W34 L1 - Female Reproduction
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
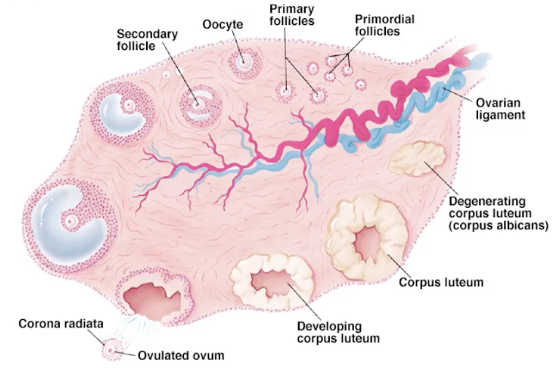
describe the ovary
elliptical structure
2-4cm long
~7million oogonia develop into ~ 500,000 primary oocytes
each oocyte contained in a primary follicle
outer layer of granulosa cells
develops outer layer of cells known as theca
give a brief overview of the different stages of an egg
primordial follicle - single immature egg surrounded by single layer of supporting cells; resting state which eggs are stored in ovary
primary follicle - egg that has been recruited to start growing at beginning of each monthly cycle
secondary follicle - are multiple layers of cells surrounding the egg. Also, fluid-filled spaces start to appear within these layers
what is an oocyte
an egg
what is the ovary comprised of
a thick cortex filled will follicles, a small central medulla filled with nerves and vessels
how many eggs are used each month
~ a couple dozen primordial follicles to become primary follicles
they grow
the largest and quickest developing of them become recruited into that month cycle and continue to develop
slower ones undergo atresia and apoptosis
~ 6 follicles keep growing
by the time it comes to ovulation, you have a single dominant follicle for a human that releases an egg
what does a follicle consist of
An oocyte: The central germ cell that has the potential to be fertilized.
Surrounding somatic cells: These cells provide nourishment, protection, and regulatory signals to the developing oocyte. These include:
Granulosa cells: A layer (or multiple layers as the follicle matures) of cells directly surrounding the oocyte. They play a crucial role in oocyte development and hormone production.
Theca cells: A layer of cells located outside the granulosa cells. They contribute to hormone production, particularly androgens, which are then converted to estrogens by the granulosa cells. derived from the same precursor cells as muscle cells so have some muscle-like characteristics
Theca interna: hormone secreting
Theca externa: muscular capsule
how is female germ cell meiosis distinct from that of males
Timing is Different:
In females, the process starts way before birth. The early stages of meiosis begin in the ovaries of a female fetus (prenatally). However, it gets paused at a specific point (the primary oocyte stage) and doesn't continue until puberty.
In males, meiosis doesn't start until puberty.
Unequal Cytoplasm Division:
When a female germ cell divides during meiosis I, it splits into two cells of very different sizes. One gets almost all the cytoplasm (the watery stuff inside the cell) and becomes the secondary oocyte (which can potentially become the egg). The other gets very little cytoplasm and is called a polar body. This polar body usually just breaks down.
In males, when a germ cell divides, it splits more evenly into two cells of roughly the same size.
Meiosis II Completes Differently:
In females, the secondary oocyte starts meiosis II after ovulation but gets paused again! It only completes meiosis II if it gets fertilized by a sperm. If there's no sperm, it doesn't finish the process. (entry of sperm into egg triggers egg to complete second division)
when meiosis II ceises, chromosomes remain linked by chiasmata
can be like this for 20, 30, 40 years waiting to be ovulated
stored with replicated DNA like this because safest way - if a bit of DNA gets damaged its got an undamaged template copy to repair it
In males, meiosis II goes all the way to completion, resulting in four functional sperm cells.
One Functional Gamete vs. Many:
The end result of female meiosis (if fertilization happens) is typically one functional egg cell (ovum) and a couple of polar bodies that don't develop further. This makes sense because the egg needs to be big and have lots of nutrients to support a developing embryo.
The end result of male meiosis is four functional sperm cells, which are small and mobile, designed to travel and fertilize the egg.
