med surg II final study guide
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
ICP
- intracranial pressure
- 10% CSF
- 12% blood
- 78% brain tissue
- any changes in ANY volume will cause changes in pressure in the brain --> if one component increases, another must decrease to maintain normal
- ability to compensate is limited
normal ICP range
- 5-15 mHg
- elevated if >20 mmHg sustained
ICP sx
- change in LOC: PRIORITY
- Cushing's Triad
- ocular signs
- compression of oculomotor nerve: unilateral pupil dialation, sluggish or no response to light, inability to move eye upward, eyelid ptosis
- diplopia, blurred vision, EOM changes
- decrease in motor function: hemiparesis/hemiplegia, decerebrate posturing, decorticate posturing
- headache that is continuous and worse in the AM
- projectile vomiting with no nausea beforehand
CPP equation
- MAP-ICP
- normal is 60-100
- MAP: SBP+2(DBP)/3
ngt/ogt related to head injuries
- avoid gastric dilation
- prevent aspiration
- start nutritional supplement early
ventriculostomy purpose
- tx interstitial cerebral edema
- monitoring ICP, brain perfusion
- tube drains the excess fluid --> if indicated, can be intermittent or continuously
ventriculostomy management
- evaluate pt condition
- ensure no leaks, kinks, blocks, differences in height, incorrect height, bubbles, and air
- carefully monitor the volume drained
- prevent infection
ICP and hyponatremia
- hyponatremia can increase ICP with cerebral edema --> osmotically driven movement of water into the brain
- manage fluid and electrolyte balance --> IV hypertonic saline
- monitor for DI or SIADH
improving cerebral perfusion
- maintain head in midline position, prevent extreme neck flexion
- HOB elevated, not >30 degrees
- turn slowly
- avoid coughing, straining, valsalva --> increases intrathoracic pressure contributes to increased ICP by impending the venous return
- avoid hip flexion: decrease the risk of raising the intra-abdomnial pressure, which increase ICP
mannitol
- plasma expander
- osmotic diuretic
- monitor fluid and electrolyte status
- decreases cerebral edema
- used to treat h/a associated w increased ICP
concussion D/C teaching
- report: headache that worsens or doesnt go away, nausea, uncontrolled vomiting, increased confusion, change of personality, drowsiness/inability to wake up, slurred speech, weakness, numbness, seizures, loss of consciousness,
- ensure rest then gradually return to regular activities
- ibuprofen or acetaminophen for headaches
subdural hematoma sx
- sx can show like increased ICP
- decreased LOC
- headache
- ipsilateral pupil dialtion or fixed pupil with severe
blood thinners with head injuries
- ensure assessment of if pt is on anticoags
- contusions can have an increased risk of hemorrhage if on anticoags
battle's sign
- sign of head injury (basilar skull fracture)
- postauricular ecchymosis (bruising behind the ear)
- may mean that there is a significant internal injury to the brain
racoon eyes
- sign of head injury
- bruising around the eyes (periorbital ecchymosis)
- can be a sign of skull or facial fracture (very classic sign of basilar skull fracture)
- can also be a sign of subgaleal hematoma
emergent interventions of epidural hematomas & s/sx
- sx: unconsciousness, brief lucid interval, followed by decrease in LOC, HA, N/V, focal findings
- rapid evacuation: craniotomy if swelling is extreme, burr-holes
measure for leaking CSF
- HOB elevated
- loose collection pad under nose/over ear
- no sneezing or blowing nose
- no NG tube
- no nasotracheal suctioning
- monitor for with battles sign and racoon eyes
how to verify the presence of CSF
- Dextrostix or Tes-Tape strip: test leaking fluid using a strip to determine whether glucose is present (cerebral spinal fluid gives a positive reading; do not test with blood if in the fluid bc blood carries glucose)
- Halo or ring sign (if blood present in leakage): allow leaking fluid to drip onto a white gauze pad and observe the drainage (blood coalesces into the center and a yellowish ring encircles the blood if CSF is present)
Glasgow Coma Scale
- 3-15 --> 3 is worst, 15 is best, 8 or less is severe brain injury
- three parameters: best eye response, best verbal response, best motor response
what does eye opening response include?
- approach to bedside
- verbal command
- pain
scoring of eye opening response
(4) spontaneous response
(3) opening of eyes to name or command
(2) lack of opening of eyes to previous stimuli but opening to pain
(1) lack of opening of eyes to any stimulus
(0) no response
what does verbal response include?
