Microscopic Examination of Urine Part I
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
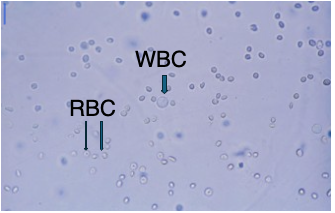
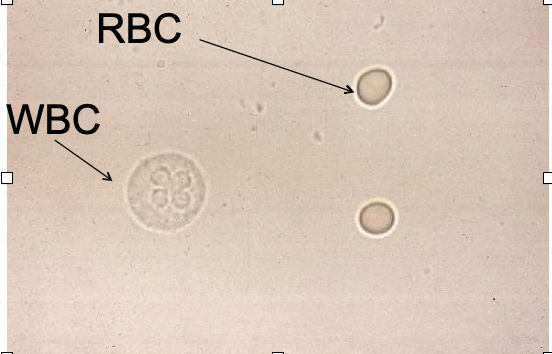
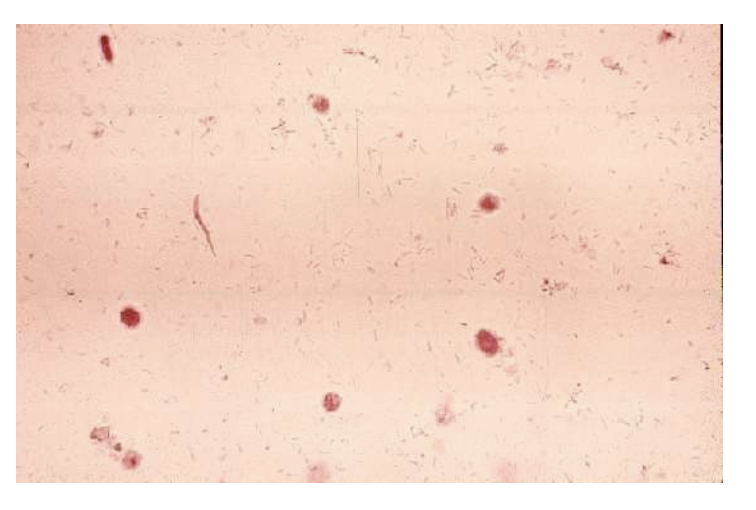
RBCs in Urine Microscopy
Size: ~7 μm; no nucleus
Normal range: 0–2 RBCs/hpf
In concentrated urine, RBCs appear small and crenated
Rarely seen unless there's contamination or pathology
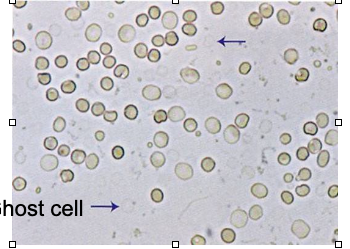
Ghost Cells in Urine
Seen in dilute (hypotonic) urine
RBCs swell and lyse, but membranes remain intact
Appear as empty, faint outlines
Do not count in RBC estimate — just note as “present”
Contextual note:
Ghost cells result from osmotic lysis and may indicate prolonged urine dwell time in hypotonic conditions. Their presence helps explain low RBC counts when hematuria is suspected.
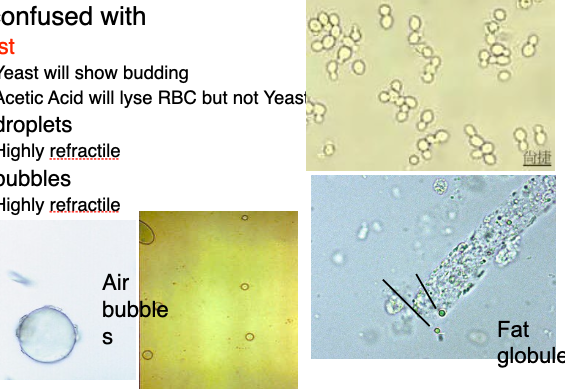
Red Blood Cells Confused with…
Yeast: Budding; resists acetic acid lysis
Oil droplets: Highly refractile, variable in size
Air bubbles: Refractile and shiny; vary in size
Fat globules: Persist with acetic acid; ID via Sudan III or polarized light
Confirmatory tip:
Add 1 drop of acetic acid to 1 drop of sediment — if RBCs disappear, blood was present. Yeast and fat will remain.