when does the egg cell become haploid
when it gets the next set of chromosomes from the sperm
never spends extended time in haploid state
what is anisogamy
reproductive system characterized by differentially-sized male and female gametes
most successful strategy for reproduction
what does endocrine mean
long distance signalling via the blood stream
what does paracrine mean
short range signalling - a cell talks to its neighbours
what does autocrine mean
self signalling - a cell expresses a signalling molecule and the receptor for that molecules
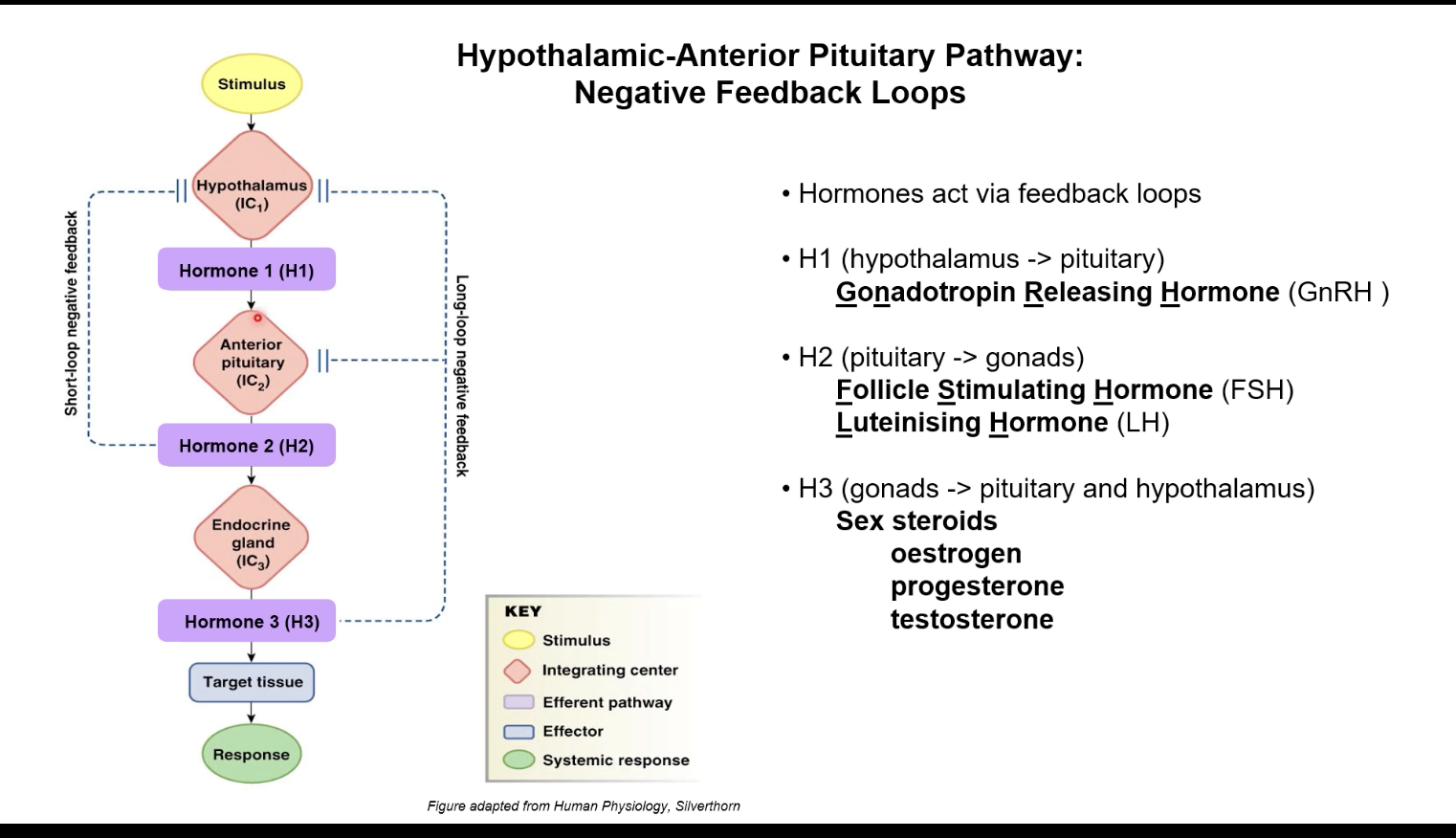
describe the negative feedback loop for the release of hormones
Stimulus: Something in your body signals a need for a change.
Hypothalamus (Integrating Center 1 - IC₁): The hypothalamus receives this signal and releases Hormone 1 (H1). In the case of the reproductive system, this H1 is Gonadotropin Releasing Hormone (GnRH). GnRH travels a short distance to the anterior pituitary.
Anterior Pituitary (Integrating Center 2 - IC₂): The hypothalamus's hormone (H1) tells the anterior pituitary to release Hormone 2 (H2). For the gonads, these H2 hormones are Follicle Stimulating Hormone (FSH) and Luteinizing Hormone (LH). FSH and LH travel in the bloodstream to the gonads.
Endocrine Gland (Integrating Center 3 - IC₃) / Gonads: The hormones from the anterior pituitary (H2) stimulate the endocrine gland (in this example, the gonads) to release Hormone 3 (H3). These H3 hormones are sex steroids like oestrogen, progesterone (mainly in females), and testosterone (mainly in males).