- verbal questioning with maximum arousal
scoring of best verbal response
(5) appropriate orientation & conversant with correct identification of self, place, year, and month
(4) confusion; conversant but disoriented in 1 or more categories
(3) inappropriate or disorganized use of words (ex: cursing); lack of sustained conversation
(2) incomprehensible words & sounds (ex: moaning)
(1) lack of sound, even with painful stimuli
(0) no response
what does motor response include?
- verbal command (ex: raise your arm, hold up 2 fingers)
- pain (pressure on proximal nail bed)
scoring of best motor response
(6) obedience of command
(5) localization of pain; lack of obedience but present of attempts to remove offending stimulus
(4) flexion withdrawal; flexion of arm in response to pain without abnormal flexion posture
(3) abnormal flexion; flexing of arm at elbow & pronation or making a fist
(2) abnormal extension; extension of arm at elbow usually with adduction & internal rotation of arm at shoulder
(1) lack of response
(0) no response
discharge teaching with concussion victims
- instructions for observation & accurate reporting of symptoms or changes in neurologic status
- observation & management of intracranial pressure
neuro ICU delegation
- VS (routine)
- setting up room
- feeding (oral and pt can chew)
- walk to bathroom (if pt allowed and stable)
- let RN know when moving the patient!
neurogenic shock sx
- occurs within 30 mins of SCI (T5 or above)
- can last 1-3 weeks
- affects sympathetic chain of ANS: lead to profound vasodilation and blood pooling in their periphery, profound hypotension and bradycardia, inability to regulate body temp (poikilothermia), hypovolemia, decreased CO
cervical spine injuries
- tetraplegia (paralysis of four extremities)
- loss of resp muscle function
- resp insufficiency: loss of phrenic nerve innervation to the diaphragm, decreased strength in chest and abd wall, require intubation
- ineffective cough
- ortho hypo: lightheadedness, dizziness, nausea
functional limitations with location of spine injuries
- C1-T1 = tetraplegia (paralysis of 4 extremities)
- above C3 = total loss of respiratory muscle function & will arrest in minutes if not intubated
- C3-C5 = respiratory insufficiency; requires intubation (biggest concern is respiratory compromise if above C5) - loss of phrenic nerve (innervation of the diaphragm)
- above T6 = dysfunction of SNS which leads to neurogenic shock
- below T2 = paraplegia (paralysis of legs)
- cervical & thoracic injuries = paralysis of abdominal & intercostal muscles leading to ineffective cough & high risk for aspiration, atelectasis, pneumonia
thoracic injury
- risk for paraplegia
- advocate for full independence and self care in a wheelchair
autonomic dysreflexia
- massive UNCOMPENSATED cardiovascular reaction mediated by SNS for SCI at or above T6
- return of reflexes after spinal shock resolved
- no peripheral or visceral vasodialtion: efferent implses cant pass through injured spinal cord
- present most often in chronic phase after SCI
- most common precipitating cause is a distended bladder or rectum
- needs immediate resolution: can lead to status epilepticus, stroke, MI, death
autonomic dysreflexia manifestations
- HTN: SBP 20-40 above baseline
- throbbing headache: check BP when reported
- flushing and marked diaphoresis above level of injury
- bradycardia (30-40)
- piloerection
- blurred vision or spots in visual field
- nasal congestion
- anxiety
- nausea
autonomic dysreflexia nursing interventions
- elevate HOB 45 degrees or sit upright
- start bladder and bowel training program acutely continuing into rehab (facility/home)
- assess for and remove cause: immediate cath, remove stool impaction, remove constricting cloth/right shoes
- notify HCP
- monitor and tx BP
- monitor VS
SCI rehabilitation
- retraining psychological processes and management of changes
- organized around pt goals and needs
- include EVERYONE in planning
psychosocial with SCI
- education
- encouragement
- include in plan for independence
tonic-clonic seizure
- body stiffens (tonic) with subsequent jerking of extremities
- tx with ativan, dilantin, tegretol
absence seizures
- typical: unresponsive, staring spell
- atypical: staring + jerking-eye/lips
myoclonic seizure
- rhythmic arm abduction (3 movements/sec) followed by arm elevation
- tx with zarontin, klonopin
Interventions during a seizure
