Pediatric Advanced Life support (PALS) 2025 Manual S) questions and answers with expert solutions + rationales
1/102
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
103 Terms
List 11 clinical signs of tissue hypoxia that indicate respiratory distress.
1-tachypnea
2-bradypnea (late)
3-apnea (late)
4-tachycardia (early)
5-bradycardia (late and ominous)
6-cyanosis (late)
7-pallor
8-nasal flaring
9-fatigue
10-agitation
11-altered mental status
The above were signs of what medical condition that can be immediately life threatening?
Explain difference between hypoxemia and tissue hypoxia.
1-Hypoxemia is low oxygen content in arterial blood. Initially measured with pulse oximetry.
2-Tissue hypoxia is low oxygen content in tissues other than arterial blood. There is no direct test for measuring tissue hypoxia. We depend on clinical signs to detect this condition.
3-Hypoxemia and hypoxia are not mutually assured. You can have hypoxia without hypoxemia and vica-versa,
Is hypoxia the same as hypercarbia?
No. HypOxIA and HypERCARBIA are two different conditions. They have different clinical signs, but these signs do overlap, making the use of ABG critical in differentiating the two conditions.
What blood test can be used to differentiate hypoxia from hypercarbia as causes of signs of respiratory distress?
Arterial Blood Gas can pick up hypercarbia, but not hypoxemia.
Compare signs of hypoxia and hypercarbia.
Hypoxia Hypercarbia
1-tachypnea 1-tachypnea
2-bradypnea (late)
3-apnea (late)
4-tachycardia (early)
5-bradycardia (late)
6-cyanosis (late)
7-pallor
8-nasal flaring 2-nasal flaring
9-fatigue 3-fatigue
10-agitation 4-agitation
11-altered mental status 5-altered mental status
How is respiratory distress/failure categorized?
By severity (failure is more severe by definition than distress)
By anatomic location of cause.
What are the possible anatomic sites causing respiratory distress?
1-upper airway
a-nose
b-pharynx
c-hypopharynx(=larynx)
2-lower airway
a-trachea
b-bronchi
c-bronchioles
3-Lung tissue
a-pneumonia
b-pulmonary edema
c-ARDS
4-Disordered respiratory control system
a-CNS
i-seizures
ii-Central Nervous System infections
iii-head injury
iv-hydrocephalus
v-brain tumor
vi-neuromuscular disease
1)-myasthenia gravis
2)-Lou Gehrig's disease/Amyotrophic lateral sclerosis
The above describe what?
Signs of upper airway obstruction (10)?
1-tachypnea
2-increased respiratory effort
3-crying
4-change in voice ( hoarseness or "barky" cough)
5-stridor (usually inspiratory)
6-poor chest excursion (chest rise)
7-see-saw chest/abdominal motion on inspiration
8-poor air entry on auscultation
9-increased inspiratory respiratory effort ( inspiratory retractions, use of accessory muscles of respiration, nasal flaring)
10-drooling, snoring or gurgling sounds
The above are signs of what condition or of what classification of cause of respiratory distress?
Signs of lower airway obstruction (6)?
1-tachypnea
2-increased respiratory effort
3-wheezing (usually expiratory, but can be inspiratory)
4-coughing
5-prolonged expiratory phase
6-retractions, nasal flaring and prolonged expiration
The above are signs of what classification of cause of respiratory distress?
Signs of lung tissue disease causing respiratory difficulty (7)?
1-tachypnea
2-increased respiratory effort
3-diminished breath sounds
4-grunting
5-tachycardia
6-hypoxemia (despite administration of supplementary O2)
7-crackles (rales) and decreased air movement
The above are signs of what classification of cause of respiratory distress?
Signs of disordered control of breathing (5)?
1-Variable/irregular respiratory rate
2-Variable respiratory effort
3-Central apnea
4-Shallow breathing
5- normal or decreased air movement
The above are signs of what classification of cause of respiratory distress?
Causes of upper airway obstruction?
1-Croup
2-Anaphylaxis
3-FBO
4-tonsillar hypertrophy
5-epiglottis
6-pharyngeal or peritonsillar abscess, retropharyngeal abscess, or tumor
7-congenital airway abnormality( congenital subglottic stenosis)
Treatment of respiratory distress due to croup?
Mild croup
1-cool mist+oxygen
