pelvis anatomy
1/233
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
234 Terms
most inferior aspect of the abdominopelvic cavity.
pelvis
what surrounds the pelvis?
it is surrounded by the pelvic girdle.
how is the pelvis subdivided?
the pelvis is subdivided into the greater pelvis (above pelvic brim) and the lesser pelvis (below pelvic brim).
what covers the pelvis externally?
externally, the pelvis is covered by the inferior anterolateral central body wall, gluteal region, and perineum.
what is the pelvic girdle?
the pelvic girdle is a basin shaped ring of bones that connects the vertebral column with the leg bones.
what function does the pelvic girdle serve?
it bears weight when sitting and standing.
how does the pelvic girdle affect posture?
the pelvic girdle transfers weight from the central skeleton to the limbs for upright posture.
what does the pelvic girdle provide?
it provides muscular attachments for the central body wall and lower limbs.
what does the pelvic girdle protect?
the pelvic girdle protects the internal organs of the pelvis.
what support does the pelvic girdle provide?
it provides support for the central body's internal organs, pelvic internal organs, and a gravid (pregnant) uterus.
what attachments does the pelvic girdle provide?
it also provides attachments for erectile bodies of the external genitalia.
how is the pelvis divided?
the pelvis is divided into greater and lesser pelvis by the oblique plane of the pelvic inlet/superior pelvic aperture.
what is the pelvic brim?
the pelvic brim is the bony rim surrounding the pelvic inlet.
what forms the pelvic brim?
the pelvic brim is formed by the sacral promontory, ala of the sacrum, and the right and left linea terminalis (arcuate line and pecten pubis).
what is the pubic arch?
the pubic arch is formed by the ischiopubic rami.
where do the ischiopubic rami meet?
the ischiopubic rami meet at the pubic symphysis, with borders defined by the subpubic angle.
what structures bound the pelvic outlet?
the pelvic outlet is bounded by the pubic arch anteriorly, ischial tuberosities laterally, the inferior margin of the sacrotuberous ligament posterolaterally, and the tip of the coccyx posteriorly.
where is the greater pelvis located?
the greater pelvis is superior to the pelvic inlet, bounded by the iliac alae posterolaterally and the anterosuperior aspect of s1.
what occupies the greater pelvis?
the greater pelvis is occupied by some internal organs: ileum and sigmoid colon.
what is the lesser pelvis?
the lesser pelvis is the true pelvic cavity, between the pelvic inlet and outlet.
what bounds the lesser pelvis?
it is bounded by the pelvic structures of the hip bones, sacrum, and coccyx.
what forms the walls and floor of the pelvic cavity?
the walls and floor of the pelvic cavity are formed by muscles and bones.
what is the pelvic floor?
the pelvic floor is formed by the funnel-shaped pelvic diaphragm.
what does the pelvic diaphragm include?
the pelvic diaphragm includes the coccygeus muscles and the levator ani muscles.
what is unique about levator ani muscles?
levator ani muscles are difficult to differentiate, but relax for urination and defecation.
how does the pelvic floor stretch?
the pelvic floor stretches like a hammock suspended from the attachments of the pelvic walls and contains the urogenital hiatus.
does the peritoneum reach the pelvic floor?
the peritoneum does not reach the pelvic floor.
where are the pelvic internal organs located?
except for the ovaries and uterine tubes, the pelvic internal organs are subperitoneal.
how does the peritoneum cover the uterus in females?
in females, the peritoneum covers the superior uterus and descends its posterior surface before reflecting on the anterior rectum, forming the recto-uterine pouch.
what are broad ligaments?
the broad ligaments, which are folds of the peritoneum, enclose the ovaries and uterine tubes.
what is the purpose of prenatal training?
prenatal training (lamaze classes) attempts to train women to voluntarily relax pelvic floor muscles while increasing central body pressure.
how does prenatal training help during childbirth?
this supplements the uterus in passing a child, minimizing resistance.
what injuries can occur to the pelvic floor during childbirth?
injury to the pelvic floor during childbirth can involve the perineum, levator ani ligaments, and fascia.
which muscles are most commonly torn during childbirth?
the pubococcygeus and puborectalis are the most commonly torn muscles.
what can changes in pelvic floor muscles cause?
changes in these muscles, which surround the urethra, vagina, and anus, can cause urinary incontinence, fecal incontinence, or prolapse of pelvic organs.
what is an episiotomy?
episiotomy, a surgical incision to enlarge the vaginal opening, is used to decrease global tearing, for arrested descent, or during fetal distress.
are episiotomies commonly used?
episiotomies are not as commonly used as in the past.
what are common pelvic fractures?
pelvic fractures can include fracture of the pubic rami, which is very common due to narrow rami around the obturator foramen.
how can fractures occur in the pelvis?
fracture can occur with crushing injury or lateral compression of the pelvis.
what is the nature of pelvic ring fractures?
fracture of the pelvic ring almost always involves multiple fractures; surgical intervention usually depends on stability.
what can happen if bones are broken in the pelvis?
if bones are broken, surrounding tissues can be damaged, such as ruptured urinary bladder or urethra, or shearing forces to iliac arteries/veins and pelvic nerves.
