IB BIOLOGY OPTION D: HUMAN PHYS
5.0(1)
Card Sorting
1/200
Earn XP
Description and Tags
Last updated 1:06 PM on 4/25/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
201 Terms
1
New cards
What is nutrition?
the supply of nutrients
2
New cards
What are essential nutrients?
Essential nutreients are substances that the body needs but it cannot synthesize, and thus they must be in the diet
3
New cards
What are the four chemical groups of essential nutreints?
Minerals - specific elements such as calcium or iron
Vitamins - chemically diverse carbon compounds needed in small amounts, such as ascorbic acid and calciferol
Amino acids - some of the 20 are not able to be synthesized by humans but obviously necessary for protein creation
Fatty acids - essential for the same reason, example: omega-3 fatty acids
Vitamins - chemically diverse carbon compounds needed in small amounts, such as ascorbic acid and calciferol
Amino acids - some of the 20 are not able to be synthesized by humans but obviously necessary for protein creation
Fatty acids - essential for the same reason, example: omega-3 fatty acids
4
New cards
What is malnutrition?
Malnutrition is a deficiency, imbalance, or excess of specific nutrients in the diet.
5
New cards
Where is appetite controlled?
Appetite is controlled by a center in the hypothalamus. The small intestine, pancreas and adipose tissue secrete different hormones when nutrient levels are too high. If the hypothalamus receives these chemicals it reduces the desire to eat.
6
New cards
What is obesity?
Obesity is the excessive storage of fat in adipose tissue, due to the prolonged intake of more energy in the diet than is used in cell respiration.
7
New cards
What health issues does obesity make more likely?
Obese persons are more likely to experience hypertension (high blood pressure) and type II diabetes
8
New cards
What is starvation and what can it lead to?
Starvation is a prolonged shortage of food. Once glycogen and fat reserves are used up, starvation can lead to the breakdown of body tissue to be used in cellular respiration
9
New cards
What is vitamin C deficiency and why does it happen?
Vitamin C, also known as ascorbic acid, is needed to synthesize collagen fibres in body tissues such as skin and blood vessel walls. Humans cannot synthesize ascorbic acid so it must be ingested. Without it humans get scurvy. Scurvy only happens in us and few other mammals because most mammals have the enzyme needed for abscorbic acid synthesis.
10
New cards
What is Phenylketonuria ?
Phenylketonuria (PKU) is when the level of phenylalanine (an essential amino acid) becomes too high in the bloodstream. It is caused by an insufficiency or lack of phenylalanine hydroxylase, which turns phenylalanine into tyrosine. The insufficiency or lack of this enzyme is due to a mutation of the gene that codes for it.
11
New cards
How is phenylketonuria treated?
Phenylketonuria symptoms are not present in fetuses because the mother's body regulates phenylalanine concentrations. Phenylketonuria is now tested for at birth so that a diet can be implemented to prevent most/all harmful consequences
12
New cards
Explain vitamin D deficiency in humans
Without sufficient vitamin D the body cannot absorb enough calcium from food in the gut. The consequence is osteomalacia. Osteomalacia is inadequate bone mineralization due to calcium salts not being deposited or being reabsorbed, so bones soften. In children, osteomalacia is called rickets.
13
New cards
What is anorexia and what are its consequences?
Anorexia is a condition in which an individual does not eat enough food to sustain the body, even though the food is available. As with starvation body tissues can be broken down, and with severe anorexia even the heart muscle is broken down.
14
New cards
Explain the relation between cholesterol and heart disease.
There has been research showing a correlation between high levels of cholesterol in blood plasma and an increased risk of coronary heart disease(CHD).
-Only low-density lipoprotein is implicated in CHD
-Reducing cholesterol consumption has very little effect on blood cholesterol levels
-The liver can synthesize cholesterol, so dietary cholesterol is not the only source
-Genetic factors are more important than dietary intake
-Positive correlation between intake of saturated fats and of cholesterol, so maybe its the sat fats, not the cholesterol, that caues risk of CHD
-Only low-density lipoprotein is implicated in CHD
-Reducing cholesterol consumption has very little effect on blood cholesterol levels
-The liver can synthesize cholesterol, so dietary cholesterol is not the only source
-Genetic factors are more important than dietary intake
-Positive correlation between intake of saturated fats and of cholesterol, so maybe its the sat fats, not the cholesterol, that caues risk of CHD
15
New cards
How do you measure the energy content of food?