- maintain safety: maintain airway, support head, turn to side, loosen constrictive clothing, ease to floor, do not restrain pt or place any objects in mouth
- assess: start time/how long, bitten tongue, soft tissue damage, cyanosis, abnormal resp rate, apnea (ictal) absent or abnormal breath sounds, airway occlusion, HTN, tachy/brady, bowel incontinence, urinary incontinence
- may need oxygen, suctioning after
- assess for any injuries if pt falls as a result of a seizure --> head injuries
dilantin administration
- oral antiseizure
- maintain good oral hygiene
- take with food, no milk, no antacids
- don't stop abruptly
- sx: diplopia, drowsiness, ataxia, mental slowness
anticipating a seizure
- seizure precautions
- assess & record seizure details
- position patient on their side & give antiseizure meds
- collaborate with PT, OT, RT
- If the patient has had seizures, monitor for aural phase signs
- make sure u have an oxygen & suction device
seizure precautions
- bed in the lowest position
- padded side rails
- have suction canister ready to go in room
- assist with ventilation (if no return of spontaneous breath = code blue)
- avoid sharp objects and furniture in the room
- cushion head with a pillow
- PRN meds ready
NANDAs with seizures
- anxiety
- powerlessness
- social isolation
- risk for fall-related injury
- difficulty coping
- impaired breathing
status epilepticus
- state of continuous seizure activity or condition when seizure recur in rapid succession without return to consciousness between seizures
- any seizure lasting longer than 5 mins, neuro emergency, can occur with any type of seizure
- causes brain to use more energy than supplied: neurons become exhausted and cease to function; permanent brain damage may result
- dysrhythmias and muscle fatigue
status epilepticus nursing interventions
- ABCs !!!
- give med: rapid acting IV lorazepam (Ativan)
- support airway
- time it!!
- prep for intubation & go to ICU
status epilepticus medications
- rapid acting IV lorazepam (ativan) or diazepam (valium)
- slows the activity so its not as severe & avoids respiratory compromise
- dont discontinue abruptly
seizure phases
1. prodromal phase
2. aural phase
3. ictal phase
4. postictal phase
TIA
- transient (brief) episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia, but without acute infarction of brain
- hx of TIA is associated with an increased risk of stroke
- tx with ASA 81-160
CVA
- interruption of the blood supply that results in the death of brain cells
- ischemia to part of brain
- severity of loss of function varies according to location and extent of brain damage: physical, cognitive, and emotional impact on pt and family
priority diagnostics for CVA
- MRI
- noncontrast CT scan
- indicates size and location of lesion
- differentiate between ischemic and hemorrhagic stroke
modifiable risk factors for CVA
- HTN
- heart disease
- serum cholesterol
- smoking
- obesity
- sleep apnea
- metabolic syndrome
- lack of physical exercise
- poor diet
ASA with stroke prevention
- antiplatelet to prevent the development of a thrombus or embolus
intracerebral hemorrhage s/sx
- neuro deficits/decreased LOC
- severe HA (worst of life)
- N/V
- HTN
TPA
- used to reestablish blood flow through a blocked artery to prevent cell death
- must be administered within 3-4.5 hrs of onset of clinical signs of ischemic stroke
- during infusion pt VS and monitor closely to assess improvement or potential deterioration related to intracerebral hemorrhage
- pt carefully screened: no GI bleed, any recent bleed (15-20 days ago)
working around hemianopsia
- blindness occurs in the same half of the usual field of both eyes
- move objects into the visual field that the pt can see
- during rehab, train pt to adapt to things in the affected side --> stimulates return of normal function
prioritizing care amongst neuro pt
- LOC
- bleeding risk
- resp system
- pts taking tPA !! (close monitoring of vitals & neuro status)
communication difficulties with CVA
- supportive
- frequent, meaningful communication
- maximize communication abilities
- assess for ability to speak and understand
- speak slowly and calmly using simple words or sentences
- gestures may be used to support verbal cues
- structure conversation so that it permits simple answers by the pt "yes/no"
- is the most difficult problem for pt and family (speech, comprehension & language deficits) -> teach caregiver & family communication strategies (SUPPORT COMMUNICATION BETWEEN PT & FAMILY)
- speech therapy
