ADH and body fluids
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
What is Body fluid homeostasis reliant on?
What determines how much water you need per day?
In regards to the water balance equation, What is the intake? What is the outake?
Fluid Homeostasis:
Blood Volume and Pressure: Blood volume is the primary determinant of blood pressure.
Composition: Concentration of solutes and osmolality
Water Distribution and Requirements:
Varies by age, gender, and muscle mass
Water Balance Equation: Intake – Output = Balance:
Intake: fluids, food, metabolism
Output: urine, sweat, GI losses, insensible losses (transdermal and respiratory tract)
What type of fluid w/in body is affected by gains/loses of fluid?
Describe the tonicity of losses
Describe the main type of regulation on body fluid homeostasis
Fluid Compartments: All gains/losses affect extracellular fluid (ECF)
Tonicity of Losses:
Most losses are hypotonic
Urine can be iso-, hypo-, or hypertonic
Regulation: (hormonal, neuronal controls, and local factors)
Hormonal regulation is the main one:
Affects Osmolality and Volume
Kidneys = primary effector Organ
Excess water/electrolytes are excreted via urine
What are the two fluid compartments w/in body?
Describe Fluid Movments of:
Solutes?
Water?
What are the two transport Routes?
Explain how Capillary Exchange is determined?
Differentiate between Osmolality, Osmolarity and Tonicity
Body Fluid Compartments:
Intracellular (ICF)
Extracellular (ECF): Plasma, Lymph, Interstitial, Transcellular (e.g., CSF, urine, sweat)
Fluid Movement:
Solutes: move via [] or electrochemical gradients
Water: Rapid exchange between ICF and ECF in response to osmolality/tonicity changes
Transport Routes: Transcellular (Aquaporins), Paracellular (Junctions)
Capillary Exchange:
Exchange between subcompartments of the ECF
Governed by Starling forces: hydrostatic and oncotic pressures
Osmolality vs Osmolarity vs Tonicity:
Osmolality: concentration of solute particles per kg of solvent
Osmolarity - concentration of solute particles per L of solvent. Uniform across compartments; independent of membranes
Tonicity: reflects non-penetrating solutes and depends on membrane permeability (σ): Permeant (σ=0), Impermeant (σ=1)
What do Starling Forces Dictate?
What is Filtration Rate?
Formula for Sterling Force Equation?
Starling forces:
The movement of fluid across a capillary wall is determined by the hydrostatic (P) and oncotic (π) pressures:
Filtration Rate: volume of fluid moving across the capillary wall (expressed in units of either volume/capillary surface area or volume/time)
Filtration rate=Kf [(Pc−Pi)−σ (πc−πi)]
Describe the influence that ECF Volume and Extracellular osmolality has on the body
What organ is especially vulnerable to osmoality changes and the result of this?
What is the full formula/approximation of normal blood osmolality?
Differentiate the effects that Isotonic and hypo/hypertonic fluid changes has on ECF/ICF
ECF Volume/Extracellular Osmolality:
ECF Volume: blood pressure, tissue perfusion, and organ function
Extracellular osmolality: cell volume, impacting cellular and CNS function.
This occurs especially in brain: Swelling/Shrinkage → confusion, seizures, or coma
Normal plasma osmolality Equation:
Full formula: 2[Na⁺] + [Glucose] + [Urea]
Approximation: ~2[Na⁺]
***Normal = 275–295 mOsm/kg H₂O***
Iso vs Hypo/Hyper Tonicity Changes on ECF/ICF:
Isotonic: affect ECF only
Hypo/Hyper: cause shifts in ICF volume due to osmosis
How do you calculate Total Body Water(TBW) for males/females?
How is the TBW distributed among ICF/ECF?
Describe the further subsection w/in the ICF and what physiological changes could cause these subsectiosn to increase or decrease
How do we estimate Blood Volume and what is the formula?