2-dexamethasone (0.6 mg/kg IM, not to exceed 10 mg)
Mod.-Severe
1-cool mist+oxygen
2-dexamethasone (0.6 mg/kg IM, not to exceed 10 mg) or nebulized
3-L -epinephrine (1:1000) nebulized has proven to significantly reduce croup symptoms 30 minutes after treatment.
4-Nebulized budesonide (2 mg)
5-Inhaled Decadron when budesonide unavailable
6-NPO
Severe
1-6 above
7-Intubate
8-ventillate
The above are current therapies for________?
Treatment of respiratory distress due to anaphylaxis?
1-epinephrine 0.01 mg/kg IM or IV
2-Albuterol for wheezing
√MDI
√cont. nebulizer
3-benadryl
√Pediatric Dosage: 2-5 mg/kg.
√Adult Dosage: 25-50 mg.
√Routes: Slow IV push or deep IM.
4-H2blocker
√Zantac (ranitidine)
Bolus IV: 50 mg IV q6-8h
Continuous IV: 6.25 mg/h IV
Oral Dosing: 150 mg PO bid
√Pepcid (famotidine)
Oral dosing: 20 to 40 mg PO bid
√Tagamet (cimetidine)
Bolus parenteral dosing: 300 mg IV or IM q6h
Continuous IV Dosing: 37.5 mg/h IV
Oral Dosing: 400 mg PO bid
5-methylprednisolone (SoluMedrol)
6-Trendelenburg+IV epi titrate+IV isotonic crystalloid 20 ml/kg
1-Formula for calculating "Arterial Oxygen Content" (AOC)?
2-What clinical tests/observations are needed to be able to calculate AOC?
1) AOC=[1.36 x Hgb conc. X SpO2]+[0.003xPaO2]
2) CBC, pulse oximetry, ABG
What clinical and laboratory measurable parameters do you need to be able to calculate the Arterial Oxygen Content?
1-serum Hgb concentration (obtained from CBC) in units of g/dL
2-SpO2=Saturation pulse oxygen (Pulse ox machine reading) in units of %
3-PaO2=Partial pressure arterial oxygen (obtained from arterial blood gas test) in units of mm HG
What are 5 environmental or patient physiologic factors that can cause hypoxemia?
1-low ambient PO2
2-Alveolar hypoventilation
3-Diffusion defect
4-Vent./Perfusion (V/Q) imbalance
5-Shunt
Mechanism by which _____ causes hypoxemia?
1-Low ambient PO2
2-Alveolar hypoventilation
3-Diffusion defect
4-V/Q mismatch
5-Shunt
1-decreased ambient partial pressure O2 (PO2)
2-increased arterial PCO2->increased alveolar CO2->decreased alveolar O2 available for uptake
3-Alveolar/capillary memb. less gas permeable
4-Failure of arterioles to shut down in areas of lung that are hypo-inflated-not irreversible
5-Fixed ongoing perfusion in areas of lung that are not ventilated-not irreversible
How is hypoxemia from ______ treated?
1-Low ambient PO2
2-Alveolar hypoventilation
3-Diffusion defect
4-V/Q mismatch
5-Shunt
1-supplemental O2
2-supplemental O2, restore normal ventilation
3-supplemental O2+CPAP or intubation+PEEP+O2+mech. vent.
4-intubation, PEEP, O2, mech. vent.
5-Surgical repair
Management of hypoxia due to upper airway obstruction?
If mild:
1-Position comfortable if conscious
2-O2 via nonrebreathing mask
If severe (unconscious)
1-Position head-tilt+chin lift
3-check airway
4-if obstructed
a)<12 mo old b)>12 mos
i-3 back slaps
ii-3 chest thrusts ii-abdominal thrusts
iii-inspect mouth-remove FOB
iv-attempt PPV
v-if unsuccessful PPV start CPR
Management of hypoxia due to lower airway obstruction?
1-Airway
√If conscious, allow assumption comfortable post.
√Stabilize C-spine
√Open airway
√Suction airway prn
√Remove any foreign bodies
√OPA or NPA
2-Breathing
√Assist ventilation (Bag-valve mask) if needed
√Hunidified O2
√Use high conc. O2 delivery system if spont. resp. present-non-rebreather mask
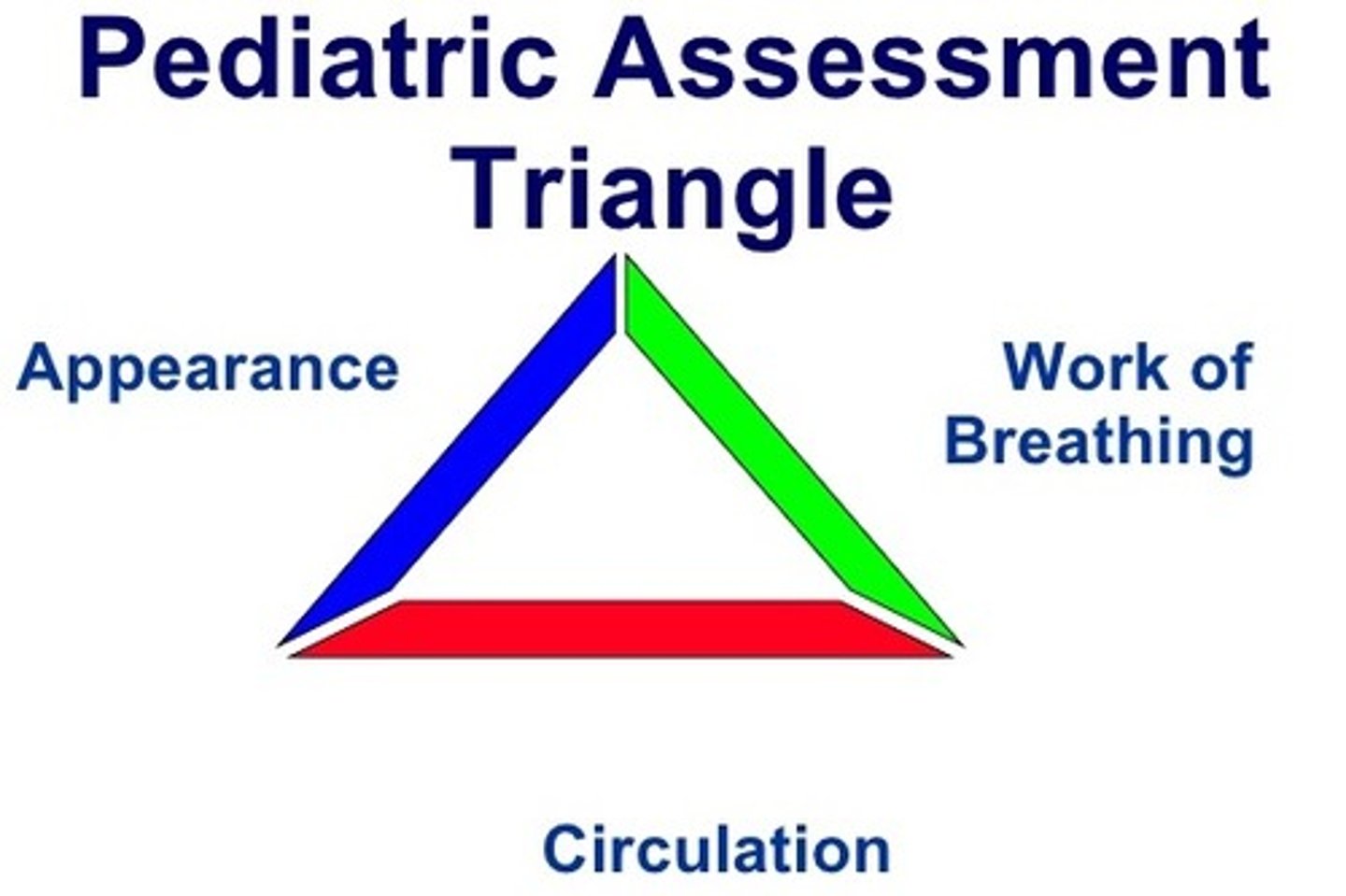
PAT
Pediatric Assessment Triangle which stands for appearance, work of breathing, circulatory status.
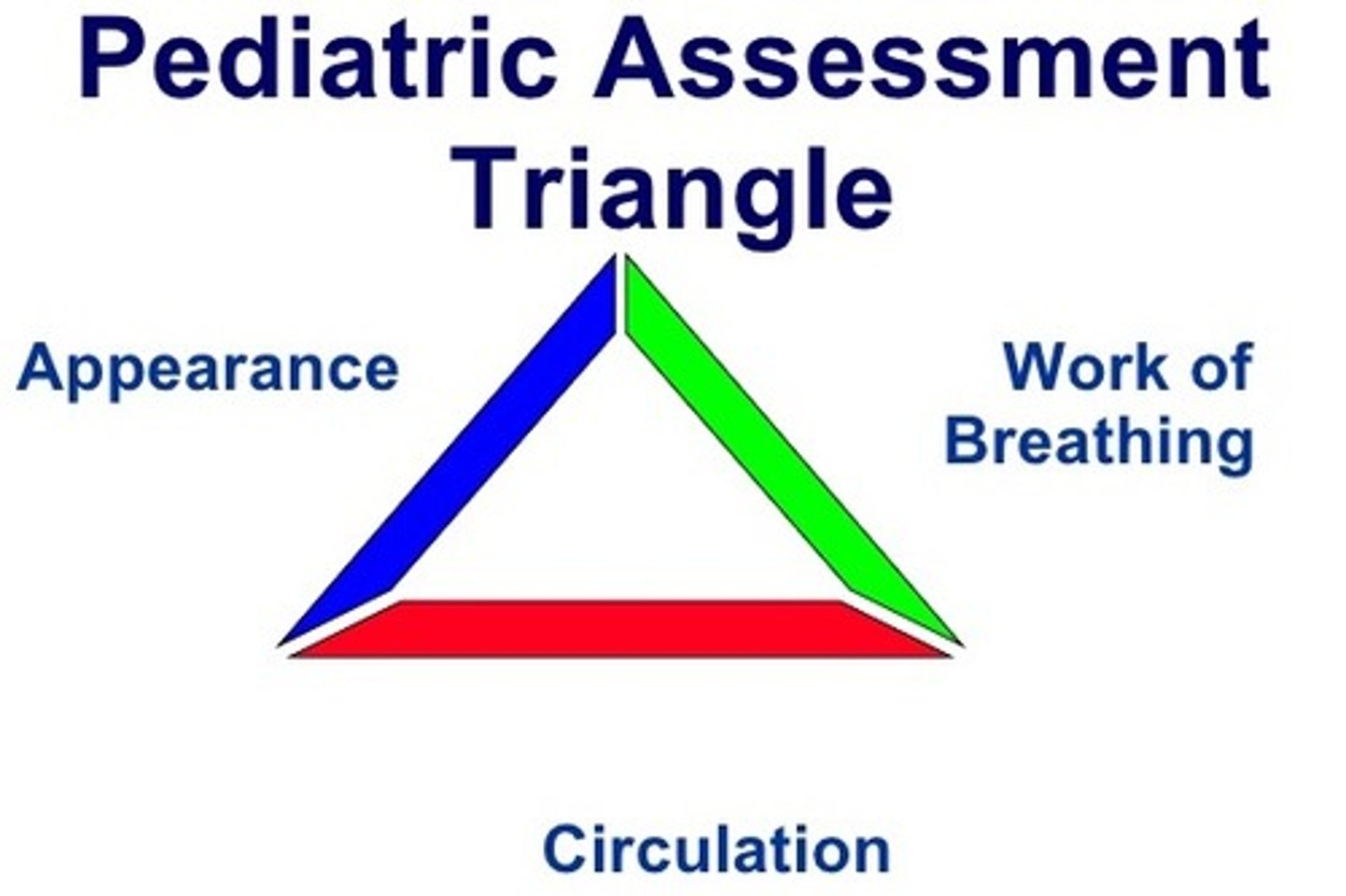
Appearance (PAT)
includes level of consciousness and ability to interact. Observe the child's appearance to evaluate the LOC.
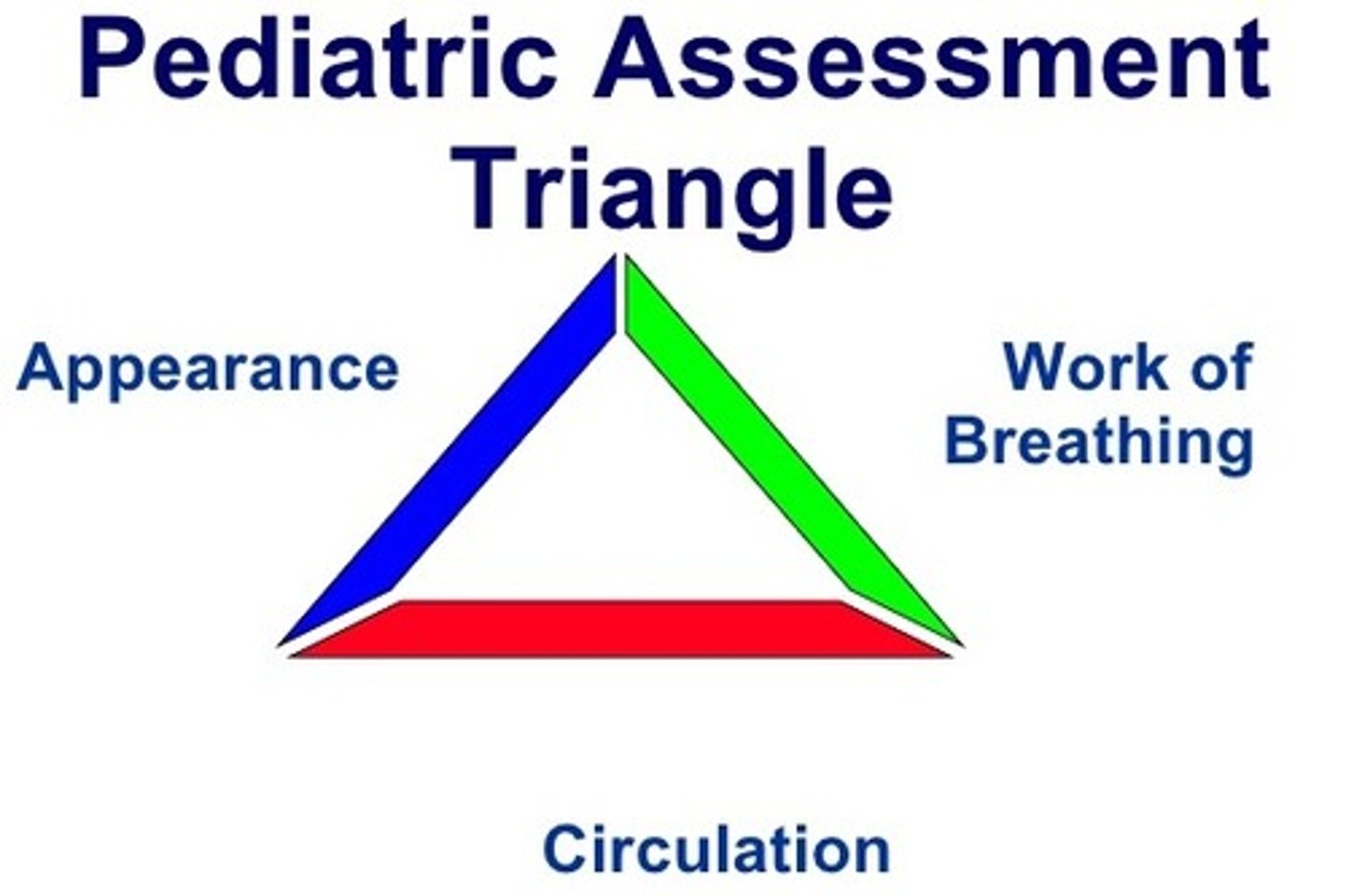
Level of consciousness (LOC)
defined by the child's tone, interactiveness, consolability, look/gaze/stare and speech/cry.
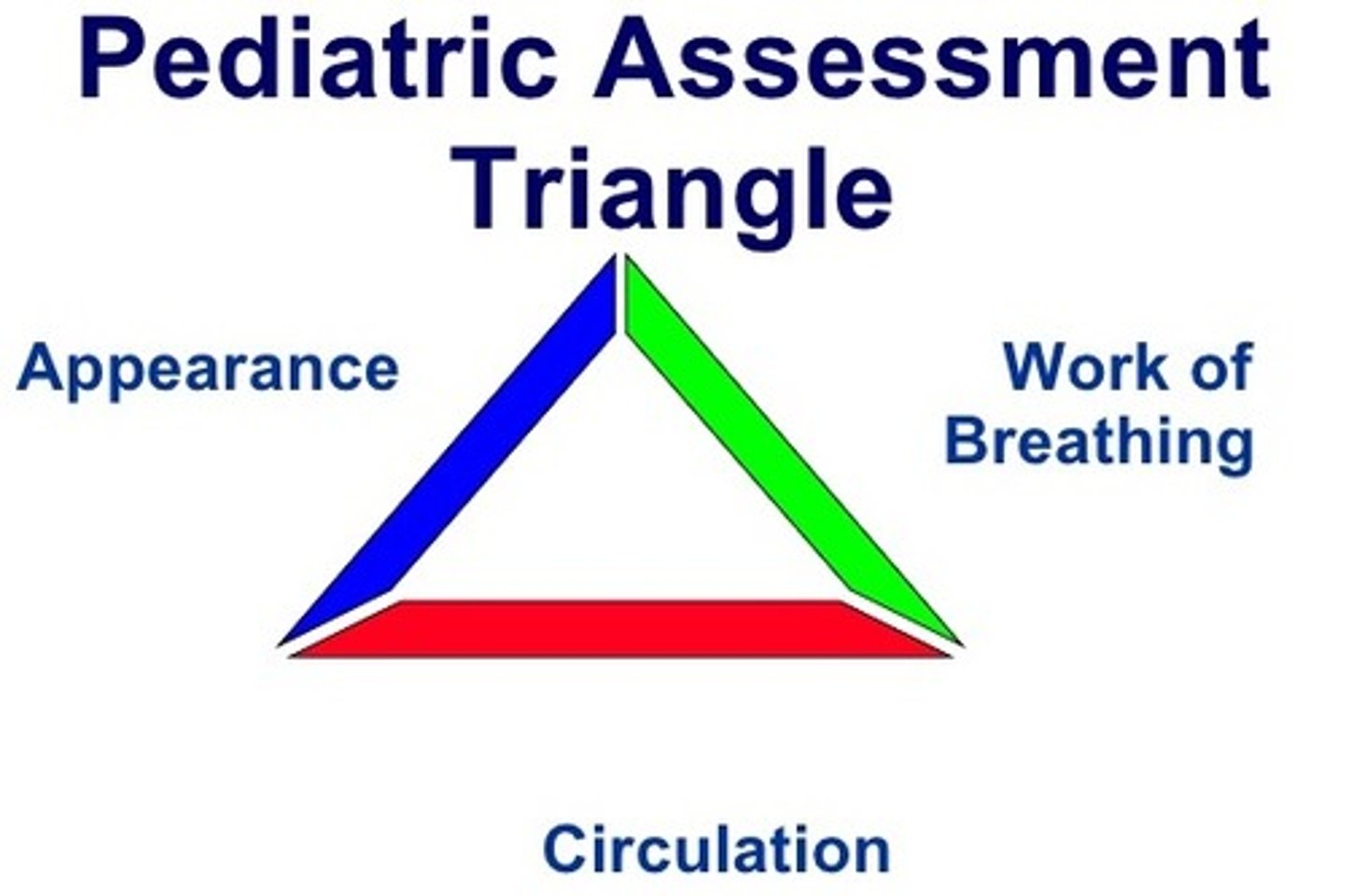
Breathing (PAT)
evaluation of work of breathing (WOB), position and any audible breath sounds (sounds of breathing with or without a stethoscope). Look for abnormal breathing such as grunting, stridor, or wheezing. Note the patient's positioning that suggests respiratory distress for ex. tripod position.