bladder and bowel training post CVA (can apply to SCI as well)
- bladder: avoid indwelling catheters, avoid bladder overdistention, adequate fluid intake
- bowel: prophylactic stool softeners or fiber, physical activity
- toileting schedule: Q2hrs have a bathroom break (bedpan, commode, or toilet)
- high fiber diet & adequate fluid intake
- adequate fluid intake w most of it given between 7am-7pm
sepsis
- 2/4 systemic manifestations of infection (temperature >100.5/<96.8, HR >90, RR >20/PaCO2<32, or WBC 12,000/<4,000) plus a confirmed or suspected infection that triggers a host response: inflammatory response
- leads to organ dysfunction and death
sepsis causes
- resp infection: 35-50%
- urinary tract: 15-25%
- intra-abdominal: 15-25%
- skin: 11%
- cath related, device related, intra-articular, boney, post-procedural
sepsis assessment
- lactate levels
- blood draw for causative agents
- start broad spectrum abx (after labs)
- start fluids
- assessment needs to be done within one hour if sepsis is a possibility
sepsis interventions
- oxygen: titrate O2 to saturations of 94-98% or 88-92% in chronic lung disease
- fluids: start IV fluid resuscitation if evidence of hypovolemia 500mL bolus of isotonic crystalloid over 15 mins and give up 30mL/kg, reassessing for hypovolemia, euvolemia, or fluid overload
- antimicrobial: give IV antimicrobials according to local antimicrobial guidelines
- blood: culture, lactate, CBC, U&E, LFTs, coags
- urine output: assess urine output and consider urinary cath for accurate measurement
anaphylactic shock
- hypersensitive allergic reaction
- immediate vasodilation due to release of vasodilation due to release of vasoactive mediators
- sx: wheezing, stridor, angioedema
anaphylactic shock intervention
- epinephrine SQ
- benadryl IVP to stop allergic process
- steroids to decrease swelling
- bronchodilators
- monitor: RR and O2 sat
septic shock
- severe sepsis + persistent hypotension or lactic acid >4 mmol/L
- systemic inflammatory response & severe hypotension despite aggressive fluid administration (hypovolemia) usually caused by gram-negative and gram-positive bacteria
signs of septic shock
- hypotension even with aggressive fluid admin (persistent)
- vasodilation
- lactate levels +4
- compensatory: tahy, tachypnea, shunting from the GI, skin, and kidneys
- worsening: paralytic ileus, oliguria, cold clammy skin
interventions of septic shock
- vasopressor if fluids do not reestablish BP and perfusion
- steroids
- oxygen
- abx
hypovolemic shock
- loss of intravascular volume hemorrhage
- causes: GI loss, vomiting, diarrhea, wound drainage, hyperglycemia, diuresis
- relative fluid loss: extravascular space leakage (third spacing) bowel obstruction, ascites, burns
hypovolemic shock sx
- Hypotension, tachycardia, decreased urine output, pale, cool, slow cap refill (>2 sec), dry mucosa
- worsening: neuro status changes --> not getting volume
- decreased stroke volume, CO, renal flow
hypovolemic shock interventions
- Monitor BP, pulse, RR, o2 sat and weights daily
- keep HOB flat
- Place patient's legs elevated
- fluid resuscitation (3mL for every 1mL of blood loss)
- stop loss of fluids or blood
- Provide oxygen as needed
- Monitor patients for signs of Fluid overload such as: Crackles in the lungs, swelling, weight gain
- Antcipate an order for CBC, Electrolytes, BUN, Creatinine
cardiogenic shock
- results from systolic and/or diastolic pumpling actions resulting in decreased CO
- MIs, cardiomyopathies, blunt trauma, severe systemic or pulmonary HTN, cardiac tamponade, metabolic changes
cardiogenic shock sx
- looks like HF
- first: tachy, HTN,
- worsening: narrow pulse pressure, pulmonary congestion with crackles
- skin shows signs of shock: pale, diaphoretic
cardiogenic shock main meds
- nitrates to dilate coronary arteries
- diuretics to decrease preload
- vasodilator to decreased afterload
chronic angina
- chest pain when there is an increased demand in vessel with plaque --> vessel cant dialate to allow blood flow to meet the myocardial demand --> O2 demand >O2 supply
- artery blocked 70% or more or left main artery blocked 50% or more
- intermittent pain with the same onset, duration, and intensity
- prinzmetal's angina: hx of headache --> spasm of major coronary
- usually goes away with nitroglycerin administration and rest
- negative troponin
- tx with nitro, ACEs and ARBs, beta blockers, and calcium channel blockers
angina assessment
- onset: sudden/gradual?
