1 - Renal Physiology, Structure of the Kidney, Glomerular Filtration
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
The kidney helps control or regulate many substances in the body. These include (8)
Body water
Electrolyte levels – Na+, K+, Cl
H+ and bicarbonate – acid base balance
Elimination of wastes, drugs, toxins ↑ new glucose
Gluconeogenesis
Long term regulation of blood pressure
Regulates red blood cell count or hemoglobin levels
Involved with Ca++ homeostasis
How does the kidney contribute to gluconeogenesis?
Produces glucose for circulation, liver is main organ for gluconeogenesis
How does the kidney contribute to regulation of red blood cell count or hemoglobin levels
produces erythropoietin → stimulates erythrocyte production
How does the kidney contribute to Ca++ homeostasis
activates vitamin D
What parts of the nephron are mainly located in the cortex of the kidney? (6)
Bowman’s capsule
Distal convoluted tubule
Glomerulus
Proximal convoluted tubule
Renal corpuscle
Part of collecting duct
What parts of the nephron are located in the medulla of the kidney? (2)
Loop of Henle
Part of collecting duct
I’m not sure if this happens, but if a blood clot developed in the afferent arteriole, it would most likely
A. Prevent blood from entering the glomerulus
B. Prevent blood from exiting the glomerulus i
C. Prevent filtrate from entering the proximal tubule
D. Prevent filtrate from exiting the proximal tubule
A. Prevent blood from entering the glomerulus
If a water molecule was to be reabsorbed from the proximal tubule back into the blood, where would it enter the blood?
A. Collecting duct
B. Efferent arteriole
C. Glomerulus
D. Peritubular capillary
E. Vasa recta
C. Glomerulus - filtration
D. Peritubular capillary - To enter proximal tubule