Abnormal Work of Breathing (WOB) signs
nasal flaring, retractions or use of accessory muscles, increased, inadequate, or absent respiratory effort, noisy breathing (for ex. wheezing, grunting, stridor)
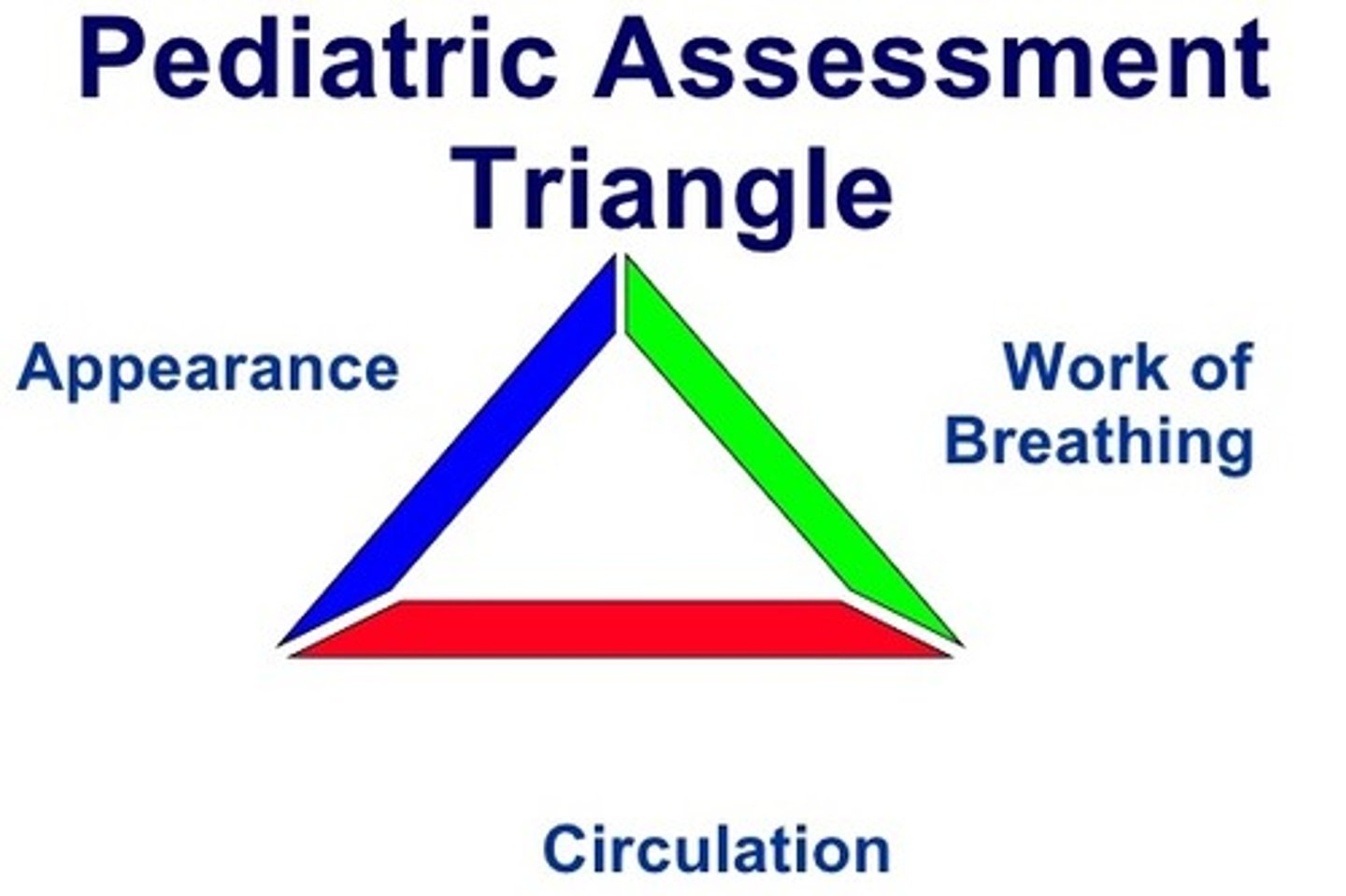
Circulation (color)
the childs overall circulatory status. Assess the child's color, which may help you assess how well the child is perfusing. This include skin color and pattern or obvious significant bleeding.
Pallor (paleness)
Pallor is a pale color of the skin that can be caused by illness, emotional shock or stress, stimulant use, or anemia, and is the result of a reduced amount of oxyhaemoglobin and is visible in skin or mucous membrane. Suggests poor perfusion, poor oxygenation, or both.