- location: precordia, substernal, diffuse ache in arm
- characteristics: precipitating, quality, radiation, sensing, timing
- Precipitating: emotions, exertion, heavy meal
- Quality: pressure, tightness, squeezing, indigestion (menopausal female)
- Radiation: chest, neck, teeth, back, shoulders, arms
- Sensing: usually low rating on 0-10 pain scale
- Time: duration, how long is it lasting
unstable angina
- new in onset
- occurs at rest
- increase in frequency, duration, or with less effort
- pain lasting greater than or equal to 10 min
- need immediate tx
- sx in women often under-recognized
MI
- abrupt stoppage of blood flow through a coronary artery causing irreversible myocardial cell death (necrosis) in the heart muscle beyond blockage
- severe chest pain that is not relieved by rest, position change, or nitrate admin,
- pain can radiate to neck, lower jaw, arms, and back
- release of catecholamines causes increase HR, BP, vasoconstriction --> BP will then decreases after compensation
- skin is ashy, clammy, and or cool to touch
- dysrhythmias: Vtach/fib- crackles, JVD, S3 S4, new murmur, fever, N/V
- thrombolytic therapy: give within 30 mins of arrival to ED, ensure no recent bleed, surgery, 2 IVS
nitroglycerin
- indications: CHEST PAIN from stable angina --> same onset, duration, feeling of pain --> to relieve chest pain
- admin: check BP, sublingual or nasal spray --> Sublingual every 5 mins for three times --> if pain does not relieve call 911
- side effects: headache, light headed, dizzy, stand up slowly --> FALL RISK
- contraindications: viagra
- action: dialate vessels to allow more blood to flow to heart --> decrease O2 demand/ increase O2 supply
digoxin
- indications: chronic heart failure, afib
- administration: daily, check HR before administering, get labs checked for drug and potassium
- side effects: headache, dizziness, N/V, confusion and weakness (bad)- contraindications: MI, hypokalemia, decreased HR
- adverse reaction: ventricular dysrhythmias
- action: increases heart contractility by increasing the sodium and therefore calcium
amiodarone
- indications: dysrhythmias --> junctional rhythm, PVC, vtach --> and symptomatic with chest pain
- administration: high HR but stable pulse
- side effects: hypotension, bradycardia