E. Vasa recta - a vessle in the medulla
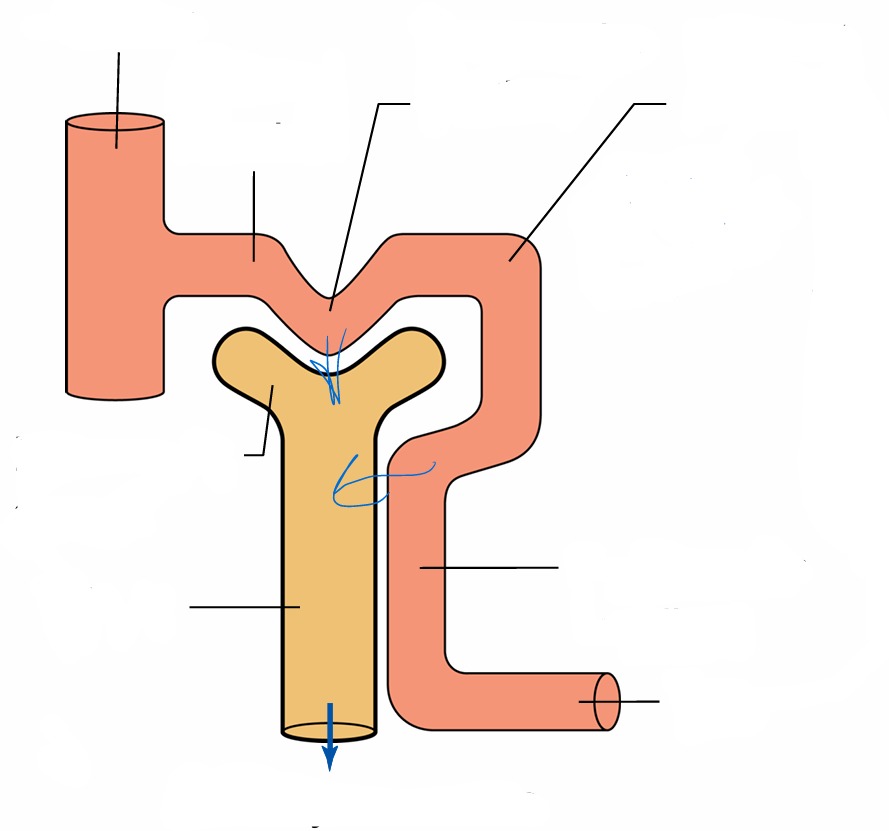
Lable
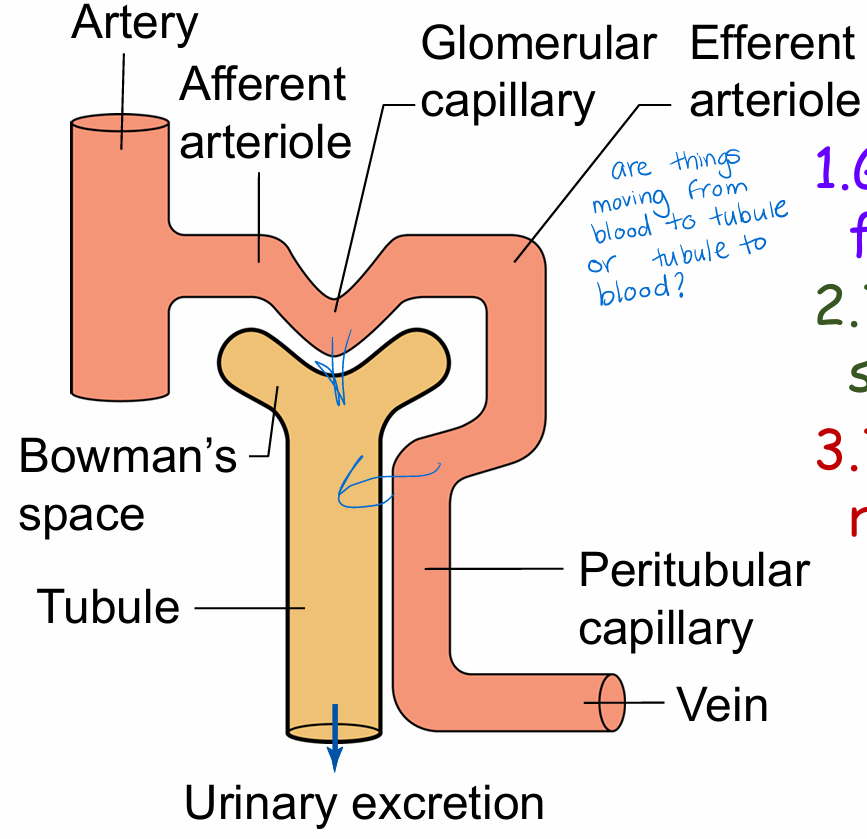
The 3 processes involved in urine production
Glomerular filtration - Blood to tubule
.Tubular secretion
.Tubular reabsorption - tubule to blood
These 3 basic renal processes determine
how much of a substance is excreted (or how the kidney does some of its main jobs!)
Substance excretion calculation
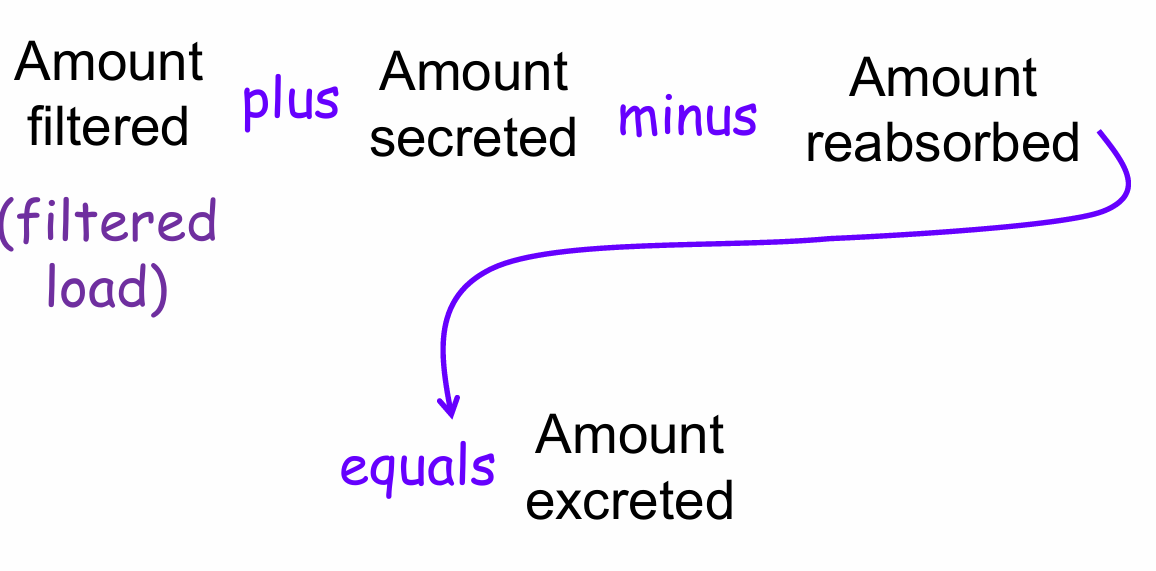
If the amount excreted is greater than the filtered load, this means that the substance was also
D. Reabsorbed
E. Secreted
E. Secreted