Hematuria Interpretation Pitfalls
Hematuria = RBCs in urine
Results may not match urine color or dipstick:
1–4 RBCs/hpf, strip may be negative (threshold ≈ 5+ RBCs/hpf)
Positive dipstick, no visible RBCs → likely lysed RBCs, Hgb, or Mgb
Contextual note:
Dipstick detects peroxidase activity, so free hemoglobin or myoglobin can trigger a positive even in the absence of intact RBCs on microscopy.
Crenated RBCs vs WBCs
Crenated RBCs: Shrink in hypertonic urine, appear granular
May be mistaken for WBCs, but are smaller in size
Acetic acid will lyse RBCs but not:
Yeast
Oil droplets
WBCs
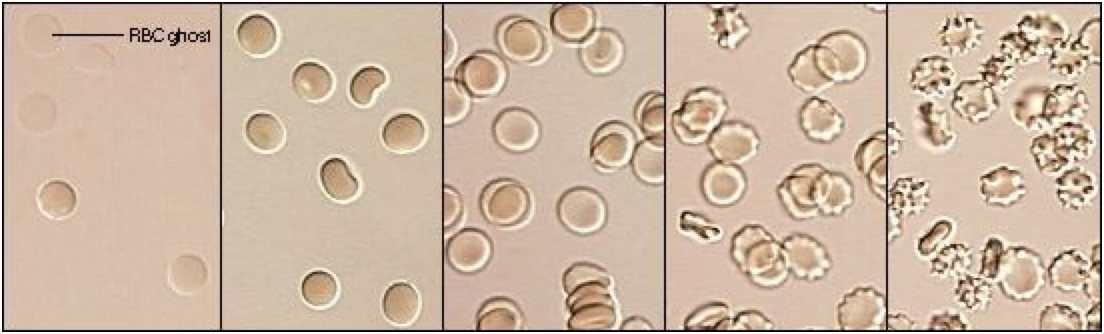
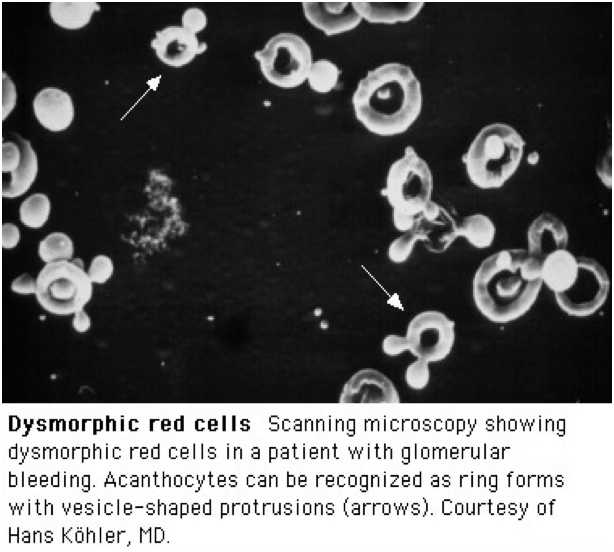
Dysmorphic RBC
Have cellular protrusions, variable size, may be fragmented
Suggest glomerular bleeding
Very rare finding; can occur post-strenuous exercise
Requires confirmation by a second MLS or technical specialist
WBCs in Urine Microscopy
Size: ~12 μm
Normal range: 0–5 WBCs/hpf
Usually neutrophils (PMNs):
Have granules and multi-lobed nuclei
Nucleus may be hard to see due to granules
WBCs in Varying Urine Osmolarity
Hypertonic urine:
WBCs shrink, may not degranulate
May yield false-negative leukocyte esterase strip test
Hypotonic urine:
