Test 8: Reproductive (cadaver)
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
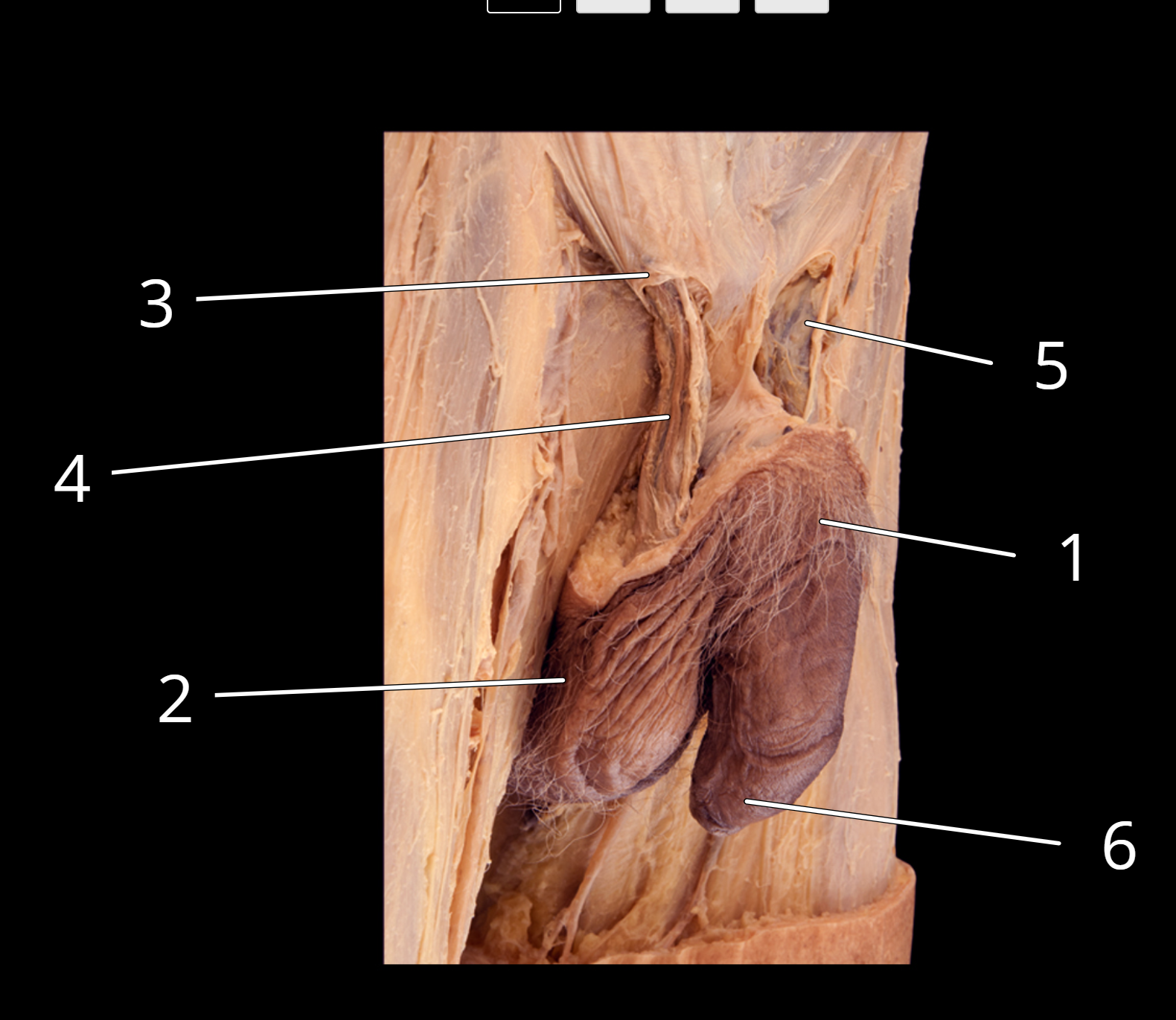
Penis and testis, lateral view
1. Penis
2. Scrotum