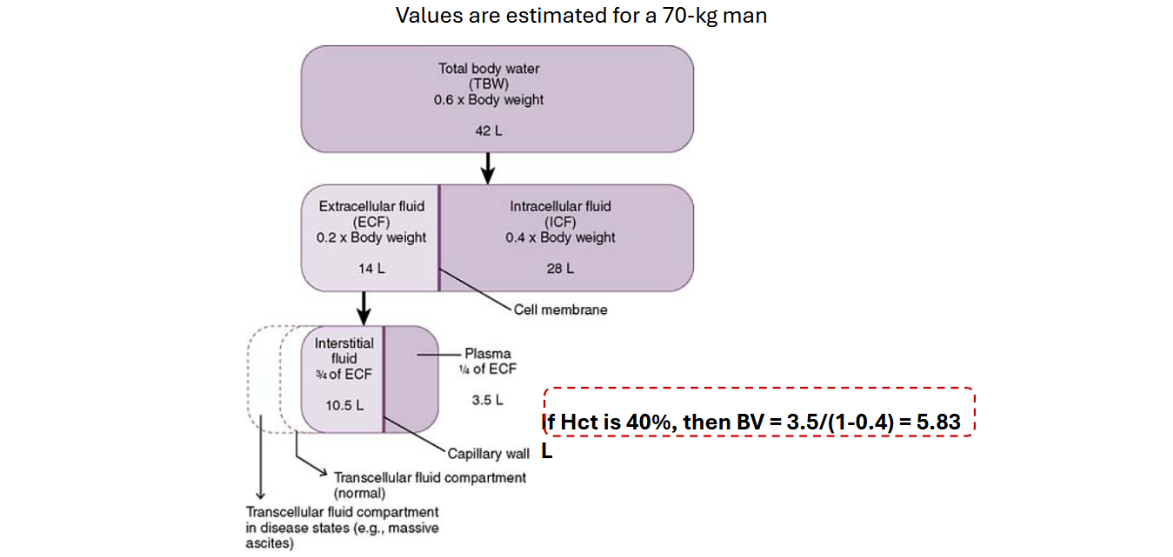
TBW:
~60% of body weight in men
~50% of body weight in women
Compartments:
ICF: ⅔ of TBW
ECF: ⅓ of TBW; DIVIDED INTO:
Interstitial Fluid (IF): ¾ of ECF — ↑ in peripheral edema
Plasma: ¼ of ECF — ↓ in dehydration
Transcellular Fluid: ↑ in ascites, pleural effusion
Blood Volume (BV):
estimated from plasma volume and hematocrit
Hematocrit (Hct): % of blood volume occupied by red blood cells
BV = Plasma Volume ÷ (1 − Hct)
If a pt is a 70-Kg male, Calculate TBW, ECF, ICF, Interstitual Fluid volume, Plasma, and blood volume is hematocrit = 35%
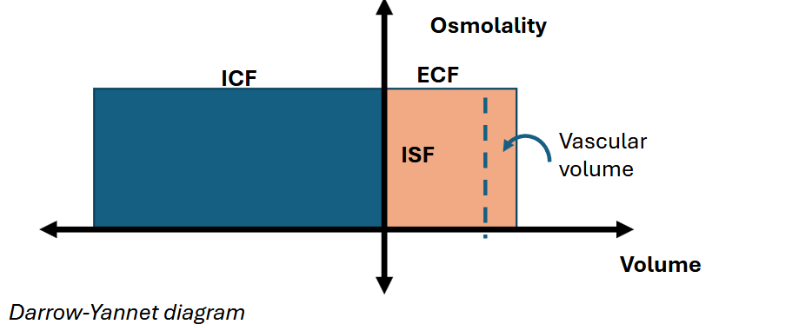
What is the function of the Darrow-Yannet Diagram and draw a general form of it
