klebsiella
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
67 Terms
Transverse Myelopathy
Combined painful radicular and transverse cord syndrome
Brown-séquard syndrome
Ventral cord syndrome
High cervical–foramen magnum syndrome
Central cord or syringomyelic syndrome
Syndrome of the conus medullaris
Syndrome of the cauda equina
What are the 8 main syndromes?
Transverse Myelopathy
a complete or almost complete sensorimotor myelopathy that involves most or all of the ascending and descending tracts
Combined painful radicular and transverse cord syndrome
Medically referred to as myeloradiculopathy.
It is most commonly caused by cervical or lumbar spinal stenosis (narrowing of the spinal canal, often due to age-related degenerative changes), a herniated disc, or an acute traumatic injury.
Brown-séquard syndrome
Hemicord syndrome
A neurological condition resulting from damage to only one side of the spinal cord, causing weakness and paralysis on the same side of the body as the injury, along with a loss of pain and temperature sensation on the opposite side
Ventral cord syndrome
sparing posterior column function
Also called anterior cord syndrome, it is an incomplete spinal cord injury caused by damage to the anterior two-thirds of the spinal cord, often from a stroke of the anterior spinal artery or a traumatic injury
High cervical–foramen magnum syndrome
A term for a group of symptoms resulting from compression or irritation of the brainstem, spinal cord, and nerves at the foramen magnum due to conditions like Chiari malformation, tumors, or bone abnormalities
Central cord or syringomyelia syndrome
a spinal cord injury with a primary symptom of greater weakness in the arms than the legs
condition where a fluid-filled cyst (syrinx) forms in the spinal cord and can cause symptoms similar to Central Cord Syndrome
Syndrome of the conus medullaris
a medical emergency resulting from compression or injury to the conus medullaris, the terminal part of the spinal cord. It is characterized by symptoms such as sudden back pain, saddle anesthesia (loss of sensation in the perineal area), and bladder and bowel dysfunction (incontinence or retention).
Syndrome of the cauda equina
a medical emergency caused by compression of the cauda equina nerve roots at the lower end of the spinal cord, leading to symptoms like severe lower back pain, leg weakness, and loss of bladder or bowel control
Spinal cord injury
Is one that causes myelopathy or damage to white matter or myelinated fiber tracts that carry signals to and from the brain. It also damages gray matter in the central part of the spine, causing segmental losses of interneurons and motorneurons.
Incidence of SCI
Highest among persons age 16-30, in whom 53.1 percent of injuries occur; more injuries occur in this age group than in all other age groups combined
Males represent 81.2 percent of all reported SCIs and 89.8 percent of all sports-related SCIs
Among both genders
auto accidents, falls and gunshots are the three leading causes of SCI, in that order.
Among males
diving accidents ranked fourth, followed by motorcycle accidents
Among females
Medical/surgical complications ranked fourth, followed by diving accidents
Auto accidents
Leading cause of SCI in the United States for people age 65 and younger
Falls
Leading cause of SCI for people 65 and older.
Sports and recreation-related SCI
Primarily affect people under age 29.
Trauma
automobile crashes, falls, gunshots, diving accidents, war injuries, etc.
Tumor
Meningiomas, ependymomas, astrocytomas, and metastatic cancer.
Ischemia
Resulting from occlusion of spinal blood vessels, including dissecting aortic aneurysms, emboli, arteriosclerosis.
Developmental disorders
Spina bifida, meningomyolcoele, and other.
Neurodegenerative diseases
Demyelinative diseases
Multiple Sclerosis
Transverse myelitis
From spinal cord stroke, inflammation, or other causes
Vascular malformations
Arteriovenous malformation (AVM),
Dural arteriovenous fistula (AVF)
Spinal hemangioma
Cavernous angioma
Aneurysm
Sequelae of SCI
Tissue disruption: Primary cell death, breaking of axons, etc.
Injured spinal cords show progressive tissue loss
Central hemorrhage necrosis develops over 2-3 hours,
White matter blood flow falls by 50% by 3 hours
Metabolism is compromised with high lactic acid levels
Neuronal apoptosis
Peaks at 48 hours after injury in the gray matter surrounding the injury site
Neuronal apoptosis & Oligodendroglial apoptosis
Two types of Apoptosis?