Target Tissue: Hormone 3 (H3) travels in the blood to its target tissues in the body, causing a response.
Negative Feedback: This is the crucial part for regulation! Hormone 3 (H3) can then act as a signal to go back to the brain and tell it to slow down the release of the earlier hormones (H1 and H2). There are two main types shown:
Long-loop negative feedback: Hormone 3 (from the gonads) travels all the way back to the hypothalamus and/or the anterior pituitary to inhibit the release of H1 and/or H2. It's like the final product telling the factory to make less.
Short-loop negative feedback: Hormone 2 (from the anterior pituitary) can also go back to the hypothalamus to inhibit the release of H1. It's like a middle manager telling the boss to slow down.
what does negative feedback with a delay result in
results in a cycle
like the menstrual cycle
what hormones do the gonads secrete
oestrogens
androgens
inhibin
activin
follistatin
AMH
what hormones does the planceta secrete
CG - chorionic gonadotrophin, hCG
PL - placental lactogen, hPL
what hormones in regards to reproduction does the anterior pituitary gland secrete
LH
FSH
what hormones in regards to reproduction does the hypothalamus secrete
GnRH - gonadotrophin-releasing hormone
which hormones are glycoprotein hormones
FSH
LH
Activin
Inhibin
AMH
hCG
what are the glycoprotein hormones like
large molecules
highly charged
very water soluble
travel well in bloodstream due to their charge & how they interact with water
means they cannot cross a plasma membrane though
need a cell surface receptor sitting on surface of the cell able to respond to that hormone
how do FSH and LH act
they act through cell surface receptors which then send a secondary message within the cell due to their glycoprotein hormone characteristics
What is a key characteristic of "nuclear hormones," and what are some examples?
Lipid based - typically transported around body by binding to protein carriers
Non polar - dissolve easily in oils and water; dissolve across cell membrane
They can go directly into the nucleus (the control center) of a cell to tell the DNA what to do.
(not a scientific category like steroid hormones and peptide hormones)
Think: "Nuclear" like the nucleus of a cell!
Examples:
Steroid Hormones: These are made from cholesterol and include:
Estrogen
Testosterone
Cortisol
Thyroid Hormones: T3 and T4 (important for energy and growth).
How they work (simplified):
They are usually small and can slip through the cell's outer layer.
Inside, they bind with receptors.
Translocate into nucleus and transcribe target genes
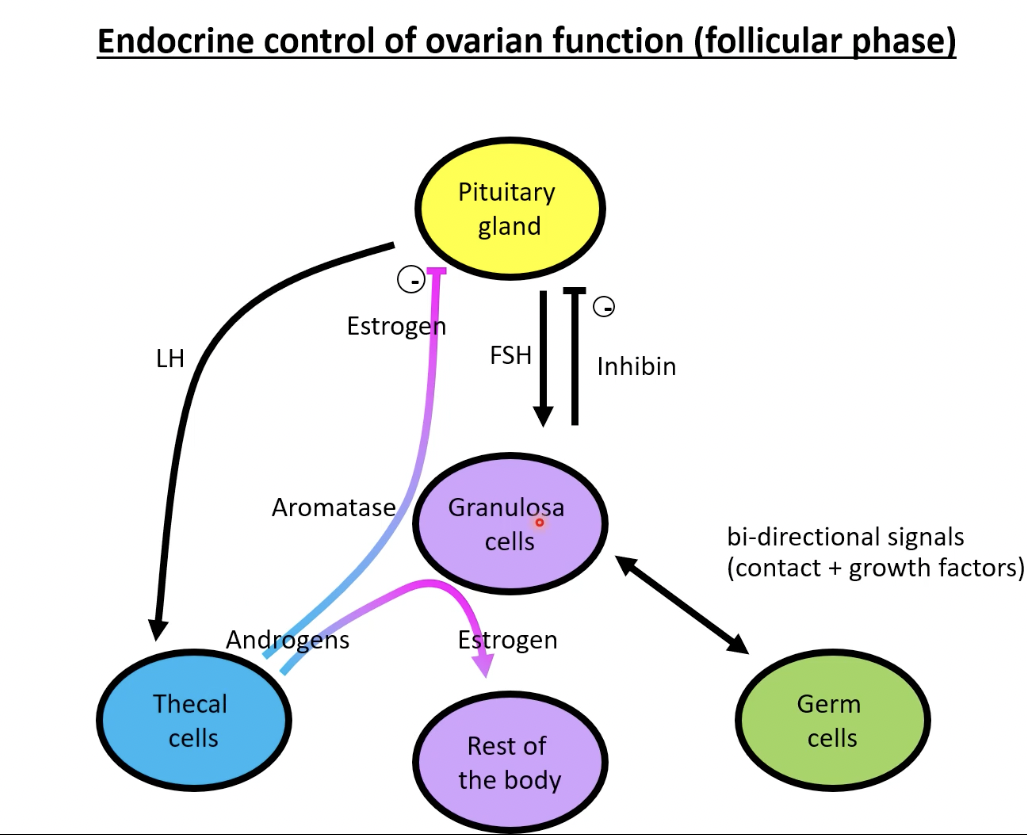
Endocrine Control of Ovarian Function: Follicular Phase
Pituitary Gland: Releases FSH (Follicle-Stimulating Hormone) and LH (Luteinizing Hormone). Think of these as the main signals from the brain to the ovary.