Darrow-Yannet Diagram: Visualizes fluid shifts and osmolality changes in clinical conditions
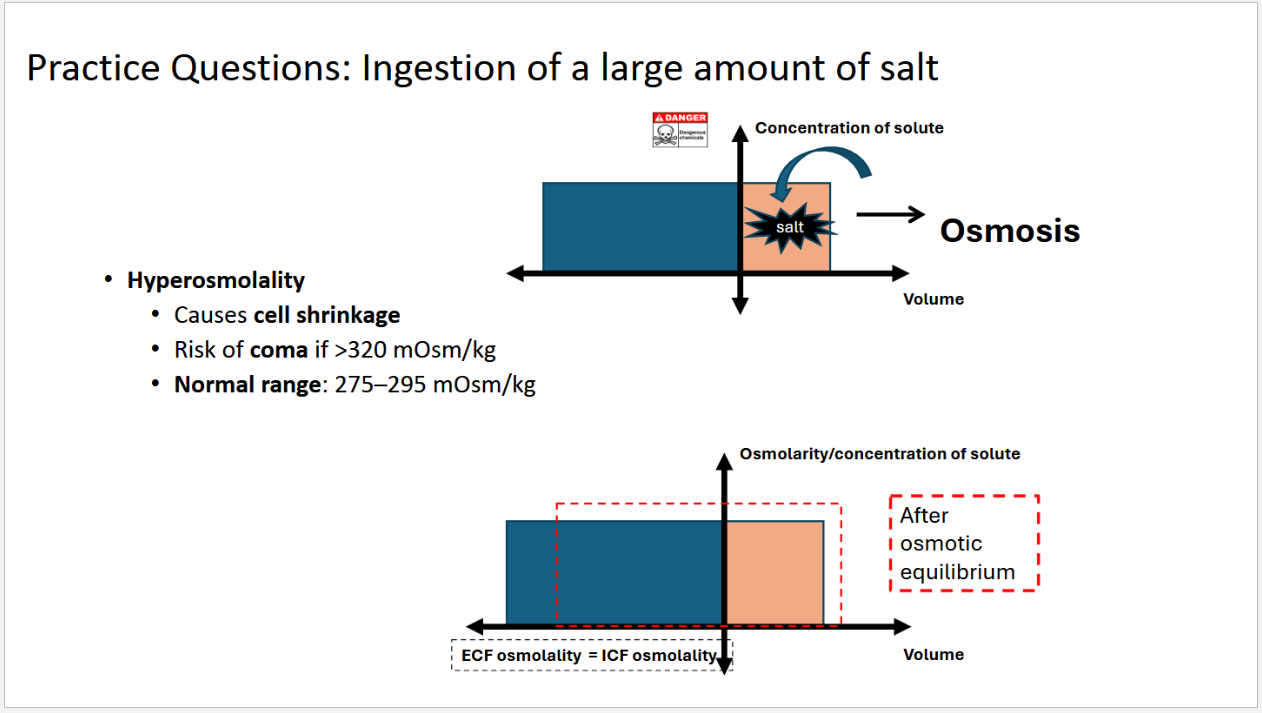
Draw out the Darrow-Yannet Diagram if a pt ingest a large amount of salt?
What is a clinical consequence of this high salt consumption?
Draw out the Darrow-Yannet Diagram if a pt ingest a large amount of water?
What is a clinical consequence of this high water consumption?

Draw out the Darrow-Yannet Diagram for each scenario and explain what could cause this change?
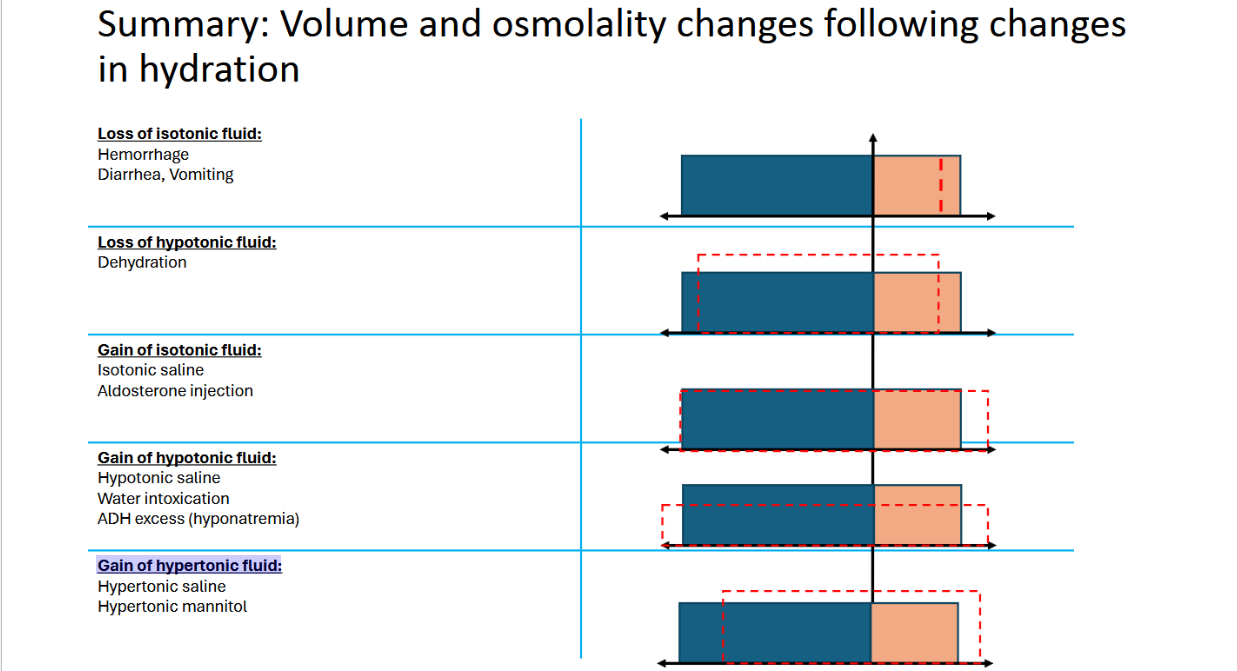
Loss of isotonic fluid:
Loss of hypotonic fluid:
Gain of isotonic fluid:
Gain of hypotonic fluid
Gain of hypertonic fluid:
What does ECF Volume and BP depend on? What is it regulated by?
