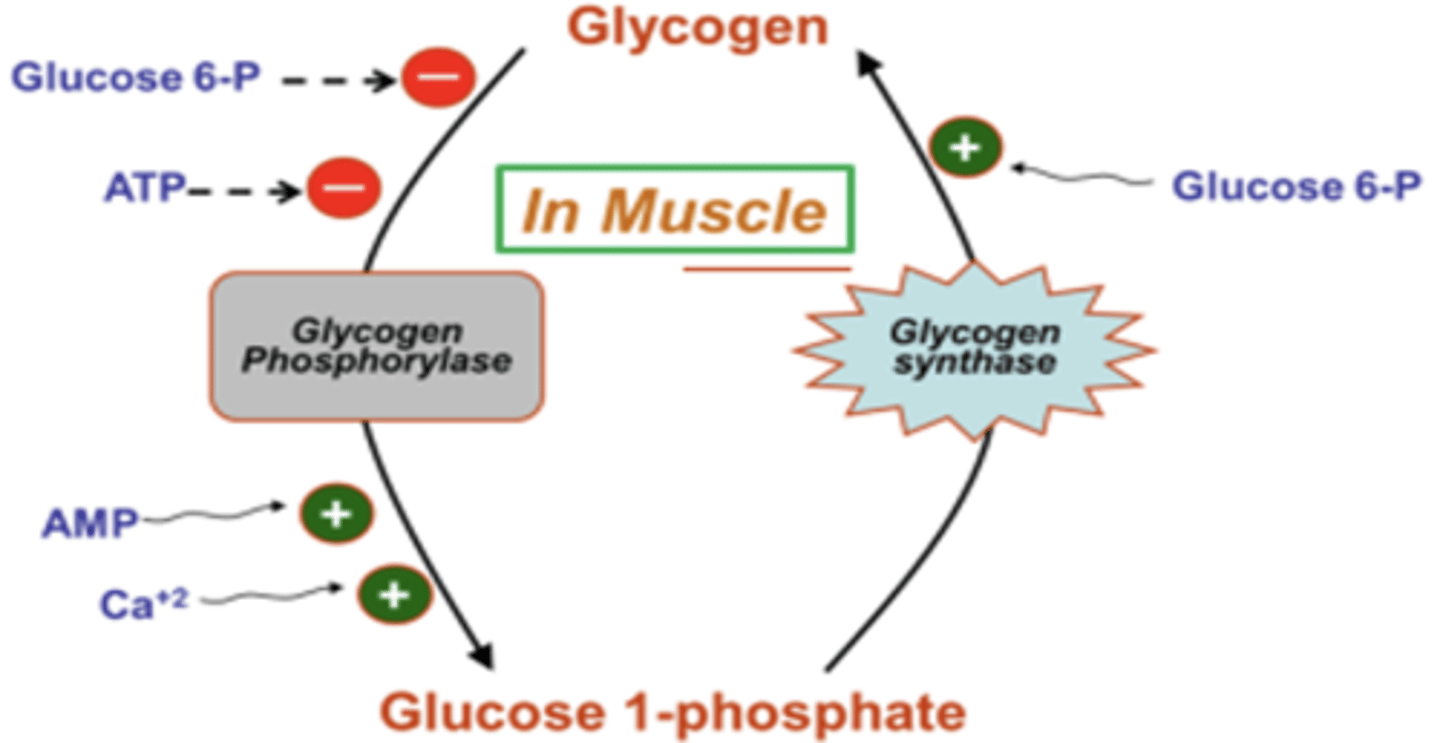
what are the positive allosteric regulators of glycogen metabolism in muscle (3)
1. AMP
2. Ca2+
3. glucose 6-PO4

REMEMBER ALL OF THIS
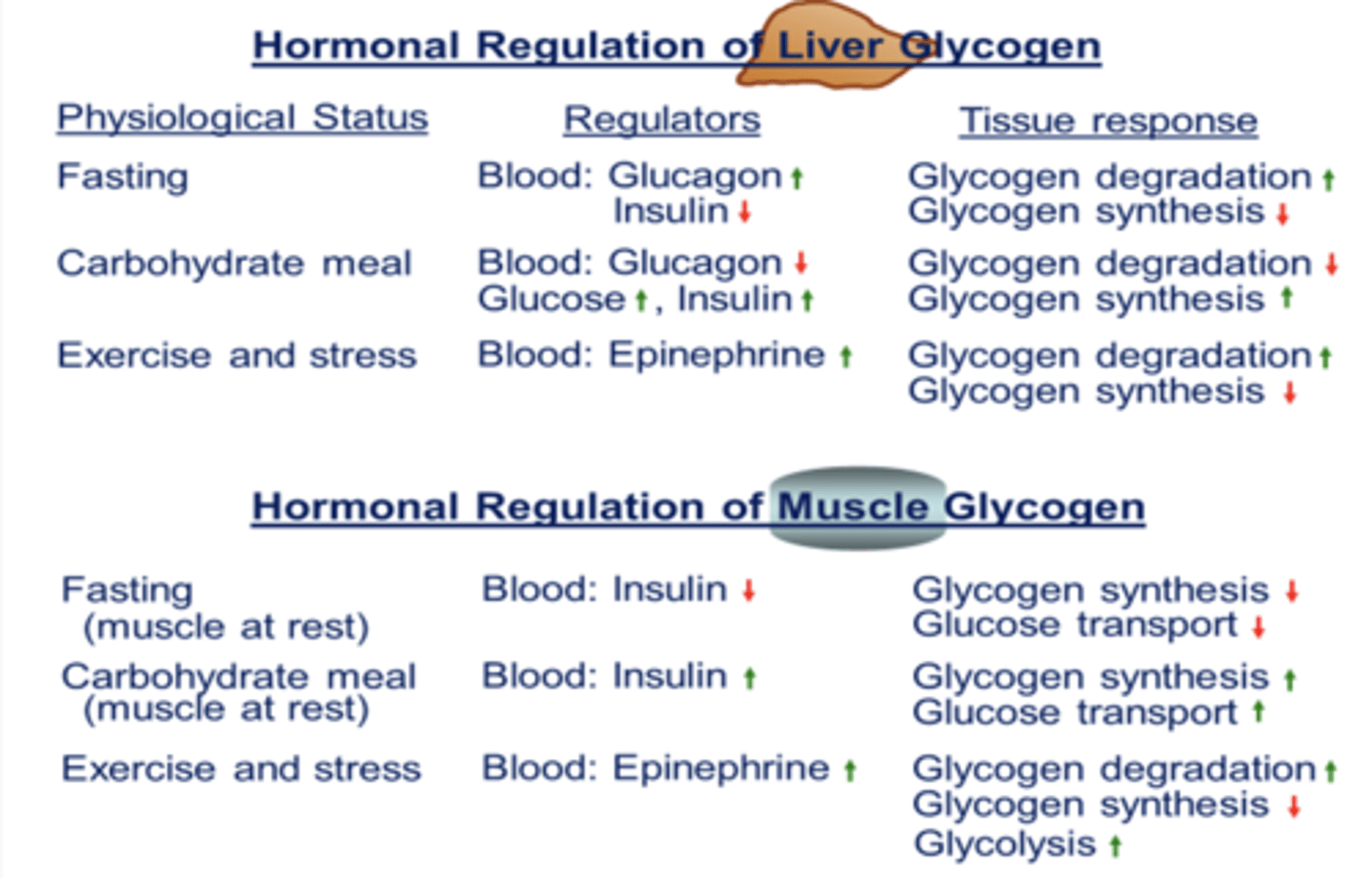
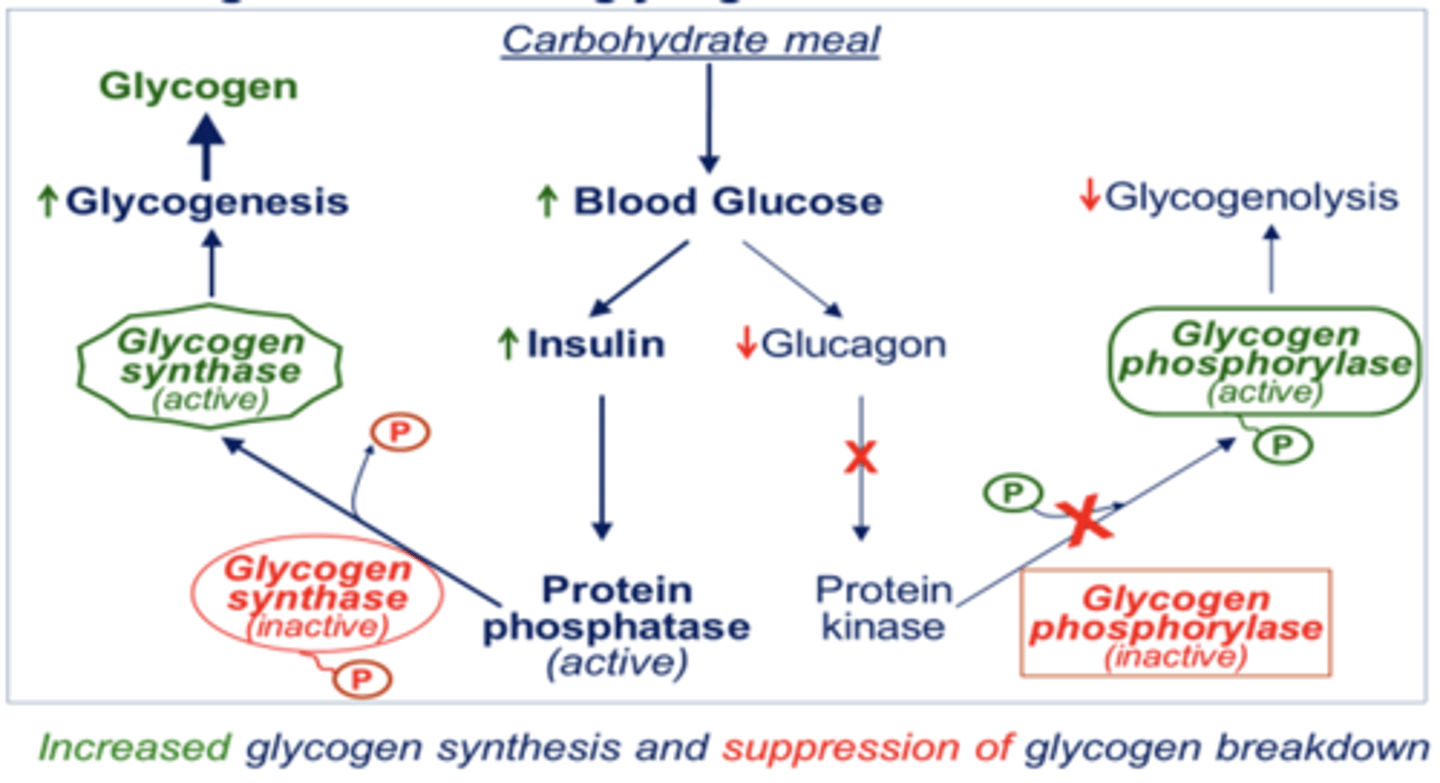
regulation of liver glycolysis in FED state
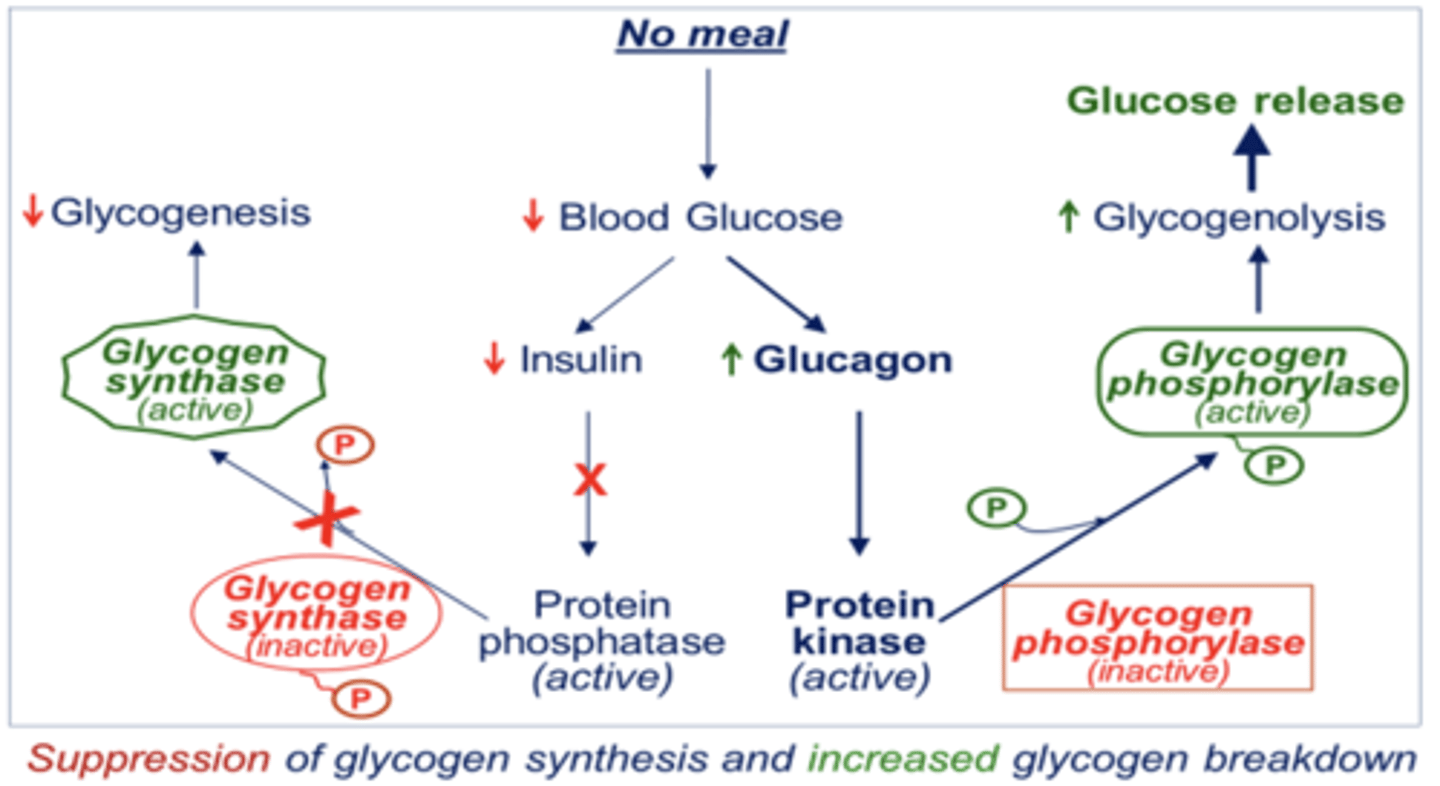
regulation of liver glycolysis in FASTING state
