kidneys 1
1/132
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
As early as the _______ of embryonic development, the kidneys begin to form from the columns of mesoderm (intermediate
mesoderm).
second week
third week
fourth week
first week
third week
What describes the following?:
is the earliest nephric stage in humans, and constitutes the mature kidney in most primitive vertebrates.
Consists of 6-10 pairs of tubules.
Tubules then turn into cloaca
The pronephros disappears completely by the 4th week of human embryonic life.
Pronephros
What develops by the formation of mesonephric tubules from the intermediate mesoderm, it is the principal excretory organ during early embryonic life (4—8 weeks)?
Mesonephros
In males, what develops into the rete testis, the ejaculatory ducts, the epididymis, the ductus deferens, and the seminal vesicles?
the Wolffian duct
What is one of the paired embryogenic tubules that drain the primitive kidney (mesonephros) to the claoaca?
The Wolffian duct also known as the mesonephric duct
What arises caudal to the mesonephros at five weeks of development; it is the permanent and functional kidney in higher vertebrates; It is derived from the intermediate mesoderm?
Metanephros
What is the functional units of the kidney, arise from the intermediate mesoderm around each ureteric bud?
the nephrons
When does nephron function begin?
Nephron function begins at approximately 8 weeks.
With fetal growth, the kidneys appear to migrate from their pelvic location to the abdomen. This so-called migration is not complete until when?
5 or 6 years of life
the kidneys in infants and young children are located…
more caudal (inferior)
Kidneys are a bean shaped ______, and endocrine organs
intraperitoneal
retroperitoneal
neither
retroperitoneal
true/false: The upper poles of the kidneys are usually located at the level of the T12 vertebra and the lower poles extend to the level of the L4 vertebra.
true
What is a triangular muscle that lines both sides of the spine from hips to mid back, seen posterior medial to kidney?
Psoas muscle
What is a flat muscle posterior lateral to the psoas and immediately
posterior to the kidney?
Quadratus Lumborum muscle
What is the hilum?
located medially where the renal artery, vein, and nerves enter and leave the concave surface through a notch called the hilum
True/False: Average Adult length 9-12 cm, width 4-6 cm and AP 3-4 cm
true
What is most anterior at the hilum?
renal vein
renal pelvis/ureter
renal artery
renal pyramids
renal vein
What is most posterior at the hilum?
renal vein
renal pelvis/ureter
renal artery
renal pyramids
renal pelvis/ureter
What is between the two structures at the hilum?
renal vein
renal pelvis/ureter
renal artery
renal pyramids
renal artery
What provides support and protection from trauma and infection?
Supportive layers of Kidney
it’s a true capsule which surrounds the kidney and gives kidney a smooth appearance
fibrous renal capsule
Glisson’s capsule
adipose capsule
renal fascia/ Gerota’s fascia
fibrous renal capsule
Also referred to as perirenal fat. It envelopes both the kidney and adrenal glands.
fibrous renal capsule
Glisson’s capsule
adipose capsule
renal fascia/ Gerota’s fascia
adipose capsule
It encompasses the kidneys, adrenals, and perirenal fat. This is also
referred to as perirenal space.