FSH: The main driver of the follicular phase. It tells the granulosa cells (cells surrounding the developing egg) to grow and multiply.
Thecal Cells: Stimulated by LH, these cells produce androgens.
Granulosa Cells: These cells have aromatase, an enzyme that helps turn androgens (hormones like testosterone, produced by the thecal cells) into oestrogen.
Oestrogen: As the follicle grows, granulosa cells make more oestrogen. Estrogen has several important jobs:
It helps the follicle grow even more.
It starts to thicken the lining of the uterus, preparing for a possible pregnancy.
It sends negative feedback to the pituitary gland, which starts to lower FSH levels a bit (but not completely yet!).
Inhibin: Produced by the granulosa cells, inhibin also sends negative feedback specifically to the pituitary gland to reduce FSH production. Think of it as a fine-tuning mechanism to control FSH.
Androgens: Produced by thecal cells, they are the building blocks for estrogen in the granulosa cells.
Bi-directional Signals: The ovary and the brain (pituitary) are constantly talking to each other through these hormones (positive and negative feedback).
Germ Cell: This is the developing egg inside the follicle. While the hormones primarily act on the follicle cells, their ultimate goal is to support the egg's maturation.
Endocrine Control of Ovarian Function: Luteal Phase
Corpus Luteum: Forms after ovulation, mainly makes progesterone.
Progesterone: Thickens uterus for possible pregnancy.
LH: Keeps the corpus luteum working.
Estrogen: Also made by corpus luteum, helps progesterone.
Negative Feedback: Progesterone and estrogen tell the pituitary gland to lower FSH and LH.
Inhibin: From corpus luteum, specifically lowers FSH.
No Pregnancy: Corpus luteum breaks down, progesterone and estrogen drop, leading to menstruation.
what are the two cycles
ovarian cycle
uterine cycle
concurrent with ovarian cycle
what is the ovarian cycle
made up of
follicular phase (10-21)
ovulation phase
luteal phase (follicular remnants transform to corpus luteum)
what is the uterine cycle
menses
proliferative phase (thickening of endometrium)
secretory phase
after ovulation
thickened endometrium converts to a secretory structure
corresponds to the luteal phase
if no pregnancy then layers of endometrium are lost
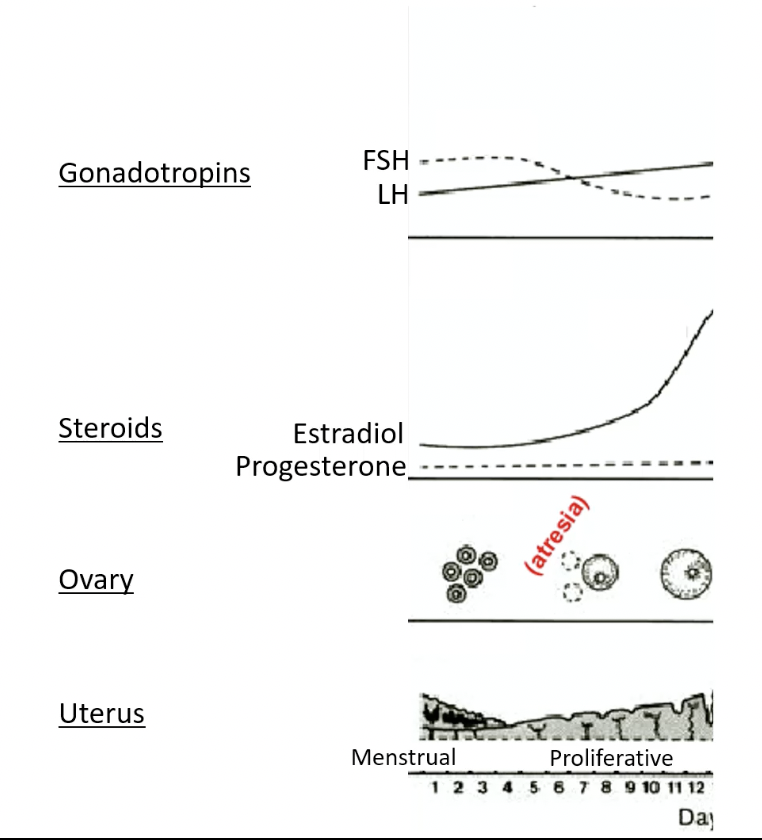
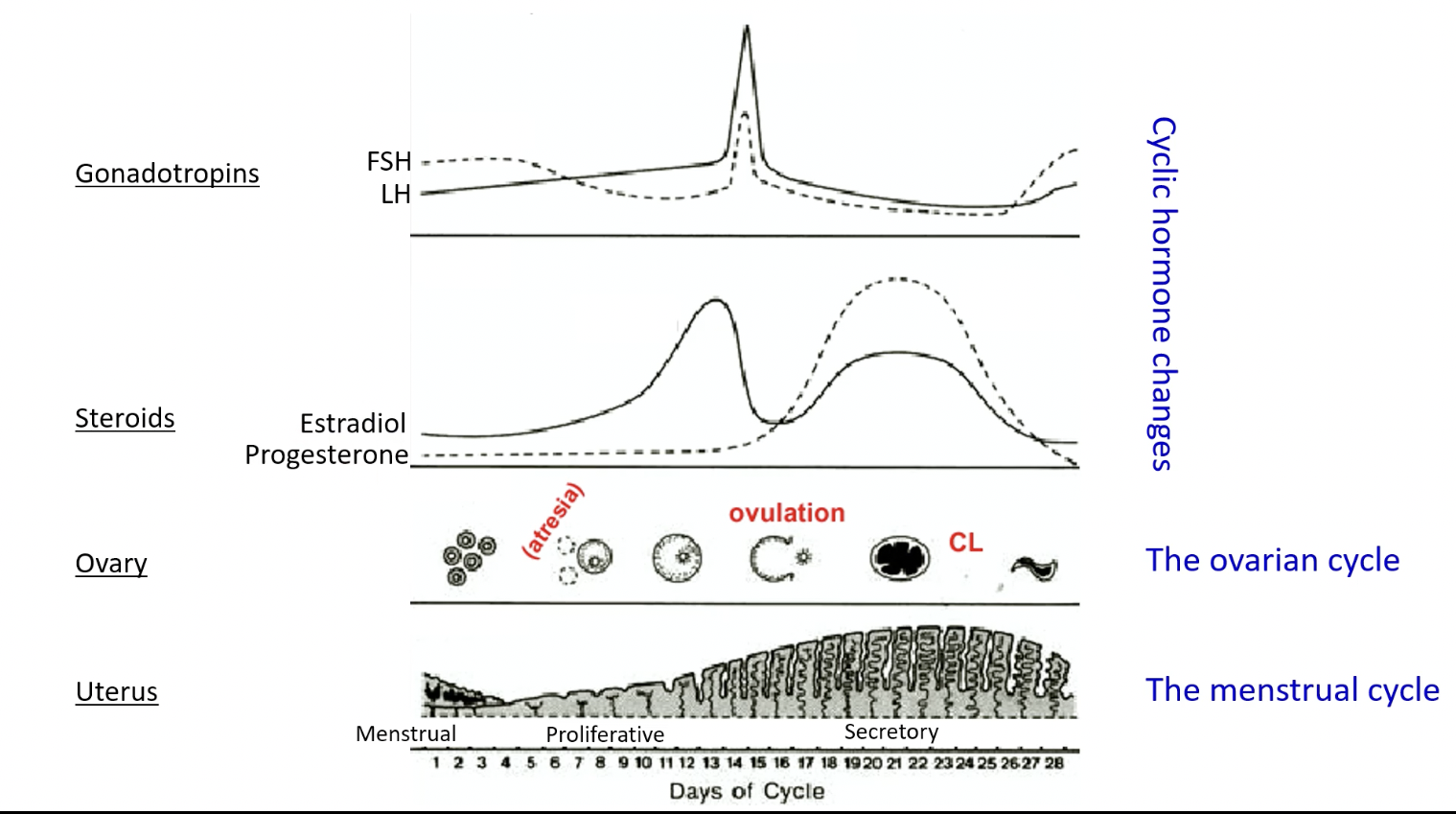