Either none, some, or all of a substance that enters the kidney can be excreted depending on (3)
How much is filtered
How much is secreted and reabsorbed
How much of each substance is excreted
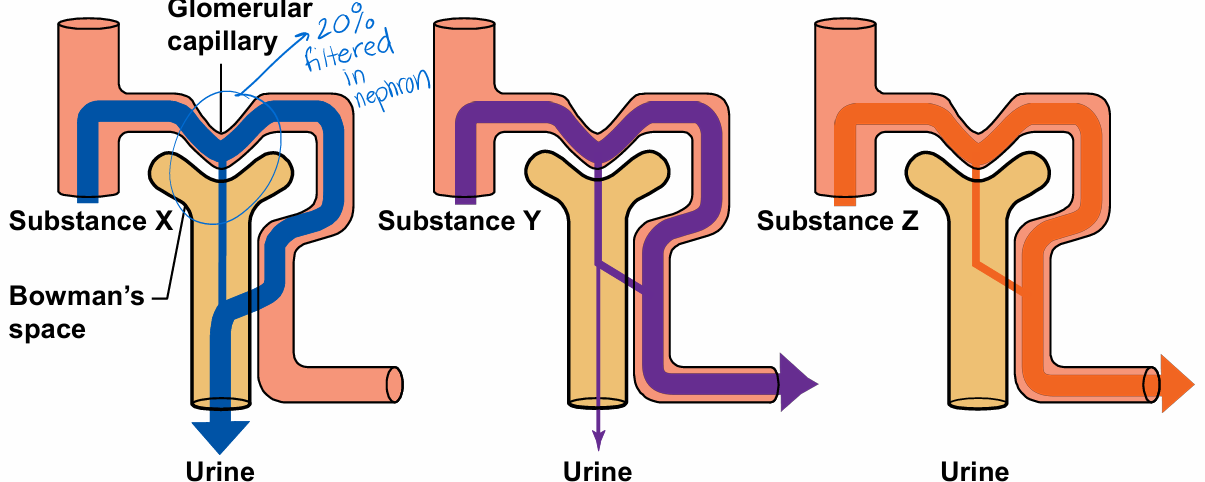
How much of each substance is excreted?
What is the glomerular filtration barrier supposed to do? (3)
1. Enable high filtration rates of water
2. Allow nonrestricted passage of small and middle-sized molecules
3. Prevent almost all serum albumin, large proteins, and cells from passing through
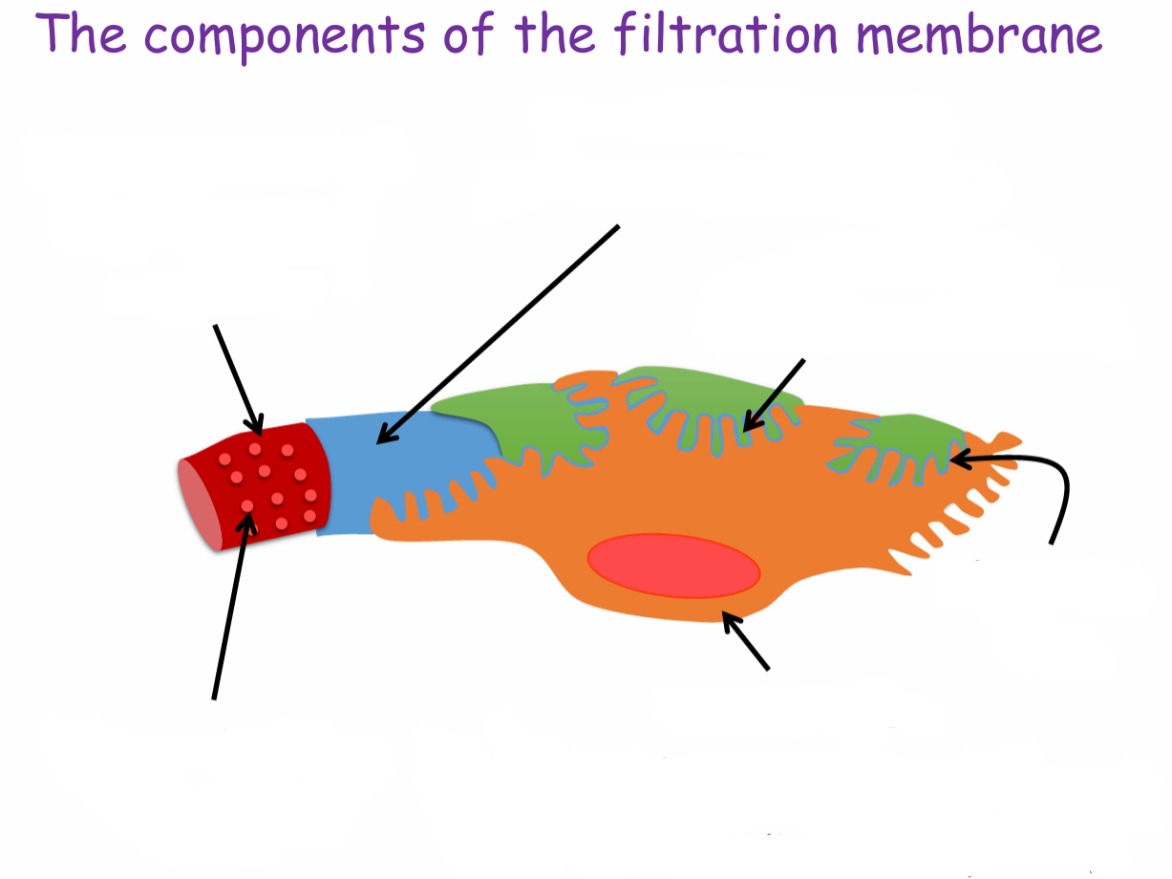
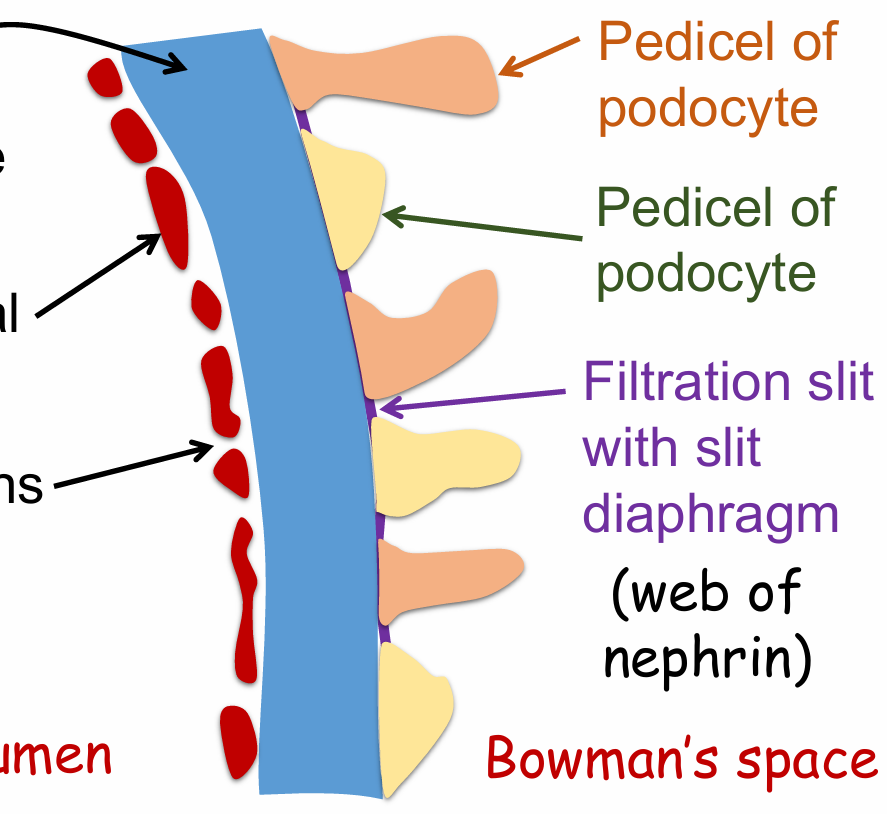