fibrous renal capsule
Glisson’s capsule
adipose capsule
renal fascia/ Gerota’s fascia
renal fascia/ Gerota’s fascia
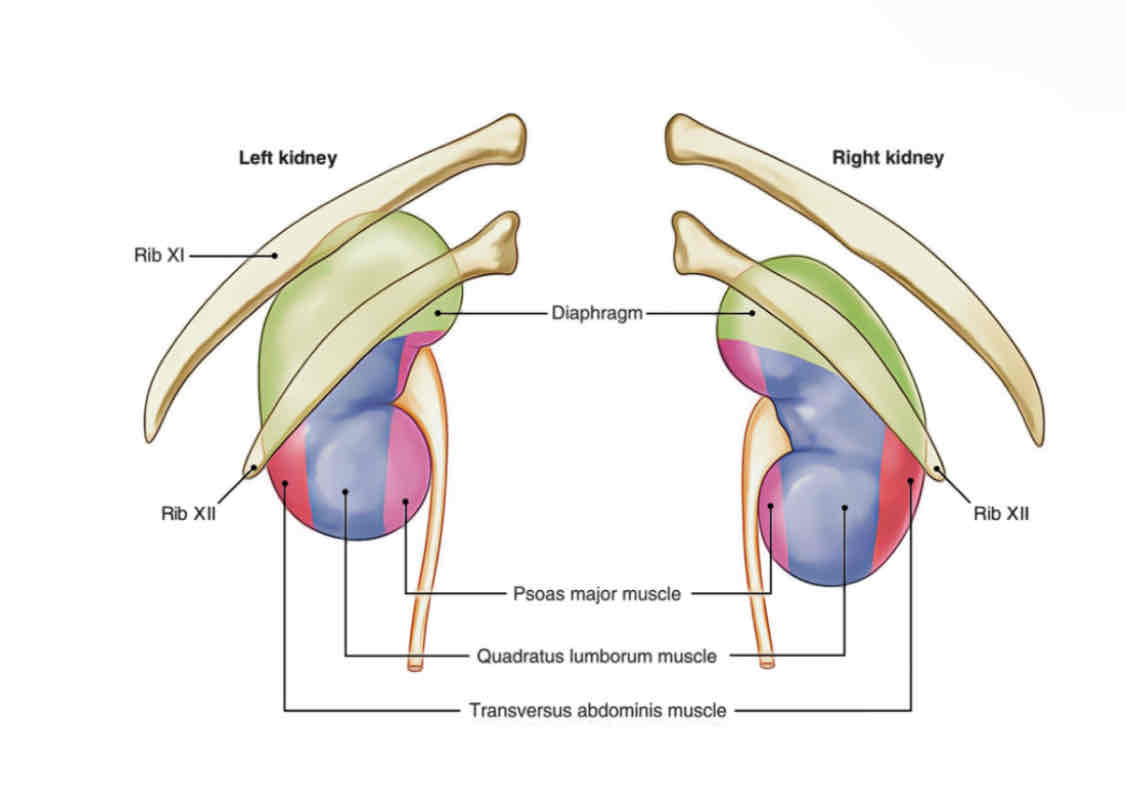
