Pharmacology Units 1-3
1/223
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
224 Terms
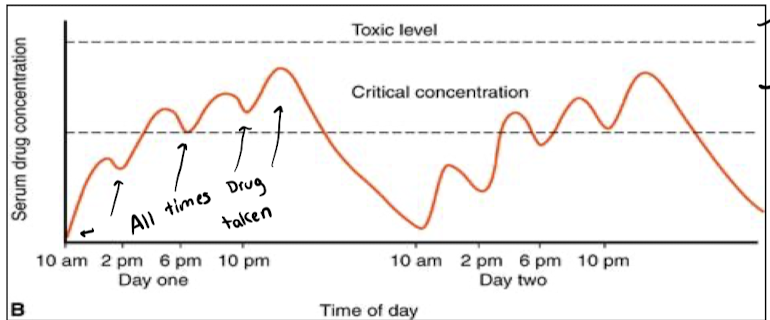
Usually measured via plasma concentration, which is taken from the patient. Graph of [drug in plasma] vs time.
![<p>Usually measured via plasma concentration, which is taken from the patient. Graph of [drug in plasma] vs time. </p>](https://knowt-user-attachments.s3.amazonaws.com/44f7aa93-b73f-4563-8f2c-ff2923fc2e6c.png)
Ineffective concentration (too low, not enough to bring about response), Critical concentration (achieves the correct response), and toxic effect (too much, has toxic effects on the patient). Correct timing of dosage used to bring about maintain critical concentration.
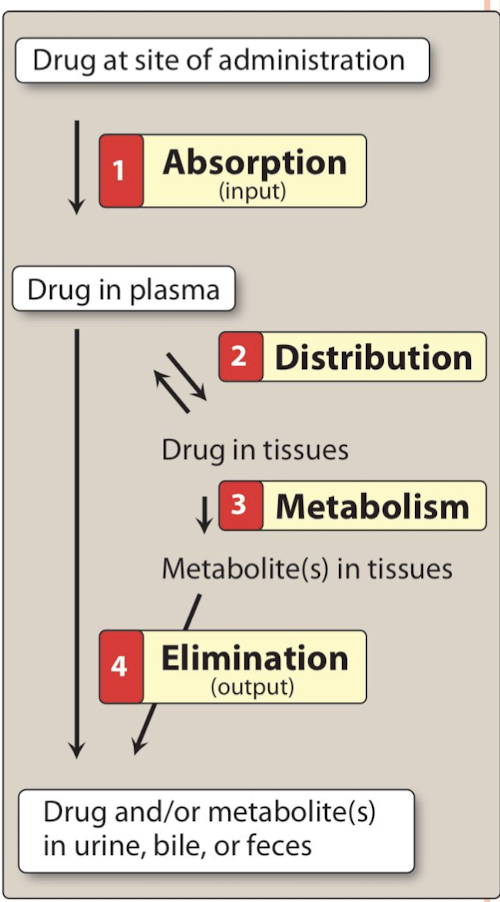
Absorption, Distribution, Metabolism, and Excretion (ADME)
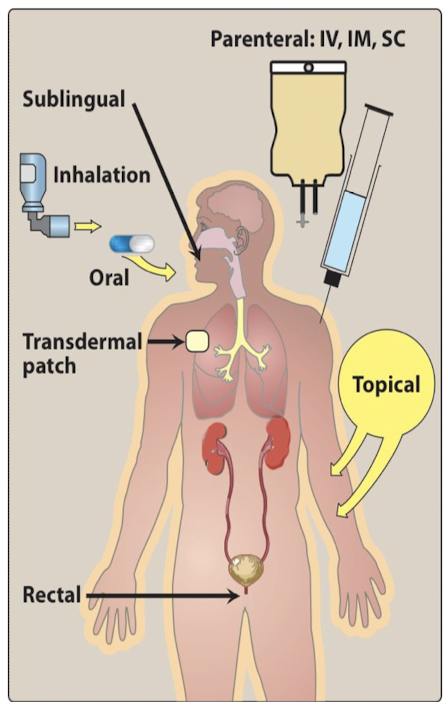
Design to get the right amount of drug to the right place at the right time. Ex. Oral, topic, parenteral, etc.
What does PK determine?
Speed of onset, the efficacy and duration of action of a drug
Biotransformation
"Happens in liver, kidneys, plasma, etc. Changing drug and modifying it."
