Lungs, breathing and Lung function tests.
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
What are the divisions of the bronchial tree?
17 divisions before alveoli, total 23 divisions
What is the nomenclature of surfactant ?
Anti-Surface
= Surf-actin
What cells is the alveoli epithelium lined by?
Alveolar type I- Gas exchange
Alveolar type II- Pneumocytes, aka stem cells, surfactant production
What tension is type 2 cells responsible to resolve?
Surface tension.
Force between molecules of water casing collapse of alveoli
How do type 2 pneumocytes appear and where in them is surfactant secreted?
Cubical secretory granules
Contain lamellar bodies that produce surfactant.
What is surfactant?
Made of oil and protein
Phosphotydlcholine (lecithin)
Phosphatydylglycerol
At what gestational age does surfactant production start?
28/40
Why is premature birth a risk in terms of surfactant?
Prem babies have decreased surfactant resulting in lung collapse, less surface tension, resulting increased risk of collapse.
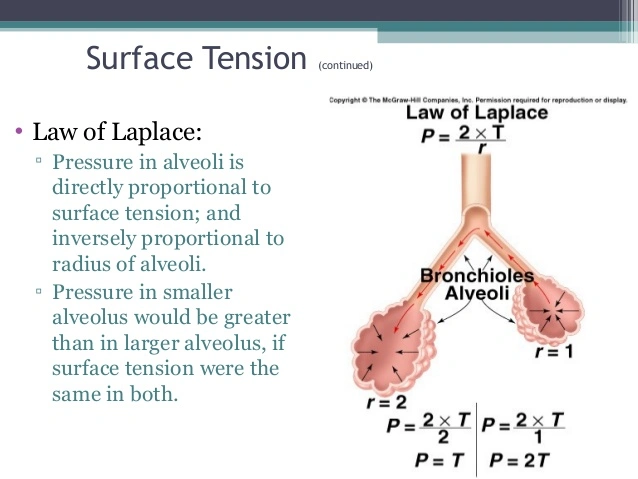
What is collapsing pressure?
Surface tension over radius (aka leplace law)
What stimulates surfactant production?
Cortisol
Thyroxin
Prolactin
What inhibits surfactant production?
Insulin
Define lung compliance.
The ability of the lung to collapse
Change in volume over (divide by) change in pressure.
What causes recoil?
Surface tension- 2/3
Elasticity ( elsatin and collagen)- 1/3
Name 3 types of spirometers?
Water seal spirometer
Dry rolling-seal spirometer
Bellows/ Wedge spirometer
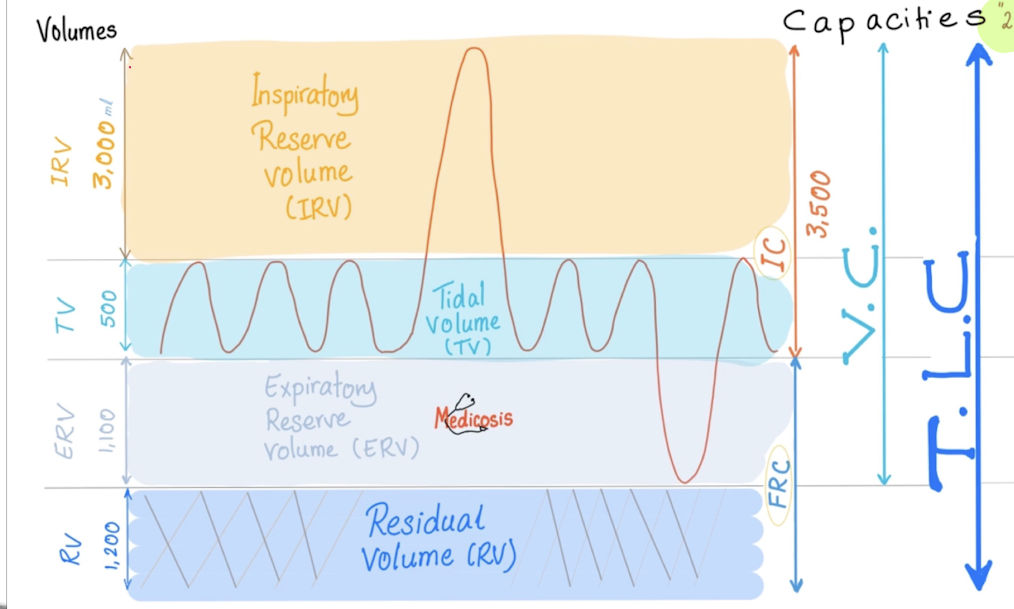
In spirometry, what is the difference between a volume and a capacity?