cycle graph of the cyclic hormones, ovarian cycle, and menstrual cycle
FSH and LH highest around day 14
estradiol highest few days before ovulation then big drop
progesterone highest around day 21, stays high for around a week
estradiol high within this window, but shorter time
uterus lining thickest at concurrent time with high progesterone and estradiol levels
corpus luteum prevalent here
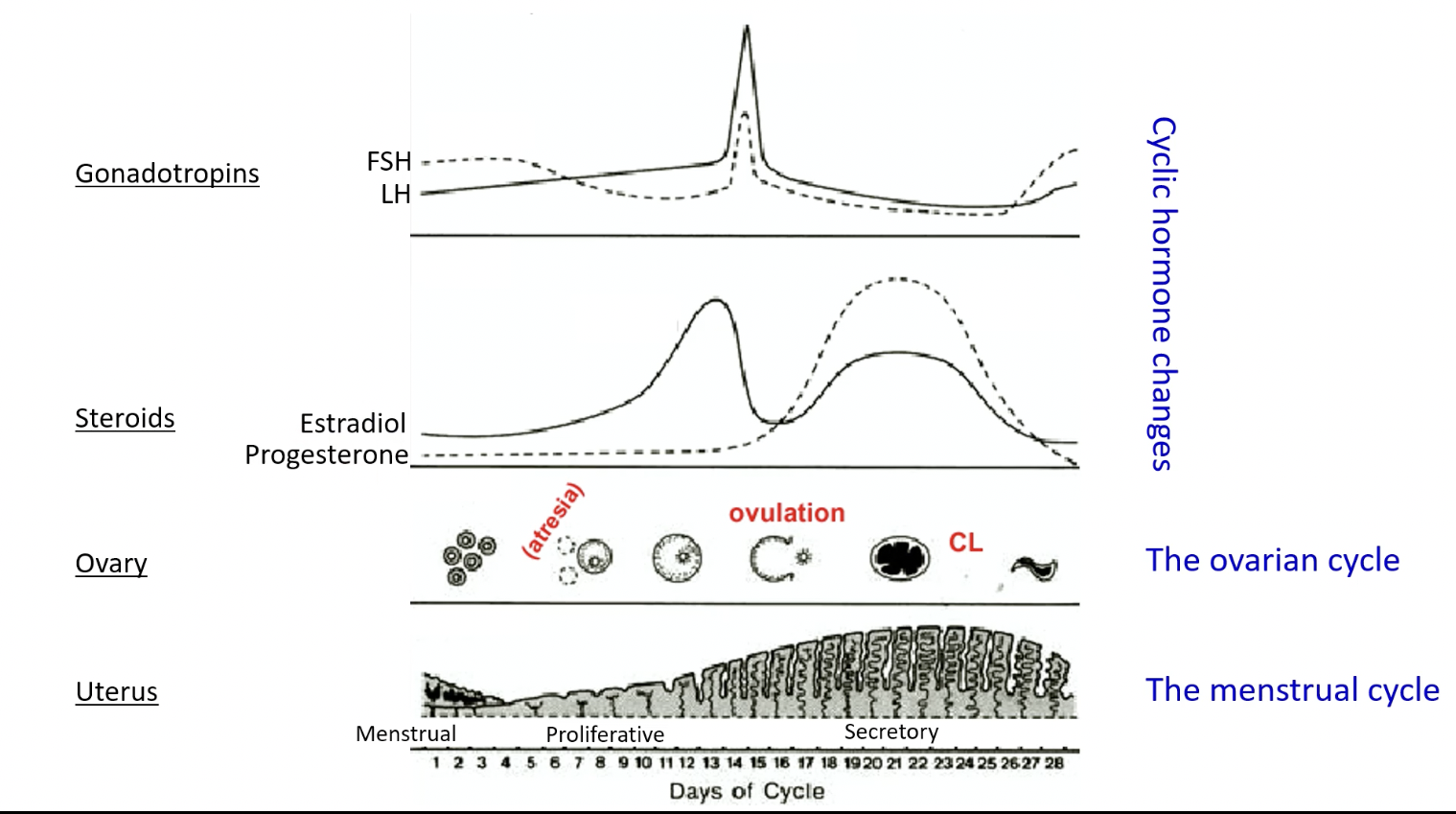
describe the follicular phase
days 1-14
cohort of 6-12 primary follicles begins to develop
FSH stimulates development of antral follicles
LH stimulates production of androgens in thecal cells converted to oestrogen by aromatase in follicular cells
about day 6 one follicle becomes dominant while others undergo atresia
late in follicular phase, oestrogen and inhibin collectively begin to repress FSH production - LH does not decline yet though
oestrogen stimulus prompts the endometrial lining to start proliferation
high levels of oestrogen at end of phase prepares uterus for potential pregnancy
cervical mucus becomes thin and stringy to facilitate sperm entry
describe the ovulation phase
day 14
oestrogen feedback at the pituitary switches direction to positive
sudden massive surge of LH (and FSH to lesser degree)