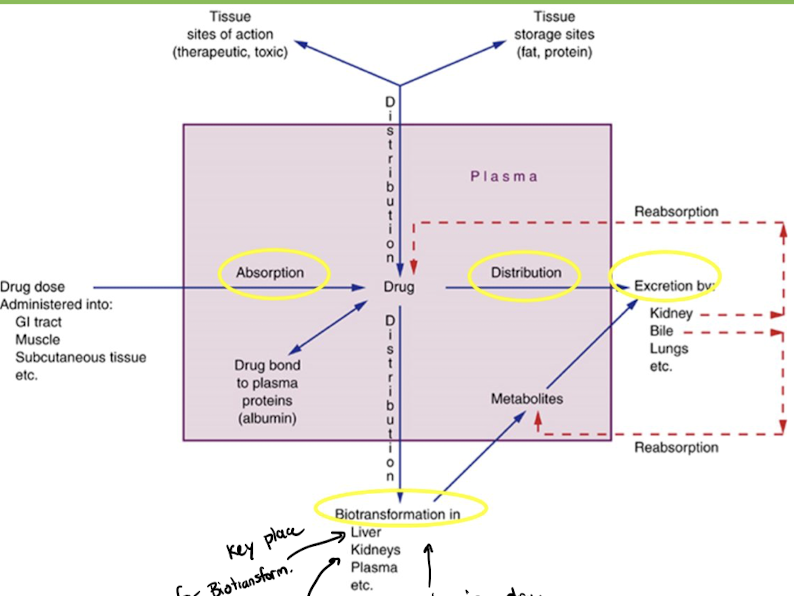
Pharmacokinetic Graph
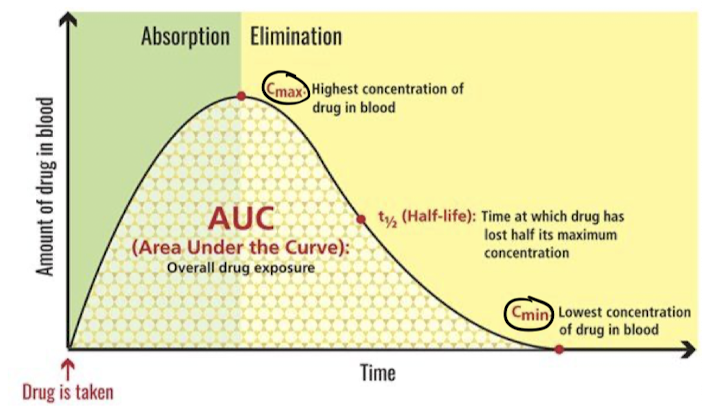
Critcal/Effective Concentration
The amount of a drug needed for a therapeutic effect
Loading Dose
A higher dose than usually used for treatment given in order to quickly reach the effective concentration
Pharmacokinetic Considerations
Onset of drug action, duration fo drug action (half-life), timing of the peak effect, metabolism or biotransformation of drug, site of excretion
Absorption
The movement of the drug from the site of administration into blood supply
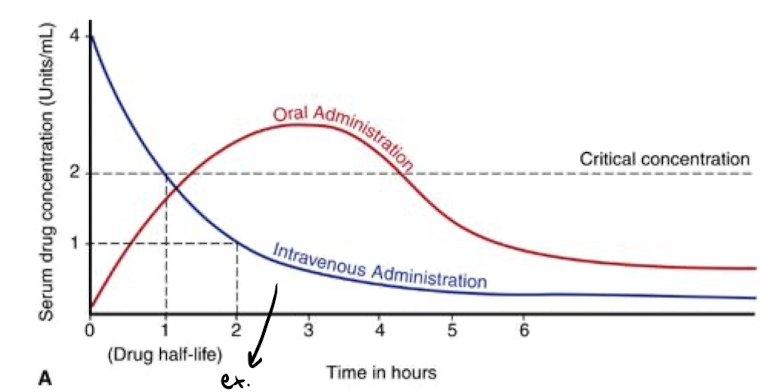
First-pass effect (metabolism)
Medications are extensively metabolized by the liver. Leads to some of the drug being metabolized before reaching the appropriate target site.
Bioavailability
The percentage of administered drug that reaches the systemic circulation.
- Ex. if 50mg are administered and 25mg are in the plasma, the bioavailability is 50%.
What is the bioavailability of a drug administered IV?
100% because does not need to be absorbed into the blood
Distribution
The movement of drugs throughout the body.
Give three examples describing distribution?
Protein-binding, blood-brain barrier, and placenta/breast milk
Metabolism
The enzymatic alteration of drug structure. Modifying the active drug.
Most important site of biotransformation (metabolism)
The liver
Why is metabolism important?
Process breaks down medications, and helps to prevent medications from causing adverse effects on the body
Excretion
Removal of drugs from the body
Most important site of excretion?
The Kidneys
Half Life
"The time it takes for the max concentration of drug in the plasma to decrease to 1/2 the peak level
What effects Half-life?
Absorption, distribution, metabolism, and excretion
First-order Kinetics
Constant fraction of the drug removed per unit time (ex. 50% removed every hour)
Zero-order kinetics
Constant amount of drug removed per unit time. Ex. 20mg removed every hour
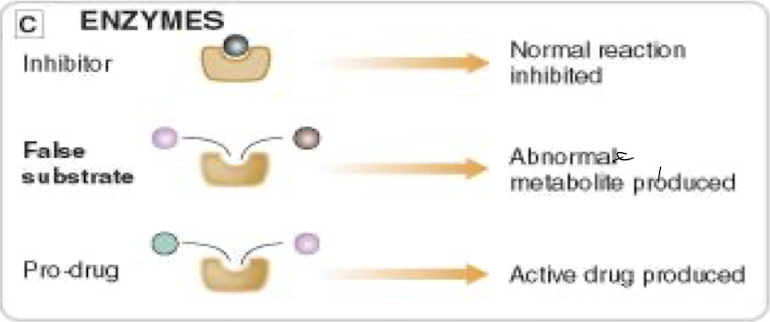
Drug Targets
Most drugs are effective by binding to proteins (some exceptions). Usually drug blocks the activity of the protein.
1) Receptors (regulatory proteins)
2) Ion channels
3) Enzymes
4) Carrier Proteins
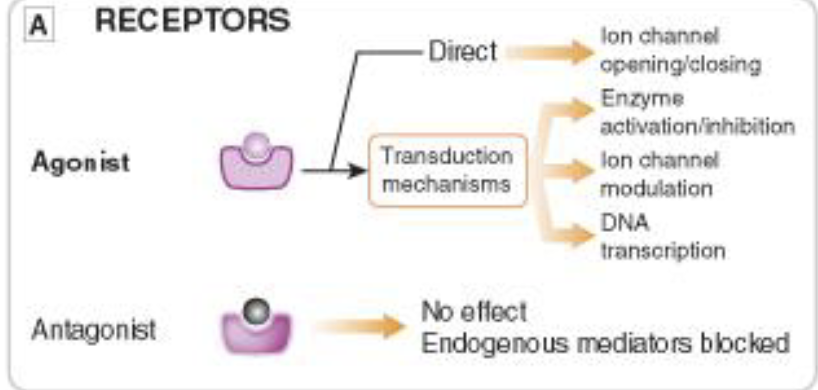
Receptors
"Most common drug target receptors. Lock and key mechanism.