Mottling
Mottle is a pattern of irregular marks, spots, streaks, blotches or patches of different shades or colours. It is commonly used to describe the surface of plants or the skin of animals. In plants, mottling usually consists of yellowish spots on plants, and is usually a sign of disease or malnutrition.Suggests poor perfusion, poor oxygenation, or both.

Cyanosis
Cyanosis is the appearance of a blue or purple coloration of the skin or mucous membranes due to the tissues near the skin surface having low oxygen saturation. Suggests poor perfusion, poor oxygenation, or both.

Petechiae
A petechia, plural petechiae, is a small red or purple spot on the skin, caused by a minor bleed from broken capillary blood vessels. Petechia refers to one of the three descriptive types of bleeding into the skin differentiated by size, the other two being purpura and ecchymosis. Petechiae are by definition less than 3 mm.

Purpura (visible bleeding wounds)
Purpura is a condition of red or purple discolored spots on the skin that do not blanch on applying pressure. The spots are caused by bleeding underneath the skin usually secondary to vasculitis or dietary deficiency of vitamin C. They measure 0.3-1 cm, whereas petechiae measure less than 3 mm, and ecchymoses greater than 1 cm. this purplish discoloration of the skin is often a sign of a life-threatening infection.

Respiratory (upper airway obstruction)
Respiratory distress
Respiratory failure
Respiratory (lower airway obstruction)
Respiratory distress
Respiratory failure
Respiratory (lung tissue disease)
Respiratory distress
Respiratory failure
Respiratory (disordered control of breathing)
Respiratory distress
Respiratory failure
Circulatory (hypovolemic shock)
Compensated shock
Hypotensive shock
Circulatory (distributive shock)
Compensated shock
Hypotensive shock
Circulatory (cardiogenic shock)
Compensated shock
Hypotensive shock
Circulatory (obstructive shock)
Compensated shock
Hypotensive shock
Primary Assessment
uses a hands on ABCDE approach and include assessment of the patient's vital signs. A-airway B-breathing C-circulation D-disability E-exposure
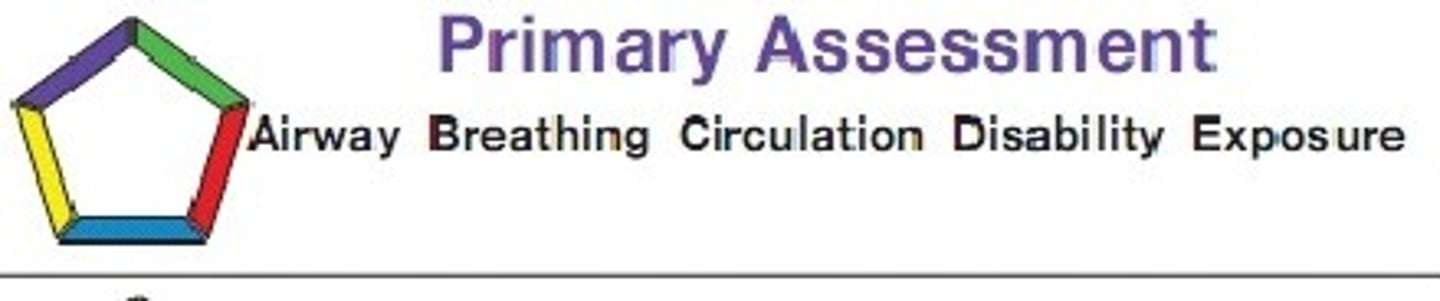
Primary Assessment (A-airway)
*look for movement of the chest or abdomen
*listen for air movement and breath sounds
*Feel for movement of air at the nose and mouth
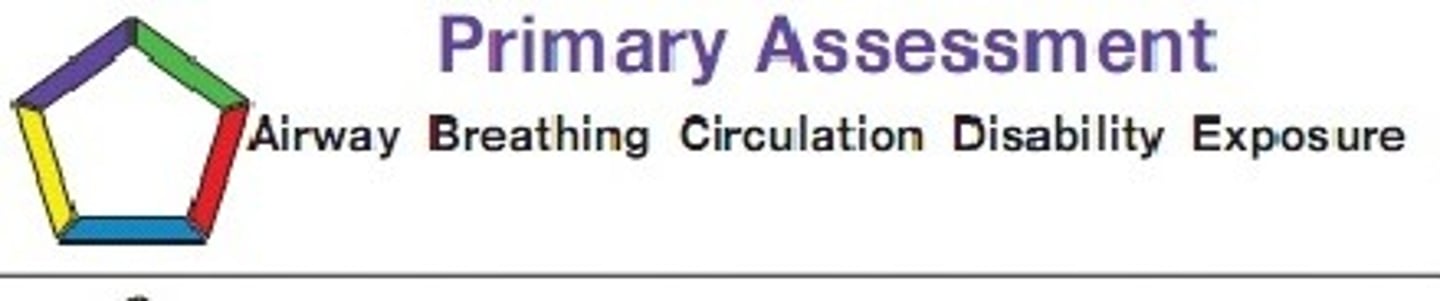
Primary Assessment (B-breathing)
*Respiratory rate and pattern
*respiratory effort
*chest expansion and air movement
*lung and airway sounds
*O2 saturation by pulse oximetry
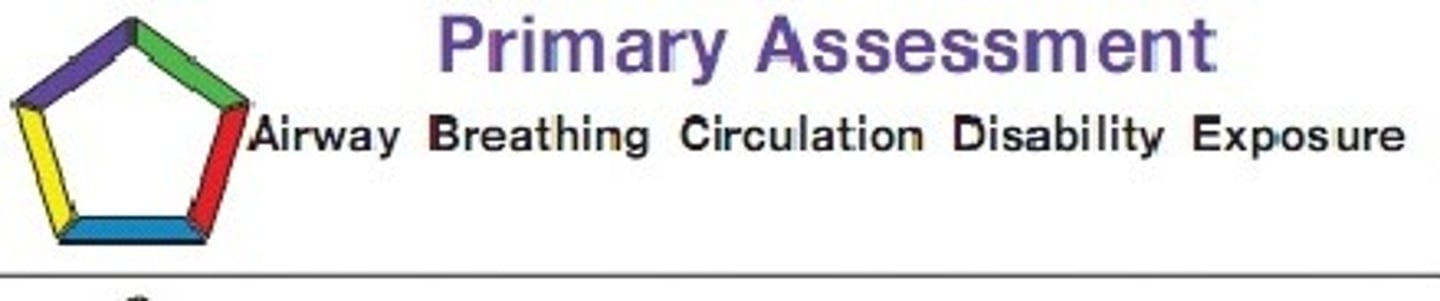
Primary Assessment (C-circulation)
*heart rate and rhythm
*pulses(both peripheral and central)
*capillary refill time
*skin color and temperature
*blood pressure
*urine output and LOC
Primary Assessment (D-disability)
Sudden and severe cerebral hypoxia may cause the following neurologic signs:
*decreased LOC
*loss of muscle tone
*generalized seizures
*pupil dilation
other signs observed that can be subtle
*decreased LOC with or without confusion
*irritability
*lethargy
*agitation alternating with lethargy
Standard evaluation
*AVPU(alert, responsive to voice, responsive to pain, unresponsive) Pediatric response scale
*Glasgow Coma Scale (GCS)
*pupil response to light
*blood glucose test
Primary Assessment (E-exposure)
*Look for signs of injury to the extremities, including deformities or brusing.
*Look for the presence and progression of petechiae and purpura (nonblanching purple discolorations in the skin caused by bleeding from capillaries and small vessels)
*look for evidence of trauma
*note any differences in warmth between trunk and extremities
Normal Respiratory Rate
infant 30-53 bpm
toddler 22-37 bpm
preschooler 20-28 bpm
school age child 18-25 bpm
Adolescent 12-20 bpm
Normal Heart Rates
Neonate awake 100-205 sleeping 90-160
infant 100-180 90-160
toddler 98-140 80-120
School age 75-118 58-90
adolescent 60-100 50-90
Pallor(paleness; lack of normal color)
location (skin or mucous)
causes (normal skin color, decreased blood supply to the skin(cold; stress; shock; especially hypovolemic and cardiogenic), decreased number of RBC (anemia), decreased skin pigmentation
Central Pallor
location (mucous membranes)
Causes (anemia, poor perfusion)
Mottling (irregular or patchy discoloration)
location (skin)
Causes (normal distribution of skin melanin, intense vasoconstriction from irregular supply of oxygenated blood to the skin due to hypoxemia, hypovolemia, or shock.
Cyanosis(blue discoloration)
location (skin or mucous membranes)