You burn the food then use this formula: Energy content of food (J/g) =
temp rise (C) x water volume (ml) x 4.2J
\-------------------------------
mass of food (g)
temp rise (C) x water volume (ml) x 4.2J
\-------------------------------
mass of food (g)
16
New cards
What does RDA stand for when relating to the nutritional content of foods?
Recommended Daily Amount
Can be in either percentage or mass units
Can be in either percentage or mass units
17
New cards
What controls the secretion of digestive juices?
Secretion of digestive juices is controlled using nerves and hormones.
18
New cards
What are the two types of glands?
Exocrine and endocrine glands.
Exocrine glands secret through a duct onto the surface of the body or into the lumen of the gut. Digestive-juice-excreting glands are exocrine.
Endocrine glands are ductless and secrete hormones directly into blood.
Exocrine glands secret through a duct onto the surface of the body or into the lumen of the gut. Digestive-juice-excreting glands are exocrine.
Endocrine glands are ductless and secrete hormones directly into blood.
19
New cards
Explain the specific control of volume and content of gastric secretions.
-The sight/smell of food stimulates brain to send nerve impulses to parietal cells
-Parietal cells respond by secreting acid, known as a reflex action
-Sodium and chloride ions also secreted, causing water to osmos into the stomach to form gastric juice
-Food enters the stomach and chemoreceptors detect amino acids
-Brain sends impulses via vagus nerve to endocrine cells to make them secret gastrin
-Hormone gastrin stimulates further sectrion of acid and pepsinogen
-Secretin and somatostatin inhibit gastrin sectrion if pH gets too low
-Parietal cells respond by secreting acid, known as a reflex action
-Sodium and chloride ions also secreted, causing water to osmos into the stomach to form gastric juice
-Food enters the stomach and chemoreceptors detect amino acids
-Brain sends impulses via vagus nerve to endocrine cells to make them secret gastrin
-Hormone gastrin stimulates further sectrion of acid and pepsinogen
-Secretin and somatostatin inhibit gastrin sectrion if pH gets too low
20
New cards
Explain the role of acid conditions in the process of digestion.
Acid conditions in the stomach favour some hydrolysis reactions and help to control pathogens in ingested food. The acid secreted by the parietal cells disrupts the extracellular matrix that holds cells together and denatures proteins exposing their polypeptide chains.
21
New cards
Describe the adaptations of the villus epithelium cells.
The structure of cells in the epithelium of the villi is adapted to the absorption of food.
-Epithelial cells on covering the villus adhere to each other ensuring that most materials pass through epithelial cells on the way to the blood stream
-Surface membrane of lumen has many microvilli, created a brush border, increasing surface area for absorption
-Many mitochondria in epithelial cells to power active transport
-Many pinocytic vesicles due to absorption of some food by endocytosis
-In epithelial cells, the side facing the lumen (apical surface) has different types of proteins to help with transport from the side facing the blood vessels (basal surface)
-Epithelial cells on covering the villus adhere to each other ensuring that most materials pass through epithelial cells on the way to the blood stream
-Surface membrane of lumen has many microvilli, created a brush border, increasing surface area for absorption
-Many mitochondria in epithelial cells to power active transport
-Many pinocytic vesicles due to absorption of some food by endocytosis
-In epithelial cells, the side facing the lumen (apical surface) has different types of proteins to help with transport from the side facing the blood vessels (basal surface)
22
New cards
Explain the role of dietary fibre in digestion
The rate of transit of materials through the large intestine is positively correlated with the fibre content.
Fibre is non-readily digestible material, and increases the mass of material passing through the intestines. This helps prevent constipation because it draws water into the intestine, which speeds movement of fecal matter.
Fibre may also reduce bowel cancer, haemorrhoids and appendicitis, and reduce appetite to prevent obesity, absorption of sugars can be slowed preventing type II diabetes.
Fibre is non-readily digestible material, and increases the mass of material passing through the intestines. This helps prevent constipation because it draws water into the intestine, which speeds movement of fecal matter.
