Male Genitalia Pathology
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
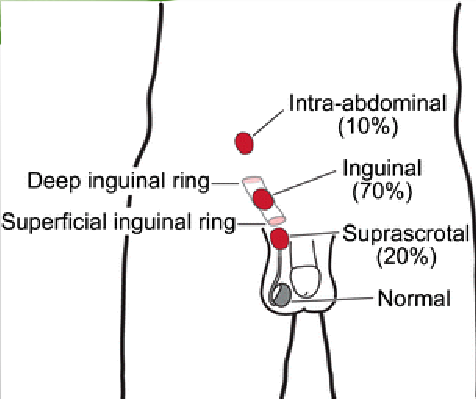
what is the Complete or partial failure of testes to descend into scrotal sac?
CRYPTORCHIDISM
• Unilateral in most cases, 25% bilateral
• Asymptomatic
cryptorchidism descent of testes occurs in 2 phases. what are the 2 phases?
phase 1: abdomen to lower pelvis by the 3rd month of gestation
phase 2: inguinal canal to scrotum within the last 2 months intrauterine
in cryptorchidism, the testes may arrest anywhere along the pathway of descent but the most common site is…?
inguinal canal
when can cryptorchidism be diagnosed?
Diagnosis can only be established with certainty after 1 year of age because descent is not always complete at birth
what cases of cryptochordism can cause sterility?
bilateral (as undescended testes become atrophic)
can still be sterile if unilateral (atrophy of descended gonad can also occur)
in cryptochordism there is a 3-5x increased risk for what type of cancer?
testicular (even if unilatera, contralateral testis is also at risk)
what is the treatment for cryptochordism?
Can be corrected with surgery
Recommended by 18 months to decrease likelihood of atrophy, infertility, and testicular cancer
where is inflammation of testes most common?
More common in epididymis than in the testis proper (esp gonorrhea and TB)
what STD affects the testis first?
syphilis
what causes epididymitis in childhood?
congenital abnormality or infection with gram-negative rods
what causes epididymitis in men under 35?
sexually transmitted gonorrhea & chlamydia
what causes epididymitis in men over 35?
urinary tract pathogens- E. coli & pseudomonas
what is the inflammation of 1 or both testicles?
orchitis
what can cause orchitis?
mumps (20-30% of cases)
Nonspecific epididymitis and orchitis usually begin as ____ that spread to the testes via the ______
UTI; spermatic cord
is sterility possible in orchitis?
yes
what is a systemic viral infection that commonly affects school aged children?
mumps
is testicular involvement common in children with mumps?
no (post puberal males get orchitis more often)
viral orchitis from mumps develops 1 week after what initial symptom?
swelling of parotid glands
how is mumps virus transmitted?
saliva and respiratory droplets
testicular tumors occur in __ per 100,000 males
6
what are the 2 main categories of testicular tumors?
germ cell tumors
seminomas
non-seminomatous
sex-cord-stromal tumors
what category of testicular tumor is described below?
Arise from Sertoli and Leydig cells
Uncommon
Usually benign
sex-cord-stromal tumors
what category of testicular tumor is described below?
95% of testicular tumors in post-pubertal males and almost all are malignant
Family hx. is important
Brothers of patients have an 8-10x increased risk
Lifetime risk is highest in Northern Europe and New Zealand and lowest in Africa and Asia
germ cell tumors
what is the most common type of germ cell tumor?