3. Superficial inguinal ring
4. Right spermatic cord
5. Left spermatic cord
6. Prepuce
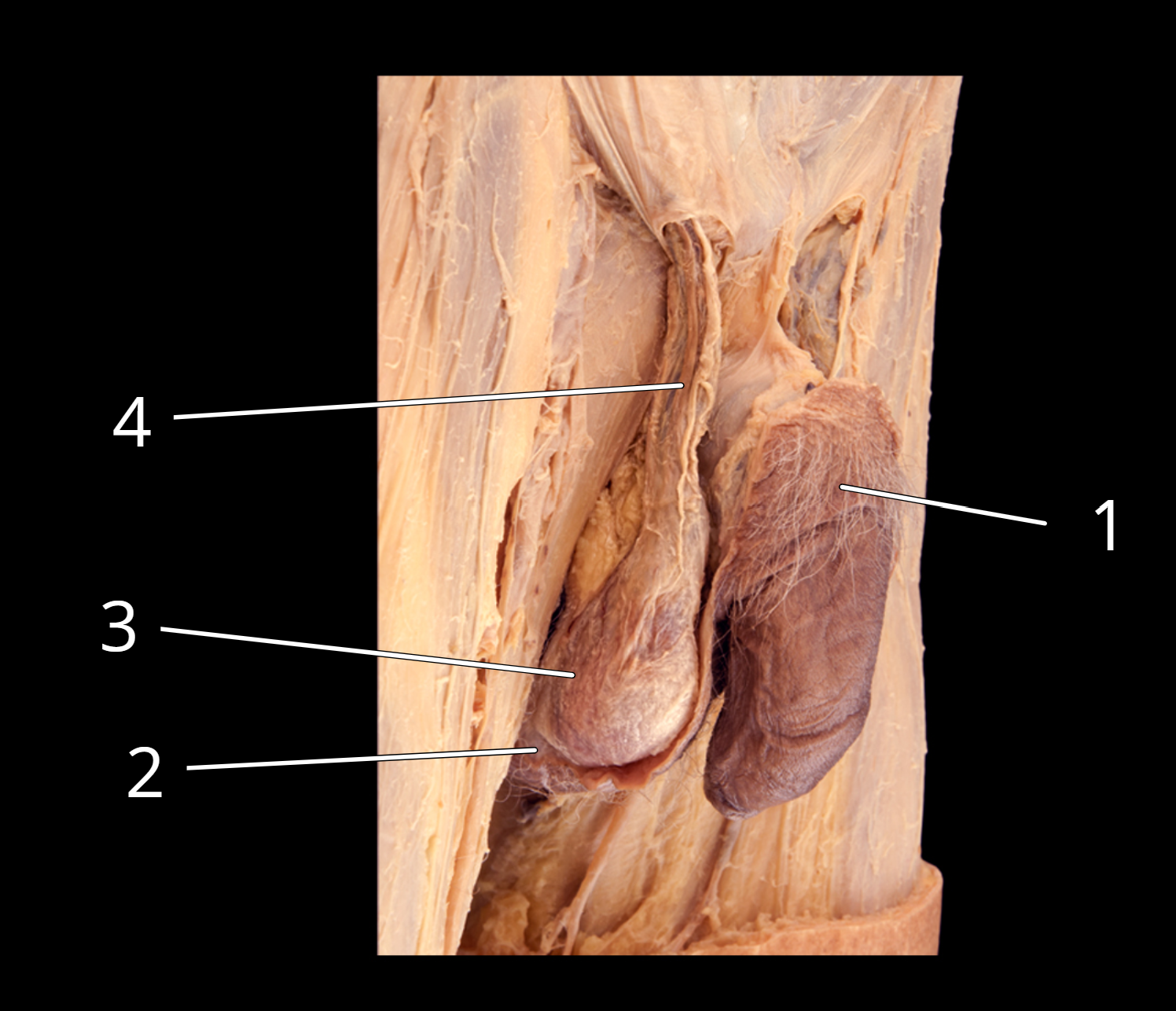
Penis and testis, lateral view
1. Penis
2. Scrotum, cut