LH surge triggers ovulation about 16-24 hours later
meiosis resumes and first polar body is produced
mature follicle secretes collagenase
egg and antral fluid are released
egg surrounded by granulosa cells, now called cumulus oophorus
cumulus-egg complex (COC) swept into fallopian tube
thecal cells remain in the ovary and switch to producing progesterone
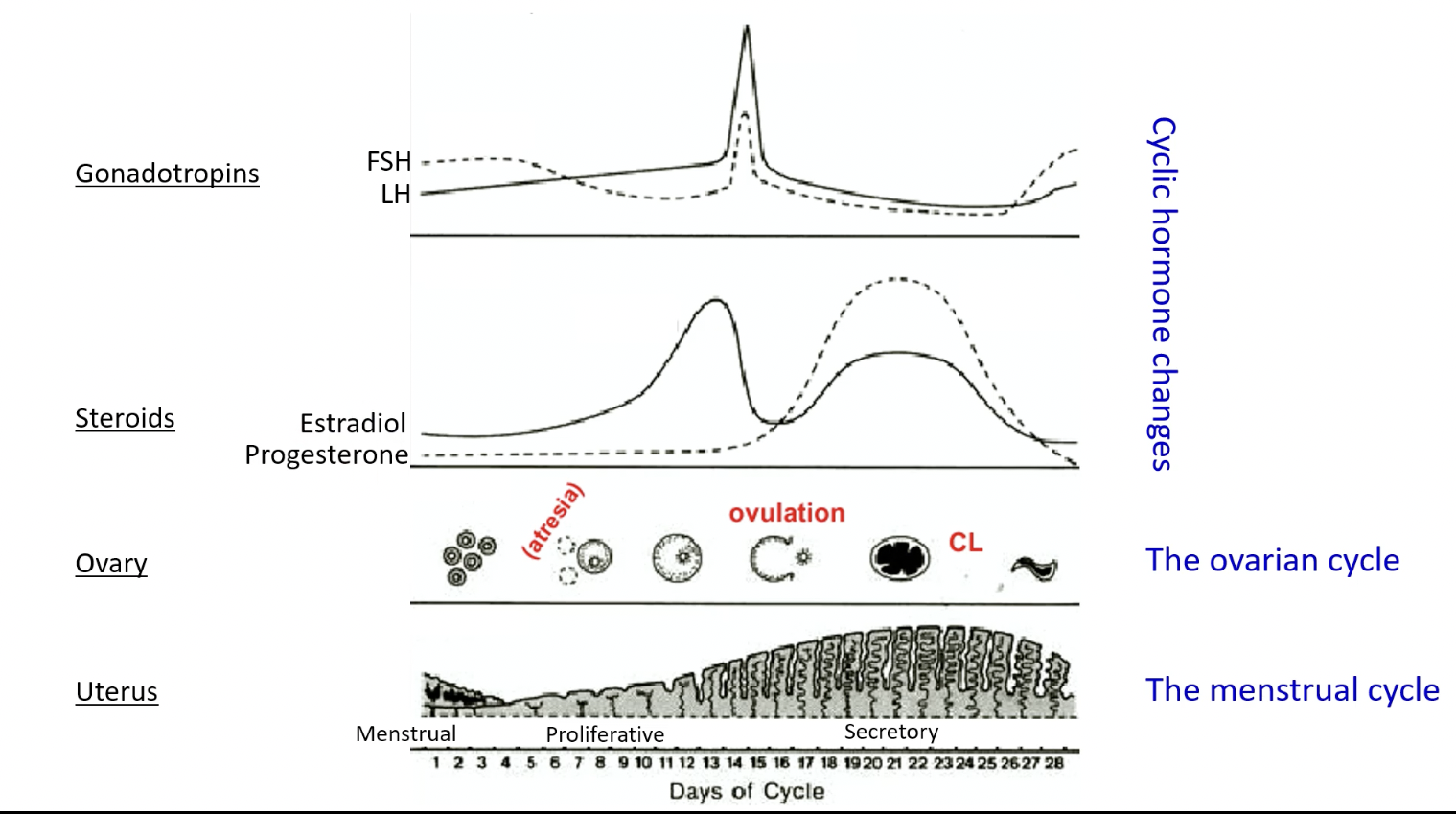
describe the luteal phase
day 15-18
corpus luteum forms from thecal cells and follicular cells that are not released as cumulus cells
produces oestrogen and progesterone to support the uterine lining until implantation
high levels of progesterone and oestrogen repress FSH and LH at pituitary
if there is no implanted embryo, the corpus luteum degenerates
declining levels of progesterone and oestrogen allow FSH and LH to rise again
initiates next ovarian cycle
what happens at perimenopause
too few follicles left
FSH and LH rising
no follicles left to respond/if they do response bc there is so few left it takes month for levels to build up until you can trigger an ovarian cycle
miss periods - highly irregular
Ovaries: Less consistent egg and hormone (estrogen, progesterone) production.