what are the primary arterial supplies to the female pelvis?
the female pelvis is supplied by paired internal iliac, paired ovarian, median sacral, and superior rectal arteries.
what are the primary arterial supplies to the male pelvis?
the male pelvis is supplied by paired internal iliac, median sacral, superior rectal, and testicular arteries.
how do testicular arteries reach the testes?
testicular arteries descend to the testes via the central body cavity and inguinal canal.
how are pelvic veins drained?
pelvic veins are primarily drained by the internal iliac veins.
how does some drainage occur in the pelvis?
some drainage occurs via the superior rectal vein to the inferior mesenteric vein, then to the hepatic portal vein.
what are the types of lymph nodes in the pelvis?
external iliac nodes drain pelvic internal organs; internal iliac nodes receive lymph from inferior internal organs; sacral lymph nodes drain to internal or common iliac nodes.
where do external iliac nodes drain?
external iliac nodes lay above the pelvic brim and drain to common iliac nodes.
where do internal iliac nodes cluster?
internal iliac nodes cluster around internal iliac and gluteal arteries, draining into common iliac nodes.
where do sacral lymph nodes lie?
sacral lymph nodes lie in the concavity of the sacrum and drain to internal or common iliac nodes.
where do common iliac nodes lie?
common iliac nodes lie superior to the pelvic brim along common iliac blood vessels, draining lymph to lumbar nodes.
what does the sacral plexus give rise to?
the sacral plexus gives rise to two major nerves: sciatic and pudendal.
what is the coccygeal plexus?
the coccygeal plexus is a smaller network formed from s4-s5 and the coccygeal nerves.
what do anococcygeal nerves supply?
anococcygeal nerves supply a small area of skin anterior to the coccyx and posterior to the anus.
what are the four routes for autonomic nerves to enter the pelvic cavity?
sacral sympathetic trunks, peri-arterial plexuses, hypogastric plexuses (superior and inferior), and pelvic splanchnic nerves.
what do sacral sympathetic trunks provide?
sacral sympathetic trunks provide vasomotor, pilomotor, and sudomotor innervation for the lower limb.
what is the function of peri-arterial plexuses?
peri-arterial plexuses have vasomotor function for the arteries they run along (ovarian, superior rectal, internal iliac).
what do hypogastric plexuses contain?
hypogastric plexuses contain sympathetic and visceral afferent nerves.
what do pelvic splanchnic nerves carry?
pelvic splanchnic nerves arise from the sacral plexus and carry presynaptic parasympathetic fibers.
how do visceral afferent fibers travel?
visceral afferent (e.g., reflex sensations, pain) fibers travel with autonomic nerve fibers.
how do visceral afferent nerves conducting reflex sensations travel?
visceral afferent nerves conducting reflex sensations travel with parasympathetic nerve fibers to the inferior hypogastric plexuses and pelvic splanchnic nerves, reaching s2-s4 spinal sensory ganglia.
what is the pelvic pain line?
the pelvic pain line describes how visceral afferent nerves conducting pain differ based on organ location in relation to the peritoneum.
how are organs classified in relation to the pelvic pain line?
organs in contact with the peritoneum (intraperitoneal, retroperitoneal) are classified as superior to the pelvic pain line.
how does pain from organs superior to the pelvic pain line travel?
pain from organs superior to the pelvic pain line follows sympathetic nerve fibers, ascending through hypogastric/aortic plexuses to inferior central body/upper lower central body spinal ganglia.
what are the organs in contact with the peritoneum classified as?
superior to the pelvic pain line.
how does pain from organs superior to the pelvic pain line follow?
it follows sympathetic nerve fibers, ascending through hypogastric/aortic plexuses to inferior central body/upper lower central body spinal ganglia.
what are subperitoneal organs?
they are inferior to the pelvic pain line.
how does pain from subperitoneal organs follow?
it follows parasympathetic nerve fibers retrograde through the pelvis and inferior hypogastric plexuses and pelvic splanchnic nerves, reaching s2-s4 spinal sensory ganglia.
what do pelvic internal organs contain?
the distal digestive organs, distal urinary tract, and reproductive organs.
what are the urinary organs?
distal ureters, urinary bladder, and urethra.
describe the urinary bladder.
the urinary bladder is a hollow organ with strong muscular walls that temporarily stores urine; its shape depends on urine volume.
where is the urinary bladder located?
it is subperitoneal and a central body organ in infants and young children.
what are the bladder walls made up of?
the detrusor muscle.
what is the internal urethral sphincter?
it is an involuntary sphincter to control urine flow.
what is the arterial supply to the urinary bladder?
arterial supply is via branches of the internal iliac artery, with inferior vesical arteries in males and vaginal arteries in females for the inferior region.
how is the venous drainage of the urinary bladder primarily done?
by the internal iliac veins.
how is the urinary bladder innervated?
it involves sympathetic fibers via the hypogastric plexus, and parasympathetic fibers via the splanchnic nerves and inferior hypogastric plexus.
what is the male urethra?
a muscular tube (18-22 cm long) that conveys both urine and semen.
what does the male urethra convey?
