Pulmonology: Respiratory Illnesses
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
Acute Bronchitis
- Respiratory virus (MCC)
- MCC of hemoptysis besides lung cancer
- 1-3 weeks
Presentation: winter months, respiratory viruses, cough, afebrile, rhonchi that clear w/ coughing
No CXR indication
RSV (includes all info, esp. what type of virus and vaccine schedule)
- Paramyxovirus
- Leading cause of bronchiolitis (inflammation of the small airways in the lung) and pneumonia in children under 1
Risk Factors: infants under 6 mo, infants under 1 yr who were premature or exposed to 2nd hand smoke
Transmission: direct contact w/ inoculation of mucous membranes (eye to mouth type)
Sx:
- URI: rhinorrhea, watery eyes, pharyngitis
- LRI: cough, SOB, wheeze
Dx: PCR
Tx: supportive (O2, Tylenol), very sick: antivirals like ribavirin or IVIG
Vaccine: all infants born in cold/flu season or entering their first cold/flu season receive a dose, pregnant moms sept-jan 32-36 weeks, at risk 60+, everyone over 75
Acute Bronchiolitis (who is most at risk?)
- Inflammatory processes that affect the bronchioles, COPD-like rxn
- MCC in 2 mo to 2 yrs= RSV
- URI prodrome LRI: like a cold to bam very bad days 3-5 (wheezing, cyanosis)
o Pulse ox a good indicator in kids
Dx= clinical
Tx: supportive (O2, hydration, antipyretics)
- Premature babies or underlying immunodeficiency or heart/ lung disease: Palivizumab (monoclonal antibody)
Croup (type of virus, indicative sign, treatment)
- Caused by a parainfluenza virus, leads to upper air way obstruction due to larynx, trachea and bronchi swelling inspiratory stridor, hoarseness, barking cough
- Clinical Dx
- Steeple sign on CXR from laryngeal narrowing
Dexamethasone, nebulized epinephrine in severe cases
Pertussis: What causes it?
- Caused by Bordatella pertussis, gram – aerobic encapsulated coccobacillus
Pertussis: 3 phases
1. Catarrhal: 1-2 weeks of non-specific malaise, rhinorrhea, cough, lacrimation
2. Paroxysmal: 2-3 months of paroxysmal (episodic) cough and whooping, often with proceeding emesis, may be worse at night
3. Convalescent: 1-2 weeks of gradual decrease in frequency and severity
Pertussis: diagnosis
- First 2 wks of sx: culture from nasopharyngeal swab or PCR blood sample
- More than 4 weeks: serum PCR
- Can be clinical (with such a characteristic cough)
- Elevated white counts
Pertussis: treatment and vaccination
Tx:
- Macrolides w/I 3 weeks of sx onset, use Bactrim if allergic
Vaccination
- Peds: 5 doses DTap (w/ diptheria and tetanus)
- 11-18 y/o: Tdap booster
- One dose Tdap recommended: 19+ w/o adolescent booster, pregnant moms
What are the types of influenza?
- Influenza A (typically more severe), influenza B (typically less severe, more GI sx)
o Contain hemagglutinin and neuraminidase on their surfaces (think H1N1)
How is influenza transmitted? What is the incubation period? What are the contagious periods?
Transmission: respiratory droplets w/I 6 feet
Incubation: 2 days, quicker in the unvaccinated
Viral shedding/contagious period:
- 24-48 hours before sx start to 1 week after symptoms start
- Can be basically immediately
- More sick= more contagious
- Return to life… 24 hours w/o fever w/o antipyretics
What are flu sx? What is a severe complication of the flu? What are two causative agents of that complication?
Sx: fever, chills, aches, fatigue, confusion, pharyngeal erythema, mild cervical adenopathy
( can be mild to severe)
Complication: Pneumonia
- Higher risk in those over 65, immunocompromised, comorbidities
- Secondary bacterial pneumonia
o MC= pneumococcal pneumonia
o Staph aureus= most serious
When do we test for the flu? How?