Ion Channels

Enzymes
Transporters
Pharmacodynamics
Actions of the drug on the body
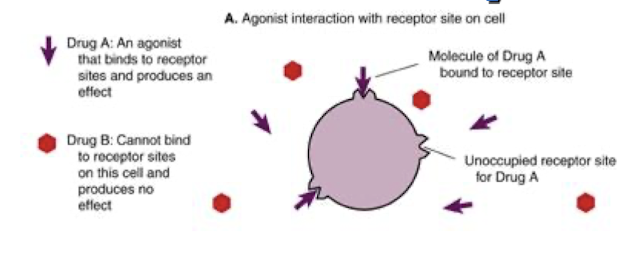
Receptor Agonists
"
- Bind to and activate the receptor bringing about a biological effect (key turns lock)
- Has affinity and intrinsic activity.
- ""Binds and activates""
- Stimulates a response
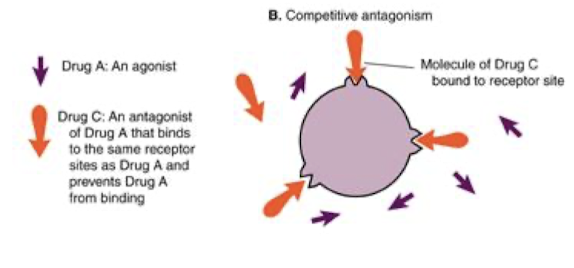
Receptor Antagonists
Bind to receptors and prevent agonists binding, thus keeping the receptor in the inactive state
Has affinity but no intrinsic activity
Prevents action of agonist
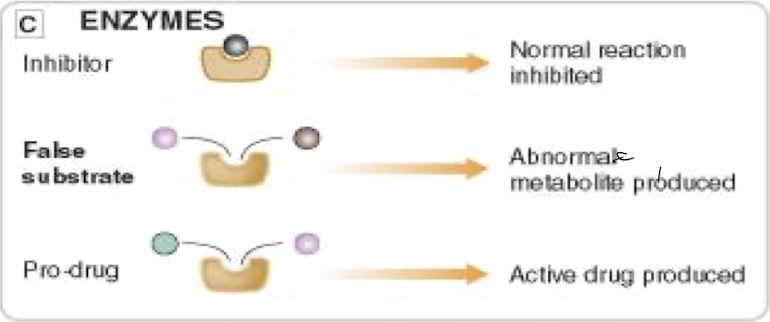
Log Dose-Response Curves (LDRs)
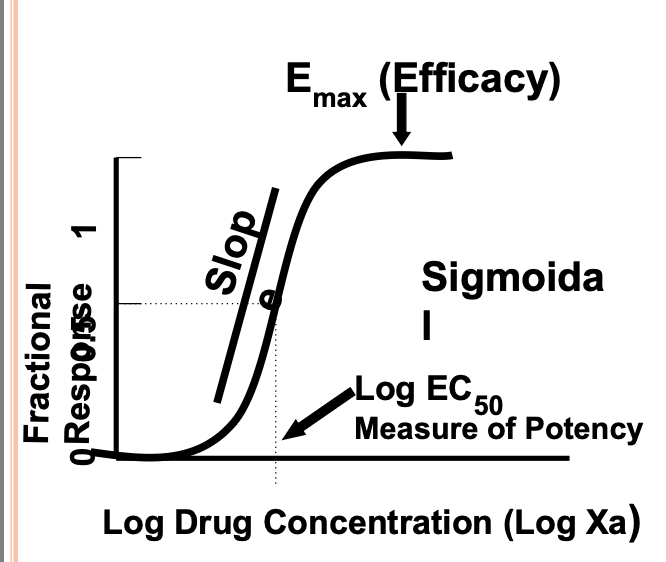
Efficacy
Maximal Effect the drug achieved in that context (at plateau on graph)
Major charactersistic influencing clinical utility of a drug
EC50
Concentration of drug bringing about 50% of the response
Potency
Described by the EC50 value. Lower EC50 = more potent. Depends on affinity and is influence by pharmacokinetics.
Slope
Steep slope means there is a small difference between barely effective and maximally effective does.