what are glycogen storage disorders characterized by
deposition of abnormal type of glycogen due to impaired synthesis of
- abnormal quantity of glycogen due to impaired degradation
what is the failure to mobilize glycogen due to
defective enzymes
- hereditary / genetic diseases
- mild and not life threatening but sometimes fatal in infancy
what is glycogen synthase deficiency type 0
elongation of glycogen will NOT occur as new glucose residues are not incorporated due to glycogen synthase deficiency
- hypoglycemic state occurs as glycogen is not available to release glucose
- hyperketonemia = early death
what is Von Gierke's disease (type I)
glycogen accumulates as its degradation is blocked
- severe fasting hypoglycemia as glucose is not released into blood stream
- affects liver and kidney
- hepatomegaly, renomegaly, progressive renal disease, and fatty liver
- hyperlipidemia, hyperlacticacidemia, growth retardation, and delayed puberty
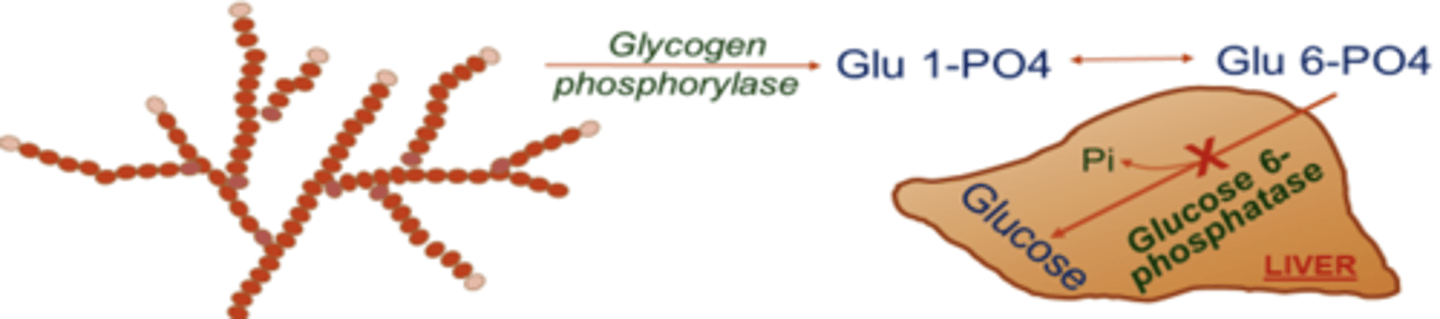
what is Von Gierke's disease (type I) caused by
glucose 6-phosphatase deficiency
is muscle tissue affected in Von Gierke's disease?