A volume is one entity
A capacity is 2 or more entities.
What muscles are involved in
Normal inhalation
Forced expiration
Forced inspiration?
Normal- Diaphragm and internal intercostal
Forced expiration-Abdominal muscles and intercostal muscles
Forced insp
Diaphragm
Ext intercostals
Sternocleidomastoids
Serratus anterior
Scalenes
Which volume cannot be meaured ( plus capacities)
Residual volume
FRC and TLC (Both need RV to calculate)
Define tidal volume
All the air breathed in and out during normal respiratory cycle (tidal, like tides in sea)
+- 500ml
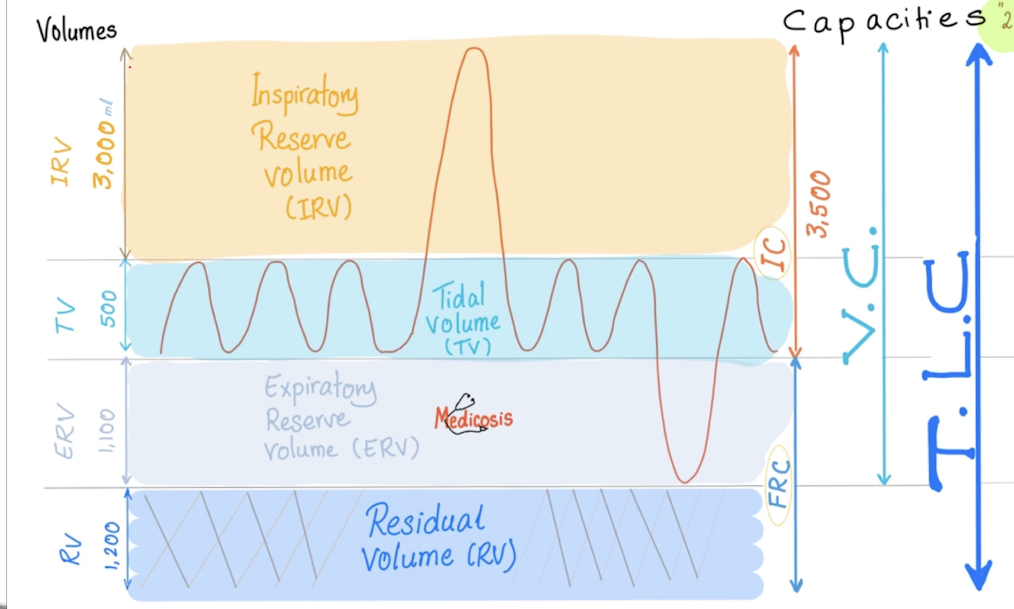
Define inspiratory reserve volume and expiratory reserve volume.
IRV- Max # of air inspired above TV
+- 300ml
ERV- Max # air expired
Define Inspiratory Capacity, Residual Volume , Functional Residual Capacity ,Vital Capacity and Total Lung Capacity.
IC= IRV +TV
RV= Air remaining after max expiration
FRC= RV + ERV
VC= Max amount that can be inspired and expired
TLC= IRV+TV+ERV+RV
What is the residual volume utilized for?
After stabbing, RV escapes, what is the remaining air called?
Maintains aeration of blood
E.g HR is 72bpm and RR is 12bpm, RV utilized while waiting for next cycle of resp.
Remaining air after stabbing aka Minimal air
What is the difference between FRV and FVC?
FVC= Maximally inhale then maximally exhale forcefully and quickly
FRC= ERV +RV
Discuss FEV1/FVC
FEV1= # air quickly and forcibly exhaled in 1 sec after max inhalation in 1 second
FVC= # air quickly and forcibly exhaled after max inhalation- timed.
Normal ratio= 80%
What are the features of obstructive lung disease?
Air trapping
Destroyed elastin resulting in decreased elastic recoil
Increased compliance
PFT features
RV , FRV, TLC increased
FEV1/FVC decreased
What are features of Restrictive lung disease?