Acrocyanosis
location (hands and feet and around the mouth(ie, the skin around the lips))
causes (normal in the newly born)

Peripheral cyanosis
location (hands and feet (beyond newborn period))
causes (shock, CHF, Peripheral vascular disease, conditions causing venous stasis)

Central cyanosis
location (lips and other mucous membranes)
causes (low ambient O2 tension (high altitude), alveolar hypoventilation(traumatic brain injury, drug overdose), diffusion defect(pneumonia), v/q imbalance(asthma, bronchiolitis, acute respiratory distress syndromes), intracardiac shunt(cyanotic congenital heart disease).

Lung and Airway Sounds-Stridor
Stridor is a high-pitched breath sound resulting from turbulent air flow in the larynx or lower in the bronchial tree.It can be inspiratory, expiratory or biphasic, although it is usually heard during inspiration. Inspiratory stridor often occurs in children with croup. Causes
Any process that causes airway narrowing can cause stridor. With infants, stridor usually indicates a congenital disorder (problem that your child is born with), including laryngomalacia, vocal cord paralysis or subglottic stenosis. If your toddler or older child develops stridor, it may occur as a result of an infection such as croup or papillomatosis. In rare circumstances, stridor can occur secondary to trauma or foreign body aspiration.
Lung and Airway Sounds-Snoring
Snoring is the sound you make when your breathing is blocked while you are asleep. The sound is caused by tissues at the top of your airway that strike each other and vibrate. Can be a sign of airway obstruction.
Lung and Airway Sounds-Grunting
typically a short, low pitched sound heard during expiration. although grunting may accompany the response to pain or fever, infants and children often grunt to help keep the small airways and alveolar sacs in the lungs open. This is an attempt to optimize oxygenation and ventilation.
is typically a sign of severe respiratory distress or failure from lung tissue disease. pulmonary conditions that cause grunting (pneumonia pulmonary contusion, and acute resp distress syndrome) It may be caused by cardiac conditions such as CHF, that result in pulmonary edema. Grunting may be a sign of pain resulting from abdominal pathology (bowel obstruction, perforated viscus, appendicitis, peritonitis).
Lung and Airway Sounds-Gurgling
is a bubbling sound heard during inspiration or expiration. It results from upper airway obstruction due to airway secretions, vomit, or blood.
Lung and Airway Sounds-Wheezing
is a high pitched or low pitched whistling or sighing sound heard most often during expiration. typically indicates lower airway obstruction in the smaller airways. Common causes of wheezing are bronchiolitis and asthma. isolated inspiratory wheezing suggests a foreign body or other cause of partial obstruction of the trachea or upper airway.
Lung and Airway Sounds-Crackles
known as rales, are sharp crackling inspiratory sounds. moist crackles indicate accumulation of alveolar fluid. They are associated with lung tissue disease (pneumonia, pulmonary edema) or interstitial lung disease.
Dry crackles are more often heard with atelectasis( sm airway collapse) and interstitial lung disease. note you may not hear crackles in the presence of pulmonary edema.
Lung and Airway Sounds-change in cry/phonation/cough (including barking cough)
When a infant's cry becomes very soft with only short sounds during expiration (like a cat) or an older child begins to talk in short phrases or single words instead of sentences this may indicate severe respiratory distress or SOB.
If an infant or child develops a "barking" cough or change in pitch of cry or voice this may indicate upper airway obstruction.
Normal Sinus rhythm, rate 100/min

Sinus bradycardia

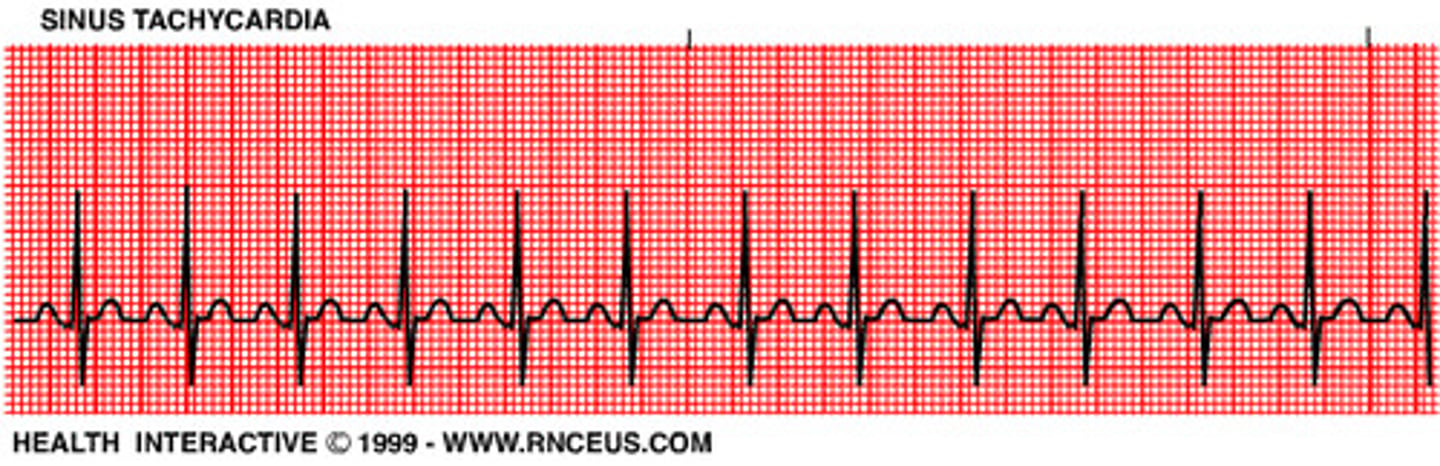
Sinus tachycardia
Sinus rhythm with first degree heart block

Ventricular tachycardia 150/min
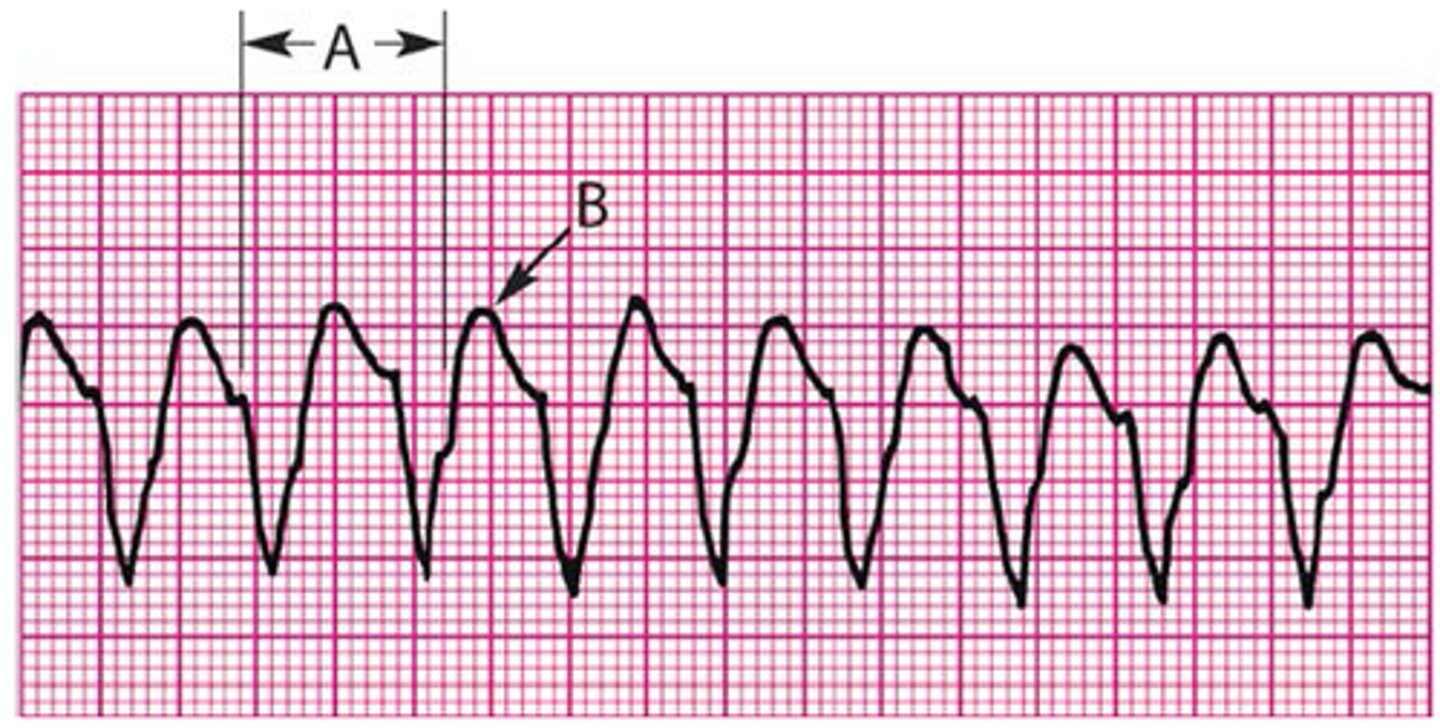
Torsades de pointes or Polymorphic Ventricular tachycardia

