Mouth and Throat Disorders
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
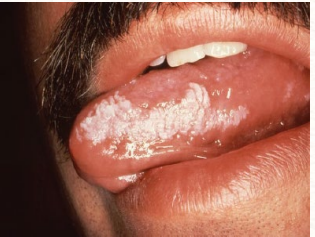
Leukoplakia
hyperkeratosis occurring in response to chronic irritation that can sometimes represent dysplasia or early invasive squamous cell carcinoma
-commonly presents as fixed white lesions on mucosal surface
tobacco, alcohol
Risk Factors of Leukoplakia
-HPV
-_______ use, specifically chew
-_________ use
Homogenous
type of leukoplakia that is uniformly white

Nonhomogenous
type of leukoplakia that is speckled between white and red lesions, higher risk of oral cancer
laser, medications
Treatment of Leukoplakia
-Surgery, _______ ablation, cryosurgery, and ___________ (retinoids, Vitamin A)
-Perform a biopsy because this is potentially malignant
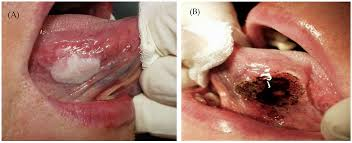
Erythroplakia
painless, erythematous, velvety patch most commonly found on the mouth floor, ventral aspect of the tongue, or the soft palate
-90% of cases are dysplasia or carcinoma

age, tobacco
Risk Factors of Erythroplakia
-_____, usually seen in older patients
-__________ and alcohol use
biopsy, surgical, referral
Diagnosis and Treatment of Erythroplakia
-Incisional _________ or exfoliative cytologic exam
-__________ excision is treatment of choise
-Early ________ is important for diagnosis
Oral Squamous Cell Carcinoma
90% of oral cancers that causes red (erythroplakia), white (leukoplakia), or a mix of both (erythroleukoplakia) sometimes with an ulcer

ulcer, lateral, floor, resection, radiation, biopsy
Symptoms and Treatment of Oral Squamous Cell Carcinoma
-Red (erythroplakia), white (leukoplakia), or mix of both (erythroleukoplakia) sometimes with an _______
-Location: ________ border of the tongue, oropharynx, and ______ of mouth
-Most, if < 2 cm are cured by local _______. __________ is alternative treatment but generally not used as 1st line for small lesions
-Any single ulcerated lesion persisting for more than 3 weeks should be sent for ________

alcohol, tobacco, older
Risk Factors and Epidemiology of Oral Squamous Cell Carcinoma
-__________ and smoking are the highest, followed by the use of chewing _______ and HPV.
-Found most often in middle aged and ________ persons
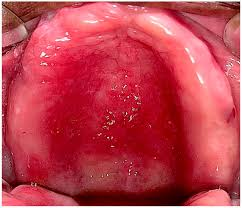
Thrush (Oral Candidiasis)
painful, creamy-white curd like patches over erythematous mucosa caused by an infection of Candida albicans

dentures, DM, immunocompromised
Risk Factors of Oral Candidiasis (Thrush)
-Use of _________, poor oral hygiene, __
-Anemia, chemotherapy or local radiation
-Corticosteroid use, antibiotic use
-_______________ state (ex HIV)
Rubbed off
The main differences between oral candidiasis and leukoplakia is that thrush can be ________ ___ and can be painful
clinical, KOH, topical, oral
Diagnosis and Treatment of Oral Candidiasis
-Usually ______
-___ prep: budding yeast with or without pseudohyphae. Could also perform a biopsy if needed
-First line treatment are _______ antifungals (Clotrimazole troches or Nystatin mouth rinse)
-______ antifungals (Fluconazole or Ketoconazole) are saved for resistant cases or for patients with immunosuppressive conditions
Denture Stomatitis (atrophic form)
inflammatory condition of the oral mucosa that occurs in denture wearers, characterized by redness, swelling, and soreness of the tissues beneath the denture
Aphthous Ulcer (Canker sore/ulcerative stomatitis)
painful, small, round ulcerations with yellow-gray centers surrounded by red halos found on buccal and/or labial mucosa
-unknown etiology, thought to be an immune mechanism

spontaneously, corticosteroids, oral, biopsied
Treatment of Aphthous Ulcer (Canker Sore/Ulcerative Stomatitis)
-Generally heal in 10-14 days __________
-Topical anesthetics (2% viscous lidocaine) could be prescribed for pain
-First line treatment for mild-moderate disease is topical ___________ (dexamethasone elixir)
-______ steroids should be given for severe disease states
-Mary’s Magic Mouthwash (2% viscous lidocaine, diphenhydramine, nystatin, hydrocortisone, mylanta)
-Large or persistent areas should be _________
Angular Cheilitis
acute or chronic inflammation located at the lateral commissures of the mouth