Steep Slope = narrow safe range
Important if upper effect is undesirable
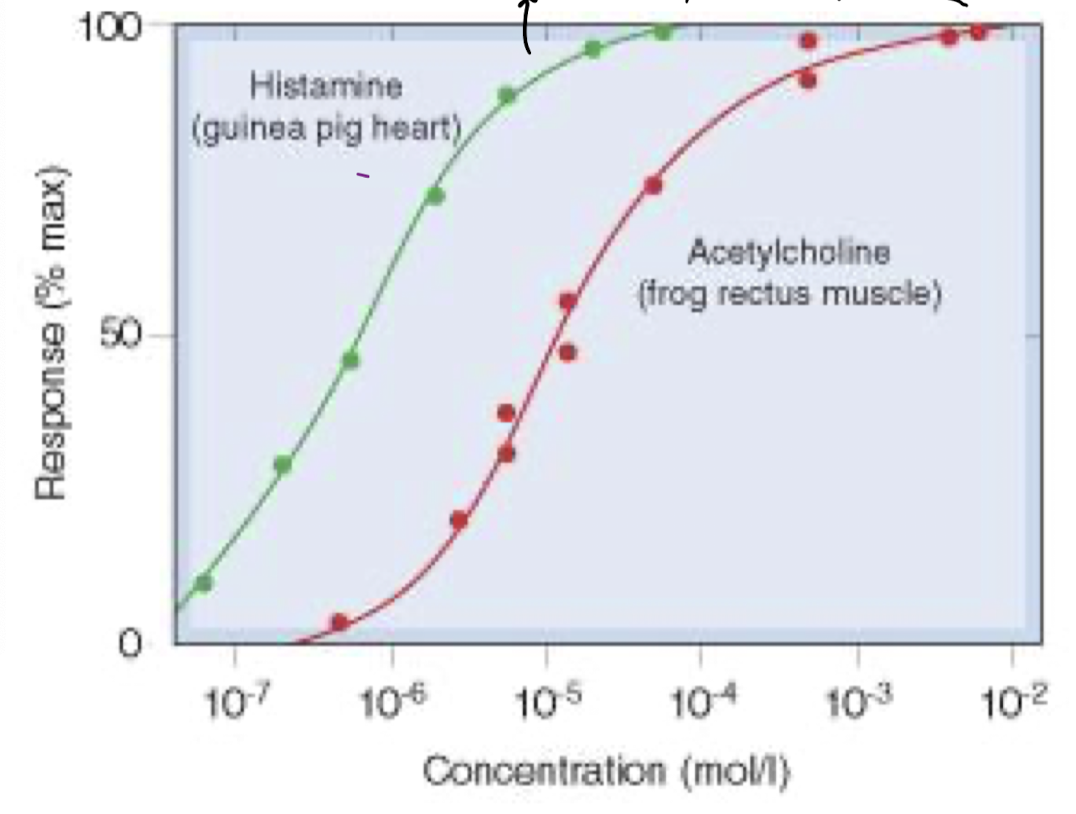
"Which drug is more potent? Efficacy?"
Histamine is more potent (lower EC50). The drugs have the same efficacy.
Agnoist Interaction
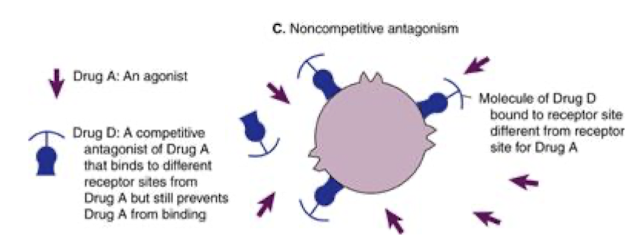
Competitive Antagonism
Noncompetitive Antagonism
LDR Curve Limitations
Can't be used if response is all-or-none
LDR curve from a single patient not representative due to biological variation
Quantal Dose Effect Curves
"Measure dose required to produce a specified effect in a large number of patients
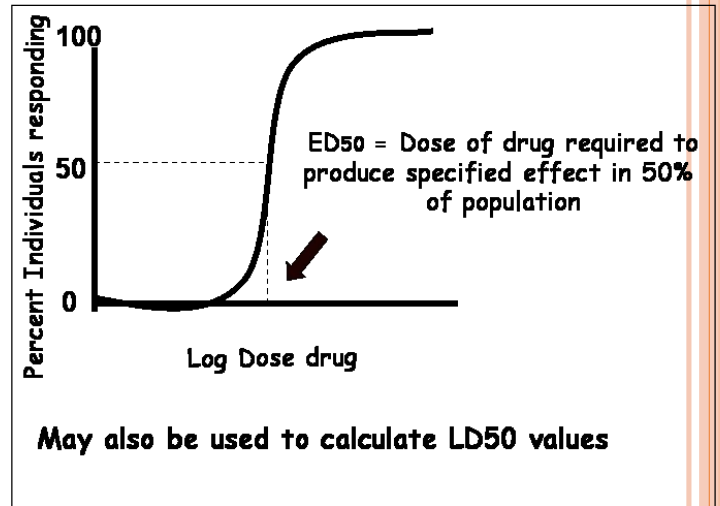
Therapeutic Index
Index of safety
LD50/ED50 or TD50/ED50
Larger TI means safer drug

LD50 and TD50
LD50 = Lethal dose in 50% of individuals
TD50 = Toxic dose (ex. vomiting) in 50% of individuals
5 ways of drug antagonism
1) Receptor block antagonism
- Rev. or irrev. competitive antagonism
2) Chemical Antagonism
- 2 substances combine in solution
3) Pharmacokinetic Antagonism
- Reduces [] of drug at site of action by modulating metab., abs., or exc.
4) Non-competitive Antagonism
- Blocks at some point in chain of events
5) Physiological Antagonism
- 2 drugs with opposing actions
4 Receptor Types
"Ligang-gated ion channels, G Protein-coupled receptors, Enzyme-linked receptors, and intracellular receptors.
