Arthrogryposis Multiplex Congenita and Osteogenesis Imperfecta
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
60 Terms
what is Athrogryposis Multiplex Congenita
joint contracture in 2 or more body areas
cause of Athrogryposis Multiplex Congenita
fetal akinesia
-decreased uterine fetal movement
severity of Athrogryposis Multiplex Congenita
68% noted for UE and LE involvement
differential diagnosis for Athrogryposis Multiplex Congenita
-osteochondrodysplasia and other dwarfing conditions
-multiple pterygium syndromes (webbing)
-contractural arachdoactyly
-freeman-sheldon syndrome
features of Athrogryposis Multiplex Congenita
-loss of skin creases
-short stature
-abnormal dimpling
-joint stiffness
-fibrotic muscle tissue/weakness
-hypoplasia
-orthopedic deformity (not symmetrical)
-pain
-functional deficits
clinical presentation of Athrogryposis Multiplex Congenita
-UR IR
-elbow flexion
-wrist flexion
-hip contracture or dislocation
-flexion and extension contracture LEs
-clubfeet
infant amyoplasia
intestine or abnormal wall abnormalities
-decreased abdominals, increased lumbar lordosis
UE surgical interventions for Athrogryposis Multiplex Congenita
-proximal humeral osteotomy
-posterior elbow release (stretching and bracing after) (to increase elbow flexion ROM)
-dorsal closing wedge osteotomy (wrist)
LE goals for Athrogryposis Multiplex Congenita
-improve ROM
-bracing
-function
LE surgical Interventions for Athrogryposis Multiplex Congenita
-PMLR's clubfeet
-hip and knee soft tissue releases
-hemiepiphyiodesis
-rotational osteotomy
-extension osteotomy
distal arthrogryposis cause
autosomal dominant trait
clinical presentation of distal arthrogryposis
-increased incidence of scoliosis and kyphosis
-tunk and head is spared
-camptodactyly
camptodactyly
distal arthrogryposis
-medially overlapping fingers
-clenched fists
-ulnar deviation of fingers
interventions for clubfoot deformities (talipes equinovarus)
-stretching
-ponsetti castign