Ventricular fibrillation or Coarse V-Fib

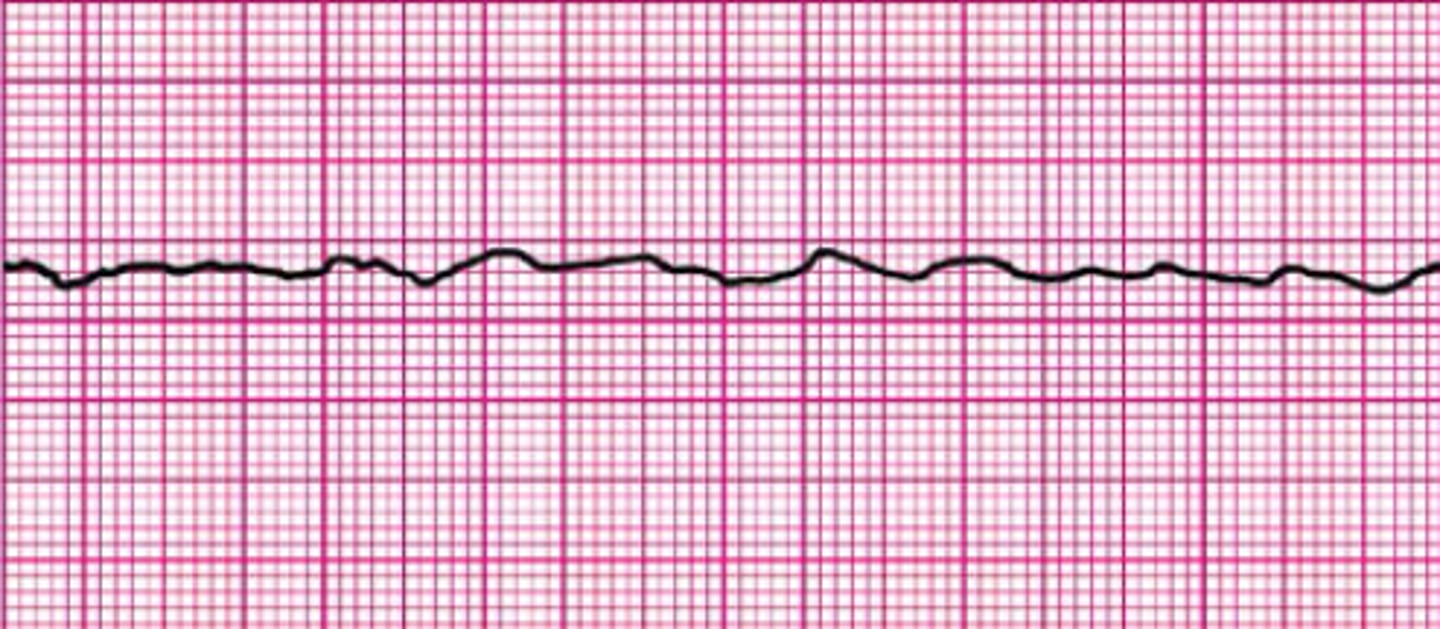
Fine V-Fib
Asystole
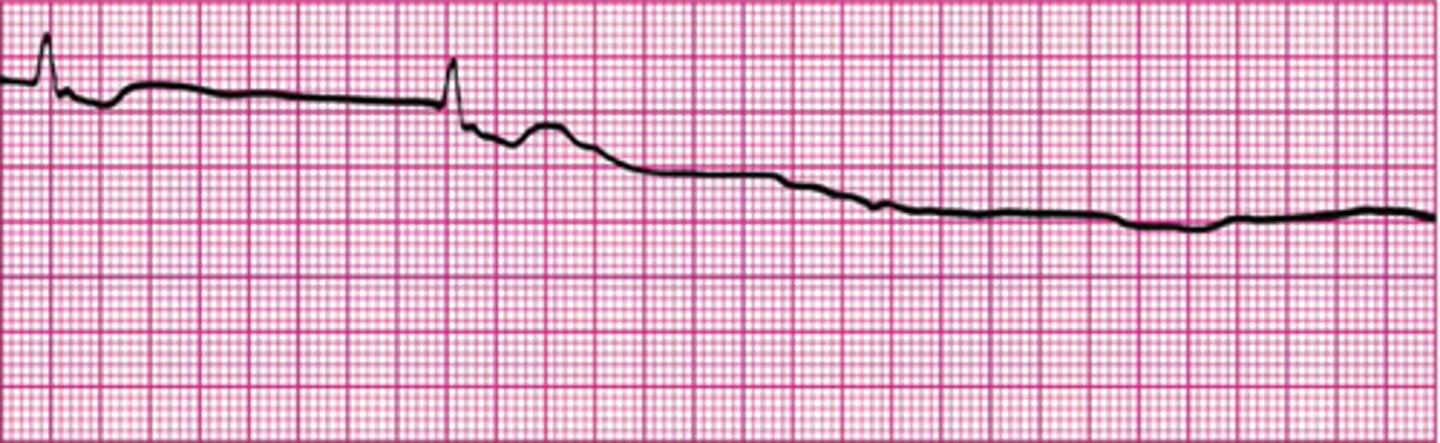
Third-degree(complete) heart block with ventricular escape rhythm
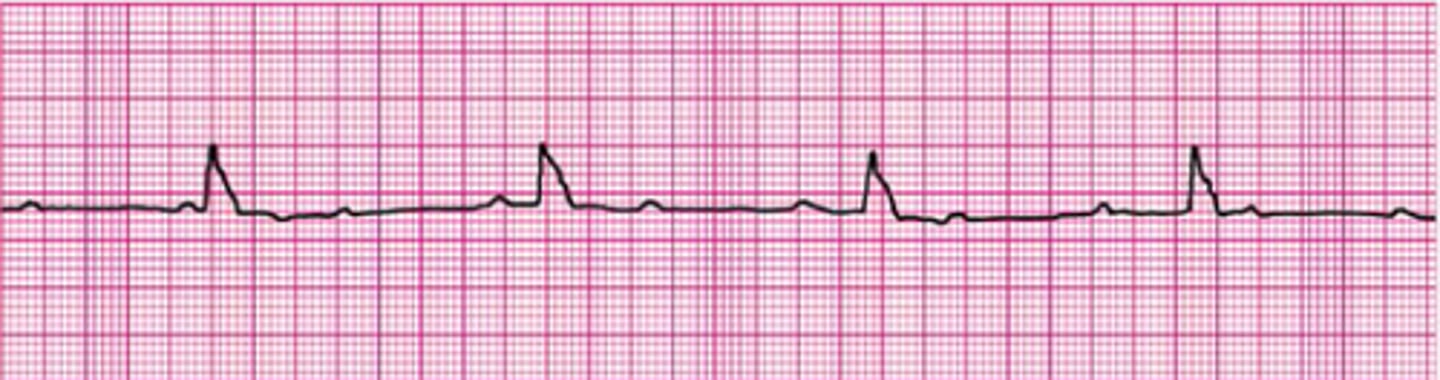
Second-degree heart block, Mobitz type 2
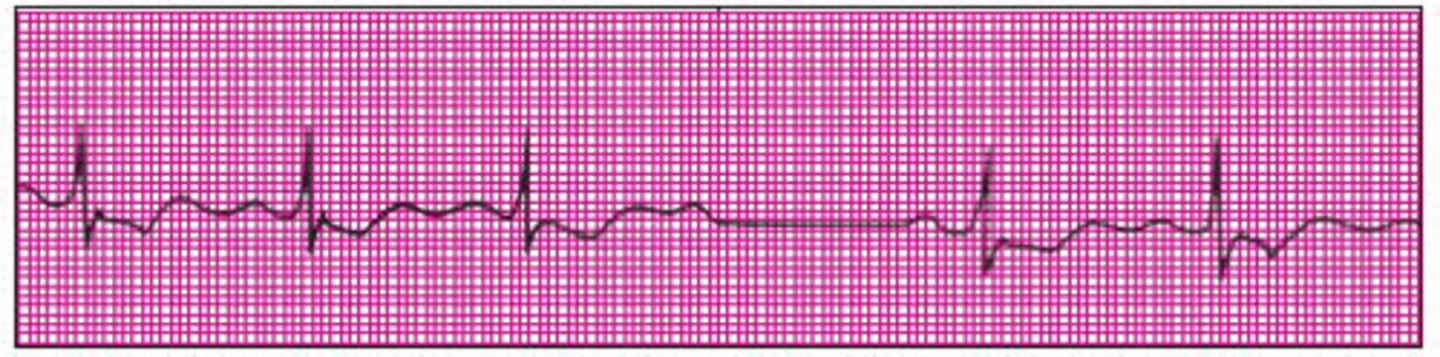
Atrial flutter
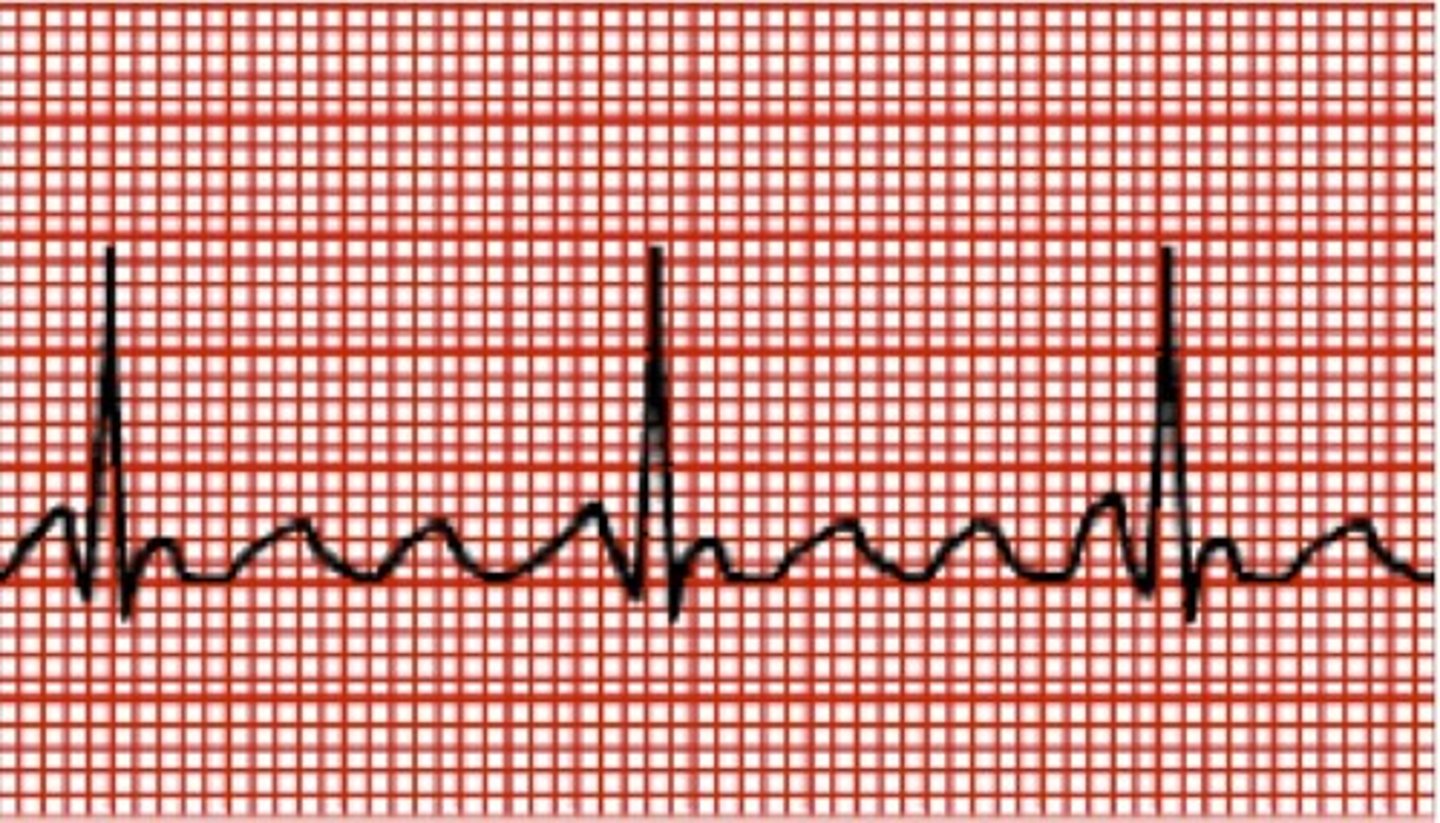
Second-degree heart block, Mobitz type 1, or Wenckebach

