Anatomy - Module 13 2026 Ratio
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
C. Ischial spine
A pregnant patient currently on labor, was noted to have arrest of fetal head descent at station 0. Which anatomical structure could have possibly caused this?
A. Ischial tuberosity
B. Sacral promontory
C. Ischial spine
D. Symphysis pubis
D. Pelvic inlet is inadequate
An examiner performed an internal vaginal exam and measured the distance between the sacral promontory and the inferior border of the symphysis pubis. The obtained measurement was 11cm. Ultrasound revealed that the fetal head size is at 10.5cm in diameter. Which of the following statement is correct?
A. An arrest of fetal head descent in station zero is more likely
B. Midpelvic plane is contracted
C. Fetal head entrapment may occur in the outlet
D. Pelvic inlet is inadequate
B. Rectovesical
If a female patient will undergo hysterectomy (surgical removal of the uterus), which peritoneal recess will become present?
A. Uterovesical
B. Rectovesical
C. Rectouterine
D. Supravesical
E. Pararectal
A. Iliac crest
The 4th lumbar vertebra is at the same level of which pelvic structure?
A. Iliac crest
B. Ischial spine
C. Sacral promontory
D. ASIS
A. Divergent
When the ischial tuberosity is more lateral than the ischial spine, the pelvic side wall is described as _____________.
A. Divergent
B. Parallel
C. Convergent
B. Ischial tuberosities
When the examiner makes a fist and place the knuckles in front of the patient’s vulva while trying to feel the bony prominence on the side of the knuckles, the physician is trying to palpate which structure?
A. Ischial spines
B. Ischial tuberosities
C. Pubic ramus
E. Ischial spine
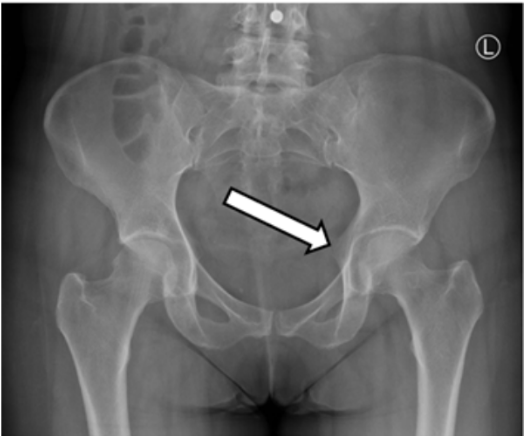
Identify the anatomical structure being pointed by the white arrow.
A. Iliopectineal line
B. Anterior superior iliac spine
C. Ischial tuberosity
D. Posterior inferior iliac spine
E. Ischial spine
D. Subpubic angle = 52 degrees
Given a fetal head size of 9cm, which of the following would be a concern during normal vaginal delivery?
A. Non-palpable ischial spine
B. Anatomical conjugate of the outlet = 8cm
C. Diagonal conjugate = 11cm
D. Subpubic angle = 52 degrees
B. Rectouterine
If a ruptured ovarian pregnancy is suspected, blood will be expected to collect in which of the following recess?
A. Supravesical
B. Rectouterine
C. Pararectal
D. Uterovesical
E. Rectovesical
A. Primordial germ cell, spermatogonium, spermatocyte, spermatid, spermatozoon
What is the correct sequence in the development of male gametes?
A. Primordial germ cell, spermatogonium, spermatocyte, spermatid, spermatozoon
B. Primordial germ cell, spermatocyte, spermatogonium, spermatozoon, spermatid
C. Primordial germ cell, spermatogonium, spermatocyte, spermatozoon, spermatid
D. Primordial germ cell, spermatocyte, spermatogonium, spermatid, spermatozoon
B. Type Ap spermatogonia --------> Type B spermatogonia
Which stage of spermatogenesis wherein cytoplasmic bridges start to appear?
A. Type Ad spermatogonia --------> Type Ap spermatogonia
B. Type Ap spermatogonia --------> Type B spermatogonia
C. Type B spermatogonia --------> Primary spermatocytes
D. Primary spermatocytes --------> Secondary spermatocytes
D. Pachytene
What stage in meiosis I wherein genetic recombination happens:
A. Diplotene
B. Diakinesis
C. Zygotene
D. Pachytene
E. Leptotene
B. Secondary spermatocytes
Which stage of the sperm cell is difficult to find in routine histologic preparation of the seminiferous tubule?