seminoma (50% of all germ cell neoplasms)
what sub-category of germ cell tumor is described below:
• Malignant
• Never occurs in infants
• Peak incidence-4th decade
• Produces bulky mass
• Gross appearance → Homogenous, gray-white cut surface
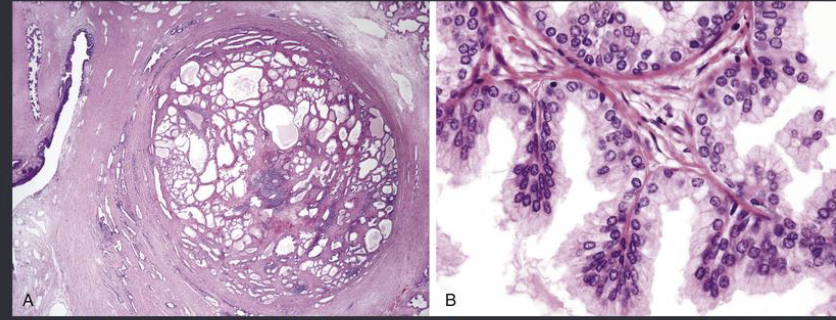
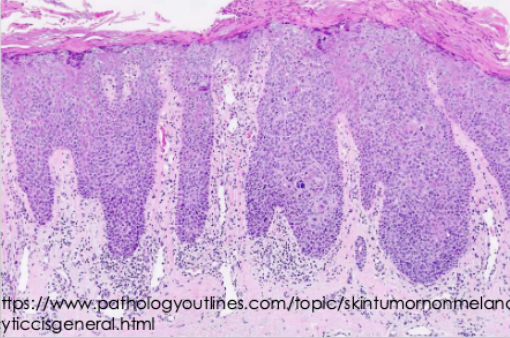
seminoma
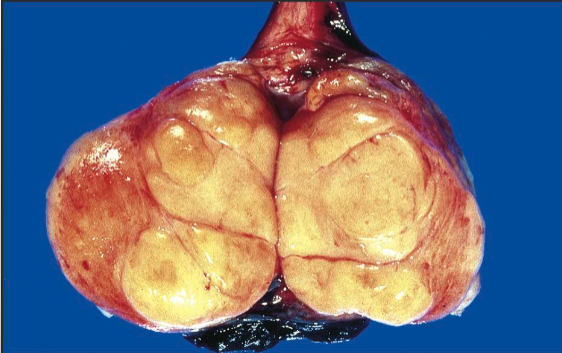
seminoma
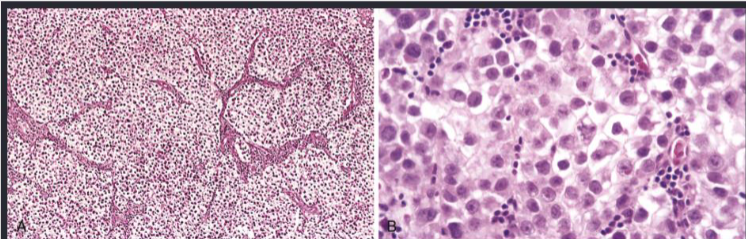
• Histopathology of SEMINOMA → Cells are large and round with distinct cell membrane, large central nucleus with prominent nucleo
what is the most common testicular tumor in infants and children up to 3 years old?
yolk sac tumor (but good prognosis in this age group)
what is a malignant, non-seminomatous germ cell tumor?
yolk sac tumor
Post pubertal yolk sac tumor more frequently occurs in combination with …?
embryonal carcinoma or other germ cell conditions
in yolk sac tumors, there is an increased/decreased serum alpha fetoprotein
increased
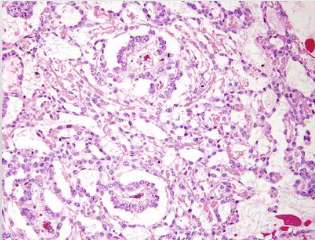
yolk sac tumor
• Have Schiller-Duvall bodies (resemble primitive glomeruli)
what are the 2 types of sex-cord tumors?
Leydig cell tumor
Sertoli cell tumor
what sub-cateogry of sex-cord tumors is described below?
• Occurs between ages of 20-60
• 5-10% are malignant
• Testicular swelling and/or gynecomastia
• Increase in androgens, estrogens, corticosteroids
Leydig cell tumor
what sub-cateogry of sex-cord tumors is described below?
• Presents as a testicular mass
• Can have gynecomastia as initial finding
• Up to 10% can be malignant
Sertoli cell tumor
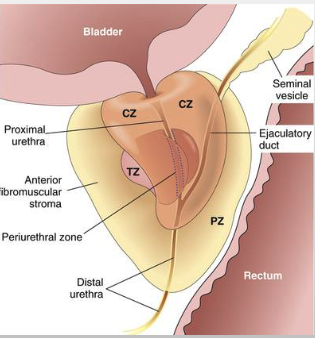
what are the 4 zones of the prostate gland?
• PZ = PERIPHERAL ZONE
• TZ = TRANSITIONAL ZONE
• CZ = CENTRAL ZONE
• PUZ = PERIURETHRAL ZONE
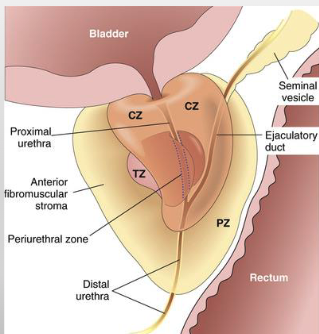
in which zone of the prostate gland do most hyperplastic lesions occur?
transitional zone
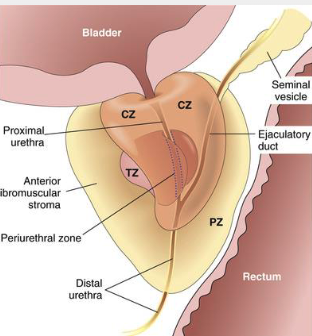
in which zone of the prostate gland do most carcinomas occur?
peripheral zone
what is the most common bacteria that causes prostatitis?