moisture, candida, staph, erythema, scaling
Etiology and Symptoms of Angular Cheilitis
-Excessive _______, most common cause is ________ albicans, and ______ aureus
-____________, maceration, ______, and fissuring
KOH, barrier, azole, mupirocin
Diagnosis and Treatment of Angular Cheilitis
-___ prep, culture for staph
-________ cream (zinc oxide), topical _______ for candida (clotrimazole and miconazole), and topical _______ for staph aureus
HSV 1, epidermis, nerve, latent, reactivate
Pathogenesis of Herpes Simplex 1
-Inoculation of ___ _ at mucosal surfaces or skin sites → virus enters _________, dermis, and sensory/autonomic ____ endings → virus lives ______ in nerve cell bodies in ganglion neurons → can ______
Gingivostomatitis, lesions, exudate, fever, child
Symptoms of the Initial Episode of Herpes Simplex 1
-____________ and pharyngitis: ______ on the gums, buccal mucosa, soft palate, and tongue
-Lip lesions
-Pharyngeal edema, tonsillar _________, ulcerative lesions
-_____, malaise, myalgias, cervical lymphadenopathy
-Usually infected as a ______

Acyclovir, lidocaine
Treatment of Initial Episode of HSV 1
-Antiviral meds: __________ or valacyclovir started within 72 hours
-Topical analgesics: viscous _________
Herpes Labialis
vesicular growths on the lip due to the reactivation of herpes simplex 1 (HSV 1)

burning, vesicle, ulcer, lip, multinucleated, cultures
Symptoms and Diagnosis of Herpes labialis
-Initial ________/itching/tingling → ________ → rupture → superficial _____ (erythematous base) → scabs
-Occurs most commonly along the vermillion border of the ___
-Diagnosed via the Tzank smear, which reveals ____________ giant cells. You can also use viral cultures, PCR, IgG and IgM
spontaneously, antivirals
Treatment of Herpes labialis
-Typically ___________ resolves within 2 weeks
-Use _________ like acyclovir and valacyclovir, most effective when started within 24-48 hours of onset
Squamous, males, tobacco, larynx, pharynx
Epidemiology, Risk Factors, and Symptoms of Malignancies of Larynx/Pharynx
-___________ cell carcinoma is the most common
-Seen more often in ______ in the 6th and 7th decade of life
-Smoking, chewing _______, and alcohol use are the biggest risk factors
-________: hoarseness, weight loss, odynophagia, hemoptysis, vocal cord immobility
-________: ear pain, 5th and 6th CN involvement, nose bleeds, and nasal obstruction
biopsy, METs, resection
Diagnosis and Treatment of Malignancies of Larynx/Pharynx
-Direct laryngoscopy to perform a _______
-CT or MRI to determine tumor extent, PET scan to assess _____
-________, radiation, and chemotherapy are the current treatments
Gingivitis (Periodontal disease)
inflammation of the gums

poor, dry, risk, bacteria, acid, gums, loss
Risk Factors and Pathophysiology of Gingivitis
-______ dental hygiene, ___ mouth, poor nutrition, smoking, age, and certain medications
-______ factors → plaque buildup → increase in ______, which produce _____ → plaque hardens turning into tartar or calculus → irritation of the gumline → inflamed ____ → periodontitis and tooth ____
bleeding, edema, 3, flossing, twice
S/S, Diagnosis, and Treatment of Gingivitis
-________ gums, receding gumline, halitosis, _____/erythema of gums, tender gums
-Diagnosed by a dentist, noting pocket depth > _ mm
-_________ daily, regular dental checkups, and brushing _____ daily
hygiene, water, sugar, bacteria, acid, cavity
Risk Factors and Pathophysiology of Cavities
-Poor dental _______, lack of fluoride in the ______, and diet high in ______
-Risk factors → increase in _______ on the tooth → bacteria produce ____ → acid destroys the enamel → tooth decay and dental ______
sensitivity, white, dark, filling
S/S, Diagnosis, Treatment, and Prevention of Cavities
-Most asymptomatic, toothache, hot/cold __________, ______ spot early on develops into a _____ spot or hole.
-Diagnosed by the dentist
-First line treatment is _______ and root canals/crowns in severe decay
-Prevention: daily flossing, brushing twice daily, regular dental exams