Oligodendroglial apoptosis
Peaks at 10-14 days after injury in degenerating white matter tracts
Stage of spinal shock
Stage of recovery
Stage of reflex failure
What are the 3 stages of SCI?
Stage of spinal shock
Sensation and motor power localized below the vertical height of the lesion are lost.
Stage lasts for 2 to 3 weeks in humans, and hours to days in lower animals due to a lesser degree of encephalitis
Stage of recovery
After a period typically ranging from 2 to 3 weeks of injury, the nerves partially recover, and the return of segmental reflexes produce paraplegia-in-flexion.
Stage of reflex failure
After a period of days the recovered reflexes again start to give way due to complete degeneration of nerve cells.
Spinal Cord Anatomy
About 18 inches long
Extending from the base of the brain to near the waist.
Many of the bundles of nerve fibers that make up the spinal cord itself contain upper motor neurons (UMNs).
Spinal nerves that branch off the spinal cord at regular intervals in the neck and back contain lower motor neurons (LMNs).
Cervical vertebrae (1-7), located in the neck
Thoracic vertebrae (1-12), in the upper back (attached to the ribcage)
Lumbar vertebrae (1-5), in the lower back
Sacral vertebrae (1-5), in the pelvis
What are the 4 sections of the spine?
The American Spinal Injury Association or ASIA
defined an international classification based on neurological levels, touch and pinprick sensations tested in each dermatome, and strength of ten key muscles on each side of the body, i.e. shoulder shrug (C4), elbow flexion (C5), wrist extension (C6), elbow extension (C7), hip flexion (L2).
Classification of SCI
Traumatic spinal cord injury is classified into five types by the American Spinal Injury Association and the International Spinal Cord Injury Classification System
Asia Class A
Indicates a "complete" spinal cord injury where no motor or sensory function is preserved in the sacral segments S4-S5
Since the S4-S5 segment is the lower segmental, absence of motor and sensory function indicates "complete" spinal cord injury.
Complete SCI
Total loss of all motor and sensory function below the level of injury.
Nearly 50 percent of all SCIs are complete.
Both sides of the body are equally affected.
Even with a complete SCI, the spinal cord is rarely cut or transected.
More commonly, loss of function is caused by a contusion or bruise,compromise of blood flow to the injured part of the spinal cord.
Asia Class B
Indicates an "incomplete" spinal cord injury where sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5.
This is typically a transient phase and if the person recovers any motor function below the neurological level, that person essentially becomes a motor incomplete, i.e., ASIA C or D
Asia Class C
Indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and more than half of key muscles below the neurological level have a muscle grade of less than 3.
Asia Class D
Indicates an "incomplete" spinal cord injury where motor function is preserved below the neurological level and at least half of the key muscles below the neurological level have a muscle grade of 3 or more.
Asia Class E
Indicates "normal" where motor and sensory scores are normal. Note that it is possible to have spinal cord injury and neurological deficit with completely normal motor and sensory scores.
Incomplete SCI
Some function remains below the primary level of the injury.
May be able to move one arm or leg more than the other, or may have more functioning on one side of the body than the other.
Often falls into one of several patterns.
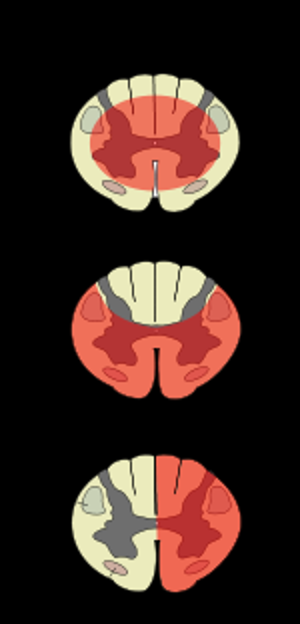
The Anterior cord syndrome
Results from injury to the anterior part of the spinal cord, causing weakness and loss of pain and thermal sensations below the injury site
But preservation of proprioception is usually carried out in the posterior part of the spinal cord.