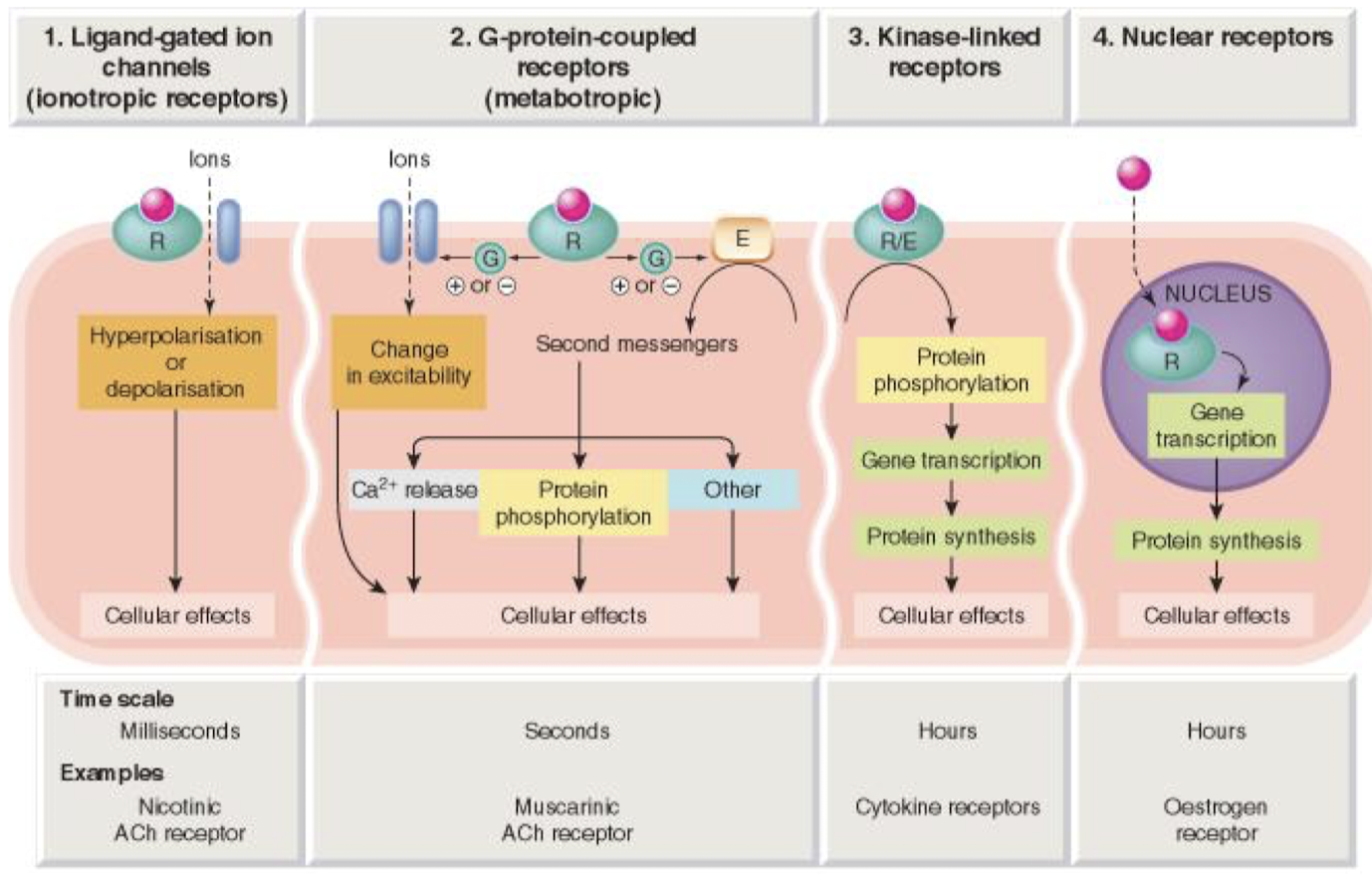
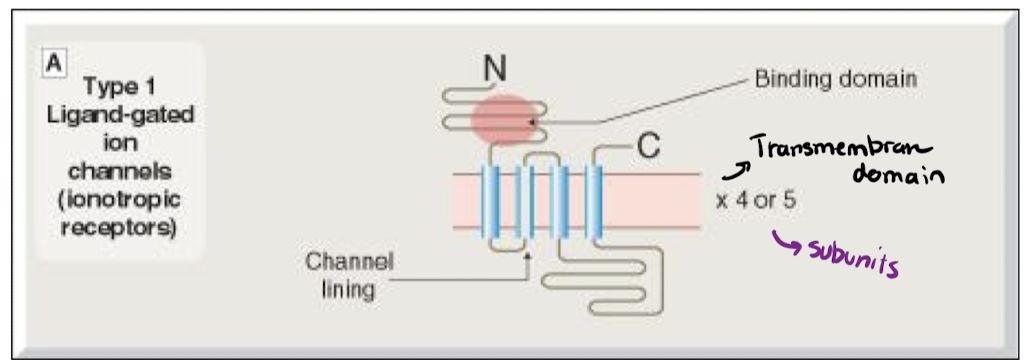
Ligand-Gated Ion Channels
"
Ion channels with a ligand binding domain (extracellularly)
Involved in fast (millisecond) neutrotransmission
G-Protein Coupled Receptors (GPCRs)
"
1 Polypetide chain (7 transmembrane domains)
Lignad-binding domain in membrane
3rd intracellular loop couples to G-protein
Also called serpentine receptors

GPCR Signalling
1) Homrone/NT binds to receptor. G protein has GDP.
2) Receptor changes shape and interacts with G protein. G protein releases GDP and binds GTP.
3) Subunit of G protein (alpha) dissociates and activates adenylyl cyclase which turns ATP into cAMP + PPi
5) Once hormone leaves, receptors reverts to resting state, and GTP is hydrolyzed to GDP. G-protein is inactivated.
Parts of a G Protein
Three parts. Alpha beta gamma.
Kinase-linked Receptors
"
Act by phosphorylation and tyrosine phosphorylation of other proteins
Single transmembrane alpha helix.
Do functions such as: mediate actions of growth factors, regulate gene transcription, etc.

Nuclear Receptors
"
Intracellular proteins
Receptor either in nucleus, or in cytoplasm + binds to agonist which moves to the nucleus
Receptors for steroids. Affects transcription etc.
