Exam 1 Therapeutic Applications
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
47 Terms
AIDET
A- Acknowledge, greet the patient and check ID band
I- Introduce, introduce self, who you are and how you are going to help them
D- Duration, how long you will be in there, as well as keep them updated
E- Explanation, explain procedures/processes/ what you are about to do
T- Thank you, thank the patient for allowing you tow work with them
Along with AIDET:
wash hands
identify patient as needed
provide privacy
infection control (PPE)
leave patient safe and comfortable
SBAR
S- situation
B- background
A- assessment
R- recommendation
Used for report
General Survey
It is the physical appearance, body structure, mobility, and behavior of a patient when you walk in to a room to meet them.
Physical appearance- age, gender, LOC, skin color, facial features, overall appearance
Body structure- stature, nutrition, symmetry, posture, position, body build/contour, physical deformities
Mobility- gait, range of motion
Behavior- facial expression, mood and affect, speech pattern, dress, hygiene
Subjective vs objective:
subjective- what the patient tells you, (pain rating, nausea, anxiety, fatigue)
objective- what you observe, (appearance of patient, vital signs, lab results)
Sorting assessment data
Physical assessment techniques
Physical assessment technique - Inspection
always comes FIRST
begins when you first meet the patient with a general survey
start assessment of each body system with inspection- compare right side to left side
Physical assessment technique - Palpation
texture, temperature, moisture, size, shape, degree of tenderness
Techniques:
finder pads→ pulses, texture, size, consistency
dorsa (back) of hand→ best for determining temperature because skin here is thinner than on palms
palm of hand→ best for vibrations, fremitus
start with light pressure and increase only when needed
Physical assessment technique - Percussion
Tapping a persons skin with short, sharpp strokes to assess underlying structures
Uses it for:
mapping location/size of organs
signaling density or emptiness of structure
detecting a superficial abnormal mass
elicting deep tendon reflex using percussion hammer
Two methods:
- Direct→ directly “strike” the body with hand
- Indirect→ striking hand hits nurses own hand
Resonance- hollow, low pitched sound
Tympany- loud, high-pitched, drumlike
Dull- muffled thud, high-pitched
Flat- absolute dullness
Physical assessment technique - Auscultation
listening to sounds produced by body
most body sounds are soft and must be channeled through a stethoscope
stethoscope does not magnify sound, but it blocks out extraneous sounds
once you can recognize normal sounds, you can distinguish the abnormal sounds and “extra” sounds
How to use the stethoscope
Diaphragm- high-pitched sounds
breath- wheezes, crackles
bowel sounds- “gurgling”
normal heart- S1/S2
Bell- low-pitched sounds
murmurs
bruits
PQRSTU
P- provoke, palliative (what makes the pain better or worse?)
Q- quality (what does the pain feel like?)
R- radiate, region (does the pain move anywhere?)
S- severity (how would you rate your pain 0-10?)
T- timing, treatment (when did the pain start?, Tried any treatments?)
U- understanding (what do you think is watching the pain?)
Chronic vs Pain
Acute-
short term
self-limiting
follows a predictable trajectory
dissipates after injury heals
Chronic-
continues for months or years
does not stop when injury heals
malignant vs nonmalignant
Fall Prevention
- result in minor to severe injuries
- reduce mobility and independence
- increase the risk of premature death
- patients who have underlying disease states are more susceptible to fall related injuries
- any aged person can be at risk
Hester Davis Fall Risk Assessment
Age-
<20 = 0 points
20-40 = 1
41-60 = 2
>60 = 3
Last known fall-
no falls = 0
within the last year = 1
within the last 6 months = 2
within the last month = 3
during the current hospitalization = 4
Mobility-
no limitations = 0
dizziness or generalized weakness = 1
immobilized or requires assist of 1 = 2
use of assistive device or requires 1 or more = 3
hemiplegic, paraplegia, or quadriplegic = 4
Medications-
no meds = 0
cardiovascular or CNS meds = 1
cardiovascular and CNS meds = 2
diuretics = 3
chemotherapy in the last month = 4
Mental Status/LOC/Awareness-
awake, alert, oriented to date, place, and person = 0
oriented to person and place = 1
lethargic or oriented to person only = 2
memory loss or confusion and requires redirecting = 3
unresponsive or noncompliance with instructions = 4
Toileting needs-
no needs = 0
use of catheters or diversion devices = 1
use of assistive device = 2
incontinence = 3
diarrhea, frequency, or urgency = 4
Volume/Electrolyte status-
no problems = 0
NPO >24hrs = 1
use of IV fluids or tube feeds = 2
nausea/vomiting = 3
low blood sugar or electrolyte imbalances = 4
Communication/Sensory-