it conveys urine from the internal urethral orifice of the urinary bladder to the external urethral orifice at the distal end of the penis and semen from the openings of the ejaculatory ducts (in the prostate) to the external urethral orifice.
how many regions does the male urethra have?
four regions: intramural (preprostatic), prostatic, intermediate (membranous), and spongy.
what is the intramural region of the male urethra?
the length of urethra prior to the prostate.
what happens in the prostatic region of the male urethra?
secretory prostatic ducts open into the prostatic sinuses, carrying prostatic contributions of semen.
where do ejaculatory ducts open?
adjacent to and sometimes into the prostatic utricle.
what is the intermediate region of the male urethra?
it begins at the apex of the prostate and passes through the perineal membrane, surrounded by the external urethral sphincter.
what is the spongy region of the male urethra?
it begins at the perineal membrane and ends at the external urethral orifice, typically with a 5 mm diameter lumen.
how long is the female urethra?
4 cm long, 6 mm in diameter.
where does the female urethra pass?
it passes inferiorly from the internal urethral orifice to the external urethral orifice, located anterior to the vaginal opening in the vestibule.
what is debated regarding the female urethra?
the presence of an organized internal urethral sphincter.
where are paraurethral glands located?
in the superior part of the female urethra.
what is the rectum?
the rectum connects the sigmoid colon with the anus, with the rectosigmoid junction lying about s3.
what is the shape of the rectum?
the rectum is not exactly straight, and its dilated terminal region is the ampulla.
what does cystoscopy involve?
viewing the urinary bladder by passing a camera through the urethra.
what structures can be palpated during rectal examinations?
the prostate, seminal glands, cervix, sacrum and coccyx, ischial spines, and ischial tuberosities.
what is urinary catheterization?
it drains urine from the urinary bladder without patient assisting in voiding.
what are the methods for urinary catheterization?
intraurethral vs. suprapubic access.
list the male internal pelvic internal organs.
ductus deferentes, seminal glands, ejaculatory ducts, prostate, and bulbo-urethral glands.
what are ductus deferentes?
paired tubes that connect the epididymis to the seminal glands at the ejaculatory ducts.
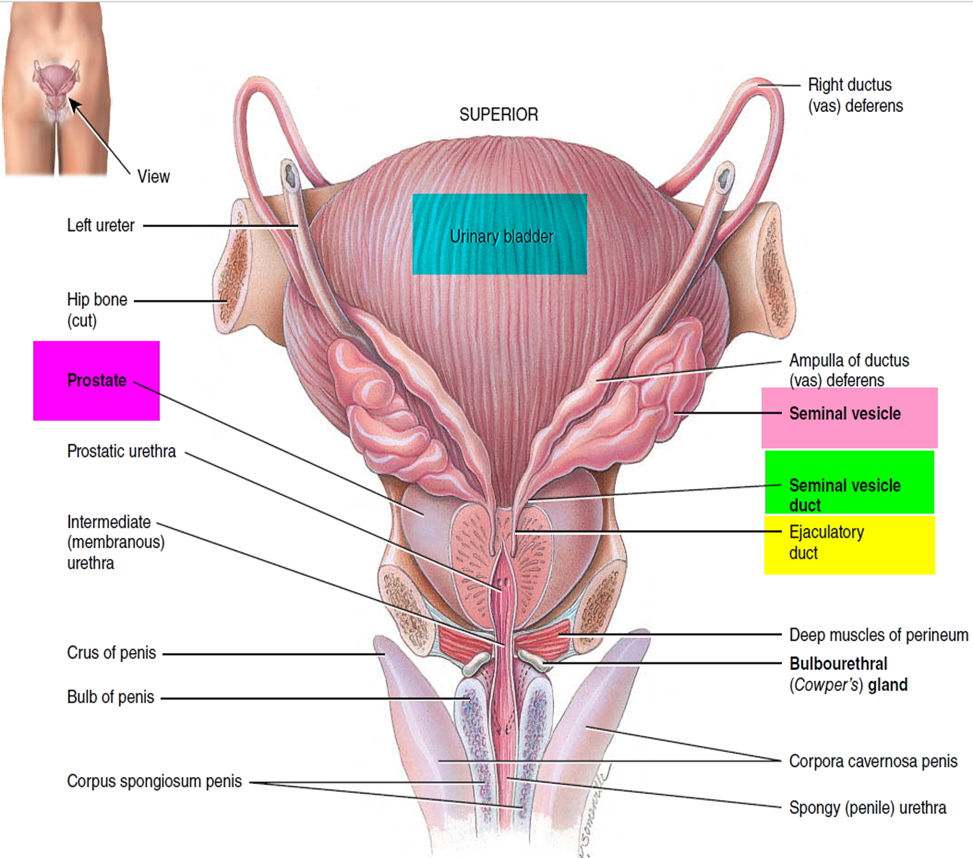
what do the fluid and sperm delivered by the ductus deferentes contribute to?
about 10% of semen volume.
what are seminal glands?
elongated structures (5 cm) that lie posterior to the prostate and are obliquely placed.
do seminal glands store sperm?
no, they produce a thick fluid (60% of semen total volume).