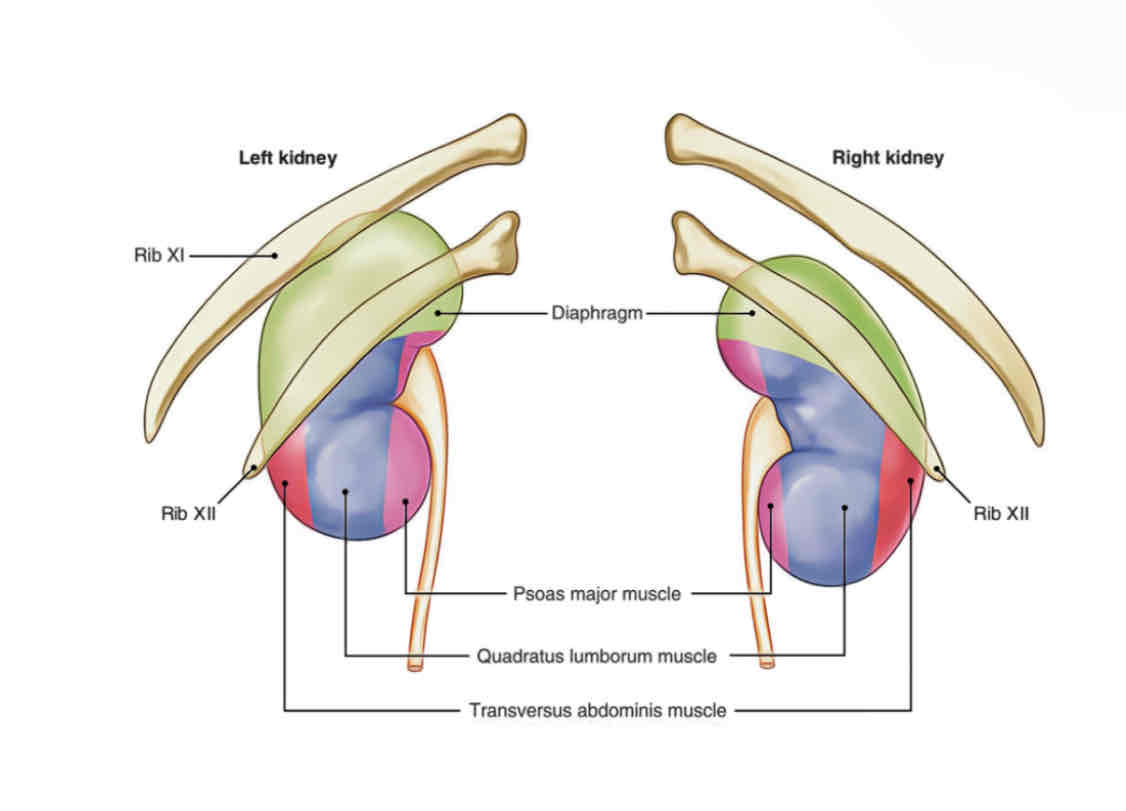
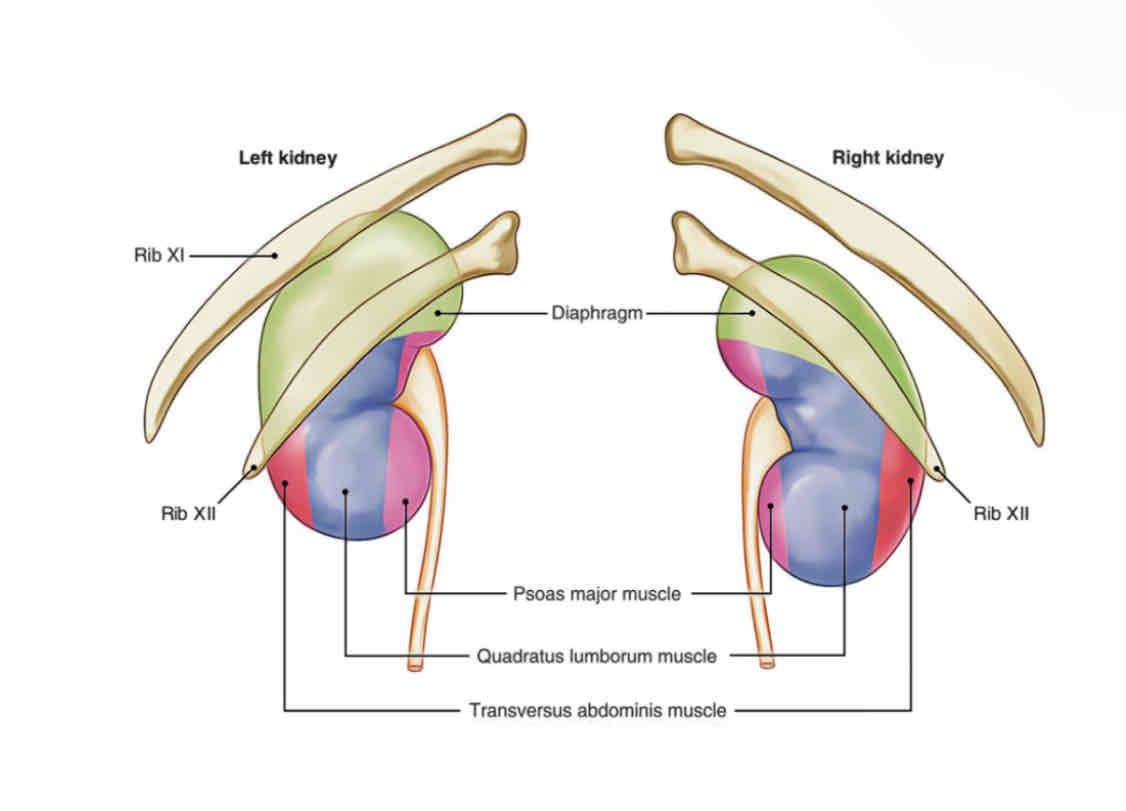
What are the three supportive muscles of the kidneys?