Decreased compliance
Normal recoil
Types
Intrinsic- Lung
Extrinsic- Thoracic wall
PFT
RV, FRC, TLC, FVC decreased
FEV 1 /FVC= Normal or high
Define the flow volume loops.
Characteristic triangular shape
Peak triangle = Peak expiratory flow rate (PEFR)
Positive deflection is expiration
Negative deflection is inspiratory flow
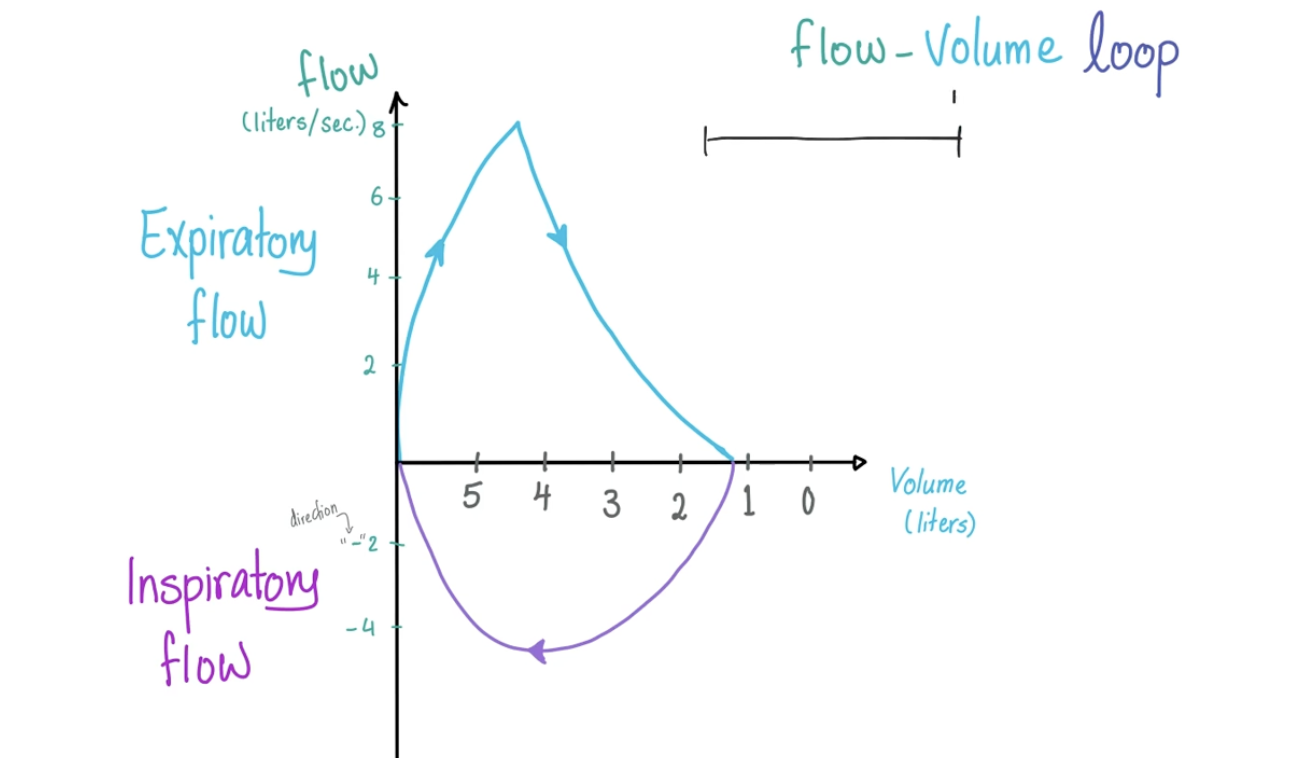
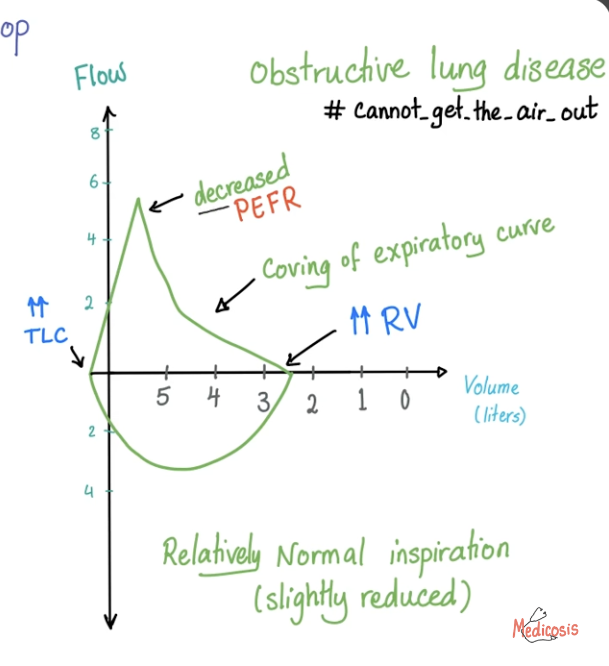
Discuss flow volume loop with obstructive lung disease.