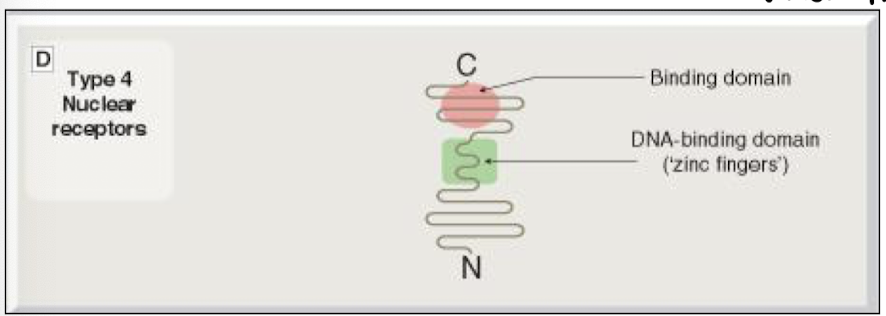
How many transmembrane receptors in each receptors?
LGIC: 4
GPCR: 7
KLR: 1
NR: 0
How many subunits in each receptor family?
LGIC: 4-5
GPCR: 1
KLR: 1
NR: 1
Specialized Domain of each receptor family?
LGIC: channel pore
GPCR: G-protein coupling domain
KLR: Enzymatic Domain
NR: Intracellular domain (Nucleus)
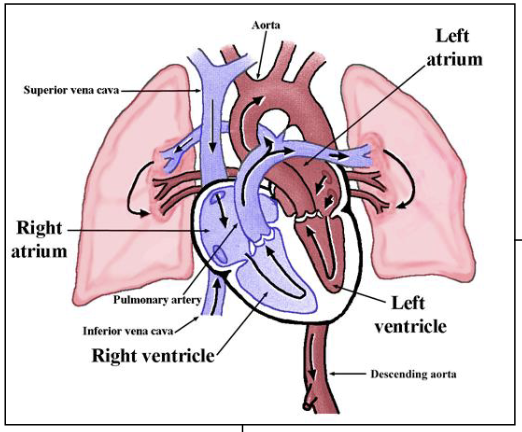
Cardiovascular System
A system composed of by a network of vessels (arteries, aterioles, capillaries, veins, and venules
4 functions of the CV system
Maintain homeostasis and favorable cellular environment
Provide continuous and controlled flow of blood through the capillaries to every cell
Deliver O2 and nutrients to cells
Exchange CO2 and waste (for elimination)
Components of the CV system and each of their subcomponents
Heart
1) Physiology
2) Electrophysiology
Blood Vessels
1) Arteries
2) Veins
3) Capillaries
Blood Cells
1) Erythrocytes
2) Leukocytes
3) Platelets
Physiology of the heart
"
Deoxygenated blood via pulmonary artery to the lungs.
Re-oxygenated blood from pulmonary vein to body via aorta.
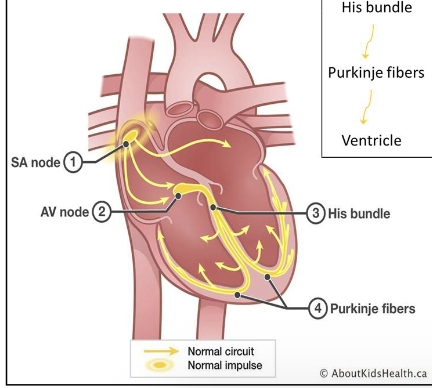
Electrophysiology
"The heart is electric. Co-ordination of contraction by a conducting system or ""nodes"".
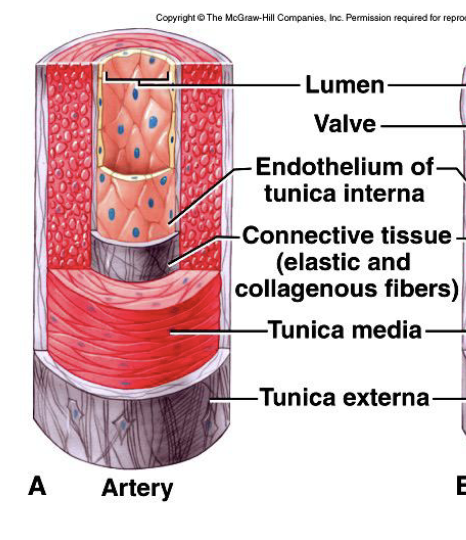
Arteries
"Tunica media: smooth mucle
- thickest layer providing support and changing vessel diameter to regulate blood flow and pressure
- lined by endothelial cells
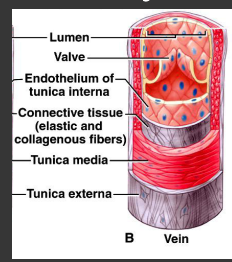
Veins
Less smooth muscle and connective tissue
Thinner walls - less pressure than in the arteries
Valves - blood flowing towar the heart (unidirectional flow)
Lines by endothelial cells
Erythrocytes
Anuclear
Contain Hb (hemoglobin)
Transport O2 to lungs
Leukocytes
"Defense Cells
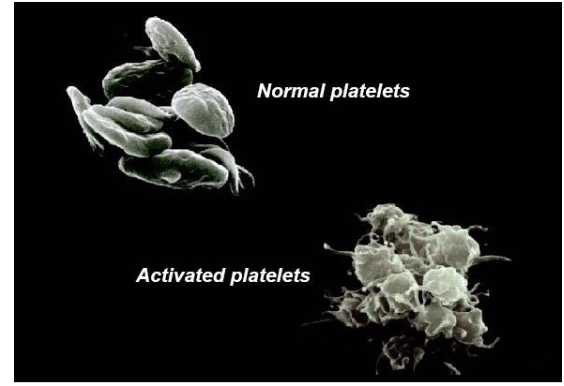
Platelets
"Form "plugs"" to stop leaks from blood vessels
Function of the Heart
Pace-making electrical signal
Force of Contraction
Function of Blood Vessels (3)