E. coli
acute or chronic prostatitis?
• Can cause urinary tract infections
• Associated with fever, chills, dysuria
• Prostate is tender & boggy
acute
acute or chronic prostatitis?
• Usually associated with recurrent urinary tract infections bracketed by asymptomatic periods
• Presenting symptoms include low back pain, dysuria, and perineal and suprapubic discomfort
chronic
both acute and chronic prostatitis is treated with…?
antibiotics
the following are signs of what type of prostatitis?
• Signs and symptoms same as chronic bacterial
• No history of recurrent urinary tract infections
• Etiology is unknown, unsure if prostate is even related
• Prominent finding - pain during or after ejaculation
• Diagnosis of exclusion
Chronic abacterial prostatitis (Chronic pelvic pain syndrome)
what does diagnosis of exclusion mean?
a medical diagnosis made when all other possible causes of a patient's symptoms have been ruled out
histologic evidence of benign prostatic hyperplasia (BPH) is found in up to % of men by the age of 80
90%
benign prostatic hyperplasia (BPH) is a common cause of ….?
prostate enlargement and urinary obstruction
benign prostatic hyperplasia (BPH) can be a proliferation of what structures?
stromal or glandular strucutres
is benign prostatic hyperplasia (BPH) premalignant?
not premalignant
the etiology of benign prostatic hyperplasia (BPH) is unknown but studies show _________ may play a role
androgens (DHT-androgen derived from testosterone)
in which zone of the prostate does benign prostatic hyperplasia (BPH) begin?
transition zone (but can encroach on lateral walls of urethra to compress slit-like orifice)
what are symptoms of benign prostatic hyperplasia (BPH)?
increased urinary frequency
nocturia
dysuria
difficulty starting/stopping urinary stream
large discrete nodules on periurethral region leading to difficulty urinating are signs of…?
benign prostatic hyperplasia (BPH)
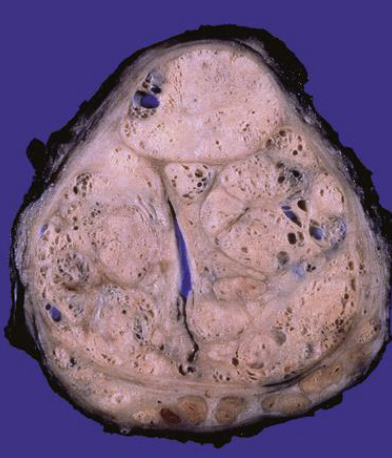
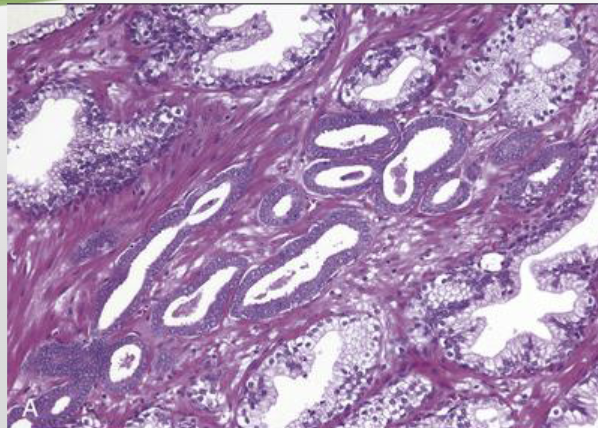
the following histopathology are signs of…?
• Hyperplastic acini
• Tightly packed, tall columnar epithelial cells with small basal nuclei
• Sometimes irregular papillary folds of epithelium
benign prostatic hyperplasia (BPH)
what is the most common cancer in men, but second in cancer-related deaths?
prostate cancer (adenomacarcinoma)
*side note: lung cancer is first in cancer-related deaths in men
does incidence of prostate cancer increase or decrease as one gets older?
increases (20%-in 50s, 70%-in 70s & 80s)
prostate cancer adenomocarcinoma arises in which zone of the prostate?
peripheral zone (posterior aspect)
*can be palpated on rectal examination
the following are various etiology of what condition?
• Age
• Race
• Family history
• Hormones
• Environment
• Androgens play role
prostate cancer adenomocarcinoma
the following describes the histopathology of what condition?