Dental Abscess
a bacterial infection that can be found by a tooth root, where the bacteria multiplies and accumulates pus
-most commonly caused by cavities

bacteria, pus, Bacteroides, pulp
Risk Factors and Pathophysiology of Dental Abscess
-Same risk factors as cavities, making them the most common cause
-_________ enters tooth via cavity/crack and travels down the root → bacteria continues to multiply leading to accumulation of ___
-____________ is the most common bacterial cause
-If the abscess invades the dental ____, there will be complications in the surrounding neurovascular structures and tissues

tooth, swelling, exam, amoxicillin-clavulanate, endocarditis, jaw
S/S, Diagnosis, Treatment, and Complications of Dental Abscess
-Toothache, ______ sensitivity, gum and facial ______, +/- fever, +/- lymphadenopathy
-May see on the oropharynx _____. Best way to see it is a dental x-ray
-Treated with antibiotics (PCN such as ___________-_________) or I&D
-Complications: invasion of other structures, _________, sepsis, osteomyelitis of the ___
Endocarditis
People with heart issues are often prescribed antibiotics before having a dental procedure because of their risk of developing ____________
viruses, gonorrhea, chlamydia
Etiology of Pharyngitis/Tonsilitis
-Most common cause are __________, followed by group A beta hemolytic strep (Strep Pyogenes)
-Mycoplasma
-STDs like __________ and ________ can also cause pharyngitis/tonsilitis

fever, exudate, oropharynx
Symptoms of Group A Beta Hemolytic Strep Tonsilitis/Pharyngitis
-_____
-Tender anterior cervical adenopathy
-Pharyngotonsillar _______, not as common as people may think
-Erythematous ____________, which causes a severe sore throat
-Palatial petechiae, which are bright red dots around the uvula and soft palate

Centor Criteria
If you are unsure of if you should test a patient for strep, you can use the _______ _______ to decide. The patient must meet > 3 criteria, which include:
Tonsillar exudate
Tender anterior cervical LAD
Fever
Absence of cough
Rapid, culture
Diagnosis of Group A Beta Hemolytic Pharyngitis/Tonsilitis
-Centor criteria (meet >3 criteria)
-______ strep test is the best initial test, usually go straight to this in practice
-Throat _______ is the gold standard, do if rapid strep test was negative or if the patient is higher risk
PCN V, cephalosporins, supportive
Treatment of Group A Beta Hemolytic Strep Pharyngitis/Tonsilitis
-Benzathin PCN G IM once, usually to treat rheumatic fever
-Oral ___ _ is the 1st line therapy, but amoxicillin is okay
-If the patient has a PCN allergy, prescribe ___________ like Cephalexin
-_________ care is also a suggestion: analgesics, salt water gargles
secondary, fever, myocarditis, abscess
You want to adequately treat Group A Beta Hemolytic Strep to avoid _________ illness such as scarlet _____, rheumatic __________, glomerulonephritis, and local _________ formation
Scarlet Fever
a complication of GABHS pharyngitis/tonsilitis characterized by a strawberry tongue, fine “sandpaper” rash

Rheumatic Fever, kidneys, abscess
Complications of GABHS Pharyngitis/Tonsilitis
-Scarlet Fever: strawberry tongue, fine “sandpaper” rash
-_________ ____: Jones Criteria, 2 major or 1 major and 2 minor
-Post-streptococcal glomerulonephritis: edema, hematuria, HTN, affects the _________
-________: peritonsillar or retropharyngeal
Recurrent, tonsilitis, 6-7
Adults get tonsillectomies largely due to infectious disease. The most common reason is _______, acute ________, with more than _-_ episodes in 1 year, 5 episodes per year for 2 years, or 3 episodes per year for 3 years (Strep)
laser, hemorrhage, injury
Techniques and Complications of Tonsillectomy
-Electrocautery, sharp dissection, _______, radiofrequency ablation
-Pain, __________ (most common), dental _______, TMJ dislocation, cautery burns
Infectious Mononucleosis
infection commonly caused by EBV/CMV associated with strep co-infection
-most often in kids/teens spread through intimate contact
Mononucleosis Triad
Fever, lymphadenopathy, pharyngitis
exudate, posterior, splenomegaly, laceration
Symptoms of Infectious Mononucleosis
-Malaise, fever, fatigue
-Severe sore throat with _________
-_________ cervical lymphadenopathy
-_____________ in 50-60% of patients, starts to resolve around 3rd week of illness. _________ is the most emergent complication of this, so tell patient to avoid contact sports for 4 weeks.