WBCs swell → form glitter cells
Glitter cells show Brownian movement
Not clinically significant — just water-swollen WBCs
Pyuria
Defined as ↑ WBCs in urine
Indicates infection or inflammation in the genitourinary (GU) tract
Possible causes:
Bacterial infection
Glomerulonephritis
Lupus erythematosus
Interstitial nephritis
Tumors
Mononuclear Cells in Urine
Rare in routine urinalysis
Lymphocytes:
Small, may mimic RBCs
Seen in early renal transplant rejection
Monocytes, macrophages, histiocytes:
May appear vacuolated or contain inclusions
If large number of Mono nuclear refer to cytology
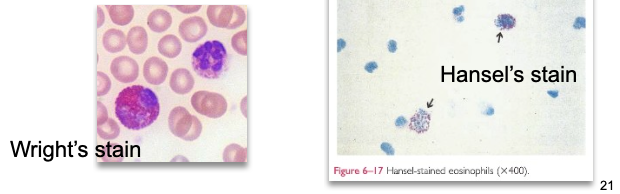
Eosinophils in Urine
Not normally present in urine
Significant if >1% of total WBCs
Visualized with Hansel’s or Wright’s stain
Associated with:
Drug-induced interstitial nephritis (most common)
UTIs
Parasitic infection (Schistosoma)
Renal transplant rejection
Epithelial Cells in Urine
Line the genitourinary tract
Three main types:
Squamous
Transitional
Renal tubular
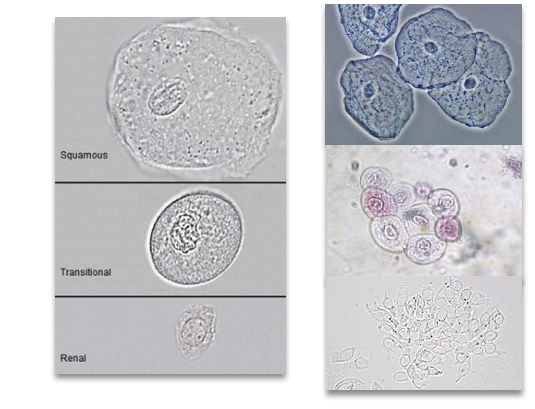
Squamous Epithelial Cells
Largest cells in urinary sediment
Prominent nucleus ≈ size of an RBC
Easily seen at 10X; may appear folded/clumped
Originate from vagina, female urethra, lower male urethra