-tenotomy
-bracing
ponsetti casting
clubfoot deformities (talipes equinovarus)
-changed every 1-2 weeks for 4-6 casts

tenotomy for clubfoot deformities (talipes equinovarus)
achilles tendon clipped to lengthen
bracing for clubfoot deformities (talipes equinovarus)
foot aBduction brace
-23 hours for 3 months
-28 hours for 3 months
-14-16 hours night until 4. years old

hemiepiphysiodesis
surgical technique used to gradually correct angular limb deformity in skeletally immature patients
-uses active growth plates to fix deformity
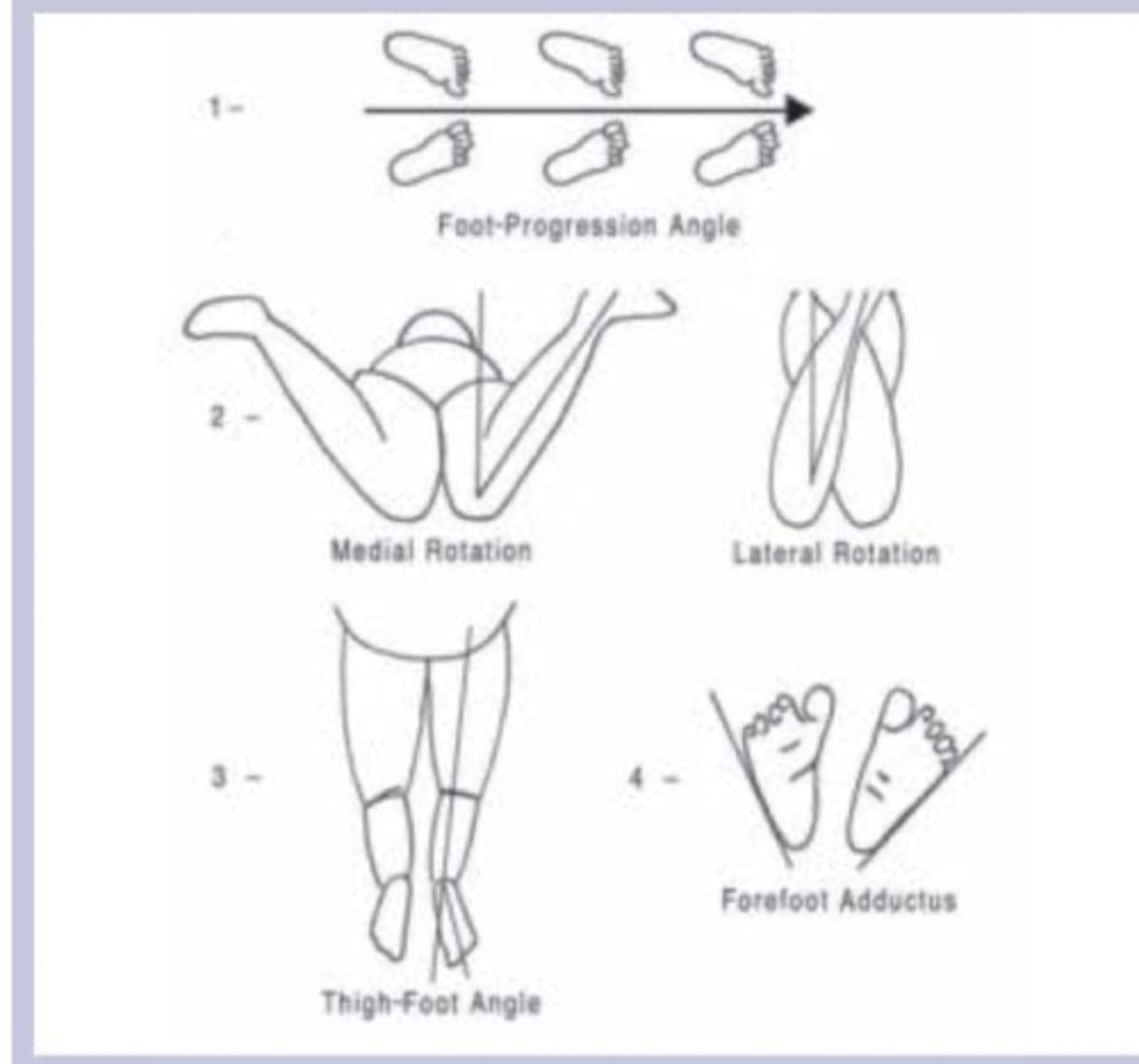
evaluation for torsional deformity
-prone IR/ER for femoral anteversion and retroversion
-thigh foot angle for internal or external tibial torsion
goals for Athrogryposis Multiplex Congenita
-improve function (pt specific)-> modification or orthopedic intervention
-promote independence
-maximize participation
-reduce pain
ways to promote independence for Athrogryposis Multiplex Congenita
-use momentum
-use environment
-practice difficult skills to determine best method
outcome measures for Athrogryposis Multiplex Congenita
-pediatric outcome data collection instrument (PODCI)
-pt reported outcomes measurement information system (PROMIS)
-Endurance (EASE)
-pain scale
-medical outcome study
-gillette functional assessment questionnaire
-2 min walk test
Pain Among Adolescents and Young Adults article
Athrogryposis Multiplex Congenita
-7 day average pain associated with decreased functional mobility
-better coping scores were associated with greater mobility
positioning with Athrogryposis Multiplex Congenita
-infant: preserve and increase ROM
-child: preserve joints to be functional
Osteogenesis Imperfecta (OI) cause
genetic disorder group usually involving type 1 collagen (main building block in bones)
diagnosis of Osteogenesis Imperfecta (OI)
-clinical presentation
-biochemical
-molecular tests
clinical types of Osteogenesis Imperfecta (OI)
-8 main types