no
how to treat Von Gierke's disease
administration of uncooked starch
what is Pompe's disease (type II) caused by
lysosomal alpha 1->4 and alpha 1->6 glucosidase deficiency
what is Pompe's disease (type II)
inborn lisoosmal enzyme defect in liver, heart, and muscle
- accmulation of glycogen in lysosomes
- muscle hypotonia
- massive cardiomegaly due to thickening of heart muscles
- affects pumping of blood; death from heart failure by age 2
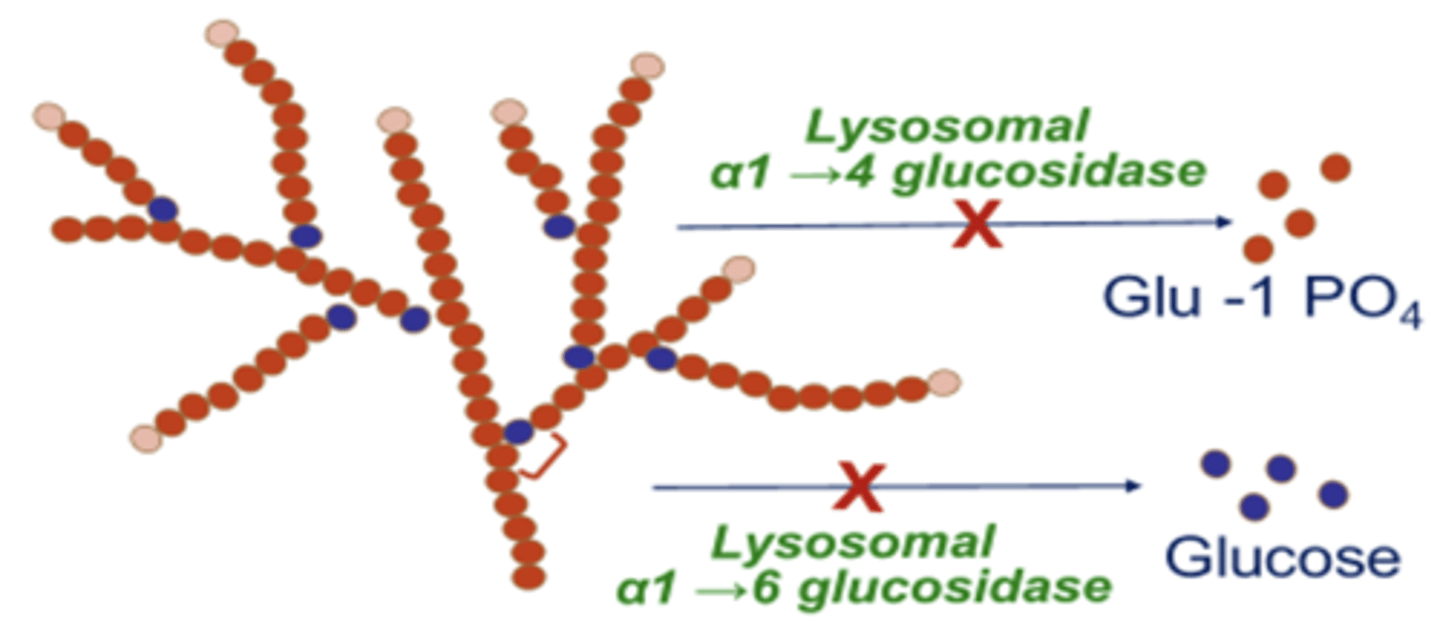
how to treat Pompe's disease (type II)
enzyme replacement therapy available
what is Forbe's / Cori disease (type III) caused by
limit dextrinosis; debranching enzyme deficiency
what is Forbe's / Cori disease (type III)
accumulation of characteristic branched glycogen limit dextrin
- fasting hypoglycemia; hepatomegaly in infants
what is McArdle's syndrome (type V) caused by
skeletal muscle glycogen phosphorylase deficiency
what is McArdle's syndrome (type V)
muscle glycogen is abnormally high
- poor exercise tolerance
- temporarily weakness and cramping after exercise
- no rise in blood lactate during strenuous exercise
- myoglobinemia and myoglobinuria
is the liver affected in McArdle's syndrome (type V)
no
what is gluconeogenesis
the process of synthesizing glucose using compounds other than carbohydrates
in normal physiological conditions when glucose is available this pathway plays a (major/minor) role
minor
when does the body turn to gluconeogenesis for energy (3)
1. prolonged fasting
2. starvation
3. diet with insufficient carbohydrates