Lable components of the filtration membrane
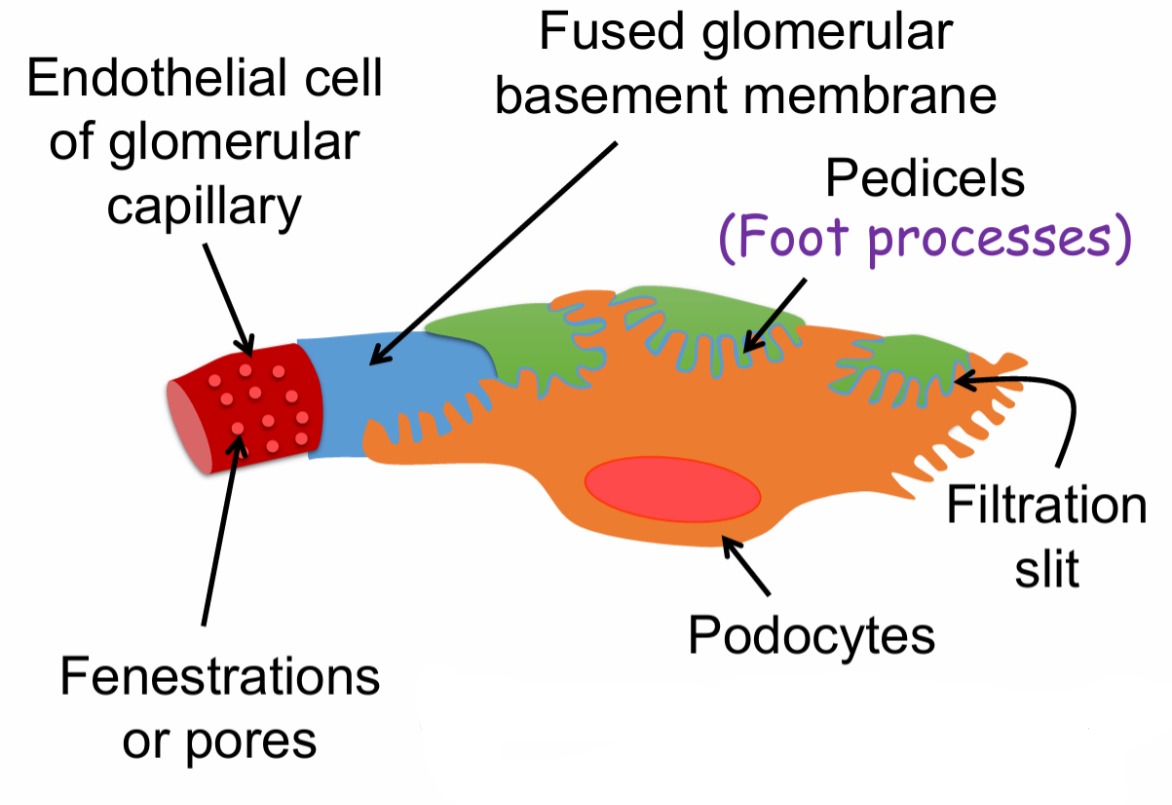
What are podocytes
Epithelial cell of the visceral layer of Bowman’s capsule
Parts of the filtration membrane in the capillary lumen (3)
Basement membrane
Endothelial cells
Fenestrations
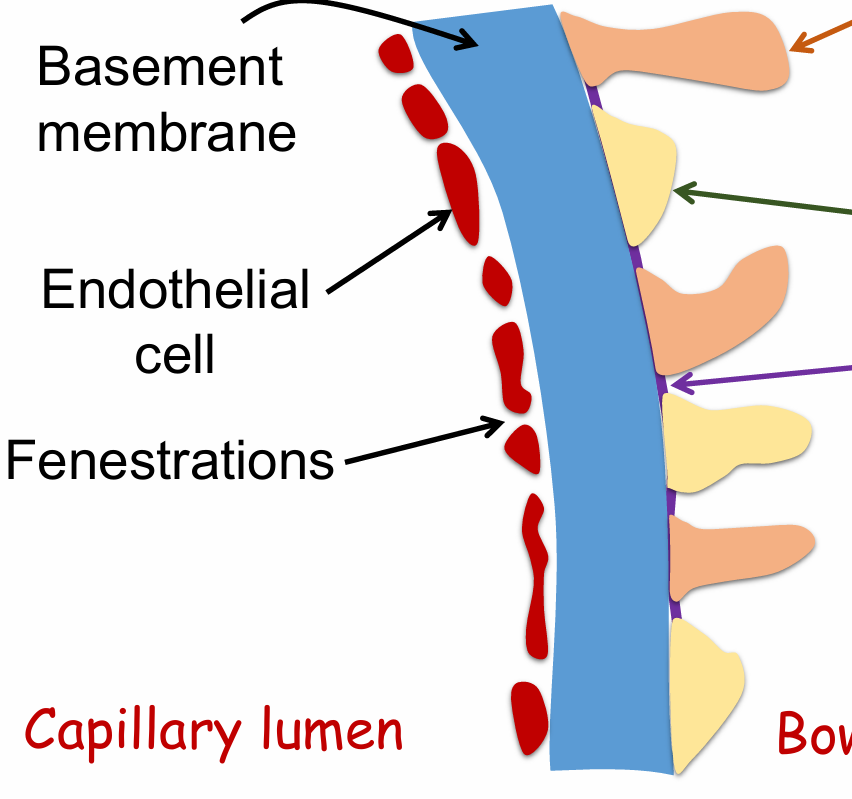
Parts of the filtration membrane in the bowman’s space (2)
Pedicel of podocyte
Filtration slit with slit diaphragm (web of nephrin)
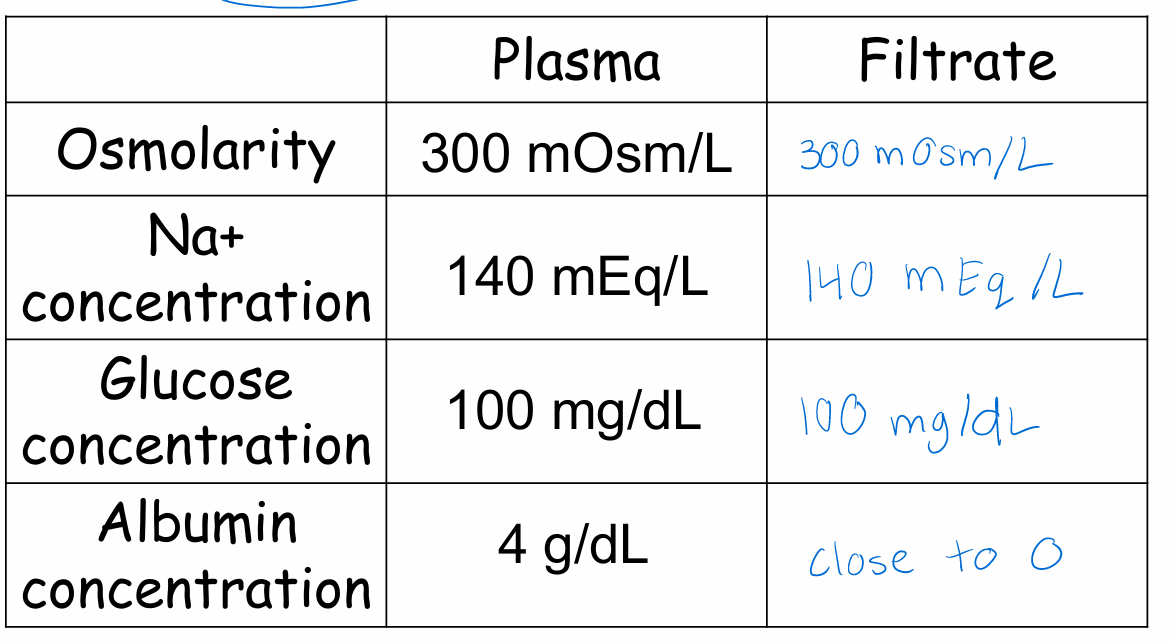
What is freely filtered?(5) What is not?(2)
Freely filtered
water
electrolytes
glucose
amino acid
urea
Not