Psoas muscle
Quadratus lumborum muscle
Transversus abdominus muscle
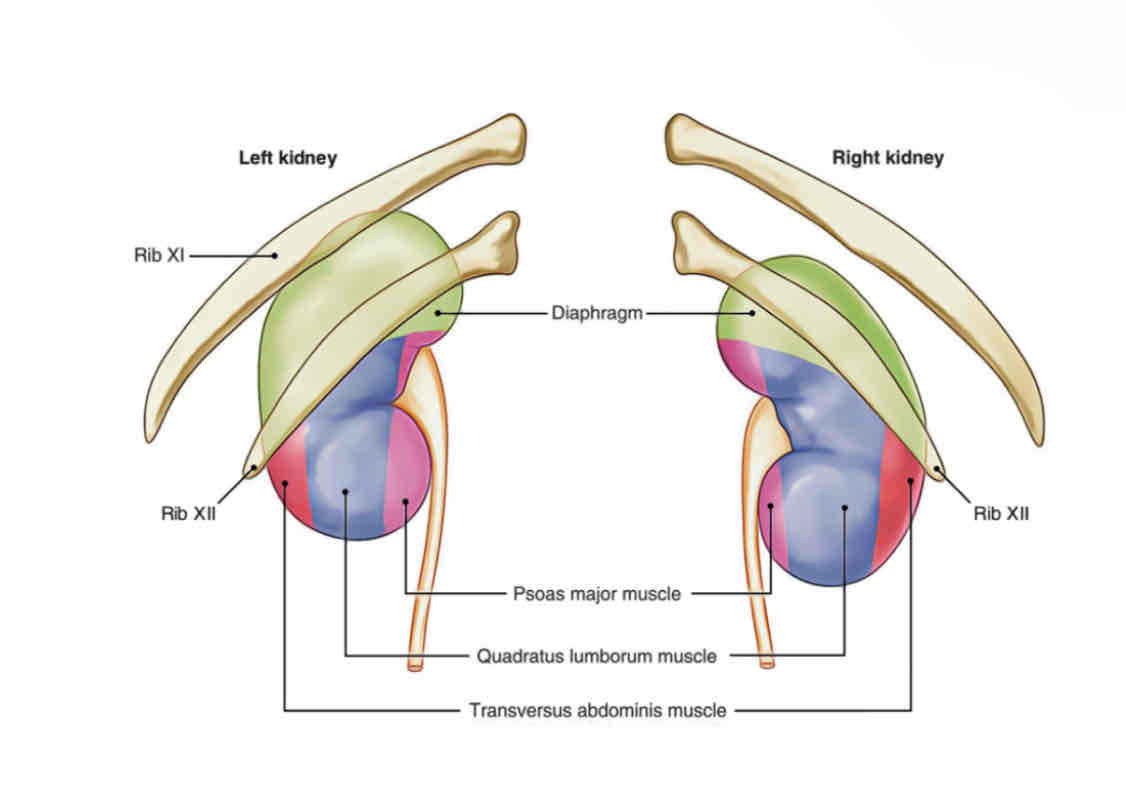
Which muscle does the following describe?