atypical, Monospot, symptomatic, 4 weeks, rash
Diagnosis and Treatment of Infectious Mononucleosis
-Mostly by physical exam
-CBC reveals ______ lymphocytes, elevated LFTs, EBV antibody titer
-__________ or Heterophile Antibody Test (test of choice)
-____________ treatment (fluids, rest, analgesics): tell them it will take weeks to feel better
-No physical activity for at least _ _____ to avoid splenic rupture
-Antibiotic if co-infection with strep, can cause ____ with Ampicillin/PCN being the most common culprit
Peritonsillar cellulitis
infectious, inflammatory reaction of the tissue between the tonsillar capsule and the pharyngeal muscles
NOT ASSOCIATED WITH PUS COLLECTION
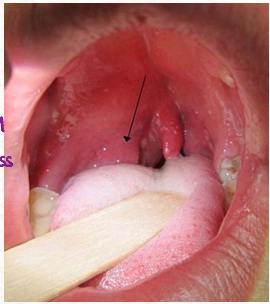
Peritonsillar abscess
collection of pus located between the tonsillar capsule and the pharyngeal muscles, most common deep neck infection
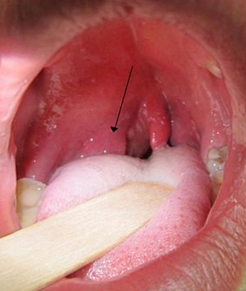
tonsilitis, strep, severe, medial, uvula, muffled, trismus
Etiology and Symptoms of Peritonsillar Abscess/Cellulitis
-Any microorganism that causes _________, most commonly bacteria (group A _____, staph aureus)
-________ sore throat, _____ deviation of soft palate which pushes the arches and makes it asymmetric
-Deviation of ______, ________ voice, fever, odynophagia
-_________, which is the inability to open their mouth due to irritation of pterygoid muscles
not, culture, US, contrast
Diagnosis of Peritonsillar Abscess/Cellulitis
Laboratory and imaging eval (often ___ necessary):
-CBC, lytes, throat culture, gram stain and _______ of abscess fluid
-Intraoral or submandibular __ to differentiate between PTA and cellulitis
-CT with IV ________ if concerned about retro or parapharyngeal abscess
amoxicillin-clavulanate
In patients with less severe peritonsillar abscesses/cellulitis, the DOC is oral __________ ________. These patients have a stable, patent airway and can handle oral fluids
Ampicillin, vancomycin, needle, sepsis
Treatment of Peritonsillar Abscesses/Cellulitis
-Less severe: oral amoxicillin-clavulanate or clindamycin for 14 days, will see improvement in patients with cellulitis but not an abscess
-Moderate to severe: IV ___________-sulbactam or clindamycin. If those drugs fail, IV _________ or linezolid should be administered.
-Surgical management: ________ aspiration is preferred, but you could perform and I&D or refer out for a tonsillectomy
-Infection can spread to other deep neck spaces, adjacent structures and eventually the bloodstream, which causes _______
Retropharyngeal Abscess
abscess found in the retropharyngeal space, posterior to the pharynx and extending from the base of the skull to the mediastinum
-develops secondarily from spread of oropharynx/oral infections of pharyngeal trauma, common pathogens are streptococci and staphylococcus
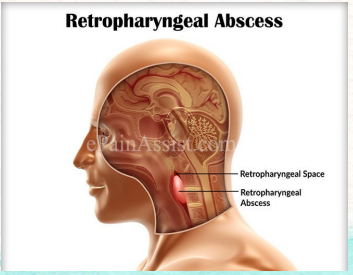
neck, rigidity, posterior, cervical, CT, cultures
Symptoms and Diagnosis of a Retropharyngeal Abscess
-Sore throat, fever, _______ stiffness/pain (nuchal ________)
-Sometimes stridor, toxic appearance
-________ pharyngeal edema
-Trismus, _________ adenopathy, and torticollis
-__ of neck and blood _______ are the common tools used to diagnose this
airway management, IV, mouth, ear, sinus, aspiration, mediastinitis
Treatment and Complications of Retropharyngeal Abscesses
-_______ __________ is the first line of treatment. Once that has been managed, emergently refer/consult to ENT
-Usually hospitalized for observation and __ antibiotics
-An infection where the ______ was the source, the patient will likely be treated with ampicillin-sulbactam/ceftriaxone + metronidazole/clindamycin + levofloxacin
-An infection where the ___ was the source, the patient will likely be treated with cefepime + metronidazole or piperacillin-tazobactam
-An infection where the ________ were the source, the patient will likely be treated with vancomycin + ampicillin-sulbactam/vancomycin + ceftriaxone + metronidazole/ clindamycin + levofloxacin
-Needle _______ or I&D to remove the abscess
-Can lead to airway obstruction, _________, sepsis, jugular venous thrombosis, and erosion of the carotid artery
Ludwig’s Angina
cellulitis of the sublingual and submaxillary spaces often arising from infection of the mandibular dentition, bilateral
-most often arises from a dental infection, caused by normal oral flora
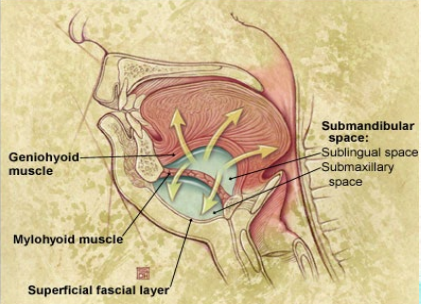
edema, chin, floor, displaced, occlusion
Symptoms of Ludwig’s Angina
-______ and erythema across submandibular area. Found mostly on the upper neck under the _____ and the ______ of the mouth
-Tongue may be ________ upward and backward
-Neck pain, stiffness
-Fever, chills, malaise
-Can lead to ________ of airway