A. Primary spermatocytes
B. Secondary spermatocytes
C. Spermatogonia
D. Spermatids
B. Golgi
What phase in spermiogenesis wherein the centrioles move towards the pole that is opposite the acrosomal vesicle.
A. Acrosomal
B. Golgi
C. Maturation
C. Capacitation
What is the biochemical process wherein spermatozoa become physiologically mature?
A. Spermiogenesis
B. Meiosis
C. Capacitation
D. Spermatocytogenesis
B. Tunica albuginea
What is the tough fibrous capsule that encloses the testis?
A. Skin
B. Tunica albuginea
C. Mediastinum testis
D. Cremasteric muscle
B. Leydig
What are the cells embedded in the intertubular connective tissue stroma of the testis?
A. Basal
B. Leydig
C. Principal
D. Sertoli
D. Tubuli recti
What are straight tubes located at the mediastinum testis that are continuation of the seminiferous tubules?
A. Rete testis
B. Ductuli efferentes
C. Ductus epididymis
D. Tubuli recti
B. The testicular arteries arise from the abdominal aorta.
Which statement is true regarding the testis?
A. The epididymis is made up of rete testis and ductus epididymis.
B. The testicular arteries arise from the abdominal aorta.
C. The ductus deferens is part of the intratesticular ducts.
D. The testis is divided into complete lobes by the capsule.
C. Main
What prostatic glands occupy the peripheral 2/3 of the prostate gland?
A. Submucosal
B. Mucosal
C. Main
D. Tyson
D. The mucosa has small round cells that are likely stem cells for the epithelium.
Which statement is true regarding a seminal vesicle?
A. Consists of multiple, highly coiled tubes bound by fibromuscular tissue.
B. Secretes PSA that helps liquefy coagulated semen for slow release of sperms.
C. The muscular layer is made up of inner, middle and outer smooth muscle fibers.
D. The mucosa has small round cells that are likely stem cells for the epithelium.
B. Bulbourethral
Which accessory gland of the male reproductive system does not contribute a significant amount to the volume of the semen?
A. Prostate
B. Bulbourethral
C. Seminal vesicle
A. Zonula occludens
What type of junctional complex that divides the lumen of the seminiferous tubules into basal and adluminal compartments?
A. Zonula occludens
B. Desmosomes
C. Zonula adherens
D. Gap junction
D. None of the above
The Transversus Abdominis muscle is the origin of which layer of the spermatic cord?
A. Cremaster muscle and fascia
B. External Spermatic fascia
C. Internal Spermatic fascia
D. None of the above
A. Urethra
The Corpus Spongiosum is pierced centrally by what anatomical structure?
A. Urethra
B. Dorsal nerve of the penis
C. Deep artery of the penis
D. Ureter
B. Prostatic
Which part of the Male urethra is considered to be the widest & most distensible?
A. Spongy
B. Prostatic
C. Intermediate
D. Preprostatic
C. Tunica albuginea of the penis
A blunt force or trauma in an erected penis may lead to rupture or injury of what anatomical structure?
A. Intramural part of the male urethra
B. Ejaculatory duct
C. Tunica albuginea of the penis
D. Tunica vaginalis
A. Ductus deferens
Vasectomy is a male sterilization technique which will primarily involve the cutting or ligation of what anatomical structure?
A. Ductus deferens
B. Epididymis
C. Ejaculatory duct
D. Spermatic cord
C. 18 – 22cm
What is the average length of a male urethra from the internal urethral orifice up to the external urethral orifice?
A. 1.8 – 2.2cm
B. 10 – 15cm
C. 18 – 22cm
D. 8 – 10cm
D. Prostatic
The Ejaculatory duct will open at what part of the male urethra?
A. Intramural
B. Spongy
C. Intermediate
D. Prostatic
C. Deep perineal pouch
The Bulbourethral glands are found within what anatomical space?
A. Ischiorectal fossa
B. Alcock’s canal
C. Deep perineal pouch
D. Superficial perineal pouch
D. Dartos muscle
Identify which of the following muscles is responsible for the wrinkled appearance of the scrotum.
A. Detrusor muscle
B. Ischiocavernosus muscle
C. Bulbospongiosus muscle
D. Dartos muscle
D. Meiosis I is not completed until the female reaches sexual maturity. (B. When primary oocytes are in the resting period, they are said to be at diplotene phase.)
Which statement is true regarding oogenesis?