Hormones: Levels fluctuate unpredictably.
Periods: Become irregular (length, flow, timing).
FSH: Levels often start to go up.
Years Before: This phase happens before menopause (no periods for 1 year).
what is the post-menopausal state like for women
elevated LH and FSH around 60s
low oestrogen and progesterone
no cycles
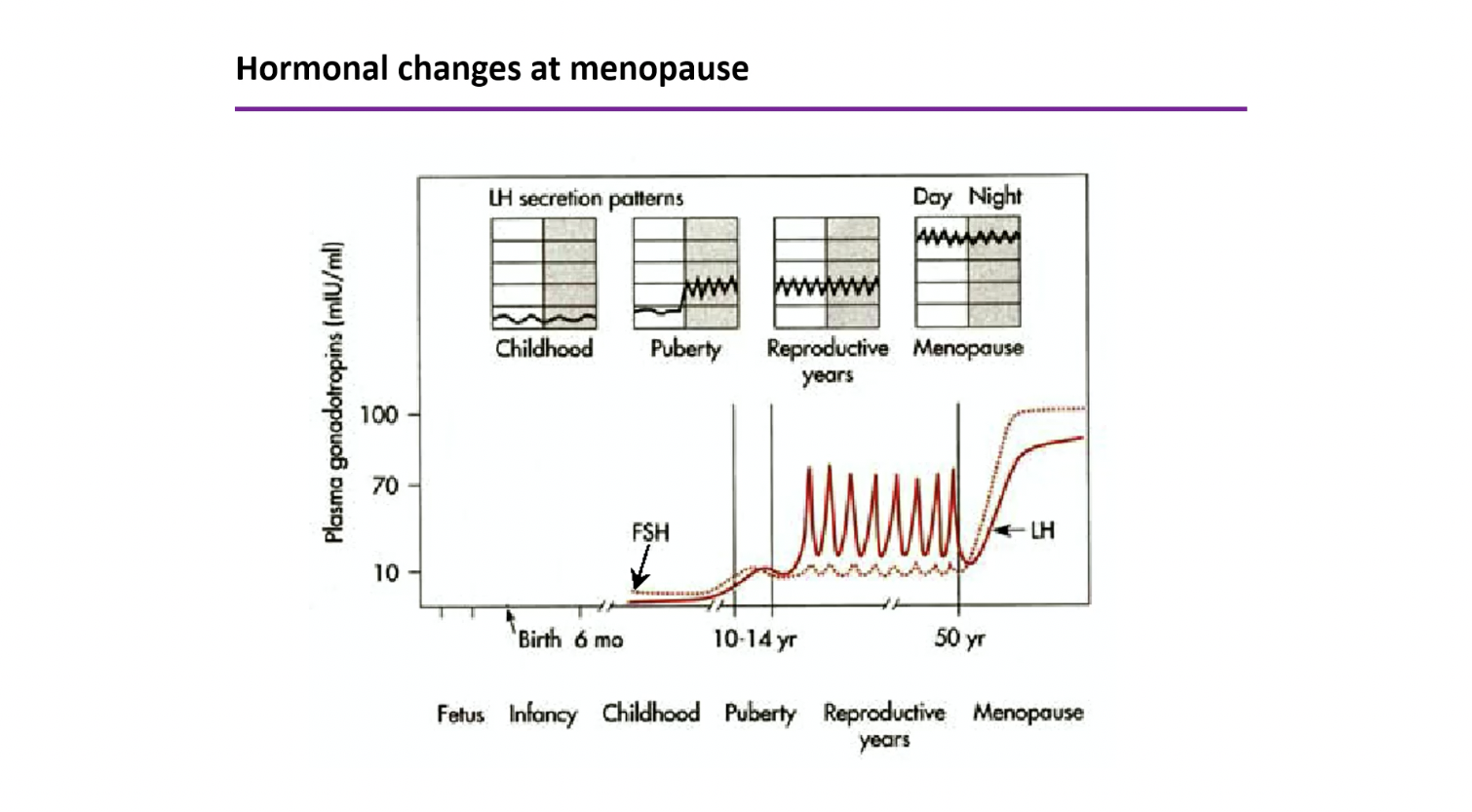
what happens in menopause
cessation of reproductive cycles
depletion of follicles
estradiol levels decrease
LH and FSH increase (no negative feedback of estradiol)
most symptoms result of estradiol deficiency
menopause symptoms
hot flushes
emotional changes/mood swings
osteoporosis
what is used to treat menopause
HRTs - oestrogen and progesterone
oestrogen therapy - oestrogen alone