Respiratory system (copy)
1/59
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
How does the trachea divide?
Trachea first divides into 2 bronchi
Left bronchi splits into 2 bronchi
Right bronchi splits into 3 bronchi
Bronchi eventually split into bronchioles
Bronchioles split into alveolar ducts
Where are cilia located? What is their function? What other cells accompany them?
Trachea, bronchi, and bronchioles are equipped with cilia
Sweep up and down to move dust/debris to the larynx, then pharynx (where we swallow)
Amongst cilia are goblet cells (cube-like cells) that produce mucus
Why do organisms require gas exchange?
Most organisms are aerobic and require oxygen
Organisms need to remove metabolic waste products such as carbon dioxide
What are 2 challenges for gas exchange for large multicellular organisms?
Metabolically active tissues may lie deep within the organism and far away from their environment
Surface-area-to-volume ratio decreases with increasing size
What are the 4 characteristics of gas exchange surfaces?
Thin: often only one cell layer, to keep diffusion distances short
Moist: to encourage gas diffusion, and because gases diffuse through membranes only in dissolved form
Large surface area (half a billion alveoli exist)
Permeable to respiratory gases (oxygen and carbon dioxide)
What is an adaptation of the amphibian axolotl?
Amphibian has six external gills for respiratory gas exchange with water
What is the concentration gradient of respiratory gases for fish?
Low concentration of oxygen, and high concentration of carbon dioxide for blood in gill capillaries
What is the concentration gradient of respiratory gases for animals?
Concentration of oxygen in the lung capillaries is lower than that of air inspired into the lungs
Concentration of carbon dioxide in the lung capillaries is higher than that in the air inspired
What two events must occur to keep concentration gradients in place?
Water must be continuously passed over the gills OR air must be continuously refreshed in the lungs
There must be a continuous blood flow to the dense network of blood vessels in both the body tissues and the tissues of the gills or lungs
How do alveoli act as an adaptation?
Lungs subdivide their volume into microspheres called alveoli
Allows air to be exposed to a large surface area of gas exchange tissue
Where is the location of the alveoli?
At terminal ends of the branches of tubes that started as tthe trachea
How do alveoli act when we expire vs inspire?
Inflate when we breathe in, deflate when we breathe out
What are the blue vs red capillaries surrounding the alveoli?
Blue - arteriole capillaries
Red - venous capillaries
What is on the inner surface of each alveolus?
Lined by a thin phospholipid and protein film called a surfactant
Specific alveolar cells secrete the surfactant, which coats the inside of each alveolus
What does the surfactant do?
Acts to reduce the surface tension of the moist inner surface and helps prevent each alveolus from collapsing each time air is expired
What structural feature facilitates the diffusion of respiratory gases?
The spherical shape of the alveoli provides a vast surface area
Each alveolus has close access to a capillary
Because capillaries are just one cell thick and each alveolus is just one cell thick, the respiratory gases only need to diffuse through two cells to enter or exit the bloodstream
What is the concentration gradient of capillaries vs alveoli?
Air inspired into the alveoli has a high concentration of oxygen and lower concentration of carbon dioxide compared to the blood in a nearby capillary
Gases diffuse according to the concentration gradient
What are pneumocytes?
Cells that make up the alveoli
What are type I pneumocytes?
Thin, flat cells that cover about 95% of the alveolar surface
Involved in the exchange of gases between the alveoli and capillaries
What are type II pneumocytes?
Cube-shaped cells covering about 5% of the alveolar surface
Secretes pulmonary surfactant
Can also differentiate into type I pneumocytes to help repair alveolar lining if it’s damaged
Since breathing is unconscious, what makes up our lungs?
Tissue that makes up our lungs is passive and not muscular, therefore the lungs are incapable of purposeful movement
What are the muscles surrounding the lungs?
Diaphragm, muscles of the abdomen, and the external and internal intercostal muscles (surrounding your ribs)
Work to either increase or decrease the volume of the thoracic cavity, leading to pressure changes in the lungs
What is Boyle’s law?
An increase in volume will lead to a decrease in pressure, and vice versa
What is the thoracic cavity?
Houses the lungs and is closed to the outside air
Lungs only have one opening — through the trachea
What is the diaphragm and what is its function?
A large, dome-shaped muscle that forms the “floor” of the thoracic cavity
When it contracts, it flattens the dome shape and increases the volume of the thoracic cavity
Steps for inspiration (breathing in)
1. The diaphragm contracts, increasing the volume of the thoracic cavity
2. The external intercostal muscles and one set of abdominal muscles both contract to help raise the rib cage. These actions help increase the volume of the thoracic cavity
3. Because the thoracic cavity has increased in volume, the pressure inside the thoracic cavity decreases. Less pressure on the passive lung tissue
4. The lung tissue responds to the low pressure by increasing its volume
5. Leads to a decrease in the pressure inside the lungs, known as a partial vacuum. Air comes through the open mouth or nasal passages to counter the partial vacuum, filling the alveoli
What happens to the muscles when you exercise?