• Adenocarcinoma- glandular formation, lined by single layer of cuboidal or columnar epithelium
• Glands are smaller & crowded than benign prostate
• Basal cells not seen
prostate cancer adenomocarcinoma
how can prostate cancer adenomocarcinoma metastasize?
via lymphatics
via hematogenous spread (bone esp axial skeleton, mandible/maxila)
what are treatment options for prostate cancer adenocarcinoma?
surgery, radiation, hormonal manipulation
what can be measured to help with diagnosis and management of prostate cancer adenocarcinoma?
prostate specific antigen (PSA)
how is prostate cancer graded?
how well-differentiated the cells are
what congenital anomaly of penis is described:
Abnormal urethral opening on ventral surface of penis due to malformation of urethral groove/canal
Hypospadias
what congenital anomaly of penis is described:
Abnormal urethral opening on dorsal surface of penis due to malformation of urethral groove/canal
Epispadias
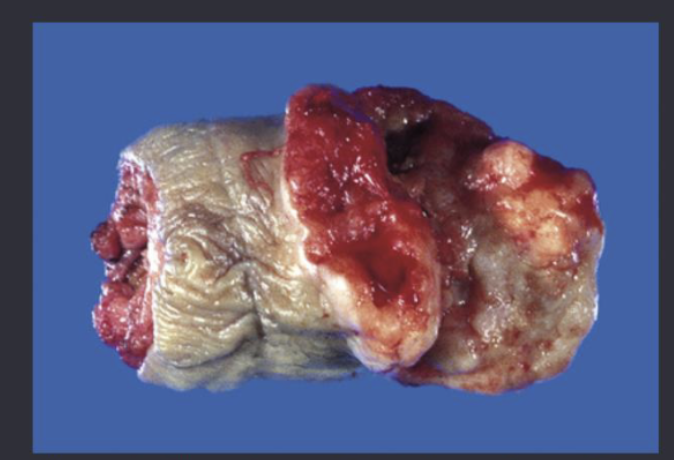
prostate cancer
Abnormal openings of the penis are sometimes constricted resulting in urinary tract obstruction and increased risk of ___
UTIs
congenital anomalies of the penis like hypospadias and epispadias can be associated with other congenital abnormalities like…?
failure of normal descent of testes
inguinal hernia
what condition is described:
local inflammation of glans penis
balantiis
what condition is described:
local inflammation of overlying prepuce
balanoposthitis
balantiis and balanoposthitis are caused by…?
candida albicans
anaerobic bacteria
pyogenic bacteria
most cases of balantiis and balanoposthitis are a result of…?
poor hygiene in uncircumcised males
what is the accumulation of desquamated epithelial cells, sweat, debris?
smegma
what are the 2 types of penile intraepithelial neoplasia? (carcinoma in situ of penis)
Undifferentiated penile intraepithelial neoplasia
Differentiated penile intraepithelial neoplasia
which type of penile intraepithelial neoplasia is associated with HPV?
undifferentiated (most commonly HPV 16)
is carcinoma in situ cancer?
no
cancer = cells where they are NOT supposed to be
carcinoma in situ = abnormal cells but where they are supposed to be
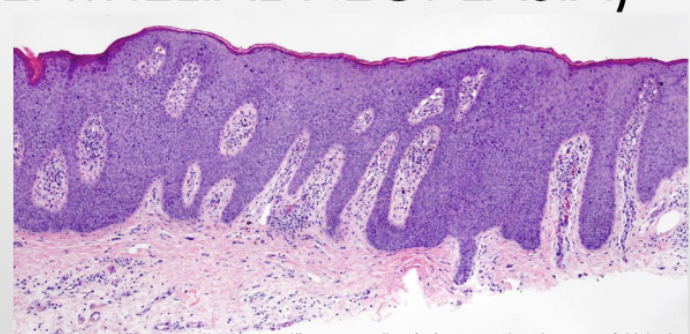
squamous cell carcinoma
is squamous cell carcinoma common in the US?
no (uncommon only 0.4% of all cancers in males)
most cases of squamous cell carcinoma are in what groups of men?
uncircumcised
what are risk factors of squamous cell carcinoma?
• Poor genital hygiene
• Infection with HPV, especially high-risk types 16 and 18
• Most pts are over 40
• Cigarette smoking elevates risk
the following describes what condition:
• Slow growing; affects glans penis or prepuce
• Asymptomatic until ulcerated
• May have cauliflower appearance, can be ulcerated
• Metastasis to inguinal lymph nodes can occur early on
squamous cell carcinoma
the following describes what condition:
• Involves sexually active adults
• Affects younger age than Bowen disease
• Presents as multiple, reddish-brown papules
• Small number may transform into SCC
• Usually regresses spontaneously
Penile high grade squamous intraepithelial lesion
the following describes what condition:
• Affects older males
• Affects shaft or scrotum
• Presents as solitary, thickened gray-white plaque
• 10% can transform into squamous cell carcinoma
Bowen disease
what are 2 types of undifferentiated carcinoma in situ of penis (penile intraepithelial neoplasia)?
penile high grade squamous intraepithelial lesion
Bowen disease
% of Bowen disease cases can transform into squamous cell carcinoma
10%