no deficits = 0
visual (glasses) or hearing deficit = 1
non-english pt, unable to speak, slurred speech = 2
neuropathy = 3
blindness or recent visual change = 4
Behavior-
appropriate behavior = 0
depression or anxiety = 1
behavioral noncompliance = 2
ethanol or substance abuse = 3
impulsiveness = 4
A score >7 indicates a high fall risk
Med administration (7 rights)
Right patient
Right drug
Right dose
Right route
Right time
Right reason/indication
Right documentation
Med administration safety
Routes of administration
enteral
topical
inhalation
irrigation
parenteral
Controlled substances
l - high abuse potential, no accepted medical use (heroin, marijuana)
ll - high abuse potential, may lead to severe dependence, must have written prescription (opium, morphine, codeine, oxycodone)
lll - less abuse potential, may lead to MOD or LOW dependence (limited quantities of opioids)
lV - less abuse potential, may lead to limited dependence (valium)
V - low abuse potential, may lead to limited dependence (cough syrups)
Narcotics in acute care:
- kept in secure locked area
- nurse administering NARC signs it out
- NARCOTICS are counted every shift by 2 nurses
- verifying amount every time
wasting of NARCOTICS
- must be witnessed by TWO licensed care providers RN or LPN
- document the amount of narcotic wasted
Basic pharmacokinetics
Know; generic name, trade name, drug classification
- never administer an unfamiliar medication
- utilize your critical thinking to assess the medication properties in relationship to your patients individual condition
- is this safe to administer
Types of medication action:
Therapeutic effect→ expected or predicted physiological response
Side effect→ unavoidable secondary effect
Adverse effect→ unintended, undesirable, often unpredictable
Toxic effect→ accumulation of medication in the bloodstream
Idiosyncratic reaction→ over-reaction or under-reaction or different reaction from normal
Allergic reaction→ unpredictable response to a medication
Medication dose responses:
Onset: time it takes for a medication to produce a response
Peak: time at which a medication reaches its highest effective concentration
Trough: minimum blood serum concentration before next scheduled dose
Duration: time medication takes to produce greatest result
Plateau: point at which blood serum concentration os reached and maintained
Biological half-life: time for serum medication concentration to be halved
Insulin administration
Standard precautions/handwashing
Standard precautions- all patients
Handwashing- single most effective method of preventing transmission of microorganisms from one patient to another
hand sanitizer/handwashing with soap
Isolation precautions
Types of Isolation Precautions
1) standard precautions- all patients
2) droplet precautions-
influenza, rubella, mumps, pneumonia
gloves and mask when entering room
limit transports and visitors
3) airborne precautions-
negative pressure room with frequent air exchange
respiratory or fitted mask when entering room
only transport patient out of room if absolutely necessary(place mask on patient)
borne precautions (TB, chicken pox, SARS)
4) contact precautions-
gloves and gown when entering
Atelectasis
partial or complete collapse of the lung that can cause SOB, etc
Respiratory interventions
Hypoventilation
Alveolar ventilation inadequate to meet the body’s oxygen demand or to eliminate sufficient carbon dioxide
Hyperventilation
Ventilation in excess of that required to eliminate carbon dioxide produced by cellular metabolism
Hypoxia
inadequate tissue oxygenation at the cellular level
Hypoxemia
low level of oxygen in the blood
Lung sounds
Pathophysiology of wheezes and crackles
Crackles-
Fine→ discontinuous, popping, intermittent explosive sounds (sudden opening of airways [alveoli]) shorter duration than course crackles
Course→ intermittent bubbling sound, inspiration/expiration or both, caused by fluid
Wheezes-
high pitched, whistling/squeaking sounds
can be heard on expiration or during both inspiration and expiration
caused from narrowed airways in the lungs
Chest tube management/ patient safety
If the patient has the following:
-pneumothorax (air in chest cavity)
-hemothorax (blood in chest cavity)
-pleural effusion (fluid in chest cavity)
-empyema (pus in chest cavity)
-post-operative care (thoracic surgeries)
A nurse checks:
tidaling→ this is normal, the ball rises and falls with breathing
bubbling in the water-seal chamber
this may be abnormal, signifies and air leak
this is normal finding with pneumothorax
chest tube is upright, below the level of the chest, and secure
Cardiac base vs apex of heart
Cardiac cycle
S1 and S2 sounds
Cardiac assessment subjective vs objective
Signs of heart failure, dyspnea, nocturia, orthopnea
cardiac, respiratory, peripheral vascular, mental status, nutrition, fluid balance/kidneys
Orthopnea→ how many pillows do you use when sleeping or lying down?