Abdominal muscles and intercostal muscles must achieve a greater initial thoracic volume
Leads to deeper breathing and more air moving into the lungs
What happens during expiration (breathing out)?
Relaxation of diaphragm
Contraction of the internal intercostal muscles results in an increased pressure on the lung
What is a spirometer?
A device used to measure lung volume
Creates a graph for lung volume vs time
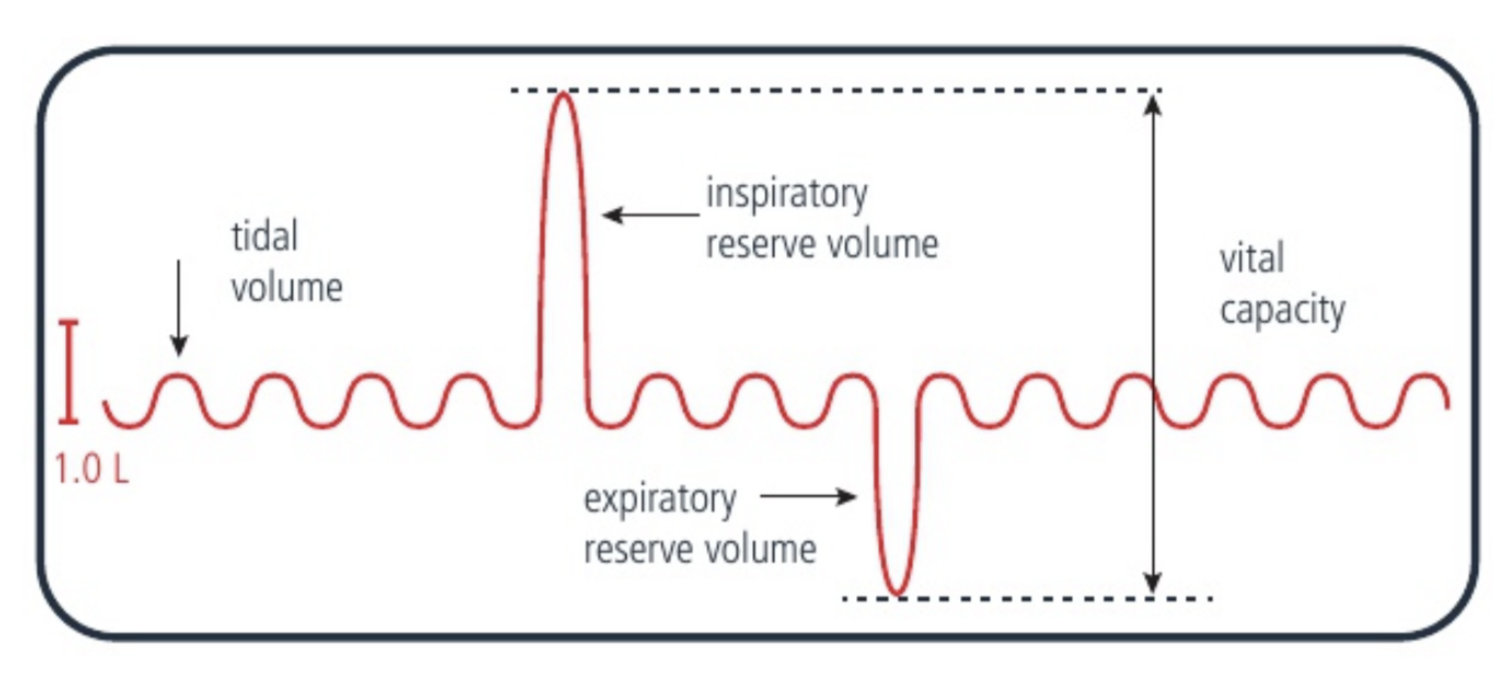
What is tidal volume?
The volume of air that is breathed in or out during a typical cycle when a person is at rest
Measured by the distance between a trough and peak
What is inspiratory reserve volume?
The maximum volume of air that a person can breathe in (measured from the peak of a normal tidal breath to the maximum point of the tidal volume)
What is the expiratory reserve volume?
The maximum volume of air that a person can breathe out (measured from the trough of a normal tidal breath to the minimum point of the tidal volume)
What is vital capacity?
Maximum amount of air a person can expel from the lungs after a maximum inhalation
The sum of the inspiratory reserve volume, the tidal volume, and the expiratory reserve volume
How does gas exchange work in amoeba?
Direct diffusion of oxygen and carbon dioxide between water and body of amoeba
How does respiration work for ticks and arachnids?
There are tracheal openings in exoskeleton
How does gas exchange work for birds?