Fibre may also reduce bowel cancer, haemorrhoids and appendicitis, and reduce appetite to prevent obesity, absorption of sugars can be slowed preventing type II diabetes.
23
New cards
What happens to ingested materials that are not absorbed?
Materials that have been ingested but then not absorbed are egested (pooped out). An example of a material like this is dietary fibre.
24
New cards
Explain how protein pumps can be inhibited by drugs.
Many diseases are worsened by the release of stomach acid. Acidity in the stomach is produced by a proton pump called the "H⁺, K⁺-ATPase". The pump uses 1 ATP to exchange 2 protons from the cytoplasm for two potassium ions in the lumen. Treating stomach acid diseases is done by proton pump inhibitors (PPIs). Each PPI permanently bonds to one pump, reducing its activity. They're not permanently effective because proton pumps are eventually replaced.
25
New cards
Explain dehydration due to cholera.
Cholera is a disease caused by infection from the bacterium Vibrio cholera. The bacterium releases a toxin that binds to receptors on intestinal cells. Once brought into the cell by endocytosis the toxin triggers a cascade response that leads to the discharge of Cl⁻ and HCO₃⁻ ions from the cell into the intestine. Water follows these ions through osmosis, leading to diarhea, and water is drawn in to replace the lost water from the blood stream, leading to dehydration.
26
New cards
Explain how bacterial infections cause ulcers.
Stomach ulcers are caused by the bacterium Heliobacter pylori. It causes part of the stomach lining to be digested by pepsin and HCl leading to open sores.
27
New cards
How does the liver act as a detoxifier?
The liver removes toxins from the blood and detoxifies them. It does this using a range of chemical conversions.
Examples:
alcohol converted into less toxic substance by ethanol dehydrogenase
Ammonia into urea
One general method the liver uses is to convert hydrophobic comounds into hydrophillic compounds for easier excretion
Examples:
alcohol converted into less toxic substance by ethanol dehydrogenase
Ammonia into urea
One general method the liver uses is to convert hydrophobic comounds into hydrophillic compounds for easier excretion
28
New cards
State the liver's role as red blood cell recycler
Red blood cells in adults last about 120 days. Old and damaged red blood cells undergo changes making them susceptible to recognition by macrophages. At the end of life they are removed from circulation and broken down in the spleen and liver.
29
New cards
Explain the role of Kupffer cells in the breakdown of red blood cells.
The breakdown of erythrocytes (red blood cells) starts with phagocytosis by Kupffer cells.
When cells get old they are engulfed by Kupffer cells, macrophages lining the liver.
When cells get old they are engulfed by Kupffer cells, macrophages lining the liver.
30
New cards
Explain the transport of iron to bone marrow.
Iron is carried to the bone marrow to produce hemoglobin in new red blood cells.
Red blood cells are created in bone marrow, and hemoglobin is synthesized in red blood cells. Iron is added to the heme group here.
Red blood cells are created in bone marrow, and hemoglobin is synthesized in red blood cells. Iron is added to the heme group here.
31
New cards
Explain the conversion of cholesterol to bile salts.
Surplus cholesterol is converted into bile salts.
Cholesterol is both absorbed through food and synthesized by liver cells. The liver also regulates cholesterol levels, synthesizing or breaking down cholesterol as necessary.
Cholesterol is both absorbed through food and synthesized by liver cells. The liver also regulates cholesterol levels, synthesizing or breaking down cholesterol as necessary.
32
New cards
Explain how the liver processes nutrients.
The liver intercepts blood from the gut to regulate nutrient levels.
The liver regulates glucose levels by storing glucose as glycogen or breaking glycogen into glucose.
The body can't store proteins or amino acids so excess is broken down in the liver and the nitrogenous waste is processed by the liver.
The liver regulates glucose levels by storing glucose as glycogen or breaking glycogen into glucose.
The body can't store proteins or amino acids so excess is broken down in the liver and the nitrogenous waste is processed by the liver.
33
New cards
Explain storage of nutrients in the liver.
When glucose levels are high insulin is released triggering the liver to store glucose as glycogen. When glucose levels are low glucagon is released and glycogen, glycerol, amino acids and fatty acids are broken down in the liver releasing glucose.