Superventricular Tachycardia 230/min

Sinus rhythm with peaked T waves
Weakening of pulses as perfusion decreases
When cardiac output decreases in shock, systemic perfusion decreases incrementally. The decrease in perfusion starts in the extremities with a decrease in intensity of pulse and then an absence of peripheral pulses. As cardiac output and perfusion decrease further, there is eventual weakening of central pulses.
Capillary refill time
is the time it takes for blood to return to tissue blanched by pressure. A prolonged capillary refill time indicate low cardiac output. Normal capillary refill time is 2 sec or less.
Common causes of sluggish, delayed or prolonged capillary refill are dehydration, shock and hypothermia. Note that shock can be present despite normal or even brisk capillary refill time.
Fast Respiratory Rate (tachypnea)
the first sign of resp distress in infants. Can also develop during periods of stress.
Fast Respiratory Rate (quite tachypnea)
a fast respiratory rate that is not accompanied by signs of increase respiratory effort. Common causes high fever, pain, anemia, cyanotic congenital heart disease, and sepsis (serious infection) or dehydration.
Slow Respiratory Rate (bradypnea)
common causes: Respiratory muscle fatigue, a CNS injury or problem that affects the respiratory control center, severe hypoxia, severe shock, hypothermia, drugs that depress the respiratory drive, muscle diseases that cause muscle weakness.
Bradypnea or an irregular RR in an acutely ill infant or child is an ominous clinical sign and often signals impending arrest.
Increased Respiratory Effort
results from conditions that increase resistance to airflow(asthma or bronchiolitis) or that cause the lungs to be stiffer and difficult to inflate(pneumonia, pulmonary edema, or pleural effusion). Non pulmonary conditions that result in severe metabolic acidosis(shock, dka, salicylate ingestion, inborn errors or metabolism) can also cause increased respiratory rate and effort.
Signs of increased respiratory effort
nasal flaring, retractions, head bobbing or seesaw respirations. prolonged inspiratory or expiratory times, open-mouth breathing, gasping, use of accessory muscles. grunting is a serious sign of resp distress or failure.
Cause of Seesaw breathing
found mostly in children with neuromuscular disease. weakness of the abdominal and chest wall muscles. is caused by strong contraction of the diaphragm that dominates the weaker abdominal and chest wall muscles. The result is retraction of the chest and expansion of the abdomen during inspiration.