– Major groin muscle
– Primary flexor of the hip joint
– Lies posterior to the inferior pole of each kidney
Psoas muscle
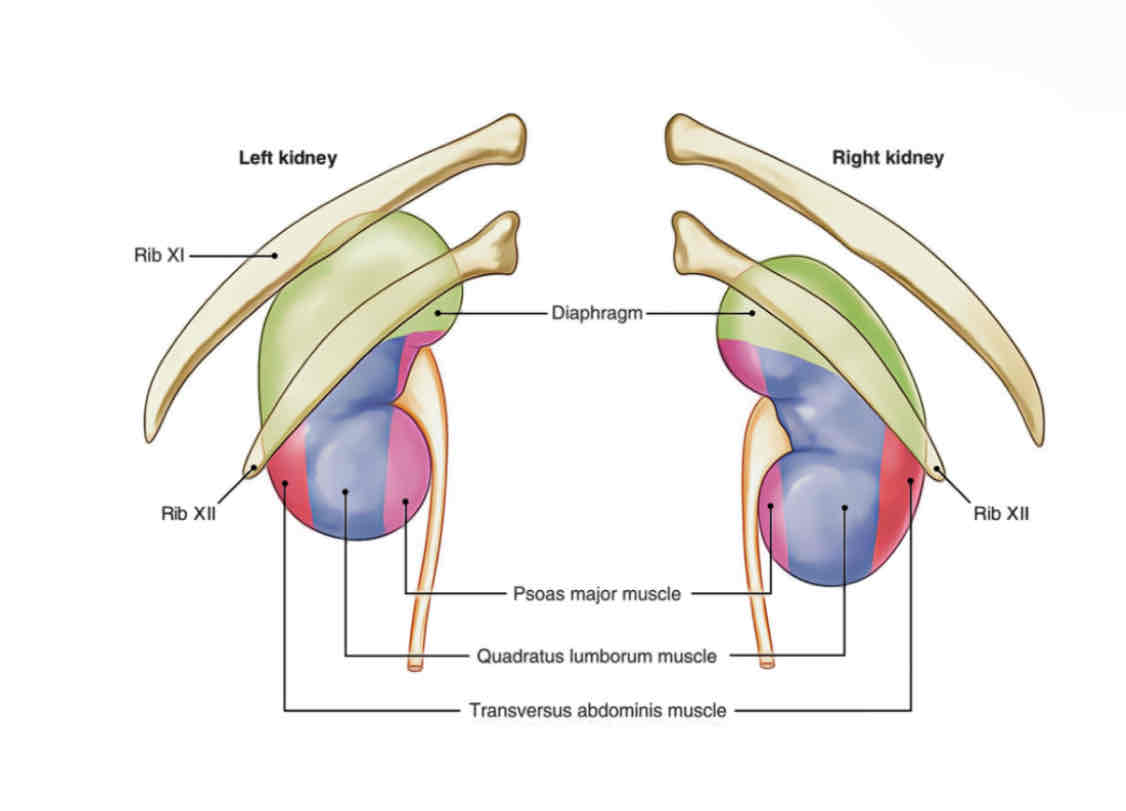
Which muscle does the following describe?