Iron, vitamin A, vitamin D are stored in the liver when in excess and released into blood when there is a deficit.
Iron, vitamin A, vitamin D are stored in the liver when in excess and released into blood when there is a deficit.
34
New cards
What are the causes of jaundice?
When the liver breaks down red blood cells, a pigment is produced called bilirubin. Buildup of bilirubin causes jaundice. In adults, liver problems that contribute to jaundice can be caused by alcoholism, liver diseases and blood diseases.
35
New cards
What are the consequences of jaundice?
People with jaundice experience discoloration in the skin and eyes due to the deposition of excess bilirubin (pigment) in the skin tissues. Jaundice is actually a symptom, not really a disease.
36
New cards
Explain the dual supply of blood to the liver.
Blood is brought to the liver by both the hepatic portal vein and the hepatic artery.
The hepatic portal vein carries the most blood and brings blood from the stomach and intestines. The blood can be rich in nutrients if eating has just occurred but oxygen levels are low.
The vein subdivides into sinusoids in the liver, like capillaries but wider and walls are not continuously lined with cells. This allows blood flowing through to come in contact with liver cells.
The hepatic artery brings oxygen-rich blood from the aorta.
The hepatic portal vein carries the most blood and brings blood from the stomach and intestines. The blood can be rich in nutrients if eating has just occurred but oxygen levels are low.
The vein subdivides into sinusoids in the liver, like capillaries but wider and walls are not continuously lined with cells. This allows blood flowing through to come in contact with liver cells.
The hepatic artery brings oxygen-rich blood from the aorta.
37
New cards
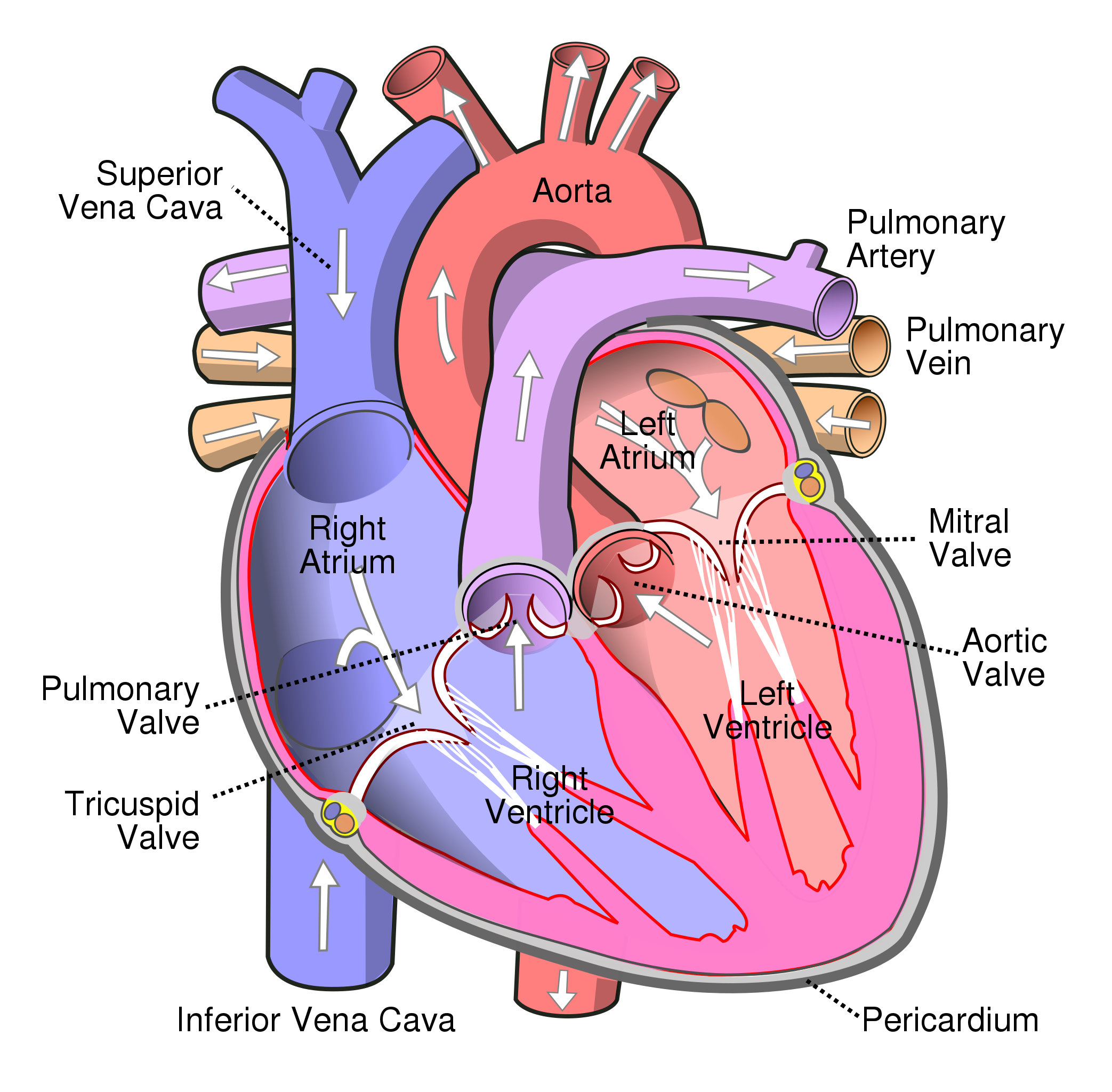
Diagram of heart
38
New cards
Explain the structure of cardiac muscle cells. What does their structure allow them to do?
Cardiac muscle cells are striated, like skeletal muscles. However cardiac muscle cells are shorter and wider than skeletal muscles, and normally only have one nucleus per cell. The cells are Y-shaped and all interconnected into a complex network. Where one cell connects to another there is a junction called an "intercalated disc". This junction consists of a double membrane with gap junctions allowing cells to connect cytoplasms. This overall structure allows them to be physically connected (Y-shapes) and have quick electrical/ion transport (connected cytoplasms) meaning that stimuli in one cell causes the entire network to contract as if it were one large cell.
39
New cards
What is the definition of systole?