Larger proteins
Cells
How filtration occurs
Fluid (i.e. what will be the filtrate) moves from the glomerular capillary to Bowman’s space via bulk flow
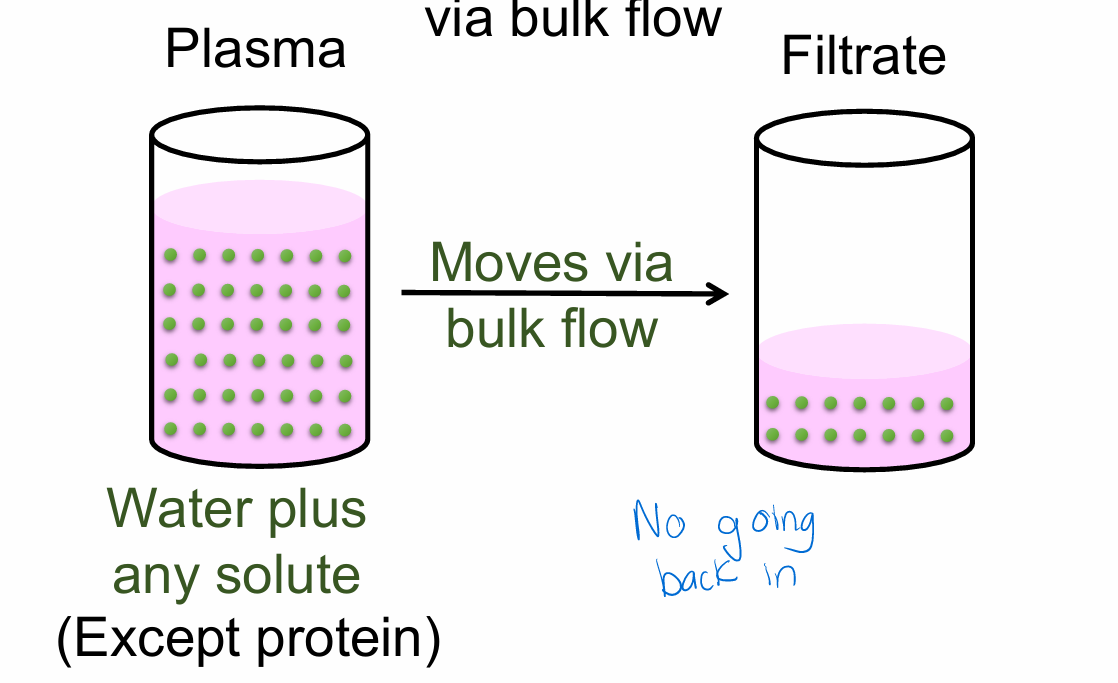
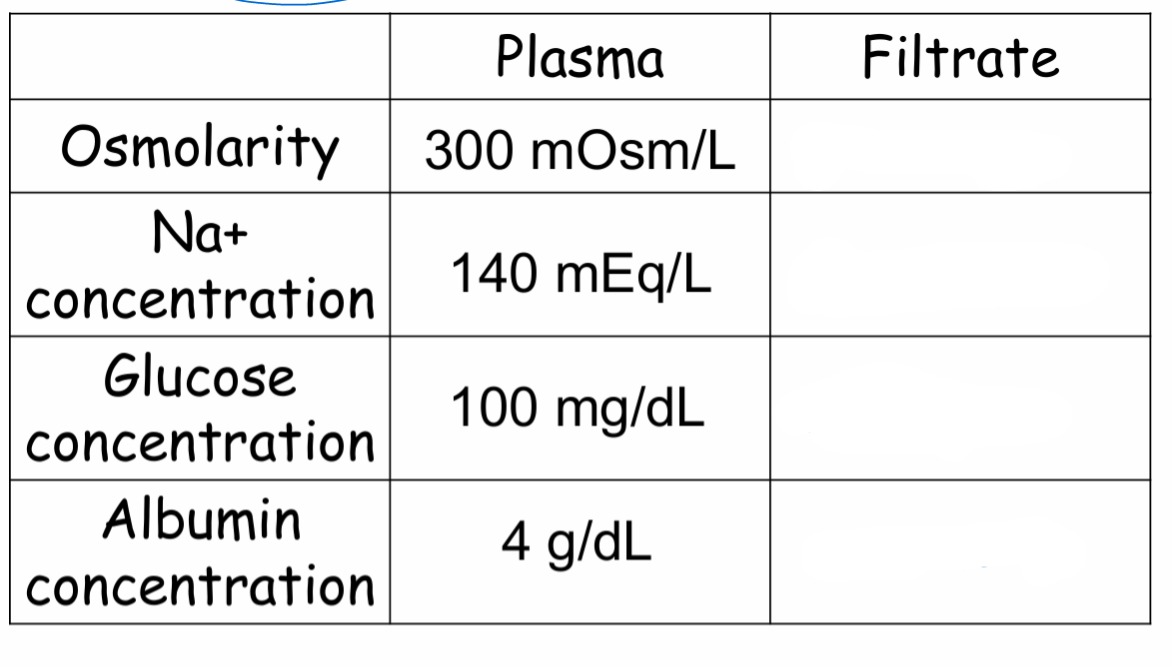
How does the filtrate that is produced compare to plasma?
Same concentration
The forces that affect filtration
Starling forces
Hydrostatic pressure - the pressure
of the fluid
Oncotic pressure - the pressure of protein in the fluid
Which forces will promote (P) and which forces will oppose (O) filtration (the movement of fluid from the blood to Bowman’s capsule)?