– Muscle of the posterior abdominal wall
– Lies posterior and medial to each kidney
Quadratus lumborum muscle
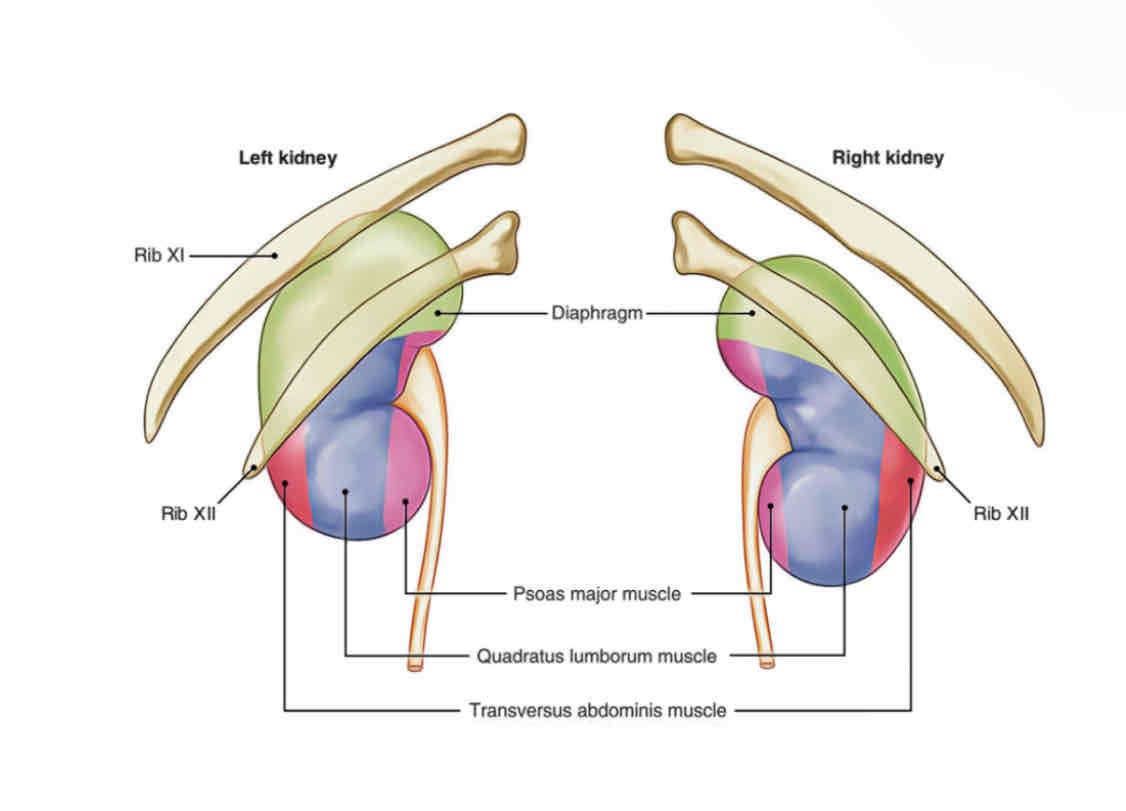
Which muscle does the following describe?
– Deepest layer of flat muscles of the anterolateral wall
– Lies lateral to each kidney
Transversus abdominus muscle
The kidney is composed of two types of tissue:
renal parenchyma and renal sinus
What is the point at which the distal convoluted tubule comes in contact with the afferent arterioles and secretes rennin?
Juxtaglomerular Apparatus
what is an enzyme important for regulating sodium and water retention; regulates blood pressure?
rennin
What is the capsule that surrounds the kidney?
true capsule/renal capsule
What is the sonographic appearance of the cortex?
Cortex is isoechoic or hypoechoic to liver
what extends from the capsule to the base of the pyramids and performs blood filtration?
the cortex
What consists of the cortex and the medulla?
renal parenchyma
What contains the renal corpuscles and the proximal and distal convoluted tubules of the nephron?
the cortex
The medulla contains ___________ renal pyramids. Pyramids are anechoic.
8 to 18
What are triangular structures with the wide portion (base) facing the renal cortex and the narrow tip (apex) converging toward the renal sinus?
Pyramids
What contains the loop of Henle and collecting duct?
Medulla
What separates the medulla from the cortex?
Arcuate arteries
Where does reabsorption occur?
Medulla
What is the inner hyperechoic portion of the kidney?
Renal sinus
What is the collecting system of the kidney and is the central portion of
the kidney, and it contains the collecting system (major and minor calyces), arteries and veins, lymphatics, fat, fibrous tissues, and part of the renal pelvis.