No pathological significance — normal sloughing
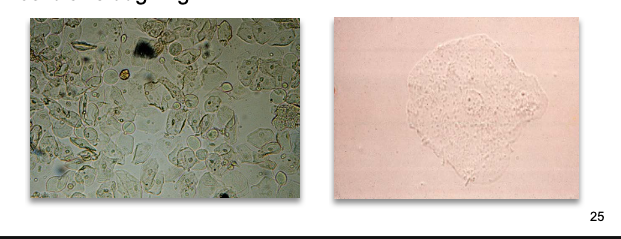
Clue Cells
Squamous epithelial cells coated with Gardnerella vaginalis
Appear granular and irregular
Indicative of bacterial vaginosis (when numerous)
Not typically reported on urine microscopy — seen on vaginal wet preps
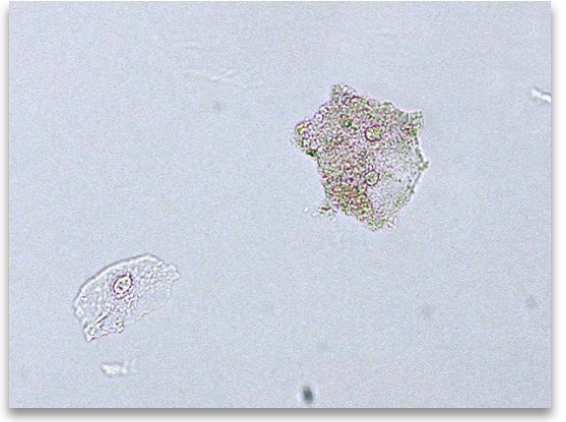
Transitional Epithelial Cells
Smaller than squamous, but slightly larger than RTE
Have centrally located nuclei
Appear in various shapes: spherical, polyhedral, caudate
Often have a well-defined edge
Can be difficult to distinguish from renal tubular epithelial (RTE) cells
Originate from the lining of the renal pelvis, calyces, ureters, and male urethra
increased amounts seen in catheterization
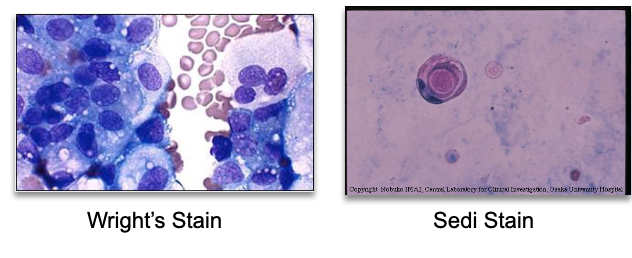
Abnormal Transitional Cells
Vacuoles or irregular nuclei may suggest:
Viral infection
Malignancy (e.g., bladder cancer)
Refer to cytology for evaluation
Stains: Wright’s or Sedi stain
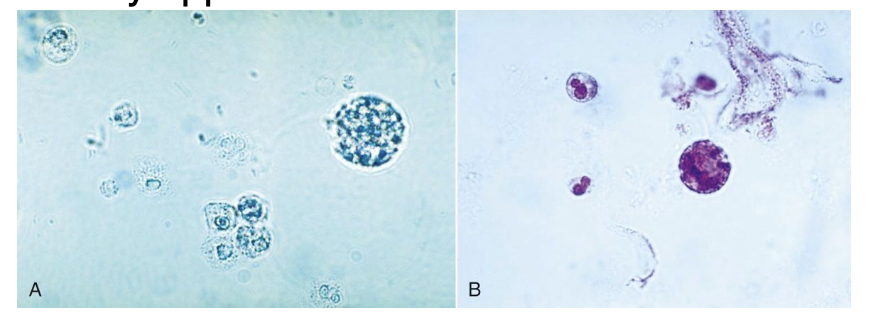
Renal Tubular Epithelial (RTE) Cells
Smaller than squamous, larger than WBCs
Shape: cuboidal, columnar, or round (often flattened edges)
Nuclei are typically eccentrically located
0–2/hpf = normal