What does Osmolality and water balance dependent on? What is it controlled by?
ECF Volume and blood pressure:
Depends on the sodium balance and is linked to the sodium content in body fluids
Osmolality and water balance:
Depends on water intake and renal water excretion
Water follows Na⁺ to maintain stable plasma osmolality
Controlled by ADH (AVP)
Where is ADH synthesized?
Where is it transported to?
Describe this mechanism
ADH Origin, synthesis, release:
Synthesized in the paraventricular and supraoptic nuclei
Transported to Post. Pit. for release
MECH:
prohormone packaged into vesicles w/ cleavage enzymes
transported along axons
stored @ axon terminals
released into bloodstream upon stimulation
Origin/Function of ADH?
Differentaite between the threshold for AVP secretion in Post. Pit vs Thirst Center
Stimuli for Secretion/Inhibition?
Kidney Effect?
Regulation of ECF osmolality/Blood Volume?
Degradation?
Receptors?
Origin and Function:
Secreted by the posterior pituitary to regulate water retention.
AVP secretion threshold: ~285 mOsm/L
Works with hypothalamic thirst centers to maintain fluid balance by regulating drinking behavior
Thirst stimulation threshold: ~295 mOsm/L
Stimuli for Secretion:
↑ Plasma osmolality (≥1–2%)
↓ Plasma volume (≥10–15%)
Angiotensin II, nausea, nicotine
Inhibited by ANP (atrial natriuretic peptide),
cortisol, ethanol
Kidney Effect:
Promotes water reabsorption, reducing urine output.
Regulation:
Osmoreceptors detect ECF osmolality changes
Baroreceptors respond to volume changes
Sensitivity increases with lower vascular volume
Degradation:
Transported in free form in the blood. The half-life is ~
15-20 min, degrades in the liver and kidneys
Receptors:
Gq/Ca++ pathway; on vascular smooth muscles, causes contraction
V2: Gs/cAMP/PKA pathway;
on the basolateral side of renal cells: increase water reabsorption.
reduces water excretion in urine
What are osmoreceptors?
Osmoreceptors are sensory receptors in the thirst center (in the hypothalamus, outside of the blood-brain barrier)
Describe the Main effect of ADH in the Kidneys
Short Term Effects?
Long Term Effects?
Main Effect:
ADH (aka AVP) → V2 receptors (on basolateral membrane of renal collecting duct cells) → enhance water reabsorption, concentrate urine, and conserve body water.
Short Term:
ADH → G protein Cascade → insertion of aquaporin-2
(AQP-2) water channels into the apical membrane
Long Term:
increases synthesis of aquaporins
Describe how ADH influences Urine Composition/Flow Rate