-22 genetic mutations identified
Osteogenesis Imperfecta (OI) types I-IV
-silence type original classification system
-based on clinical and radiological classifications
Osteogenesis Imperfecta (OI) types V-VIII
expanded in 2004 and 2007
-due to distinct clinical features
-genetic inheritance of autosomal recessive
Osteogenesis Imperfecta (OI) type I
mild
-most common and most mild type of OI
-few obvious symptoms
-height may be average or slighly shorter than average when compared with unaffected family members, but within normal range for age
order of types for Osteogenesis Imperfecta (OI)
not in order of severity
Osteogenesis Imperfecta (OI) type II
most severe
-numerous fractures and severe bone deformity are evident at birth
-small stature with underdeveloped lungs and low birth weight
-infants may die within weeks from respiratory or other complications
-sometimes referred to as lethal OI
Osteogenesis Imperfecta (OI) type III
severe
-fractures present at birth and x-rays may reveal healed fractures that occurred before birth
-progressive bone deformity is often seen
-short stature
-barrel-shaped rib cage
-spinal curvature and compression fractures of vertebrae
Osteogenesis Imperfecta (OI) type IV
moderate severity
-mild to moderate bone-deformity is often seen
-spinal curvature and compression fracture of the vertebrae
-barrel-shaped rib cage
Osteogenesis Imperfecta (OI) type V
moderate
-similar to type IV in appearance
-large hypertrophic calluses form at fracture or surgical procedure sites
-calcification restricts forearm rotation
genetic inheritance for autosomal dominant Osteogenesis Imperfecta (OI)
types 1-5
-1 parent or spontaneous mutation
genetic inheritance for autosomal recessive Osteogenesis Imperfecta (OI)
types mutation from both parents
Osteogenesis Imperfecta (OI) clinical presentation
-boney deformity
-fractures
-joint hypermobility
-blue sclera
-brittle teeth
-hearing loss
-CNS abnormalities
-arterial dissection
-bruising