3. Testis in external spermatic fascia
4. Spermatic cord
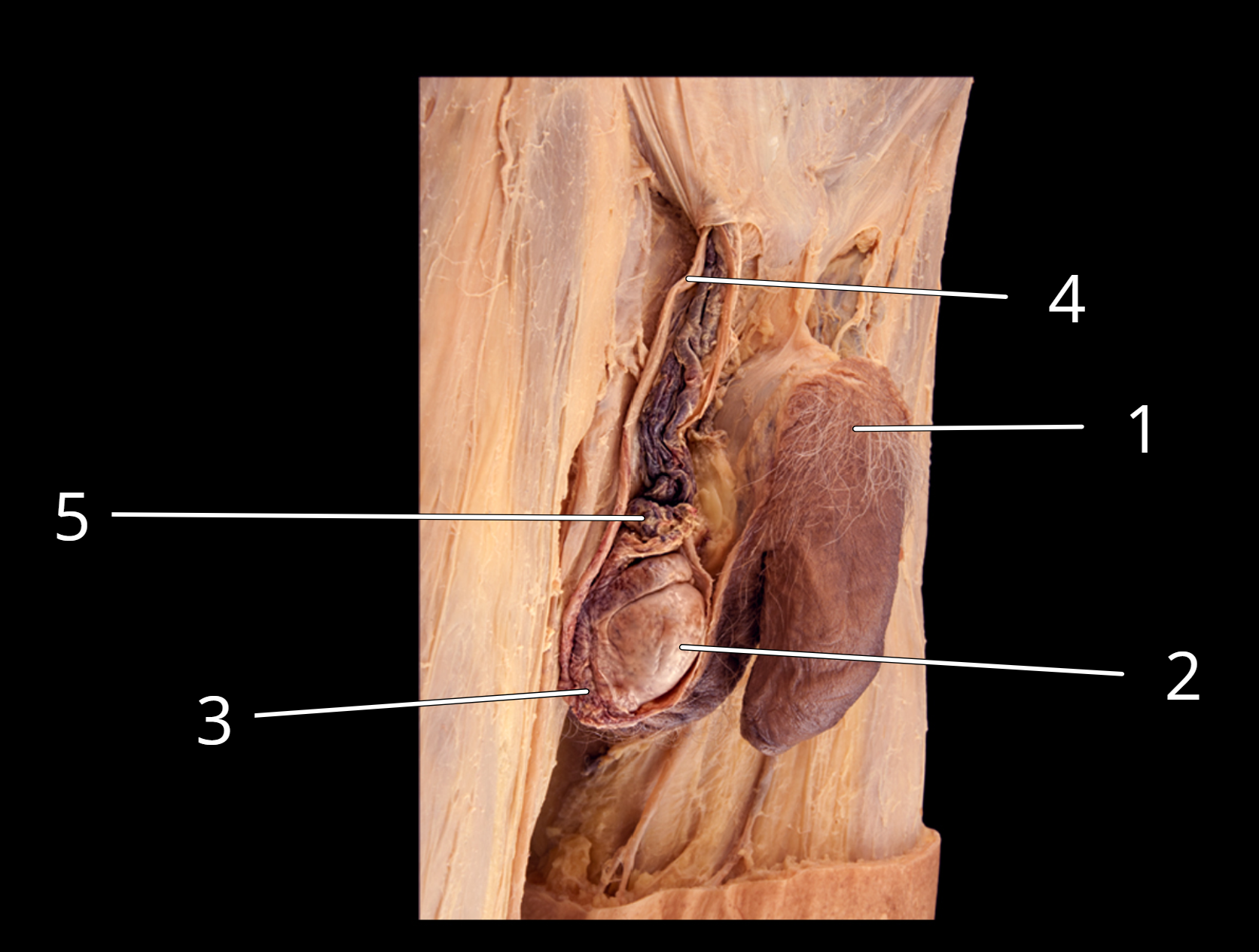
Penis and testis, lateral view
1. Penis
2. Testis
3. Epididymis
4. Ductus deferens