A. When the ovum is formed, meiosis II is immediately started and completed.
B. When primary oocytes are in the resting period, they are said to be at diplotene phase.
C. At birth, the female has about two million primary and secondary oocytes.
D. Meiosis I is not completed until the female reaches sexual maturity.
D. Theca interna
What cells in the ovarian follicle produce the precursor of the hormone testosterone?
A. Secondary oocyte
B. Granulosa
C. Primary oocyte
D. Theca interna
D. Graafian
What ovarian follicle has a single layer of flattened epithelial cells encasing the oocyte?
A. Secondary
B. Primordial
C. Primary
D. Graafian
A. Cortex
What area in the ovary contains the ovarian follicles?
A. Cortex
B. Tunica albuginea
C. Germinal epithelium
D. Medulla
A. Antrum
What histologic structure signals that the primary follicle is already a secondary follicle?
A. Antrum
B. Corona radiata
C. Theca folliculi
D. Zona pellucida
D. Zona pellucida
What is the thick glycoprotein membrane that surrounds the oocyte in a follicle?
A. Corona radiata
B. Theca folliculi
C. Antrum
D. Zona pellucida
B. Distal third (C. Middle third)
What part of the fallopian tube where fertilization usually occur?
A. Proximal third
B. Distal third
C. Middle third
C. When spermatozoon enters the ovum.
When is meiosis II of the oocyte completed?
A. When secondary oocyte is formed.
B. When the follicle ruptures at the stigma.
C. When spermatozoon enters the ovum.
D. When the spermatozoon’s and the ovum’s membranes fuse.
B. Peg
What cells in the fallopian tubes secrete nutrients for the conceptus?
A. Ciliated
B. Peg
C. Endothelial
D. Smooth muscle
B. Secretory
What phase of the endometrial cycle wherein the glands become tortuous?
A. Menstrual
B. Secretory
C. Proliferative
B. Labia majora
What structure of the external genitalia is the homologues of the scrotum?
A. Clitoris
B. Labia majora
C. Major vestibular glands
D. Labia minor
B. Nabothian
What cyst is formed when the ducts of a cervical gland get clogged?
A. Minor vestibular gland
B. Nabothian
C. Uterine gland
D. Bartholin’s gland
A. Adipose tissue determines size of inactive mammary gland.
Which statement is true regarding the mammary gland?
A. Adipose tissue determines size of inactive mammary gland.
B. Lactiferous ducts merge to form a lactiferous sinus.
C. The glands of Montgomery open at the nipple.
D. Consists of 15 to 20 separate simple tubuloalveolar glands.
B. Apocrine
Which mechanism is used to secrete fat produced in the mammary gland?
A. Holocrine
B. Apocrine
C. Merocrine
B. Mesovarium
The Ovaries are suspended within the pelvis by a short mesentery called:
A. Mesosalpinx
B. Mesovarium
C. Mesometrium
B. Suspensory ligament
What anatomical structure is attached on the lateral aspect of the ovaries, and is considered as a peritoneal fold wherein the ovarian vessels will pass through to supply the ovaries?
A. Ovarian fimbria
B. Suspensory ligament
C. Round ligament
D. Ovarian ligament
D. Posterior fornix
A 33 y/o female patient was suspected of having a Ruptured Ectopic pregnancy. The attending physician wanted to confirm his diagnosis by performing culdocentesis. In performing this procedure, what anatomical landmark is deemed most helpful to access the Rectouterine pouch?
A. Lateral Fornix (Left)
B. Lateral fornix (Right)
C. Anterior fornix
D. Posterior fornix
A. The Round ligament of the uterus is attached antero-inferiorly to the utero-tubal junction and to the labia majora via the inguinal canal.
Which of the following statements will correctly describe the Round ligament of the Uterus?
A. The Round ligament of the uterus is attached antero-inferiorly to the utero-tubal junction and to the labia majora via the inguinal canal.
B. The Round ligament of the uterus is a single layer of peritoneum extending at the sides of the uterus.
C. The Round ligament of the Uterus is a continuation of the Mesosalpinx.
D. From the Uterus the Round ligament will pass through the inguinal canal to reach the Labia minora.
C. Myometrium
Identify which of the following layers of the uterus will primarily contract upon hormonal stimulation to expel the baby & placenta?