Air cannot come out
PEFR decreased
Coving of expiratory curve
Inspiration relatively normal
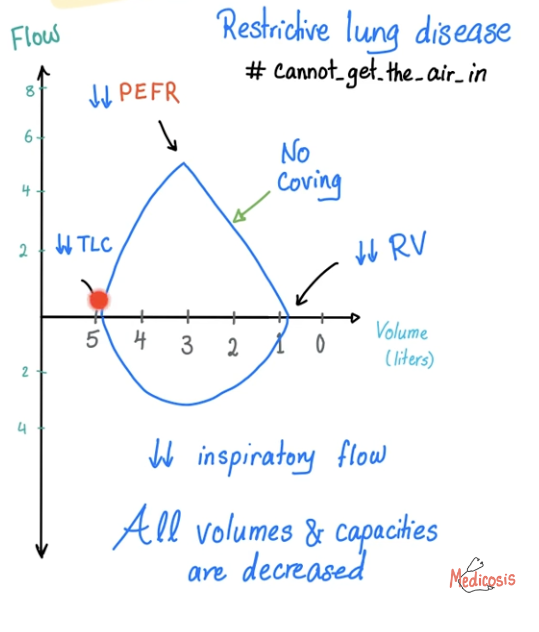
Discuss flow volume loops in regards to restrictive lung disease.
Air can’t come in
Decreased volumes and capacities
Decreased PEFR
No coving- Normal expiration
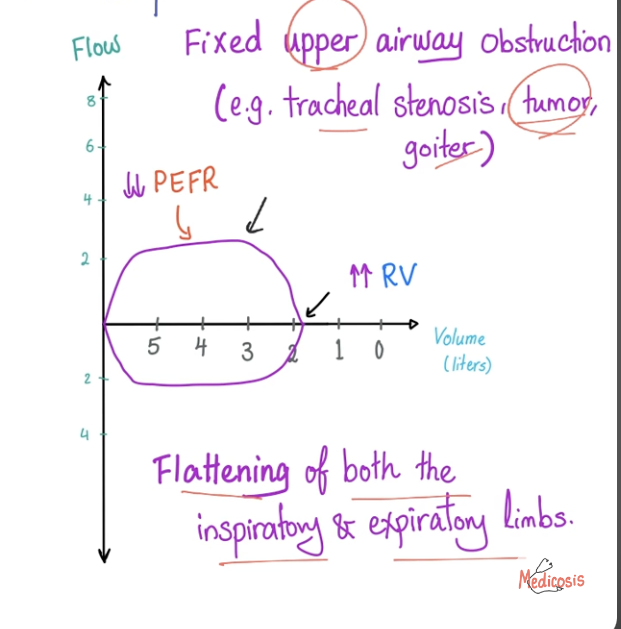
Discussed Flow volume loops in fixed upper airway obstruction.
Air can’t get in or out e.g upper airway obstruction- trachea, goitre
Flattening of both insp and exp limbs
Name the lung protective strategies.
Lower tidal volume of 4-8 ml/lg of IBW
Lower plateau pressures": <30 cm of H2O
Higher peep
Spontaneous breathing trials
Conservative fluid
Prone positioning
NIV
Paralysis
Permissive hypercarbia- to achieve lower plateu pressures and TV except in metabolic acidosis and high ICP
Why is prone positioning utelised in ARDS?
Most infiltrates are seen in dependent areas
Prone positioning redistributes blood flow and ventilationto least affected areas of lung
Promote secretion clearance
Shifts mediastinal contents anteriorly to assist recruitment of atelectatic regions
What are the downside of proning
Improvements if PF ratio seen with proning are transient , does not improve clinical outcomes, time on ventialtion or time in ICU