5. Testicular artery and pampiniform plexus of veins
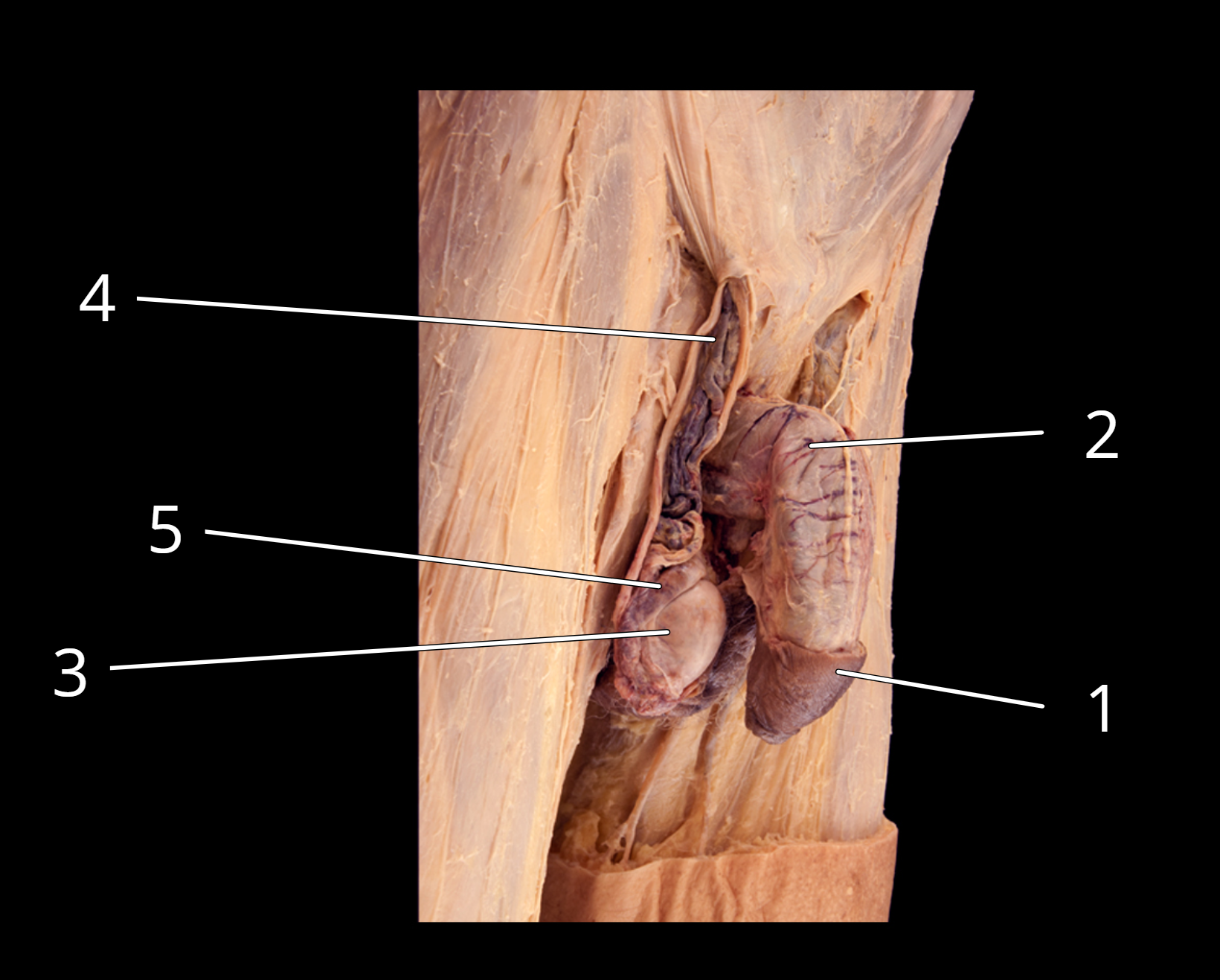
Penis and testis, lateral view
1. Prepuce
2. Penis
3. Tunica albuginea of testis