CABG complications
- abrupt closure from coronary artery dissection and vascular injury at the artery access site
- bleeding, infection, stroke
CABG
- tx of STEMI and ACS
- requires sternotomy and cardiopulmonary bypass
- uses arteries and veins for grafts --> radial graft being used
- palliative tx
- coronary revascularization
CABG assessment
- surgical site care, check incision
- graft site frequent assessment: pulse, color, temp, cap refill
- radial artery harvest site
- leg incisions
- pain management: NTG, morphine
- DVT prevention
- pulmonary hygiene
- cognitive dysfunction
HF
- abnormal clinical syndrome that involves failure to pump and/or fill the heart
- heart cannot supply enough blood to meet the oxygen needs of the tissue and organs
- involves diastolic or systolic dysfunction
- ejection fraction: amt of blood pumped by LV with each heart beat --> 55-65%
HF teaching
- monitor: faces (fatigues, limitation of activities, chest congestion, edema, SOB) reappearance of SX, what to report, go to follow ups, join support groups
- get vaccines and reduce risk factors
- low sodium diet --> DASH diet, individualized recs
HF common meds
- digoxin
- diuretics: furosemide --> check BP and HR, give in AM, increases release of fluid, can cause hypokalemia --> dig toxicity
- beta-blockers: relax blood vessel and decreases HR and improve blood flow, decreases workload and O2 demand
- calcium channel blockers
carvediolol (Coreg)
- contraindicated in pulmonary edema
- brady, heart block, or sick sinus syndrome (unless a pacemaker is in place)
- decompensated HF requiring IV inotropic agents
paroxysmal nocturnal dyspnea
- sudden wakening of SOB at nighttime
- pt feels suffocated
- sx of Left sided hf --> CHF sx
- sit pt up when sleeping
- can be a sign of mitral valve regurgitation
JVD assessment
- position pt supine with head elevated and observe for pulsation that does not match radial pulse rate
- sign of: MI, right sided HF, cardiac tamponade, and myocarditis
- indicates: complication of pulmonary edema
chronic HF objective data
- skin: color and temp --> cool, diaphoretic, pallor
- resp: rate and sounds --> crackles, frothy blood-tinged sputum
- tachy, S3, S4
- abdominal distention
- new or sudden onset of sx is priority --> decompensated HF