Glomerular capillary hydrostatic pressure (PGC)
Glomerular capillary oncotic pressure (πGC)
Hydrostatic pressure in Bowman’s space (PBS)
Colloid osmotic or oncotic pressure in Bowman’s space (πBS)
Glomerular capillary hydrostatic pressure (PGC) - P
Glomerular capillary oncotic pressure (πGC) - O
Hydrostatic pressure in Bowman’s space (PBS) - O
Colloid osmotic or oncotic pressure in Bowman’s space (πBS) - P
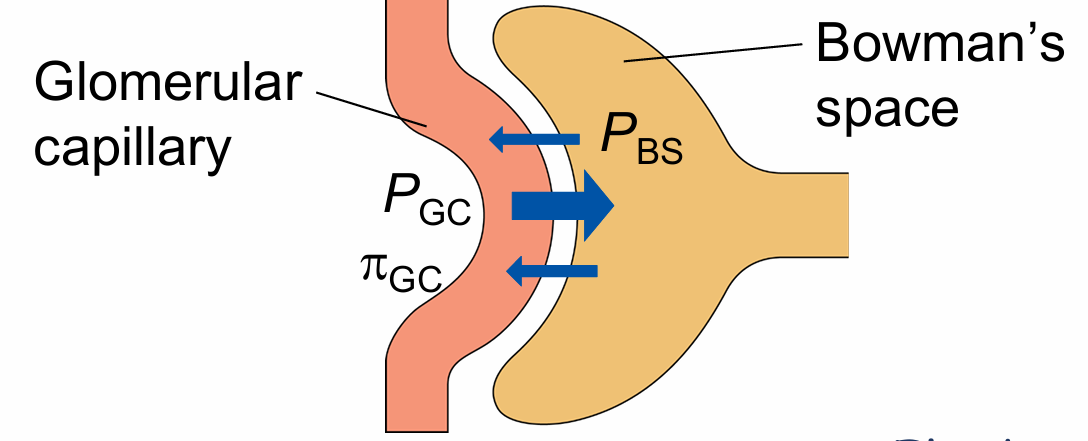
Net filtration pressure or ultrafiltration pressure calculation
Net effect: (PGC – PBS – πGC) = Fluid is filtered
*Normally, the amount of protein in the filtrate is so small, that BS pressure is 0)
What else affects glomerular filtration? (2)(1)
Hydraulic permeability of the filtration membrane
Surface area of the filtration membrane
Also known as Kf - filtration coefficent
Glomerular filtration equation
Kf x net filtration pressure
All of these same forces affect filtration in other capillary beds (e.g. in skeletal muscle)
So why is the end result so different in the kidney (that is, about 20% of plasma flowing through the glomerulus is filtered)? (1)(4)
Because, compared to other capillary beds:
Kf is much higher - Due to the design of the filtration membrane
PGC is much higher - Due to the higher resistance in the efferent arteriole compared to a venule!
Low resistance in renal arterial
High resistance in efferent arterial
GFR in young healthy kidney
125 mL/ min or 180 L/ day
GFR is regulated. But how?
Change in the net filtration pressure
How can the net filtration pressure, and hence GFR, change?
PGC - Controlled changes in GFR. Adjusted to suit the body’s needs
PBS, πGC, πBS - Uncontrolled changes in GFR, Change mainly when something is wrong
Without any type of compensation, what will happen to PGC and GFR if blood pressure or mean arterial pressure goes down?
PGC will decrease
GFR will decrease
But PGC, and hence GFR, can be adjusted by constricting or dilating the afferent or efferent arteriole
How will dilation of an arteriole affect blood flow?
Increase blood flow
What will happen to PGC and GFR if the afferent arteriole is dilated (efferent arteriole stays the same)?
PGC will increase
GFR will increase
More blood flow in
What will happen if you constrict the afferent arteriole?
Decrease GFR
What will happen to PGC and GFR if the efferent arteriole is dilated (afferent arteriole stays the same)?
PGC will decrease
GFR will decrease
What will happen if you constrict the afferent arteriole and the efferent arteriole to the same degree?
GFR stays the same
Take home message about MAP and filtration
MAP can fluctuate throughout the day.
Despite changes in MAP, within a certain range, GFR remains fairly constant by dilating or constricting the afferent or efferent arteriole.
Autoregulation
If a person becomes very dehydrated causing the plasma protein concentration to increase, what will happen to GC and GFR?
πGC will increase
GFR will decrease
πGC = blood colloid osmotic or oncotic pressure
Think water stays with or is attrackted to protein
What will happen if the filtration membrane is damaged and becomes more permeable to protein?
πBS will increase
GFR will increase
πBS = Bowman’s space colloid osmotic or oncotic pressure
What will happen if a person develops a kidney stone that gets stuck in the ureter and blocks the outflow of urine from the kidney?
PBS will increase
GFR will decrease
PBS = Bowman’s space hydrostatic pressure
Determinants of PGC (3)
Mean arterial pressure
Resistance at the afferent arteriole
Resistance at the efferent arteriole