A. Uterine cervix
B. Perimetrium
C. Myometrium
D. Endometrium
D. The Uterine artery will pass superiorly to the ureter before reaching the uterus.
Which of the following statements will correctly describe the relationship of the uterine artery to its surrounding structures?
A. The Uterine artery will exit in the greater sciatic foramen and will re-enter the pelvic cavity via the lesser sciatic foramen to supply the uterus.
B. The Uterine artery will pass inferiorly to the ureter before reaching the uterus.
C. The Uterine artery will travel and enter the inguinal canal passing superior to the ureter before reaching the uterus.
D. The Uterine artery will pass superiorly to the ureter before reaching the uterus.
A. Ampulla
Which of the following parts of the Uterine tube is considered to be the widest & longest?
A. Ampulla
B. Infundibulum
C. Uterine part
D. Isthmus
B. Uterine artery
The Upper part of the vagina is supplied by what artery?
A. Vaginal artery
B. Uterine artery
C. Internal pudendal
D. External iliac
A. Week 33
Earliest period from time after fertilization for the descending testes to hit and reach the “scrotal floor”: (in weeks)
A. Week 33
B. Week 12
C. Week 8
D. Week 28
B. Hilum of the Indifferent Gonad (hilum of primordial testis or primordial ovary)
Estimated location of the “Primordial Germ Cells” (the maturing sperm or egg cells) during 5th week after fertilization:
A. Migrating via amoeboid movement from Yolk Sac-Allantois-Cloaca to Hindgut
B. Hilum of the Indifferent Gonad (hilum of primordial testis or primordial ovary)
C. Distal part of the Yolk Sac near the Allantois
D. Penetrated the Medulla of the Indifferent Gonad (primordial testis or primordial ovary)
B. Seminiferous Tubules and Rete Testis
The “Wolffian Ducts” will transform into the following, EXCEPT for:
A. Epididymis and Paradidymis
B. Seminiferous Tubules and Rete Testis
C. Vas Deferens and Ductuli efferentes
D. Seminal Vesicle and Ejaculatory Duct
B. SRY
Master gene for “testis” formation:
A. TAFii105
B. SRY
C. FGF-9
D. SOX-9
E. WNT-4
E. WNT-4
Master gene for “ovary” formation:
A. SOX-9
B. TAFii105
C. DAX-1
D. SRY
E. WNT-4
D. Genital Tubercle
What specific male “embryonic structure” is affected and probably has incurred insult during its entire course of development which has led to this congenital defect affecting the external genitalia (check the picture: COMPLETE DIPHALLIA or Male with Two Glans and Two Dorsal Penile Shafts):
A. Müllerian Duct
B. Wolffian Duct
C. Unaleria
D. Genital Tubercle
E. Genital Swelling

A. Sinovaginal Bulbs
What specific female “embryonic structures” is affected and probably has incurred insult during its entire course of development that have led to this congenital defect affecting the patient’s external genitalia (check the picture: a case of DISTAL BICOLPOS or DOUBLE HYMENAL OPENINGS WITH DOUBLE VAGINA OF THE LOWER 2/3rd’s):
A. Sinovaginal Bulbs
B. Unaleria
C. Wolffian Ducts
D. Müllerian Ducts

B. Müllerian ducts
CASE: A 24-year-old married female visited an OB-GYN Clinic with a chief complaint of no history of menstrual onset since adolescences. Additionally, during history-taking, the patient and husband of the patient complained of a short blind-ended vaginal vault of the index patient during trials of sexual intercourse. After a series of imagings and laboratory workups, patient was diagnosed with “Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome” or a congenital case of a biologically female patient without internal genitalia (Meaning: NO Fallopian Tubes; NO Uterus; NO Cervix of the uterus; with Absence of Upper 3rd of the Vagina leading to a shorter vaginal canal externally). (Check picture below: Presence of 2 functional ovaries held by a common ligament of the ovary proper with complete absence of intervening female internal genitalia.
This MRKH syndromic disorder is due to congenital absences of these embryonic structures in a female’s body:
A. Wolffian ducts
B. Müllerian ducts
C. Indifferent Gonads
D. Cloacal folds

A. Cloacal Folds
CASE: (Check the picture) This is a case of “Penoscrotal (Penis + Scrotum) Transposition” or a complete congenital positional exchange between Scrotum and Penile Shaft. This is due to an insult to which embryonic structure?
A. Cloacal Folds
B. Wolffian Duct
C. Indifferent Gonad
D. Müllerian Duct