Inhalation: air is breathed in, goes to air sacs
Exhalation: air from air sacs goes out
What is haemoglobin?
Protein molecule found within red blood cells (erythrocytes) that is responsible for carrying most of the oxygen within the bloodstream
What is the structure of an erythrocyte?
A plasma membrane surrounding cytoplasm filled with haemoglobin molecules
Have no nuclei and few organelles
What is the structure of a haemoglobin molecule?
Each haemoglobin molecule is composed of 4 polypeptides and has quarternary structure
Each polypeptide has a haem group near its centre, and each haem group has an iron atom within it
How does haemoglobin bind to oxygen?
Iron atom within the haem group binds with the oxygen
Because haemoglobin has a total of 4 iron atoms with 4 haem groups, it has the capacity to transport four oxygen molecules (in this form, it is saturated)
What is cooperative binding?
Oxygen molecules bind to identical areas within haemoglobin (iron atoms)
Any oxygen molecule bonded to haemoglobin increases its affinity for oxygen
Molecular shape of haemoglobin is influenced by it binding with oxygen molecules
What is the role of carbon monoxide in binding to haemoglobin?
Competitive to oxygen, binds to iron of haemoglobin
Affinity of haemoglobin to carbon monoxide is higher than oxygen (thus, oxygen won’t bind if carbon monoxide is present)
Erythrocyte transfusion is necessary to replace no longer functioning erythrocytes
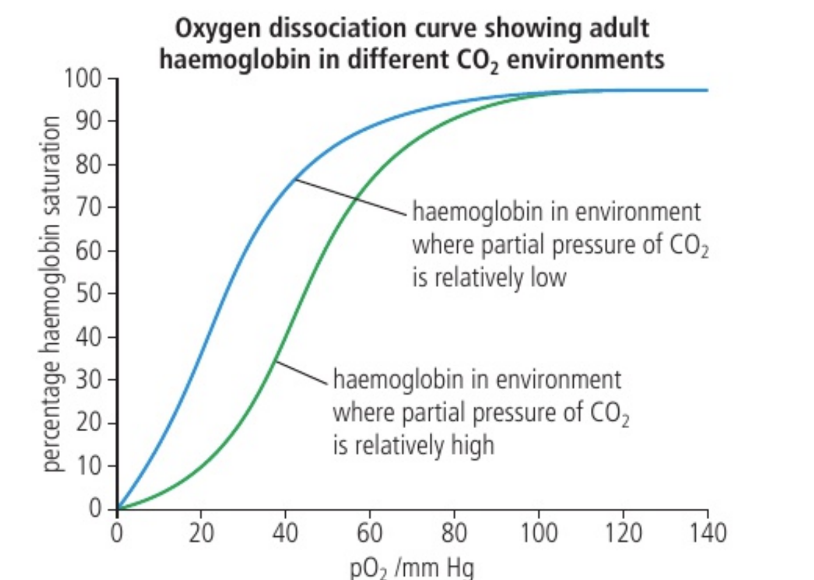
Which area of each polypeptide does carbon dioxide bind to?
The allosteric site of haemoglobin
The binding of carbon dioxide to haemoglobin results in an increase in the release of oxygen molecule and is known as the Bohr shift
This mechanism is known as allostery
What are two situations where the Bohr shift makes sense?
Binding to carbon dioxide is most likely to occur where carbon dioxide is at greater concentrations, in muscles and other body tissues, as a product of cell respiration (also, oxygen is needed here)
In lung tissue, the alveoli of the lungs has relatively low concentrations of carbon dioxide and high concentrations of oxygen. This permits haemoglobin to lose carbon dioxide, thereby giving the haemoglobin renewed affinity for bonding to oxygen
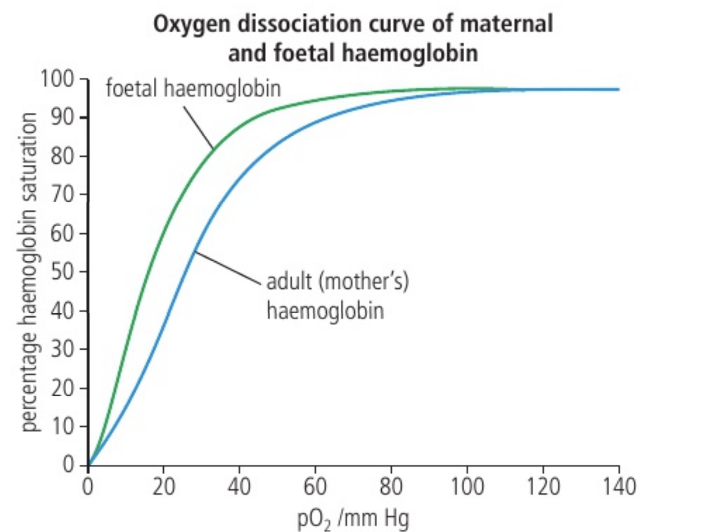
Why is there a structural difference between foetal haemoglobin and adult haemoglobin?