Renal sinus
What drains each of the medullary pyramids?
Minor calyces
True/False: There are 2-3 major calyces and each connects to several minor calyces
true
What combines to form the renal pelvis?
Major calyces
What is the upper expanded portion of the ureter located at the
hilum, posterior to blood vessels?
Renal pelvis
What is funnel-shaped transition from the major calyces to the ureter?
Renal pelvis
What is the functional unit of Kidney consisting of the renal corpuscle, proximal convoluted tubule, descending and ascending limbs of Henle’s loop, distal convoluted tubule and collecting tubules?
Nephron
What consists of glomerulus and glomerular capsule (Bowman’s capsule)?
Renal corpuscle(Malpighian body)
What surrounds the glomerulus?
Bowman’s Capsule
What consist of a the cluster of capillaries?
Glomerulus
What has an ascending and descending limb, these loops along with
their blood vessels and collecting tubes for the pyramids in the medulla?
Loop of Henle
What is farthest from the glomerulus; helps regular potassium excretion?
Distal Convoluted Tubule
What collects the filtrate?
collecting duct
What originates from the lateral aorta and is Immediately inferior to
the superior mesenteric artery (SMA)?
Main renal artery(s)
True/False: It is uncommon for individuals to have more than one renal artery arising from the aorta. Variants include more than one unilaterally or bilaterally.
false, because It is common for individuals to have more than one renal artery arising from the aorta. Variants include more than one unilaterally or bilaterally.
What enters the kidney hilum anterior to the ureter and posterior to
the renal vein?
renal artery
What is longer as it needs to pass posterior to the IVC?
right renal artery
After entering the renal hilum, the renal artery divides into five ___________ within the renal pelvis
segmental arteries
The segmental arteries branch into the __________ that course along side of the renal pyramids
interlobar arteries
The interlobar arteries arch over the base of the pyramids to form the
_____________
arcuate arteries
Branching from the arcuate arteries are the __________. These will give rise to the afferent arterioles to enter the renal glomeruli which is a component of the nephron
interlobular arteries
What is the correct order of the arteries?
• Renal artery to
• Segmental artery to
• Interlobar to
• Arcuate artery to
• Interlobular artery to
• Afferent arterioles to
• Glomerulus to
• Efferent arterioles
After passing through the glomerulus, blood exits through the
efferent arterioles to drain into the __________
interlobular veins
Paralleling the arcuate arteries, the ________ course along the base of the medullary pyramids
arcuate veins
Converging of the arcuate veins, the __________ are formed and run in between the medullar-y pyramids
interlobar veins
What is formed by the convergence of the interlobar veins, these veins will converge to form the main renal vein?
Segmental veins
What does this describe?: The renal vein exits the kidney hilum anterior to the renal artery and ureter. The left renal vein is longer passing between the abdominal aorta and the SMA on its way to confluence with the IVC.
Main renal vein
What supplies the kidneys, adrenals, and ureters?
Renal artery
What courses posterior to the IVC and anterior to the right psoas
muscle?
Right renal artery
What courses anterior to the left psoas muscle?
Left renal artery
Both renal arteries course posterior to the _______
renal veins
Renal Arteries have normal…..
Low resistance flow with low resistive index (RI)
What does increased RI >0.7 indicate?
renal dysfunction and ischemia
What an cause increased resistance in the parenchyma?
Renal dysfunction, renal arterial stenosis, renal vein thrombosis
What drains the kidneys, ureters, and adrenals?
renal veins
What courses anterior to the RRA to enter the IVC?
RRV
What originates at the renal hilum anterior to the LRA and courses between the aorta and superior mesenteric artery (SMA), then anterior to the proximal RRA to reach the IVC?
LRV
What can cause the kidney to enlarge and renal function to decrease?
Thrombosis of the renal vein
What are the functions of the kidneys?