-short stature
-triangular face
prenatal diagnosis of Osteogenesis Imperfecta (OI)
usually at 18-34 weeks by ultrasound
differential diagnosis for Osteogenesis Imperfecta (OI)
-child abuse (types I and IV)
-malignancy
-hypogonadism
-juvenile osteoporosis
-infantile hypophosphatasia
physical exam for Osteogenesis Imperfecta (OI)
-head circumference
-limb asymmetry
-scoliosis
-pectus carinatum (pigeon test)
-fontanel size
-ROM
examination for Osteogenesis Imperfecta (OI)
-physical exam
-selective skeletal survey
-DEXA scan
-molecular and biochemical studies of collagen
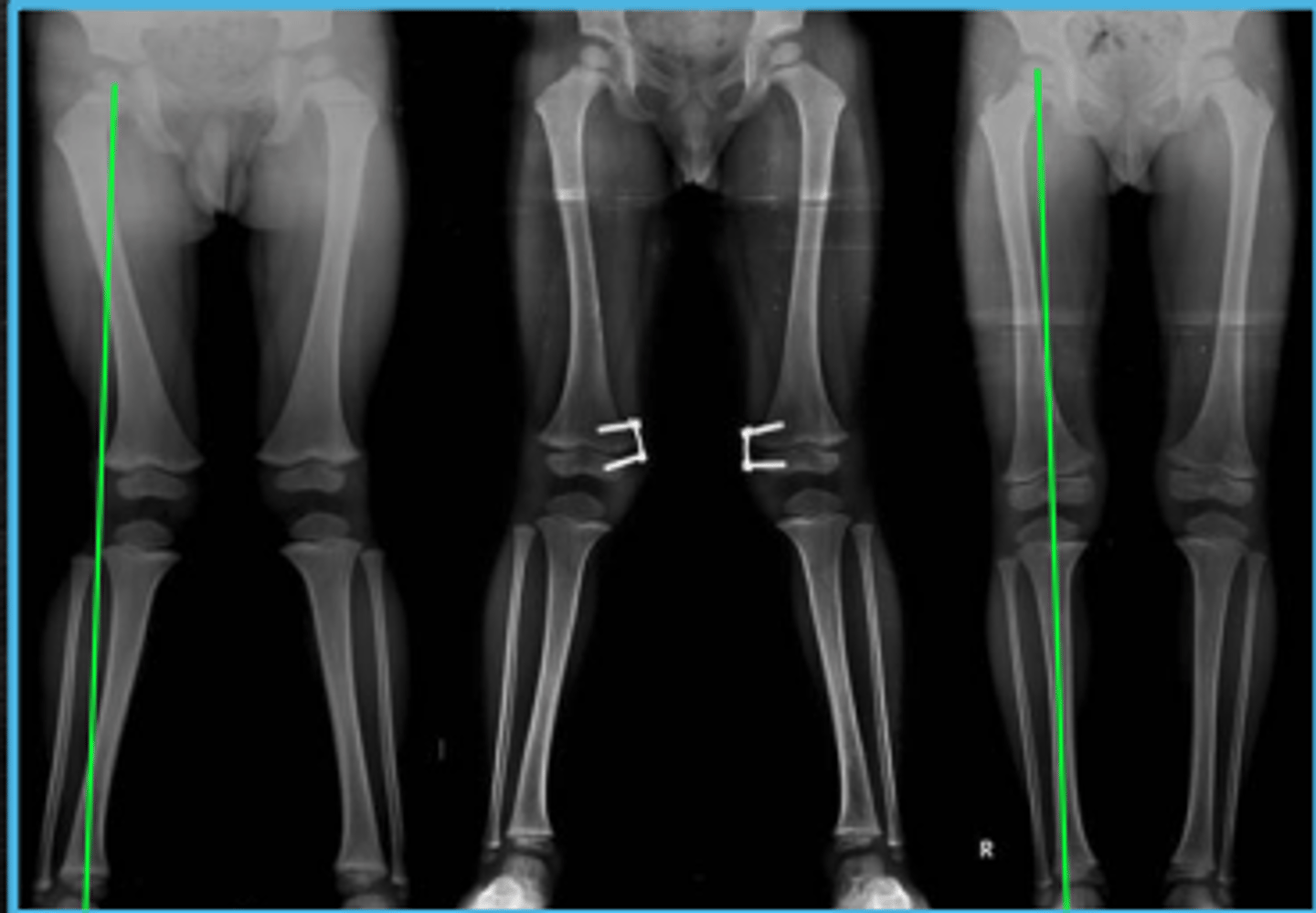
radiographs for Osteogenesis Imperfecta (OI)
-bone mineralization
-fractures/pseudoarthrosis
-alignment/deformity
-fractures might not show up immediately on children
DEXA scans for Osteogenesis Imperfecta (OI)
-use low cost and low dose radiation
-looks at bone mineral density
-lumbar spine and hips are primary sites
-height correction BMD (z-scores) in children with less than or greater than average height)
pharmaceutical treatment for Osteogenesis Imperfecta (OI)
bisphosphonates (diphosphonates)
-not FDA approved for use with OI but standard of care
types of bisphosphonates for Osteogenesis Imperfecta (OI)
-nitrogenous (bone resorption interference)
-non-nitrogenous (apoptosis)
administration of bisphosphonates
-oral
-IV infusion
-IV injection
side effects of bisphosphonates
-heartburn
-photosensitivity
-sore mouth
-bone and muscle pain
-headaches
pharmacokinetics for bisphosphonates
-approximately 50% excreted by the kidneys
-absorbed into the bone
-half life of 10 years
radiographs after bisphosphonate treatment
-pamidronate "zebra lines" at metaphysis
-benign lines of sclerosed non decalcified cartilage that indicate reduced treatment effectiveness

therapeutic goals for Osteogenesis Imperfecta (OI)
-educate on handling and positioning
-fracture reduction
-deformity prevention
-activity precautions/modifications