ADH role in Urine: ADH → Less Water Excreted in Urine → More Concentrated Urine (***b/c less water in urine = more solutes***)
What disease is associated w/ insufficient ADH response?
Excess ADH?
Insufficient ADH Response – Diabetes Insipidus:
Excess ADH – Syndrome of Inappropriate ADH Secretion (SIADH)
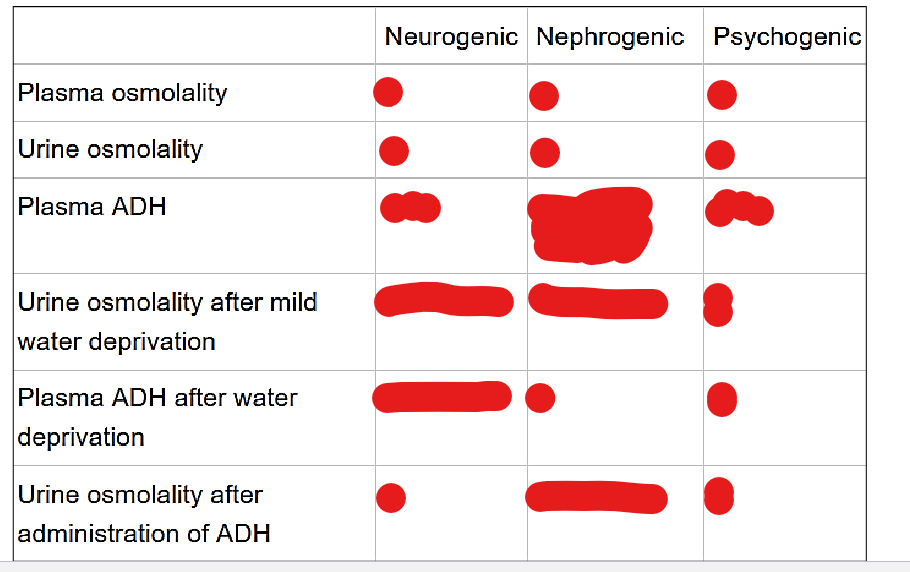
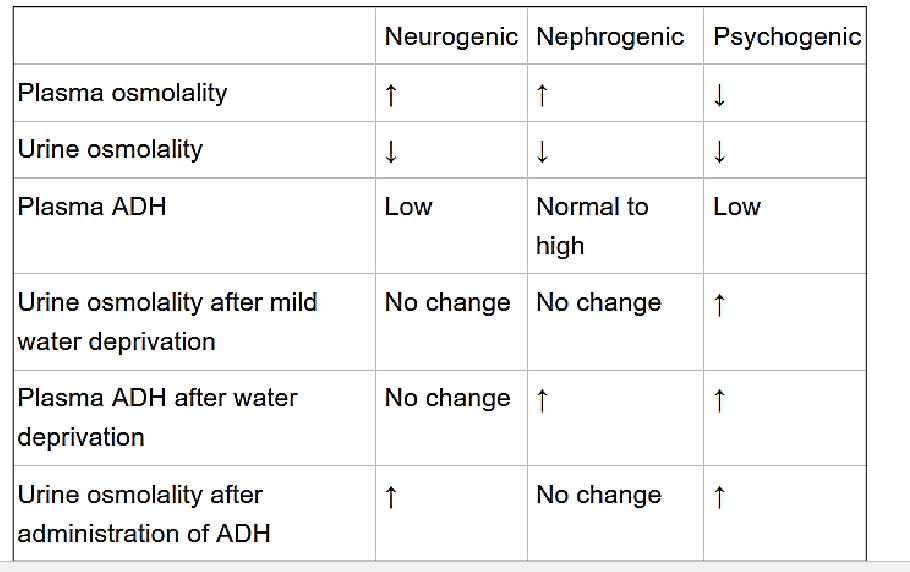
What are the common symptoms of diabetes insipidus (DI)?
Describe the Characteristics of Neurogenic (Central) DI:
What can it be caused by?
DAmages to what structures could also cause this?
Ultimate effect of this?
Describe the Characteristics of Nephrogenic DI:
What mutations cause this?
ultimate effect of this?
Describe the Characteristics of Psychogenic (Primary Polydipsia) DI:
Caused By?
How is it different from true DI
Common Symptoms:
Increased urinary flow (up to 25 L/day)
dehydration
Increased thirst
Neurogenic (Central) DI – Low ADH:
Caused by mutations in the pre-pro-vasophysin (preprohormone) gene
May result from damage to the hypothalamus (e.g., hypothalamic tumors) or posterior pituitary (e.g., metastatic disease)
Leads to insufficient production or release of ADH
Nephrogenic DI – Normal ADH:
Mutations in V2 receptor or Aquaporin-2 (AQP-2) channels
Kidneys fail to respond to ADH
Psychogenic DI (Primary Polydipsia):
Caused by compulsive water drinking behavior
Individuals may respond to ADH treatment, distinguishing it from true DI
What is Syndrome of inappropriate antidiuretic hormone ADH release (SIADH) Characterized by?
Causes of SIADH?
Clinical Characteristics of SIADH?
Treatment?
Complications of hyponatremia?
Characteristics:
unsuppressed release of antidiuretic hormone (ADH) from \
pituitary gland or non-pituitary sources → excessive water retention/hyponatremia
Causes:
CNS Disturbances: Stroke, hemorrhage, infection, trauma, mental illness, psychosis
Drugs and diseases:
Various medications and pain-induced ADH secretion (e.g., post-surgery)
Pulmonary Diseases: Pneumonia (viral, bacterial, tuberculous)
HIV Infection
Mutation in V2 receptor gene (X chromosome) → continuous receptor activation → persistent water absorption and resistance to vasopressin receptor antagonists
Clinical Characteristics:
Increase Plasm ADH
Decrease Plasma Osmolality/ Sodium Levels
Increased Urine Osmolality/ Sodium Levels
Treatment:
Fluid restriction to correct hyponatremia
Complications of hyponatremia:
Headaches, memory issues, depression, tremors, muscle cramps
Severe cases: Cerebral edema leading to respiratory failure, seizures, hallucinations, coma, or death