- Only test when it will impact treatment (hospitalization, underlying disease, comorbidities)
- Testing Types:
o Gold standard: PCR (not realistic)
o Most common/preferred: nucleic acid amplification tets (NAAT), can distinguish A and B
o RIDT and viral culture: less common
Describe influenza treatment and the 48 hour guidelines
- Give neuraminidase inhibitor: oral oseltamivir (Tamiflu) w/I 48 hours of Sx
- After 48 hours, give if
o Hospitalized
o Severe or high risk
o Healthcare workers
o Household w/ high risk
- Can administer tamiflu prophylactically in ages over 1 in high risk groups 1-2 weeks after exposure: daycare, LTC, hospitals to PREVENT OUTBREAKS
- Have mRNA synthesis inhibitor (zofluza) way less commonly used
Describe vaccination criteria and types for influenza
- Every 6 months and older w/o contraindications by end of October, annually
o NOT egg allergy (used to be but not anymore)
o History of guillian barre syndrome w/I 6 weeks of previous influenza vax
o Younger than 6 mo
o Severe allergic rxn
- Kids 6mo-8y/o w/ first flu vaccine: get a second dose 28 days later (also if previously they only got 1 dose in the past)
Vaccine types:
- Inactivated influenza vaccines (IIVs, fluzone): egg based, quadrivalent (2 forms of A, 2 forms of B), use trivalent when quad is unavailable (2 and 1)
- Recombinant influenza vaccine (RIV4): Flubok, 18+, flu proteins
- Live attenuated influenza vaccine (LAIV): flumist non-pregnant, 2-49y/o
o NO FLU MIST: not 2-49, under 5 w/ history of asthma/wheezing, pregnant, immunocompromised (could make them sick)
What is TB? How is it spread? Where does it go in the body?
- Mycobacterium tuberculosis, acid-fast bacillus
- Leading cause of death worldwide from an infection
Spread: aerosolized microdroplets, longer exposure= more likely to get it
Location: MC is lungs, larynx 2nd, can go basically anywhere in the body
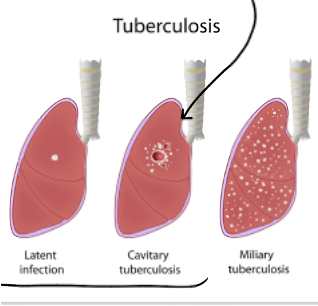
Differentiate active/latent TB and primary and secondary infections.
Primary disease: rapid progression from getting infected to having active disease
- Located in middle/lower lobes
Secondary/REACTIVE disease: disease onset after latency
- Tends to be in the apex of the lungs
Active TB: immune system is not containing TB infection, causing symptoms, infectious
Latent TB infection: infected w/ TB but not infectious to others, asymptomatic, immune system is containing the infection
What is the pathophysiology of a TB infection? Describe 3 places it may manifest and the specific disease name.
in fection causes delayed HS reaction type IV, creating caseating (central necrosis) granulomas, can do to any organ
o Scrofula: TB in cervical lymph nodes
o Pott disease: TB in vertebrae
o Miliary TB: no central necrosis
Tb Diagnosis
- Imaging CXR (diff location-middle/lower vs upper, miliary looks different)
- 3 sputum samples on 3 consecutive days for
o Acid-fast bacilli staining (rapid, inexpensive)
o Culture (takes weeks)
o NAAT (48 hours)
- +NAAT=TB, -NAAT= cannot exclude TB, wait on culture
TB Screening
o Mantoux tuberculin skin test (PPD)
§ Read 48-72 hours later, measure size of induration (bubble) not redness
o TB Gold Assay Blood Test:
§ Do if they’ve had the vaccine
o GET CXR if either are positive
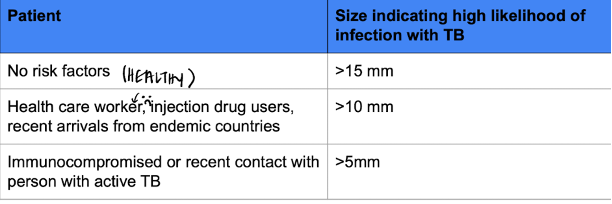
When is a TB skin test contraindicated?
When someone has had the vaccine (endemic countries)
Treatment of latent TB
- If we find latent TB (positive PPD, normal CXR)
o 3-4 months of rifampin plus or minus isoniazid
o OR less preferred: isoniazid and B6 for 9 months
Treatment of Active TB
- ACTIVE TB: AFB or NAAT +
o Respiratory isolation for 2 weeks, observe medication taking
o RIPE treatment
§ Rifampin (red secretions) 6 mo
§ Isoniazid 6mo
· Inhibits vitamin B6 neuropathy B6 supplement
· Hepatitis or neuropathy
§ Pyrazinamide 8 weeks
· Hepatitis or hyperuricemia (NOT IN PREGNANT WOMEN-DO OTHER 3 FOR 9MO INSTEAD)
§ Ethambutol 8 weeks
· Optic neuritis (E=eyes), neuropathy