Systole is the contraction of the heart's chambers.
40
New cards
What is the definition of diastole?
Diastole is the relaxation of the heart's chambers
41
New cards
What is the function of the sinoatrial node?
The sinoatrial node (often referred to as the pacemaker) is a collection of specially structured cardiac cells that spontaneously initiate action potentials without stimulation from other cells. Thanks to gap junctions the action potential quickly spreads across the entire atrium causing the atria to undergo systole (contraction).
42
New cards
What is the function of the atrioventricular node?
Signals from the sinoatrial node causing contraction in the atria cannot pass directly from the atria to the ventricles, the signal instead passes through the atrioventricular node. The function of the atrioventricular node is to create a delay between the arrival and passing of the stimulus. This delay is about 0.12 seconds between arrival and initiation of impulse. The delay is caused by a few structural things in the AV node:
-AV node cells have a smaller diameter and do not conduct as quickly
-There are fewer gap junctions in the AV node
-There is more non-conductive tissue in the AV compared to the SA node
-AV node cells have a smaller diameter and do not conduct as quickly
-There are fewer gap junctions in the AV node
-There is more non-conductive tissue in the AV compared to the SA node
43
New cards
What is the purpose of the 0.12s delay between the arrival and passing on of the stimulus in the AV node?
The delay ensures that the atria contract and empty the blood they contain into the ventricles first before the ventricles contract.
44
New cards
Explain how the contraction of the ventricle is coordinated after passing through the AV node.
The signal needs to be conducted rapidly after passing through the AV bundle, in order to ensure the coordinated contraction of the ventricle. The AV bundle receives the impulse from the AV node and conducts the signal rapidly to a fork that splits into the right and left bundle branches. The branches connect to Purkinje fibres at the base of the heart, these fibres conduct the signal even more rapidly to the ventricles.
45
New cards
What are some features of Purkinje fibres that allow them to conduct signals at such a high speed?
They have relatively fewer myofibrils
They have a bigger diameter
They have higher densities of voltage-gated sodium channels
They have high numbers of mitochondria and high glycogen stores
They have a bigger diameter
They have higher densities of voltage-gated sodium channels
They have high numbers of mitochondria and high glycogen stores
46
New cards
What causes the sound of the heartbeat?