>2/hpf = renal tubular damage or necrosis
Causes: infection, drug toxicity, heavy metals, allergic reactions
RTE’s reabsorb filtrate, therefor can take on various colors
bilirubin → yellow color
Hemosiderin → yllw-brn
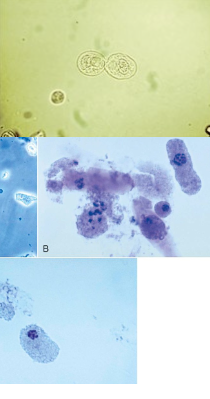
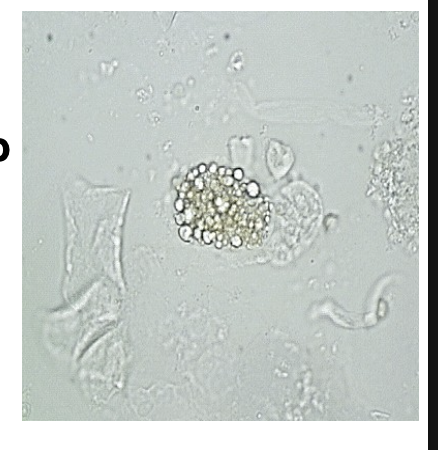
Oval Fat Bodies
RTE cells that have absorbed lipids from glomerular filtrate
Lipid appears highly refractile; often seen with fat droplets or fatty casts
Confirm with:
Sudan III or Oil Red O (triglycerides/neutral fat)
Polarized light (cholesterol → Maltese cross pattern)
May be confused with starch or crystals
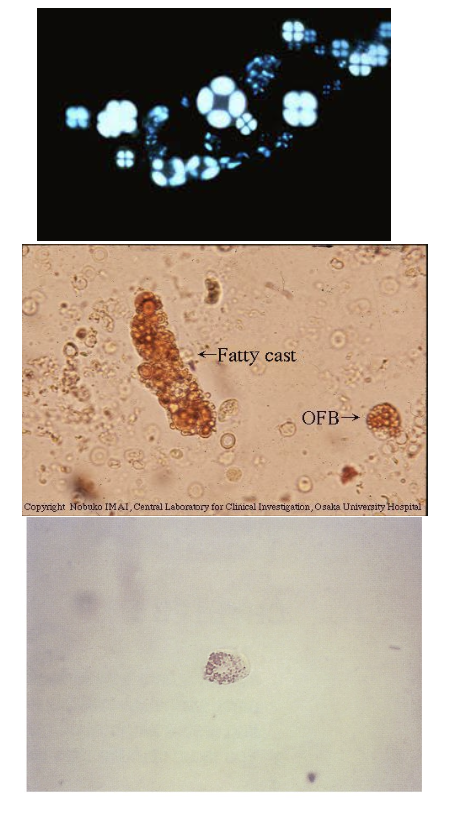
Lipiduria
Presence of fat in urine
Confirm with Oil Red O or Sudan III stain
Associated with:
Nephrotic syndrome (glomerular damage)
Tubular necrosis
Diabetes mellitus
Trauma (bone marrow fat)
Lipid storage diseases → oval fat bodies from histiocytes (not RTE)
Bacteria in Urine
Not normally present
Can multiply at room temp >2 hrs, altering results
Evaluate microscopy findings alongside nitrite and leukocyte esterase tests
Presence suggests UTI (upper or lower)
Follow up: Quantitative urine culture if UTI is suspected
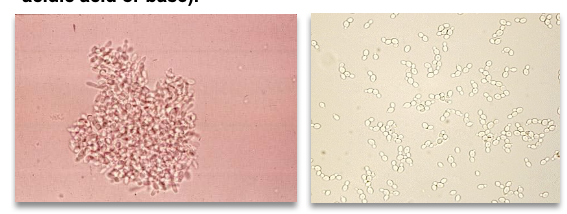