-promote independent motor skills
orthotics with boney deformities with Osteogenesis Imperfecta (OI)
-support boney fragility for protection and WB activities
-bracing cannot correct procurvatum or other deformity
-orthopedic surgery may be required to facilitate bracing
conservative management for scoliosis with Osteogenesis Imperfecta (OI)
-wheelchair positioning
-orthotics (TLSO)-> not appropriate for all children due to rib fragility
surgical interventions for scoliosis with Osteogenesis Imperfecta (OI)
-Magec Growing Rod (childhood)
-posterior spinal fusion (adulthood)
magec growin rod
for growing patients to prevent shortened stature caused by spinal fusion
-scoliosis surgical intervention with Osteogenesis Imperfecta (OI)
handle with care with Osteogenesis Imperfecta (OI)
-first rule is to listen to the patient and caregivers
-obtain subjective history of fractures and treatment
-allow pt and family to demonstrate their methods
-observe AROM
-determine ROM limitations
-seek out info from specialists
-don't pull arms and legs (during diaper change, rolling)
infant interventions with Osteogenesis Imperfecta (OI)
-positioning
-bed mobility
-head and trunk control
-sitting
-car seats
-floor play
-transitional activities
-weight bearing
-ambulation
adolescents interventions for Osteogenesis Imperfecta (OI)
-scoliosis screening, bracing, surgery
-educate about compression fractures
-low impact activity and strengthening
-independence with WC and gait
-athletic options
-self advocacy
Effect of Bisphosphonates on Function and Mobility Among Children with Osteogenesis Imperfecta article
-mobility scores greater in pts with OI type 1, 3, 4
-4 VP increased mobility as measured by Bleck scores> treatment
-oral BPs had no significant affect on function and mobility
-may increase quality of life but not necessarily function
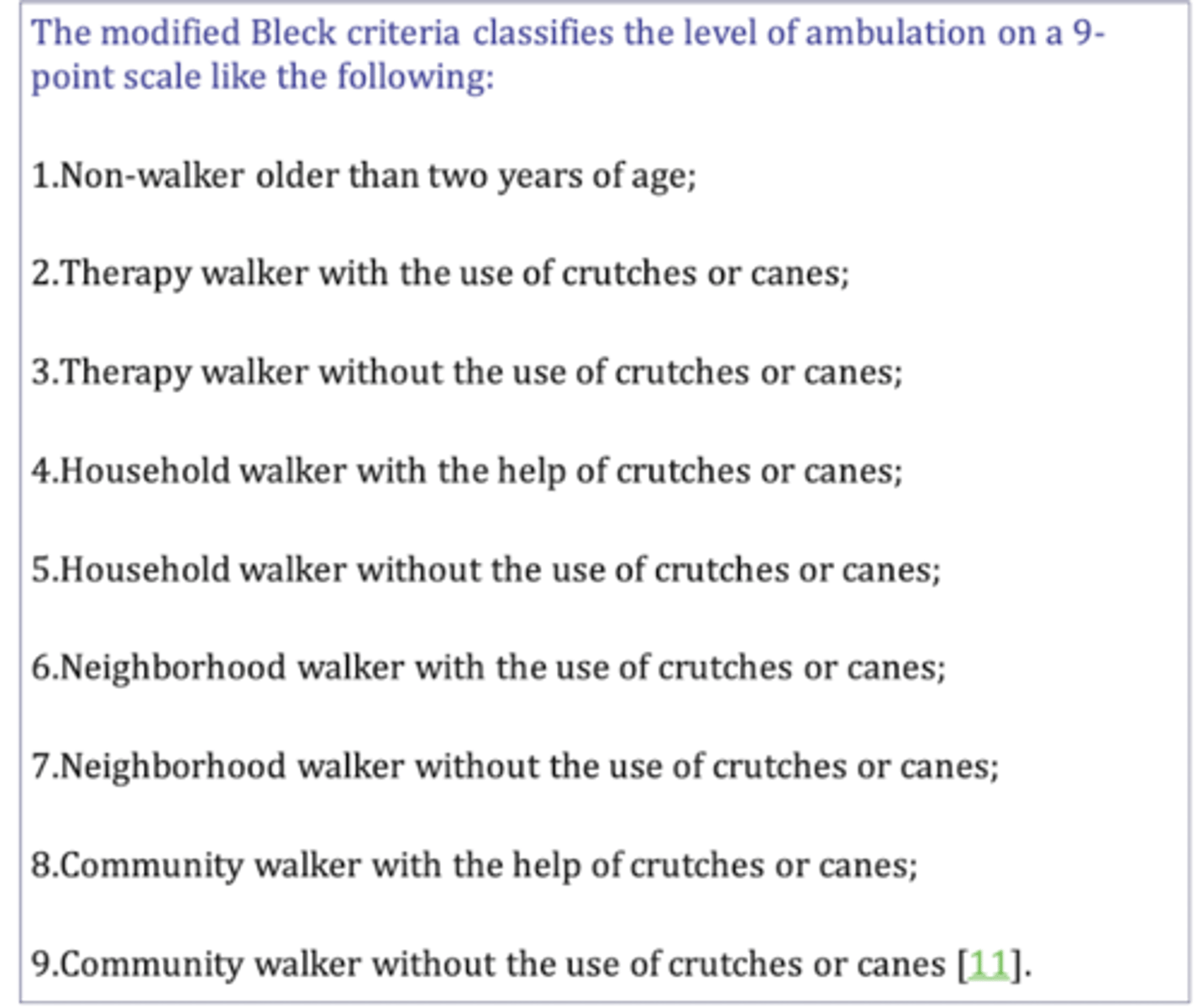
Modified Bleck
levels of ambulation with Osteogenesis Imperfecta (OI) on 9 point scale