Presence of blockage
Muscular tone/structural integrity
Pressure drop needed to move blood to and through capillary beds
Function of Blood
Water, electrolye, iron balances
Lipid and protein composition
Types of cardiovascular disease (CVD)
1) Coronary Artery Disease (CAD)
2) Peripheral Artery Disease (PAD)
3) Heart Diseases (HD) {ie Angina, Heart Failure, Myocardial Infarction)
--> Note, not all CVD are HD
Adrenergic (or Autonomous or Sympathetic) Nervous System (ANS) regulation of the CV system
Smoothe muscle cells activity (contraction of relaxation)
- Rate and force of the heart
Sympathetic Nervous Systems and CV system
Sympathetic Nervous System
- Fight or flight
- Release CAs --> to Increase Heart Rate
Catecholamines (CAs)
Released by the SNS
- Adrenaline (or Epinephrine)
- Noradrenaline (or Norepinephrine)
Parasympathetic Nervous System (PNS)
PNS releases acetylcholine (ACh) to decrease heart rate
Types of Adrenergic Receptors
"α-adrenergic receptors
- α1 and α2
β-adrenergic receptors
- β1 and β2
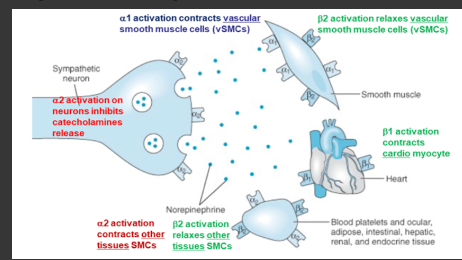
Functions of Adrenergic Receptors on smooth muscle blood vessels
"α1
- Constricts
α2
- Constrict/dilate
β1
- None
β2
- Dilate"
Functions of Adrenergic Receptors on Heart
"Alpha receptors have no effect on the heart. Only beta receptors.
β1
- Increase heart rate, increase force of contraction
β2
- Increase heart rate, increase force of contraction"
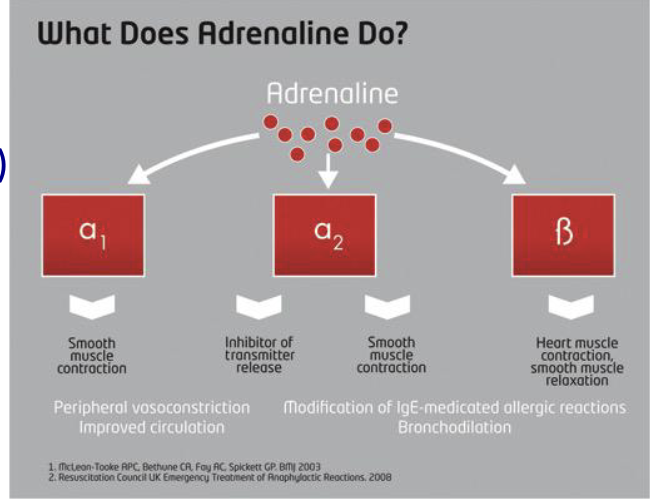
Adrenaline (or Epinephrine)
"Activates all adrenergic receptor subtypes.
Adrenergic Receptor (Cardiac Muscle)
"Cardiac Muscle
- β1 receptor increases force and rate of contraction"
Adrenergic Agonists (Vascular Smooth Muscle)
"- α1 --> contract vSMC in arterioles
-β2 -->relaxes (dilate) vSMC in skeletal muscle, liver, GI
- Alters cerebral and coronary blood flow"
Adrenergic Agonists (other muscles)
"Decrease uterine contractions
β2 receptors located on lung epithelium
- Bronchodilator (used for acute asthma attacks)"