The "lub-dub" (yes that's the term the IB uses) sound is caused by the closing of valves. The "lub" is heard when the atrioventricular valves close. The "dub" sound is heard after the ventricles are emptied and the semilunar valves close.
47
New cards
What are some variables that affect heart rate?
Variables that affect heart rate that are good to investigate are: type of excersize, intensity of exercise, recovery from exercise, relaxation, body position, breathing and breath holding, exposure to a cold stiumuls and facial immersion in water.
48
New cards
What are some ways to detect and measure heart rate?
Heart rate can be detected by using fingers to feel the pulse of an artery in the wrist, or an artery in the neck. Additionally; hand grip heart monitors, ear clips, EKG sensors, wrist watches and even camera smartphones can measure heart rate and feed data into computers.
49
New cards
Explain the use of artificial pacemakers to regulate heartbeat.
When the sinoatrial node malfunctions, patients are fitted with a pacemaker. It essentially maintains the rhythmic beating of the heart by mimicking the sinoatrial node's ability to send out a stimulus. Pacemakers can either provide a regular impulse or disarge only when a heartbeat is missed so that it beats normally.
50
New cards
Explain the graph of the ECG Trace
ECG stands for electrocardiogram, it shows the electrical signals received by the cardiac muscles.
P-wave: caused by atrial systole
QRS wave: caused by ventricular systole
T-wave: coincides with ventricular diastole
Changes to the different waves are used to detect heart pathology
P-wave: caused by atrial systole
QRS wave: caused by ventricular systole
T-wave: coincides with ventricular diastole
Changes to the different waves are used to detect heart pathology
51
New cards
Explain the use of a defibrillator to treat life-threatening cardiac conditions.
Cardiac arrest occurs when the blood supply to the heart is reduced and the heart runs out of oxygen. This can result in abnormalities in the cardiac cycle, such as ventricular fibrillation. This is the twitching of the ventricles due to chaotic contraction of individual muscle cells. A defibrillator gives off an electric discharge to restore a normal heart rhythm.
52
New cards
What is thrombosis? What are the consequences?
Thrombosis is the buildup of plaque, caused by excess levels of lipids and cholesterol in the blood, that becomes serious enough where a clot is formed and blood flow through an artery is blocked. If this occurs on the surface of the heart the consequence can be a heart attack as the heart is deprived of sufficient oxygen. Another consequence is hypertensino
53
New cards
What is hypertension? What are the consequences?
Hypertension is the greater pressure on the walls of arteries, caused by a slowing in the flow of blood (often due to thrombosis). Consequences include:
-Damage to cells that line arteries causing chain events that result in narrow and stiff arteries
-Constant high blood pressure weaken an artery causing a section of the wall to form a bulge (known as aneurysm). This aneurysm could burst and cause internal bleeding
-Constant high blood pressure can also cause stroke by weakening blood vessels in the brain, causing them to rupture.
-Constant high blood pressure also can causae kiddney failure as it damages the arteries leading into the kidney and the capillaries in the glomerulus.
-Damage to cells that line arteries causing chain events that result in narrow and stiff arteries
-Constant high blood pressure weaken an artery causing a section of the wall to form a bulge (known as aneurysm). This aneurysm could burst and cause internal bleeding
-Constant high blood pressure can also cause stroke by weakening blood vessels in the brain, causing them to rupture.
-Constant high blood pressure also can causae kiddney failure as it damages the arteries leading into the kidney and the capillaries in the glomerulus.
54
New cards
What are some risk factors that increase the risk of thrombosis and hypertension?
-Genetic predisposition
-Old age causing less flexible blood vessels
-A risk is in post-menopause females correlated with fall in estrogen
-Males are at greater risk period because of less estrogen
-Smoking raises blood pressure (nicotine causes vasoconstriction)
-High salt diet
-High levels of alcohol
-Stress
-Eating too much saturated fat and cholesterol promotes plaque formation
-Height affects blood pressure
-Sedentary lifestyle
-Old age causing less flexible blood vessels
-A risk is in post-menopause females correlated with fall in estrogen
-Males are at greater risk period because of less estrogen
-Smoking raises blood pressure (nicotine causes vasoconstriction)
-High salt diet
-High levels of alcohol
-Stress
-Eating too much saturated fat and cholesterol promotes plaque formation
-Height affects blood pressure
-Sedentary lifestyle
55
New cards
Explain blood pressure measurements.