Yeast in Urine
Small, refractile ovals; may show budding or hyphae
Common species: Candida albicans
Often seen in:
Diabetes mellitus (acidic, glucose-rich urine)
Immunocompromised patients
Vaginal yeast infections
May be a contaminant; rapid growth → interpret with caution
WBCs should be present if infection is true
Differentiation tip: Yeast resists acid/base, RBCs do not
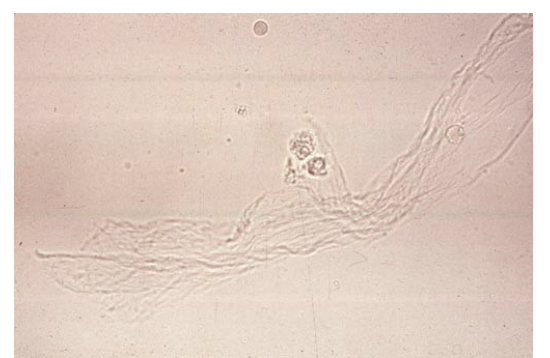
Mucus in Urine
Made by RTEs and lower GU tract glands
Major protein: Tamm-Horsfall
Appears as fine, thread-like strands with low refractive index
Seen better with lowered light at 10x
More common in females
No clinical significance, but reported (1+ to 4+)
May affect strip test values and turbidity
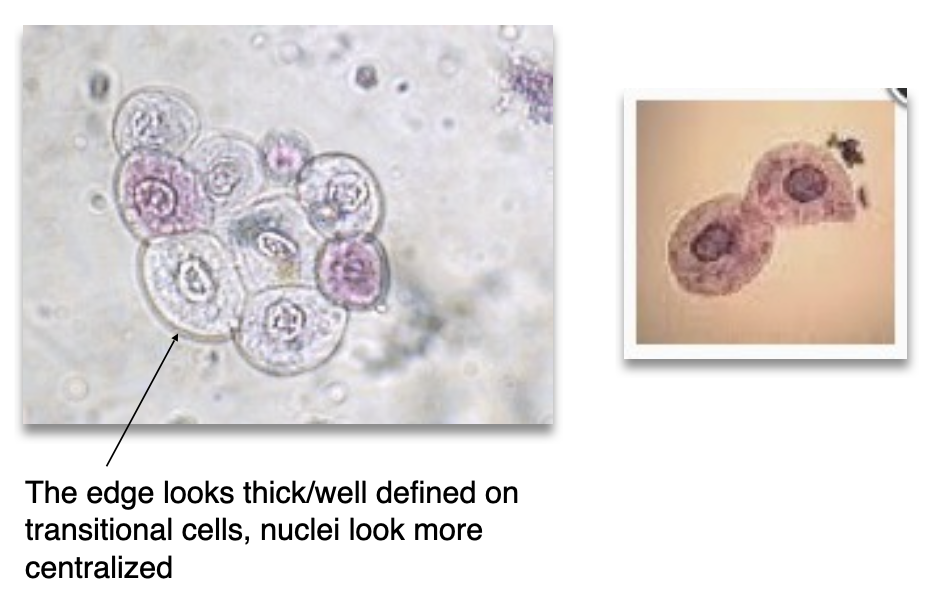
Spermatozoa in Urine
Oval head, long tail; ~½ size of an RBC
Not motile in urine (toxic environment)
Usually not clinically significant, but may cause:
False positive protein on strip due to seminal proteins
Lab policy variance: some report only with + protein
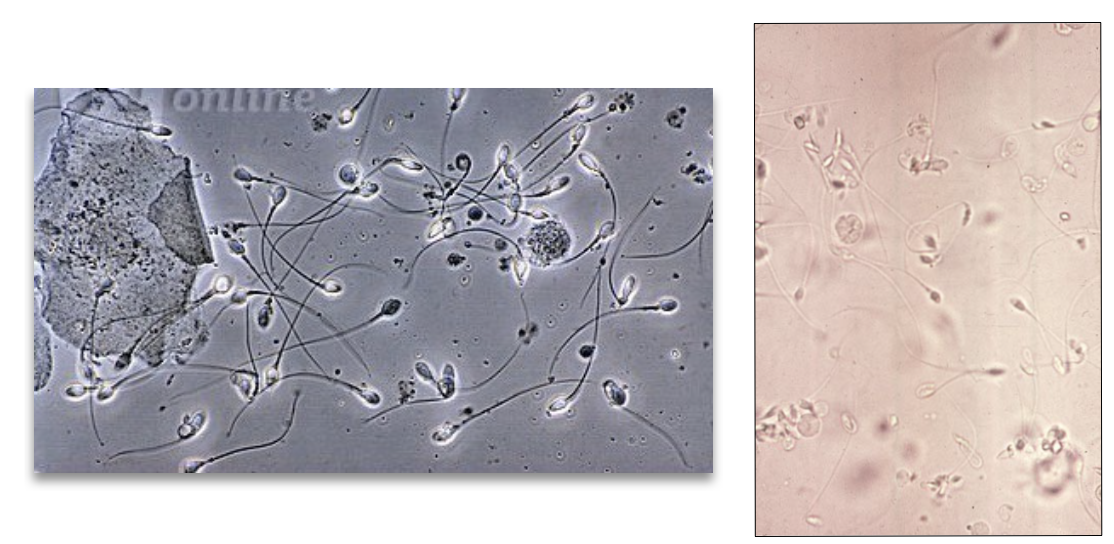
When to report Sperm
Underage or elderly females → potential legal/clinical significance
Causes may include:
Specimen mix-up
Sexual activity
Sexual assault