Dyspnea→
Nocturia→ do you awaken at night with an urgent need to void? how long has this been occurring?
Cyanosis/pallor→ have you ever noticed your facial skin turn blue or ashen?
Peripheral vascular, the P’s, grading pulses, edema
Describe the location of each area where you can assess a pulse on someone
Edema, pitting edema score +1 to +4
Preventing post op complications, pneumonia, UTI, VTE (blood clots)
Sitting up in bed
Walking as soon as possible
Review common post op complications Doc
Types of exudate (whats going on and whats bad/concerning)
How to assess all cranial nerves
12 pairs
CN I Olfactory- sensory: smell
smell something
CN II Optic- sensory: visual acuity and peripheral fields
count fingers or movement in all quandrants and periphery in each type
CN III Oculomotor- motor: controls eye movements and pupillary muscles, (PERRLA- pupils are equal, round, reactive to light, and accommodating)
move eyes in all directions except outward and down and in
CN IV Trochlear- motor: controls superior oblique muscle of the eye, eye moves in and down and out
CN V Trigeminal- sensory: upper, mid and lower face (including cornea, inside mouth and nose), motor: controls masseter muscle (chewing)
3 branches, sensation to face
ability to chew
CN VII Facial- sensory: taste with anterior 2/3 of tongue (sweet, salty, some sour), motor: facial expressions
moves face, make facial expression
CN VI Abducens- motor: abduction movements of eye (CN III, IV, & VI motor function can be tested all at once with this test)
give the side eye
CN VIII Acoustic- sensory: able to hear and balance
snap in both ears
CN IX Glossopharyngeal- sensory: taste to posterior 3rd of tongue (bitter), motor: controls swallowing
swallow
CN X Vagus- sensory: gag reflex, motor: enervates the gut, heart, and larynx
gag reflex?
CN XI Spinal accessory- motor: enervates sternocleidomastoid and trapezius muscles
push on shoulders, have them push up
CN XII Hypoglossal- motor: enervates the muscles of the tongue
stick out tongue
What is vasovagal response?
Vagus nerve is overstimulated- results in bradycardia, vasodilation- vasovagal syncope (fainting) can happen with straining during constipation
Normal vs abnormal findings of cranial nerves
size, shape, and symmetry
light reflex
brain injury
unilateral dilated, nonreactive pupil is ominous
from increasing intracranial pressure
The role of the lobes/areas of the brain
4 Lobes:
Frontal(front)→ concerns with personality, behavior, emotions, and intellectual function
Broca’s area(towards front)→ understands language but cannot express themself verbally
Parietal(middle)→ receives and processes sensations from the body- touch/pain/temp/shapes
Occipital(back)→ processes info related to vision, influences ability to read
Temporal(bottom)→ regulates hearing, taste and smell, participates in language and learning
Wernicke’s area(middle)→ speech comes out but may not make any sense, incomprehensible
Glasgow coma scale
Tool to assess LOC
A change in LOC can be subtle and can start with confusion
Eye opening
spontaneously = 4
to speech = 3
to pain = 2
none = 1
Verbal response
oriented = 5
confused = 4
inappropriate = 3
incomprehensible = 2
none = 1
Motor response
obeys commands = 6
localises to pain = 5
withdraws from pain = 4
flexion to pain = 3
extension to pain = 2
none = 1
Maximum score 15
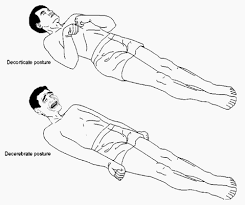
Abnormal posturing while doing painful stimuli, what do they look like
Decorticate- abnormal posturing where a person is stiff with bent arms, clenched fists, and legs held out straight
Decerebrate- involuntary body position that’s a sign of severe brain damage or major disruptions in brain function
When is it appropriate to do a full neuro assessment vs a focused neuro assessment
Complete neuro assessment: q4h
people of concerns with: headache, weakness, loss of coordination, and show signs of neurologic dysfunction
1) Mental status and LOC
2) Cranial nerves
3) Motor system
4) Sensory system
5) Reflexes
Focused neuro assessment:
1) LOC
2) Motor function
3) Pupillary response
4) Vital signs