Blood pressure comes in two numbers, a higher and lower one, and in units "mm Hg". The higher number refers to pressure in the artery caused by ventricular systole. The lower number refers to pressure in artery caused by ventricular diastole.
Hypotension (low blood pressure): 90 or less over 60 or less
Normal: Less than 120 over less than 80
Pre-hypertension: 120-139 over 80-89
Hypertension stage 1: 140-159 over 90-99
Hypertension stage 2: 160 or higher over 100 or higher
Hypertension crisis: Higher than 180 over higher than 110
Hypotension (low blood pressure): 90 or less over 60 or less
Normal: Less than 120 over less than 80
Pre-hypertension: 120-139 over 80-89
Hypertension stage 1: 140-159 over 90-99
Hypertension stage 2: 160 or higher over 100 or higher
Hypertension crisis: Higher than 180 over higher than 110
56
New cards
What is coronary heart dieseae and what are the risk factors?
Coronary heart disease (CHD) is damage to the heart as a consequence of reduced blood supply to the tissues of the heart, often due to narrowing and heardening of coronary artery.
Ethnic group differ in risk due to diets and lifestyles
Gender, age, physical activity, genotype, medical history all have different effects on probabilyt of experiencing CHD
Ethnic group differ in risk due to diets and lifestyles
Gender, age, physical activity, genotype, medical history all have different effects on probabilyt of experiencing CHD
57
New cards
What do pituitary hormones do?
Pituitary hormones are secreted by the pituitary and control; growth, developmental changes, reproduction, and homestasis.
58
New cards
What is the role of the hypothalamus in hormone secretion?
The hypothalamus controls hormone secretion by the anterior and posterior lobes of the pituitary gland. It links the nervous system to the endocrine system via the pituitary gland. The role of the hypothalamus is to secrete releasing factors that stimulate the secretion of the anterior pituitary gland's hormones. The releasing factors are transported from the hypothalamus to the pituitary gland by way of the partal vein.
59
New cards
Why do some athletes take growth hormones and how do they work?
Growth hormone is produced by the anterior pituitary. It targets receptors in liver cells. It stimulates the release of insulin-like growth factor which circulates blood and stimulates bone and cartilage growth. It also causes increased muscle mass, but not necessarily increased strength. It may also allow tired muscles to recover more quickly.
60
New cards
What are pneumocytes?
Pneumocytes are the cells that compose the wall of the alveolus. There are type 1 and type 2 pneumocytes.
Type 1: cover 90% of alveolus surface. Extremely thin. Primary purpose of gas exchange
Type 2: covered in microvilli, thicker, funtion to secrete surfactant, a substance that reduces surface tension to prevent alveolus from collapsing
Type 1: cover 90% of alveolus surface. Extremely thin. Primary purpose of gas exchange
Type 2: covered in microvilli, thicker, funtion to secrete surfactant, a substance that reduces surface tension to prevent alveolus from collapsing
61
New cards
How does high altitude affect gas exchange?
At high altitude there is low pO₂ in the air, meaning hemoglobin may not become fully saturated, and thus the tissues may not be adequately supplied with oxygen. Adaptations to high altitude can happen, red blood cell production can increase, muscles produce more myoglobin, and evolution can lead to greater mean lung surface area and large vital capacities.
62
New cards
What is emphysema?
Emphysema is a lung condition where the walls between individual alveoli break down, leading to an increase in their size and thus a decrease of surface area for gas exchange, restricting oxygen uptake into the blood. Caused by long-term exposure to airborne irritants such as smoke, air pollution or coal and silica dust. Three factors cause the damage:
-oxidation reactions produced by high concentration of free radicals in tobacco smoke
-inflammation due to body responding to irritant particles in the smoke
-free radicals and other components of tobacco smoke impair activity of enzyme alpha-1-antitrypisn which would normally block the activity of proteases that degrade the proteins that miantain the elasticity of the lung
-oxidation reactions produced by high concentration of free radicals in tobacco smoke
-inflammation due to body responding to irritant particles in the smoke
-free radicals and other components of tobacco smoke impair activity of enzyme alpha-1-antitrypisn which would normally block the activity of proteases that degrade the proteins that miantain the elasticity of the lung
63
New cards
What are the treatments for emphysema?