Infarction in anterior 2/3 of cord
Flaccid paraplegia below the level of the lesion
Dissociated sensory loss
loss of pain/temp below the level of lesion
intact proprioception and vibration
dorsal columns spared--> supplied by the posterior spinal artery
Occurs in watershed distribution (~T4)
Associated with atherosclerosis, hypotension, dissecting aneurysm, or repair of aortic aneurysms
Ipsilateral findings below level of injury
UMN signs
Loss of proprioception, vibration
Ipsilateral findings at level of injury
paresthesias and radicular pain
Contralateral findings
loss of pain and temperature extending to ~2
dermatomes below level of injury
Tabes Dorsalis
Results from injury to the posterior part of the spinal cord, usually from infection diseases such as syphilis, causing loss of touch and proprioceptive sensation.
Clinical of Brown-Sequard Syndrome
Ipsilateral findings below level of injury
Ipsilateral findings at level of injury
Contralateral findings
Tabes Dorsalis
Degeneration of posterior columns
Develops 10-20 years after syphilis
Posterior roots are affected in addition to the posterior columns
“lightning” pains
ataxia
bladder disturbance
What are the classic triad of symptoms for Tabes Dorsalis?
Signs of Tabes Dorsalis
loss of proprioception (sensory ataxia)
areflexia
argyll-robertson pupils
only react to accomodation, not to light
Conus medullaris syndrome
Results from injury to the tip of the spinal cord, located at L1 vertebra.
Cauda equina syndrome
is, strictly speaking, not really spinal cord injury but injury to the spinal roots below the L1 vertebra.
Spinal Concussion
These can be complete or incomplete, spinal cord dysfunction is transient, generally resolving within one or two days.
Football players are especially susceptible to spinal concussions and spinal cord contusions.
Numbness, tingling, electric shock-like sensations, and burning in the extremities.
Fracture-dislocations with ligamentous tears may be present in this syndrome.
Penetrating SCI
Gunshot wounds - common
Require neurosurgical decompression
May need to be immobilized with a collar or brace for several weeks
Surgery to remove the bullet does not yield much benefit and may create additional risks, including infection, cerebrospinal fluid leak, and bleeding.
Symptoms of SCI
Extreme pain or pressure in the neck, head, or back
Tingling or loss of sensation in the hand, fingers, feet, or toes
Partial or complete loss of control over any part of the body
Urinary or bowel urgency, incontinence, or retention
Difficulty with balance and walking
Abnormal band-like sensations in the thorax - pain, pressure
Impaired breathing after injury
Unusual lumps on the head or spine
Complications of SCI
Pneumonia
Decubitus ulcers
GI hemorrhage
Thrombophlebitis
Pulmonary embolism
Arrhythmia
Wound infection
AMI
Pneumonia & Decubitus ulcers
Most common complications of SCI?
Surgical Advances
Decompression and stabilization of spine.
Management of syringomyelic cysts.
Peripheral nerve bridging.
Implanting avulsed roots or nerves into the spinal cord.
Some Recent Approaches to Spinal Injury
Biochemical to overcome inhibitory factors.
Cellular approaches to provide a substrate for axonal regeneration or as cell replacement therapy.
Management of the inflammatory response.
Laminectomy

Central Cord Syndrome (Syringomyelia)
Associated with greater loss of upper limb function compared to lower limbs.
Usually results from trauma
Damage to the large nerve fibers that carry information directly from the cerebral cortex to the spinal cord.
Paralysis and/or loss of fine control of movements in the arms and hands, with far less impairment of leg movements. Sensory loss below the site of the SCI and loss of bladder control may also occur, with the overall amount and type of functional loss related to the severity of damage to the nerves of the spinal cord.
Clinical of Syringomyelia
Dissociated sensory loss
Loss of pain & temperature in a cape-like distribution with other sensory modalities spared
frequent burns/injuries to the arm (pt can’t feel pain)
Segmental paresis w/LMN signs
Horner’s (if the lesion is in the thoracic cord)
Sacral sparing
Brown-Séquard syndrome
Results from injury to one side with the spinal cord, causing weakness and loss of proprioception on the side of the injury and loss of pain and thermal sensation of the other side.