(14) Organ Transplants
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
71 Terms
Which organ has the most successful transplant rate?
cornea
Why do corneal transplants have the most successful transplant rate?
eye is immunologically privileged area and cornea isn't vascularized
refers to donor tissue
graft
refers to the recipient in a transplant
host
refers to transplants in which grafts are exchanged between members of the same species
allogenic
refers to transplants in which grafts are exchanged between members of different species
Example: using a pig valve in a heart transplant
xenogenic
How often are allogenic grafts rejected?
always
(looks like foreign tissue, except the cornea)
How often are xenogenic grafts rejected?
always
(looks like foreign tissue to the body's immune system)
What is required for allogenic and xenogenic grafts to work?
immunosuppressants
refers to a transplant in which a graft from one body part is moved to another body part on the same person
Example: skin graft
autograft
refers to a transplant in which a graft is exchanged between monozygotic twins
isograft
(works because they have the same MHC genes)
True or false: Autografts and isografts can succeed without immunosuppression.
true
If you donated a kidney to one of your classmates, what type of transplant would that be?
A. xenograft
B. isograft
C. autograft
D. allograft
D
What are the main antigens involved in graft rejection?
MHC
How many different MHC class I genes do we express?
6
(A, B, or C, one of each from each biological parent)
What are the different MHC class I genes?
A, B, C
What is the most immunogenic MHC antigen in class I?
A, B
(C is least polymorphic - less of it around, so easier to match up)
How many different MHC class II genes do we usually express?
12
(DR, DQ, and DP with 2 alpha and 2 beta forms of each; also, one of each from each biological parent)
What are the different MHC class II genes?
DR, DQ, DP
(2 alpha and 2 beta forms of each)
What is the most immunogenic MHC antigen in class II?
DR, DQ
(DP is least polymorphic - less of it around, so easier to match up)
Recognition of the MHC antigens on another individual's cells invokes one of the strongest immune responses. Why?
MHC looks very different from host cells
What specifically evokes the strong immune reaction in a transplant immune response?
donor MHC alone
(mimics a self MHC-foreign peptide complex to the host, which the host recognizes)
What is included in the binding pocket of the graft (donor) cells' MHC?
graft peptide
(which can be bound by the host's TCR)
Host vs. graft: If a graft carries only antigens that are not at all present in the host, what is the outcome?
transplant is rejected
Host vs. graft: If a graft carries only antigens that are present in the host, what is the outcome?
transplant is accepted
Host vs. graft: If a graft carries antigens that are partially present in a hybrid host (i.e. parent to child transplant), what is the outcome?
transplant is accepted
(since graft carries MHC that the child has already inherited)
Host vs. graft: If a hybrid graft carries antigens that are partially present in the host (i.e. child to parent transplant), what is the outcome?
transplant is rejected
(since graft carries MHC from both parents, one of which looks foreign to the parent being donated to)
Which is a usually better donor to the other: parents or children?
parents
(parents are better donors for children than children for parents)
What is an example of a situation in which we have a graft vs. host reaction?
bone marrow transplant
Why would graft cells attack host tissue? (what cells do the attacking and why)
graft T cells are transplanted into immunosuppressed recipients that can't reject them, so they attack the recipient
In a graft vs. host reaction, why would immunologically competent T cells in the graft tissue attack the recipient?
recipient is immunosuppressed and can't reject T cells
What cells in the host recognize graft tissue?
T cells
What cells in the graft cause the host to recognize graft tissue?
APCs
Do graft APCs have a high or low density of graft MHC molecules?
high
Do individual graft MHC molecules react weakly or strongly with the host TCR?
weakly
Individual graft MHC molecules react weakly with the host TCR. So then how can we get a full blown immune response from a graft?
cluster of graft MHCs
(generates a strong enough signal for T cell activation)
Graft MHC molecules present the graft's ____ ____, letting the MHC serve as a graft cell's "ID badge". So in the tissue that it came from, that's recognized as normal. In the host tissue that it's being transplanted to, that isn't normal.
self peptides
True or false: Graft MHC molecules, in addition to presenting their own self-peptides, can also present processed antigens of host molecules.
true
How can a graft MHC molecule induce an immune response in the host with the host's own self-antigens?
processes and presents the peptides differently so that host doesn't recognize it anymore
True or false: Even if a graft MHC molecule processes and presents a host's own antigens in a bit different of a way, then the host will still be tolerant of this MHC/antigen combination.
false
How can a host APC induce an immune reaction in the host upon receiving graft tissue?
phagocytoses graft molecules to present with host's own MHC molecules
refers to activation of an immune response from a transplant in which the APCs come from the donor
direct
refers to activation of an immune response from a transplant in which the APCs come from the recipient
indirect
cells from donor (graft) tissue that cause direct activation of recipient (host) T cells
Example: donor APCs that present graft (donor) peptide to recipient T cells
passenger leukocytes
What kind of activation is exemplified by donor APCs presenting graft peptide to recipient T cells?
direct
What kind of activation is exemplified by recipient APCs presenting graft peptide (after acquiring it from graft tissue) to recipient T cells?
indirect
Does direct activation occur primarily with CD4+ T cells, CD8+ T cells, or both?
both
Does indirect activation occur primarily with CD4+ T cells, CD8+ T cells, or both?