- monitor for decreased sats --> decompensation
MI D/C instructions
- stay on meds
- start activity slowly and gradually
- relaxation therapy
- rehab outside of the hospital
- low sodium diet
- cant resume intimacy until three flights of stairs without SOB
adenosine
- indications: supraventricular tachycardia
- administration: on cardiac monitor, stops hr for a sec (like a reboot) change position slowly with pt
- side effects: hypotension, SOB
vagal response
- vagal stimulation: bearing down, massaging chest, mechanically slowing down HR nonmedical response to tx SVT
- response: brady and risk for cardiac arrest with stimulation
EKG measurements
- P wave: upright
- PR interval: 0.12-0.20 secs
- QRS interval: less than or equal to 10 ses
- QT interval
- regularity of R-R interval
normal sinus rhythm
- everything is NORMAL
- HR: 60-100
- P-wave: normal, round, upward deflection
- PR-interval: 0.12-0.20 secs
- QRS: less than or equal to 0.10 secs
- R-R interval: regular

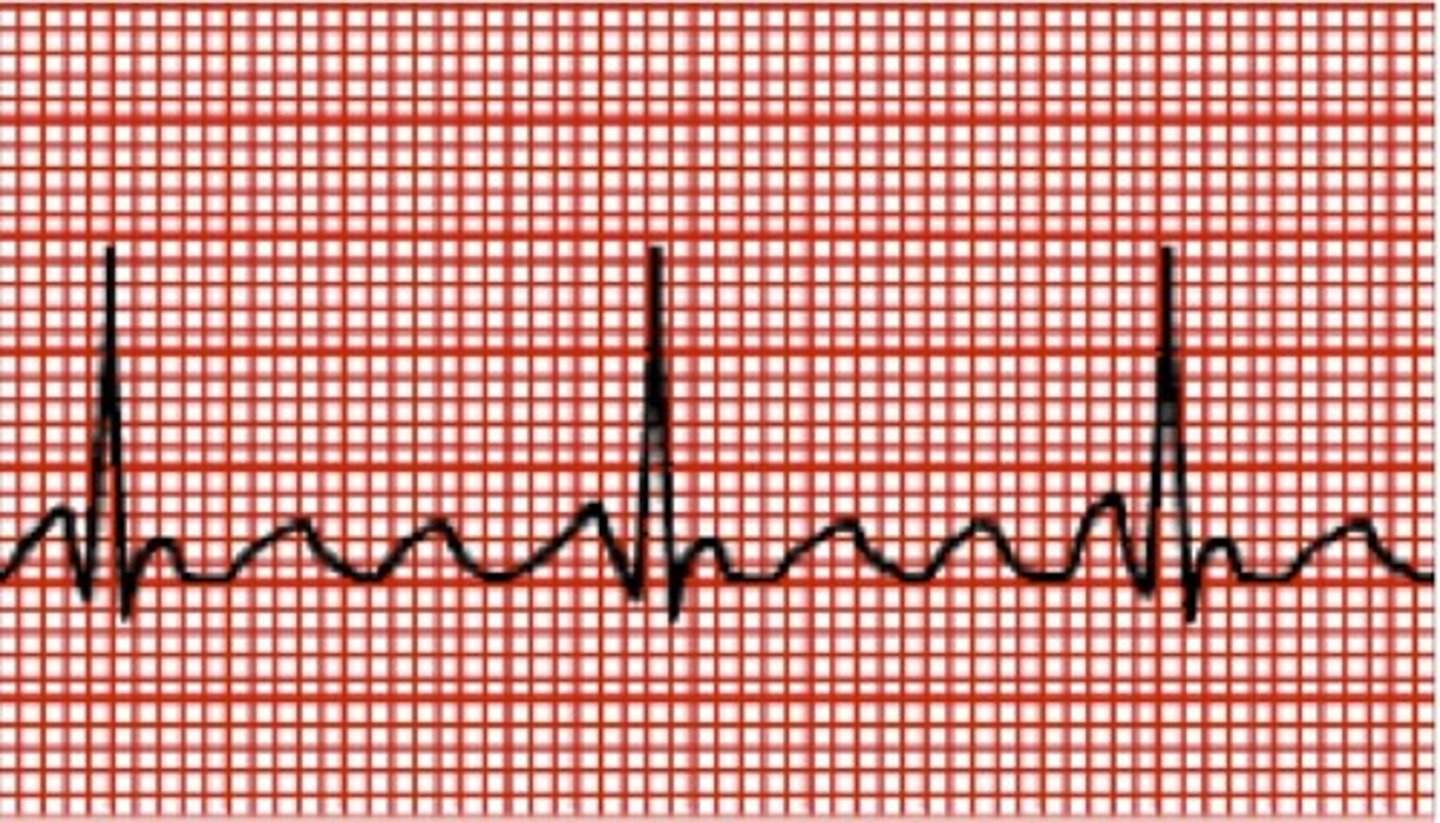
sinus tachycardia
- heart attempting to meet increased need fo oxygen to tissues
- HR: > 100
- P-wave: normal
- PR interval: normal
- QRS: normal
- R-R: regular
- unstable pt: altered LOC, ischemia, shock or decreased BP --> synchronized cardioversion

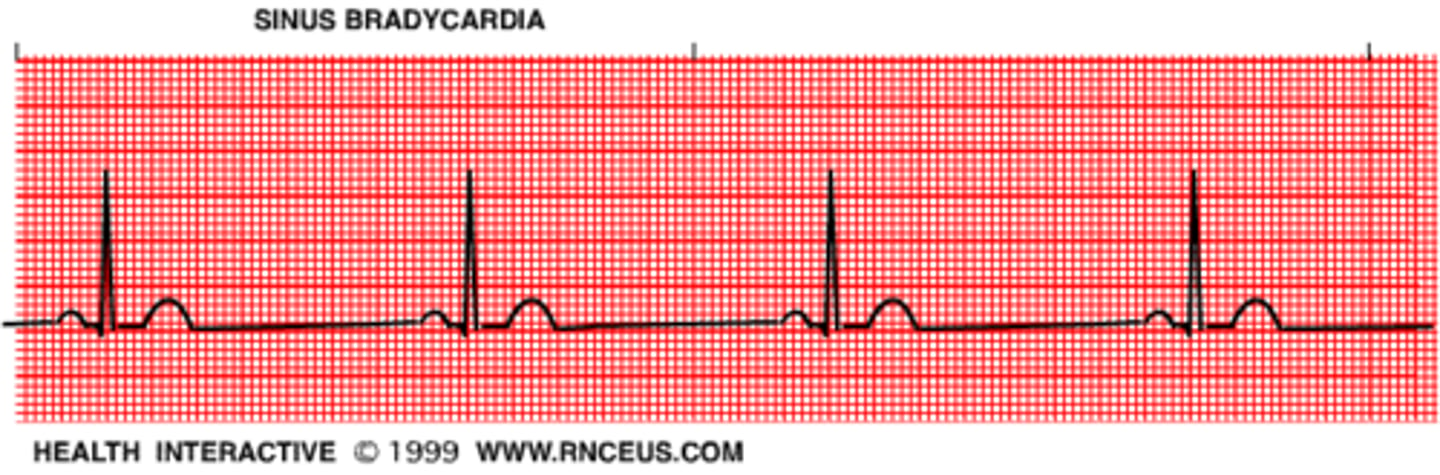
sinus bradycardia
- normal in athletes but can be induced --> vagal response
- HR: <60 BPM
- P-wave: normal
- PR interval: normal
- QRS interval: normal
- R-R interval: regular
- GIVE MEDS ONLY IF PT IS SYMPTOMATIC --> atropine
- sx: SOB, diaphoretic, dyspnea, hypotensive
atrial fibrillation
- not a full contraction of the atrium
- CAD, alcohol, caffeine, cardiomyopathy, HTN, thyrotoxicosis
- HR: >100< BPM
- P wave: completely disorganized atrial activity (irregular)
- PR interval: not measurable
- QRS: generally normal
- R-R interval: irregular, no regularity
- - rate control with digoxin or Beta blockers (lower HR)

atrial flutter
- rhythm in the atrium is more organized and less chaotic but the rate is still fast
- CAD, HTN, mitrial valve disorders, PE, cor pulmonale
- risk of CVA
- P wave: saw tooth wave baseline
- PR interval: unmeasurable
QRS interval: normal
- R-R: usually normal
- tx: beta blockers, calcium channel blockers, antiarrhythmic, DC cardioversion