Emphysema cannot be cured but there are treatments. Constant administration of oxygen-rich air, training in breathing techniques, quitting smoking, and sometimes surgery to reduce volume of lungs by removing lung tissue. Last case resort is lung transplant.
64
New cards
Minerals
specific elements such as calcium and iron
65
New cards
vitamins
chemically diverse carbon compounds needed in small amounts that cannot be synthesized by the body
66
New cards
example of 2 vitamins
ascorbic acid and calciferol
67
New cards
example of fatty acids that, along with some amino acids allow the production of proteins at ribosomes to continue
omega-3 fatty acids
68
New cards
malnutrition
deficiency, imbalance or excess of specific nutrients in the diet
69
New cards
what can carbohydrates, lipids and amino acids all be used for as a source of energy
aerobic cell respiration
70
New cards
what happens when the energy in the diet is insufficient
reserves of glycogen and fats are mobilised and used.
71
New cards
starvation
prolonged shortage of food
72
New cards
what happens when glycogen and fat reserves are used up
body tissues have to be broken down and used in respiration (starvation & anorexia)
73
New cards
Anorexia
an individual does not eat enough food to sustain the body even though it is available
74
New cards
what can happen in advanced cases of anorexia
heart muscle is broken down
75
New cards
obesity
excessive storage of fat in adipose tissue, due to prolonged in take of more energy in the diet than is used in cell respiration
76
New cards
obesity can lead to which health issues
hypertension (high blood pressure) and Type 2 diabetes
77
New cards
what is responsible for feelings of appetite or satiety
hypothalamus
78
New cards
joules of energy need to heat 1ml of water by one degree
4.2 joules
79
New cards
energy content of a food\=
(temp rise X water volume (ml) X 4.2L)/mass of food (g)
80
New cards
website to get nutritional info
my food record .com
81
New cards
what type of cholesterol is implicated in CHD
low-density lipoprotein
82
New cards
what effect does reducing dietary cholesterol have on blood cholesterol levels
very small
83
New cards
what organ can synthesise cholesterol meaning dietary cholesterol is not the only source
liver
84
New cards
what are considered more important than dietary intake when talking about heart disease
genetic factors, some families have high cholesterol even with low dietary intake
85
New cards
what does the positive correlation between dietary intake of saturated fats and intake of cholesterol mean when discussing links to heart disease
possible that saturated fats, not cholesterol, caused increase of CHD in people
86
New cards
what happens when there is insufficient vitamin D in the body
calcium is not absorbed from food in the gut to large enough quantities
87
New cards
osteomalacia
inadequate bone mineralization due to calcium salts not being deposited or being reabsorbed so bones become softened
88
New cards
rickets
bowing of legs, bone pain
89
New cards
where is vitamin D found
oily fish, eggs, milk, butter, cheese and liver
90
New cards
what is unusual about vitamin D
can be synthesised in the skin but only by UV light
91
New cards
what is ascorbic acid needed for
synthesis of collagen fibres in many body tissues including skin and blood vessel walls
92
New cards
lack of vitamin c causes
scurvy
93
New cards
why were attempts to induce scurvy in rats unsuccessful
most mammals (apart from humans) have enzymes needed for synthesis in ascorbic acid
94
New cards
two other animals that require ascorbic acid in diet
chimpanzees and guinea pigs
95
New cards
what is phenylalanine
essential amino acid
96
New cards
why is tyrosine a non-essential amino acid
it can by synthesised from phenylalanine using phenylalanine hydroxylase
97
New cards
what happens in phenylketonuria
level of phenylalanine in the blood becomes too high
98
New cards
cause of phenylketonuria
insufficiency or complete lack of phenylalanine hydroxylase due to a mutation of the gene coding for the enzyme
99
New cards
what type of disease is PKU
genetic disease and the allele is recessive
100
New cards
treatment for PKU
diet with low levels of phenylalanine, foods such as meat, fish, nuts, cheese and beans can only be eaten in small quantities