clinical, CT, culture, airway management, antibiotics, vancomycin
Diagnosis and Treatment of Ludwig’s Angina
-Usually ______ but __ is the imaging of choice. Blood cultures, gram staining, and a pus ________ are common too.
-________ _______ is the most important step in treatment. Follow this up with IV ________: ampicillin-sulbactam or ceftriaxone + metronidazole. If the patient has a penicillin allergy, prescribe clindamycin + levofloxacin. If you are concerned about MRSA, give ___________ too
-I & D
Laryngitis
inflammation of the larynx, most common cause of hoarseness
-usually viral (M. catarrhalis, H. influenzae)
hoarseness, rest, bacterial, corticosteroids, laryngoscopy
Symptoms and Treatment of Laryngitis
-___________ may persist for a week or so after URI symptoms have cleared. Usually only lasts for a few days.
-Voice _____, antibiotics if __________, and oral/IM ____________ if the patient works in a job that requires a lot of speaking
-Any patient with hoarseness that has persisted beyond 2 weeks should be evaluated by an ENT with _____________ to rule out malignancies
Sialolithiasis/Adenitis
salivary stones or back up of the salivary glands, usually occurring in the parotid, submandibular (most common), and sublingual glands

Dehydration, smoking, pain, eating, stone, fluids, massage, tart/sour
Risk Factors, Symptoms, and Treatment for Sialolithiasis/Adenitis
-_________, diuretics, anticholinergics, trauma, hx of gout or nephrolithiasis, ________, and chronic periodontal disease
-______ and swelling in the involved gland. Usually aggravated by _______. May palpate or see ____ in duct
-_______, moist heat, gland and duct _________, such on ____/_____ candies (1st line): sialogogues, analgesics, and antibiotics if concern for infection

Suppurative Parotitis
acute infection of the parotid gland, most commonly in elderly postoperative patients who are dehydrated or intubated
-other risk factors include recent intensive teeth cleaning, use of drugs that reduce salivary flow
-staph aureus
stasis, Stensen’s, unilateral, parotid, toxic, Mumps
Pathogenesis and Symptoms of Suppurative Parotitis
-Salivary ______ → retrograde seeding of ___________ duct by oral flora
-________, firm, erythematous, swollen preauricular area (over the ________ gland), fever, may appear ______
-______: common cause of bilateral parotid gland swelling but can cause unilateral swelling

Ultrasound, amylase, antibiotics, abscess
Diagnosis and Treatment of Suppurative Parotitis
-__________ is imaging of choice (CT as supplement), serum ________ will be elevated, and gram stain/cultures can be done
-Admit for IV ________ and hydration: ampicillin-sulbactam is a common course of treatment
-Aspiration or I&D if _______ forms

TMJ Disorder
acute or chronic inflammation of the TMJ secondary to trauma, repetitive jaw movement, or malocclusion of teeth
pain, clicking, ear, NSAIDs
Symptoms and Treatment of TMJ Disorder
-_______, joint _______/popping. Sometimes the patient will complain of ____ pain
-Oral _______ are the first line treatment. PT, surgery, trigger point injections, and botox injections are other potential treatment options