inadequate respiratory effort
apnea, weak cry or cough, badypnea and agonal gasps. be prepared to support airway, oxygenation and ventilation.
Hypotension
An ominous sign of impending arrest. when hypotension develops in a child with shock, physiologic compensatory mechanisms (tachycardia and vasoconstriction) have failed. Hypotension in septic shock can occur from loss of intravascular volume and inappropriate vasodilation or severe vasoconstriction and inadequate cardiac output/cardiac index.
Management of airway and breathing and support of adequate intravascular volume, cardiac function and perfusion are needed to prevent cardiac arrest.
Urine Output
an indirect indication of kidney perfusion. Children with shock typically have decreased urine output.
Decreased Responsiveness
if an ill or injured child has decreased responsiveness, immediately assess oxygenation, ventilation, perfusion and blood glucose.
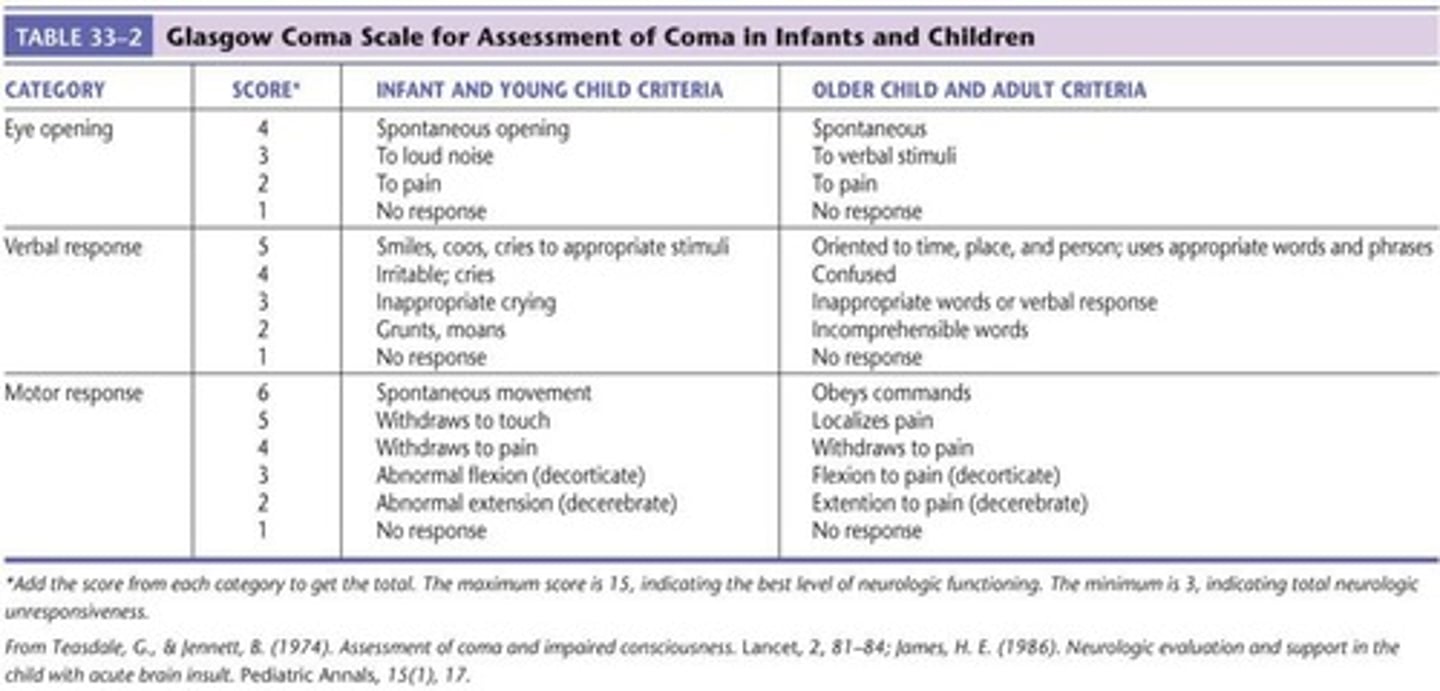
Glasgow Coma Scale
method used for evaluating a child's level of consciousness and neurologic status. The best eye opening (E), verbal (V), and motor(M) responses are individually scored. The scores are added together to produce the GCS score.
Mild head injury: GCS score 13 to 15
Moderate head injury: GCS score 9 to 12
Severe head injury: GCS score 3 to 8
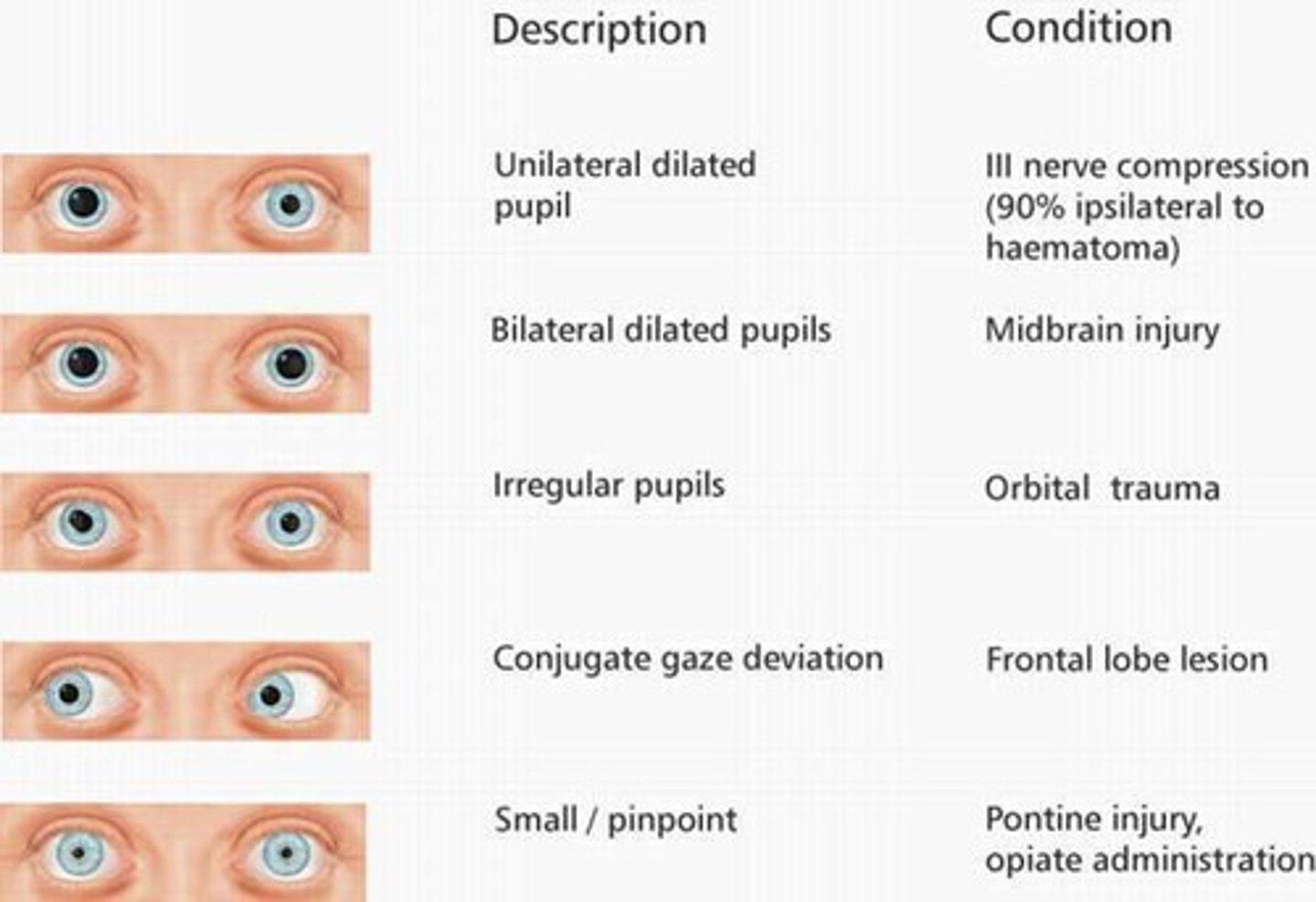
Abnormal pupil Responses and possible causes
pinpoint - narcotic ingestion (opioid)
dilated- predominant sympathetic autonomic activity, sympathomimetic ingestion (cocaine), Anticholinergic ingestion(local or systemic atropine), increased intracranial pressure.
unilaterally dilated -inadvertent topical absorption of a breathing treatment(atrovent), dilating eye drops
unilaterally dilated pupils with AMS- ipsilateral(same side) uncal herniation (lateral herniation of the temporal lobe, caused by increased intracranial pressure)
"S" signs and symptoms (S/S)
wheezing
tachypnea
tachycardia
diaphoresis
decreased LOC
Agitation, anxiety
fever
headache
decreased oral intake
diarrhea, vomiting
abdominal pain
bleeding
fatigue
time course of symptoms
breathing difficulties (cough, rapid breathing, increased Resp effort, breathlessness, abnormal breathing pattern, chest pain on deep inhalation)
"A" Allergies
medications, foods, latex, etc.
Associated rxns
"M" Medications
*patient medications, including OTC, vitamins, inhalers, and herbal supplements
*Last dose and time of recent medications
*medications that can be found in the childs environment
"P" Past medical history (Hx)
* health hx( premature birth, previous illness,
hospitalizations
*significant underlying medical problems (asthma,
chronic lung disease, congenital heart disease,
arrhythmia, congenital airway abnormality,
seizures, head injury, brain tumor, diabetes,
hydrocephalus, neuromuscular disease)
*past surgeries
*immunization status
"L" Last meal
Time and nature of last intake of liquid of food (including breast or bottle feeding in infants)
Elapsed time between last meal and presentation of current illness can affect treatment and management of the condition(possible anesthesia, possible intubation)
"E" Events
*Events leading to current illness or injury( onset
sudden or gradual , type of injury)
*Hazards at scene
* treatment during interval from onset of disease
or injury until evaluation
*Estimated time of onset (if out of hospital onset)
Physical examination (head-to-toe)
Respiratory distress-
nose/mouth( signs of obstruction, nasal congestion, stridor, mucosal edema)
-chest/lungs
-Heart (tachycardia, gallop, or murmur)
-LOC ( somnolence secondary to hypercardia, anxiety secondary to hypoxia)
Suspected heart failure and/or arrhythmias
-heart(gallop, murmur)
-lungs (crackles, difficulty breathing, intolerance of supine position)
-abdomen (evidence of hepatomegaly consistent with RT Heart Failure)
-Extremities (peripheral edema)
Trauma
-abdomen
-back
Diagnostic Assessments
help detect and identify the presence and severity of respiratory and circulatory problems.
Diagnostic tests for respiratory and circulatory problems
arterial blood gas (ABG)
venous blood gas (VBG)
capillary blood gas (CBG)
hemoglobin concentration
central venous O2 saturation
arterial lactate
central venous pressure monitoring
invasive arterial pressure monitoring
chest xray
ecg
echocardiogram
peak expiratory flow rate (PEFR)