CD4+
Which type of activation results in a more powerful and quicker transplant rejection: direct or indirect?
direct
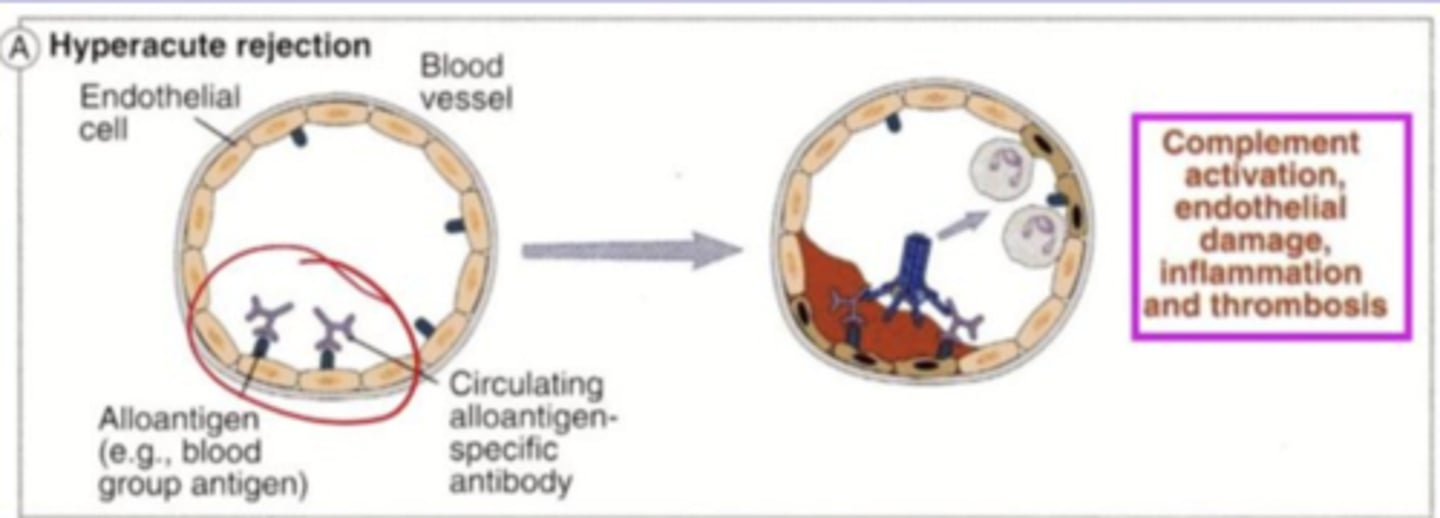
rejection that is rapid (minutes to hours) due to the recipient already having antibodies against graft antigens present on graft endothelial cells (immune system has already been primed)
hyperacute rejection
What are 3 factors that would make an individual more susceptible to a hyperacute rejection?
prior blood transfusions, multiple pregnancies, rejection of previous transplant
Hyperacute rejection occurs when the recipient already has antibodies against graft antigens present on graft endothelial cells. How do these antibodies initiate the immune response? What two effects does this have on graft tissue?
they activate complement, resulting in thrombosis and ischemic necrosis
What type of rejection often occurs with xenografts?
hyperacute
(since MALT has likely already been exposed to animal antigens from diet)
rejection that takes days to weeks and is the main cause of early graft rejection due to primary activation of T cells against alloantigens in the graft
acute rejection
What type of rejection is the main cause of early graft rejection?
acute
Acute rejection occurs due to primary activation of T cells against what in the graft?
alloantigens
(these are present in some members of the same species but not all)
Acute rejection occurs due to primary activation of mainly what kind of T cells against alloantigens in the graft?
CD8+
Does acute rejection mostly depend on direct or indirect activation?
direct
What possible parts of the graft do recipient CD8+ T cells act against?
general graft tissue itself or vessel endothelial cells
Acute rejection mostly involves cytotoxic T cells, but what else may contribute to vascular damage?
antibodies
rejection that takes months to years to occur and is often due to a genetic disparity between the donor and recipient or immunosuppressive treatment wearing off
chronic rejection
What 2 main factors contribute to chronic rejection?
genetic disparity, immunosuppressive treatment
Does chronic rejection mostly depend on direct or indirect activation?
indirect
What is the cardinal feature of chronic rejection?
thickening of blood vessel walls in graft tissue
(due to smooth muscle cell proliferation and eventual constriction)
Chronic rejection occurs due to activation of mainly what kind of T cells reacting against alloantigens in the graft?
CD4+
How do CD4+ T cells cause the thickening of blood vessels and scar formation in chronic rejection?
release cytokines to stimulate fibroblasts and smooth muscle cell proliferation
(may lure macrophages to the area to trigger the fibroblasts)
What is a notable histologic consequence of chronic rejection?
interstitial fibrosis
(scar formation)
In which type of low-grade rejection do we see smooth muscle cell proliferation, causing walls of blood vessels in the graft to thicken and eventually occlude?
chronic rejection
What type of transplant rejection is primarily triggered by antibodies?
A. chronic
B. hyperacute
C. acute
B
Good organ survival occurs when which class of MHC molecules are matched as closely as possible?
MHC class II
Which type of rejection would occur due to pre-existing antibodies to the grafted tissue?
A. hyperacute
B. chronic
C. acute
A