• Kidneys remove wastes from blood and produce about 150ml of urine a day; 95% water, 5% waste
• It helps to regulate fluid levels, pH and electrolytes
• The kidneys maintain blood homeostasis. It helps to control blood concentration and volume by removing selected amounts of water and solutes
What describes the following?
– Secreted by the posterior pituitary, increases the water permeability of the collecting tubule segments (facultative reabsorption)
– Responsible for maintaining the body’s fluid balance,
– ADH secretion increases in the event of increased water loss (sweating or diarrhea) or reduced blood volume or blood pressure (hemorrhage).
Antidiuretic hormone (ADH)
What is secreted by the adrenal cortex, increases the rate of tubular resorption of sodium and produces a concurrent loss of potassium?
Aldosterone
What is secreted by the JGA, increases in response to decreased blood pressure in the afferent arteriole secondary to sodium depletion or to a change from the supine to the upright position?
Renin
What acts as a catalyst on certain plasma proteins to produce angiotensin I, which is converted to angiotensin II by proteolytic enzymes?
Renin
What increases systemic blood pressure by acting as a potent vasoconstrictor?
Angiotensin II
What is it called when fluid is forced across a membrane into the nephron; increases with increased blood pressure; decreased with kidney disease
Glomerular Filtration
Tubular Resorption
Tubular Secretion
Glomerular Filtration
What is it called: while the fluid is within the renal tubules, it can be resorbed according to the body's needs; electrolytes and components of the fluid are selectively resorbed to allow for excretion of intended waste products
Glomerular Filtration
Tubular Resorption
Tubular Secretion
Tubular Resorption
What is the name of the selective process of disposing of the waste products and pH regulation
Glomerular Filtration
Tubular Resorption
Tubular Secretion
Tubular Secretion
What is the order of urine formation?
Glomerular Filtration
Tubular Resorption
Tubular Secretion
What increases with renal failure?
Uric Acid
White Blood Cell Count
Aldosterone
Lactate Dehydrogenase
Uric Acid
What is increased with infection and decreased with chemotherapy or radiation therapy?
Uric Acid
White Blood Cell Count
Aldosterone
Lactate Dehydrogenase
White Blood Cell Count
What increases with decreased urinary output?
Uric Acid
White Blood Cell Count
Aldosterone
Lactate Dehydrogenase
Aldosterone
What increases with chronic renal disease and renal infarction?
Uric Acid
White Blood Cell Count
Aldosterone
Lactate Dehydrogenase
Lactate Dehydrogenase
What is more specific in determining renal dysfunction?
creatinine
blood urea nitrogen (BUN)
hematuria
proteinuria
creatinine
What describes the following?:
– Normal 0.6 to 1.2 mg/dL.
– A waste product produced from meat protein and normal wear and tear on the muscles in the body.
– More specific in determining renal dysfunction than BUN levels.
– Elevated in renal failure, chronic nephritis or urinary obstruction.
– Decreases in debilitation, muscle weakness or dystrophy, starvation, hyperthyroidism
creatinine
What describes the following?:
– Normal 11 to 23 mg/dL.
– Produced from the breakdown of food proteins.
– Elevated in urinary obstruction, renal dysfunction, or dehydration.
– Decreased levels associated with over hydration, pregnancy, liver failure, decrease in protein intake, and smoking.
blood urea nitrogen (BUN)
What describes the following?:
– Visible or microscopic red blood cells in the urine.
– Associated with early renal disease.
hematuria
What describes the following?:
– Abnormal amount of proteins in the urine.
– Associated with nephritis, nephrolithiasis, carcinoma, polycystic disease, hypertension, and diabetes mellitus.
– Increases risk of developing progressive renal dysfunction.
proteinuria
What is the adult kidney size?
9 to 12-cm long, 4 to 6-cm wide, and 3 to 4-cm thick
What is paired bean-shaped structures lying in a sagittal oblique plane in the retroperitoneal cavity?
kidneys