Physiological and Pathological effects on the Heart of Catecholamines
"Physiological
β1 (cardio) receptors
- Increase intracell calcium
- Increase HR & force of contraction
- Increase cardiac efficiency
Pathological effects (can cause)
- Hypertension
- Cardiac Failure
- Myocardial Infarction"
Medical Use of Catecholamines
Cardiac arrest resuscitation
CV causes, symptoms, treatment: Anaphylaxis
- Peripheral Vasodilation
- Smooth muscle contraction
- Bronchoconstriction
Symptoms
- Increased capillary permeability (angio-, laryngeal, pulmonary edema)
- Hypotension
- Reduced consciousness
- Bradycardia (slow heart rate)
Treatment (Adrenaline) (Epi-pen)
- Increase in peripheral vascular resistance
- Improvement in blood pressure
- Reduction in angio-oedema
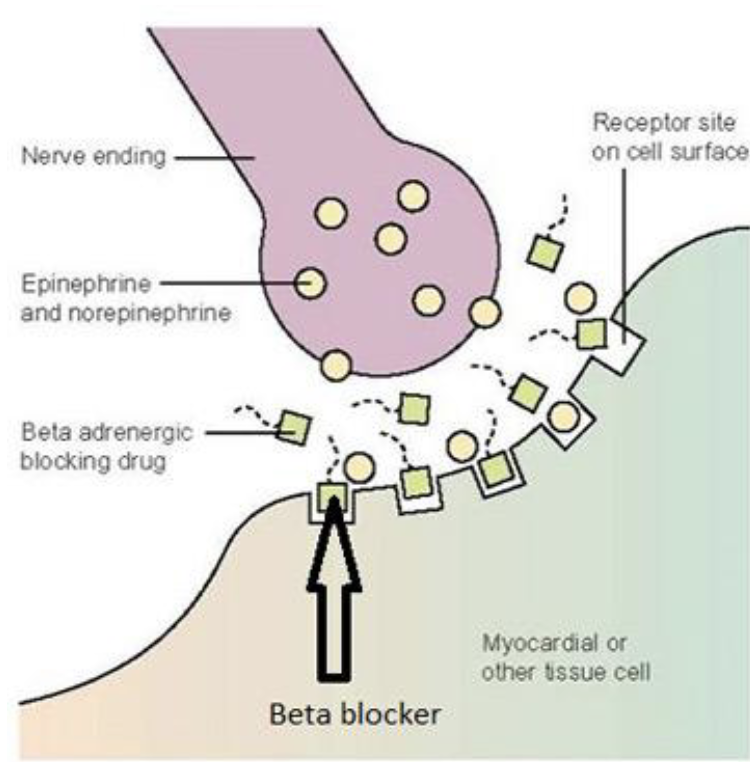
Catecholamine Antagonists
Endogenous (natural) (i.e. Adenosine)
- Exogenous (drugs) (i.e. Beta blockers)
β-Blockers
"Cardio-selective (β1) and Non-selective (β1 and β2) receptor antagonists
Used in:
- Angina: reduce cardiac work
- Hypertension: reduce cardiac output, renin release
- Post MI: Inhibit the increase in SNS activity
Side Effects:
Cardio-selective
- Do not have ""central"" effects
-*less risk of bronchoconstriction
Non-selective
- Nightmares depression, insomnia (crosses BBB)
- Bronchoconstriction (contraindicated in asthmatics)
- Hyperglycaemia (contraindicated in diabetics)
Heart Rate
Number of beats / minute
Stroke Volume (SV)
Volume of blood pumped out of the left ventricle during each sestolic cardiac contraction
Cardiac Output (CO)
Heart rate * Stroke Volume
- amount of blood the heart pumps in one minute
Venous return (preload)
Flow of blood from periphery back to the right atrium. Determines the volume in ventricle at each beat.
Peripheral Resistance (afterload)
Determines the arterial pressure that must be overcome by the pumping system.
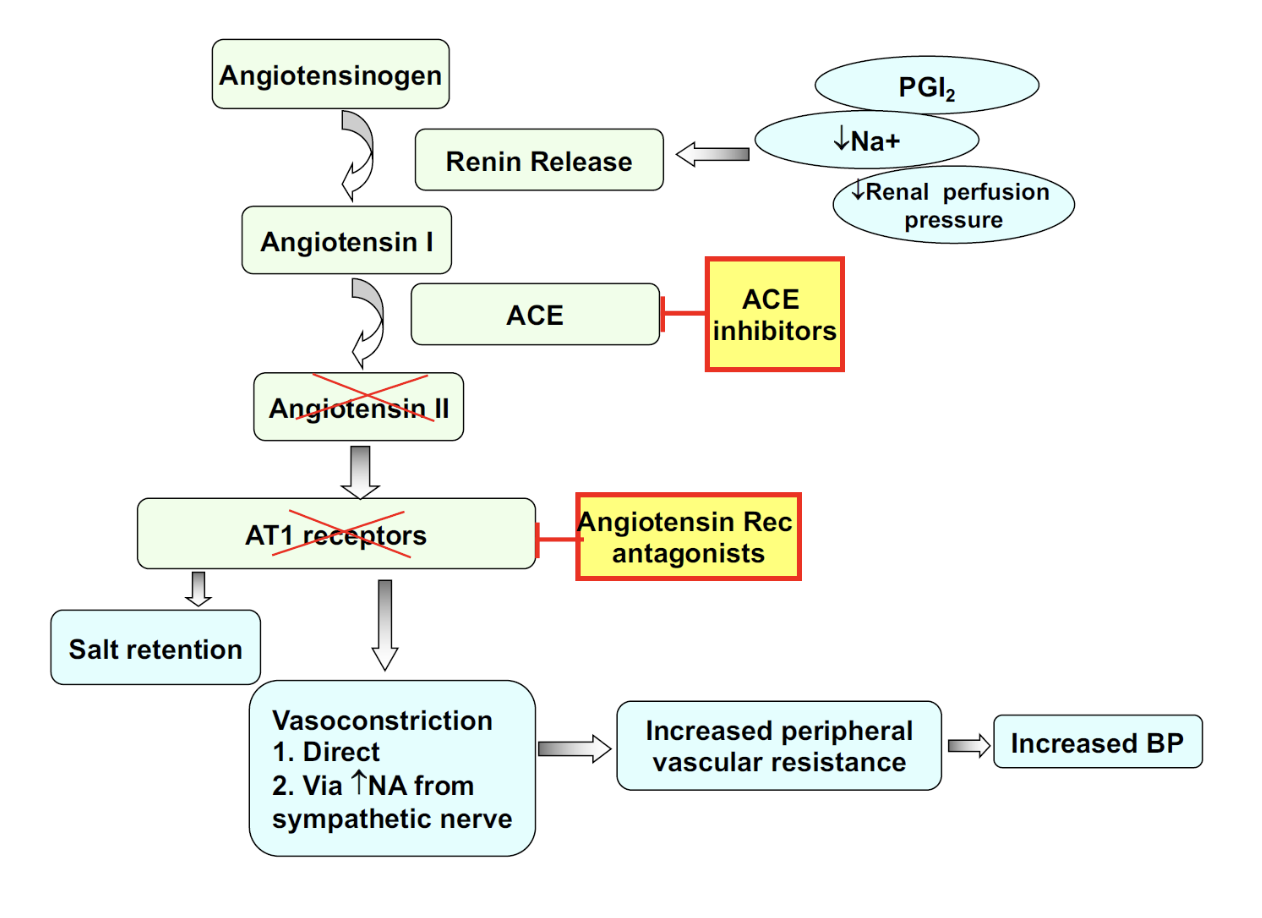
Renin-Angiotensin-System
"Red boxes are inhibitors