Enables the foetal haemoglobin to have a higher affinity for oxygen
Describe the placenta of a pregnant female.
Capillaries of the mother are very close to the foetal capillaries
Foetus is actively carrying out cell respiration. The foetal blood sent to the foetal side of the placenta is relatively low in oxygen and high in carbon dioxide
The concentration gradient, aided by the foetal haemoglobin’s greater affinity for oxygen, encourages diffusion of the mother’s oxygen to the foetus
What does the production of alveolar surfactant for a foetus signal?
That the foetus is ready to be delivered (theory that it initiates childbirth)
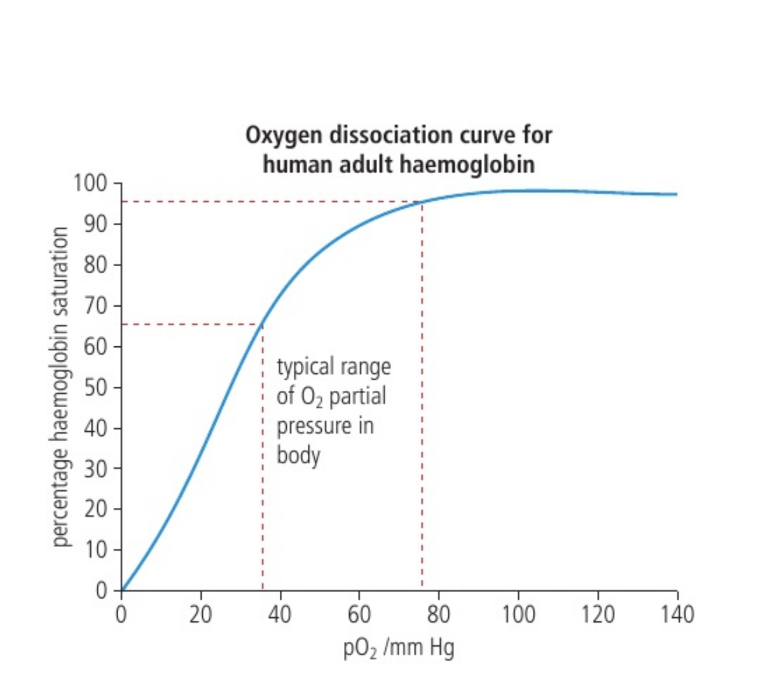
What is on the y-axis of an oxygen dissociation curve?
Percentage of haemoglobin that is transporting the maximum four oxygen molecules
What is on the x-axis of an oxygen dissociation curve?
Partial pressure of oxygen, which varies depending on where the blood is within the body
Why is the graph curved (“sigmoidal shaped”)?
Slope increases first — as haemoglobin is more saturated, its affinity for oxygen increases
Slope decreases at the end — haemoglobin’s affinity for oxygen decreases as it becomes more saturated with oxygen
Oxygen dissociation curve for foetal vs maternal haemoglobin.
At all meaningful levels of oxygen partial pressure, foetal haemoglobin is more highly saturated with oxygen
Oxygen dissociation curve displaying the Bohr shift.
Haemoglobin is more likely to release oxygen in an environment where the partial pressure of carbon dioxide is high
What is the range of normal blood pH?
7.35 - 7.45
What is myoglobin?
Monomer that has haem, which binds to oxygen
Has high affinity for oxygen, otherwise it would lose oxygen to haemoglobin
Located within muscles and acts as an oxygen reservoir
What are respiratory centres?
Group of cells that controls the ventilation of the lungs
Where are respiratory centres located? What happens at rest?
Located in the medulla
When at rest, spontaneous action potentials are released by these cells, which travel to your diaphragm and intercostal muscles to maintain breathing at a relatively slow and controlled pace
What receptors allow feedback control of the ventilation rate?
Chemoreceptors located in the medulla monitor the levels of carbon dioxide and pH in the blood passing through the medulla
What does body activity do to pH of blood?
When carbon dioxide enters a red blood cell, the following reaction, catalysed by carbonic anhydrase, occurs:
Carbon dioxide + water —> Carbonic acid
Carbonic acid dissociates into bicarbonate ion and hydrogen ion
Lowers pH of the blood
What do chemoreceptors do when blood is more acidic?
Chemoreceptors in the medulla sense this increase in hydrogen ions and send action potentials at a higher rate proportional to the number of hydrogen ions
All of the muscles, associated with lung ventilation, especially the diaphragm and intercostal muscles, respond
Rate of ventilation increases (and the volume of air moving in and out)
What happens when exercise decreases?
Hydrogen ion concentrations will also decrease and action potentials sent from the respiratory centres will decrease