4. Testicular artery and pampiniform plexus of veins
5. Epididymis
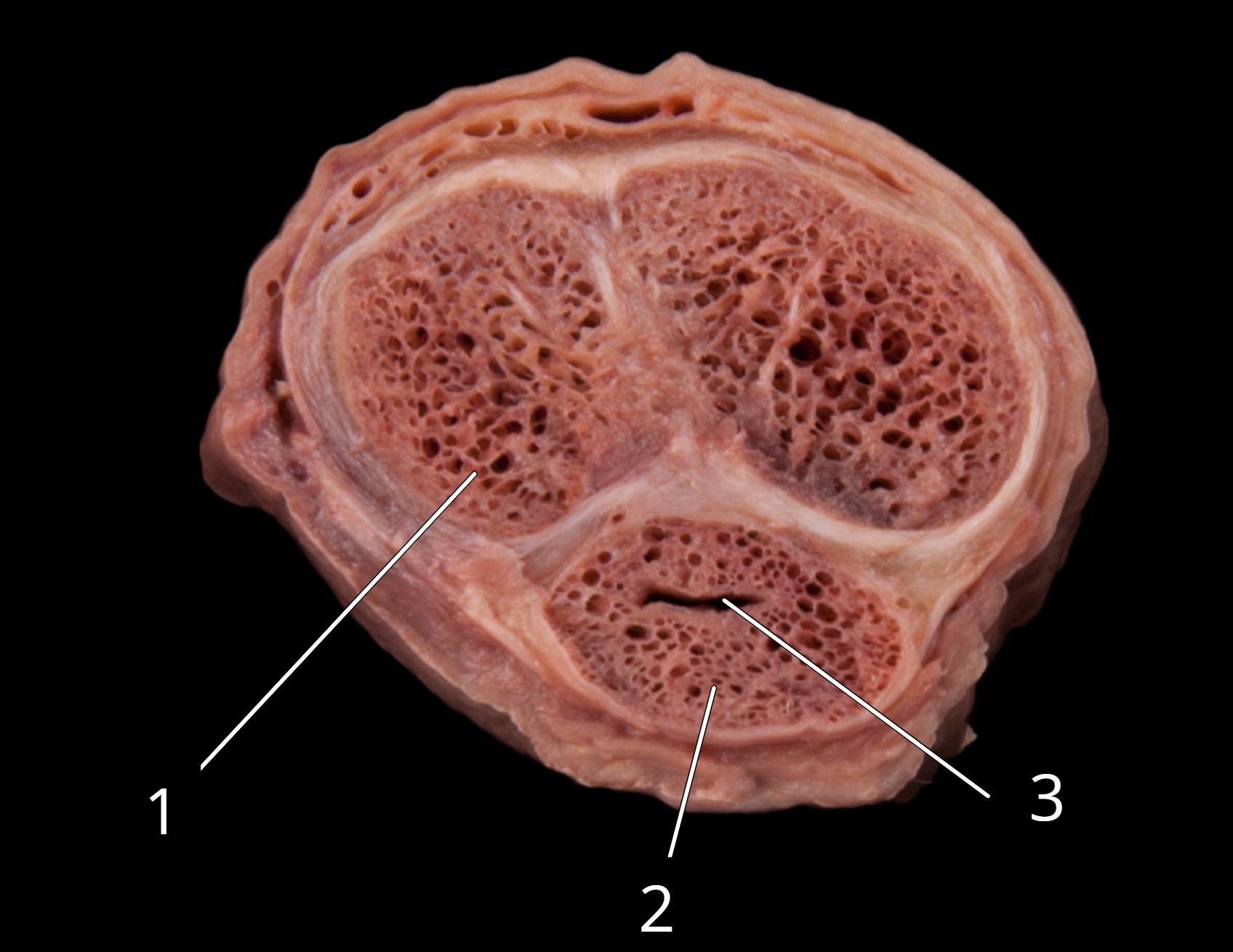
Penis, transverse section
1. Corpora cavernosa
2. Corpus spongiosum
3. Penile urethra
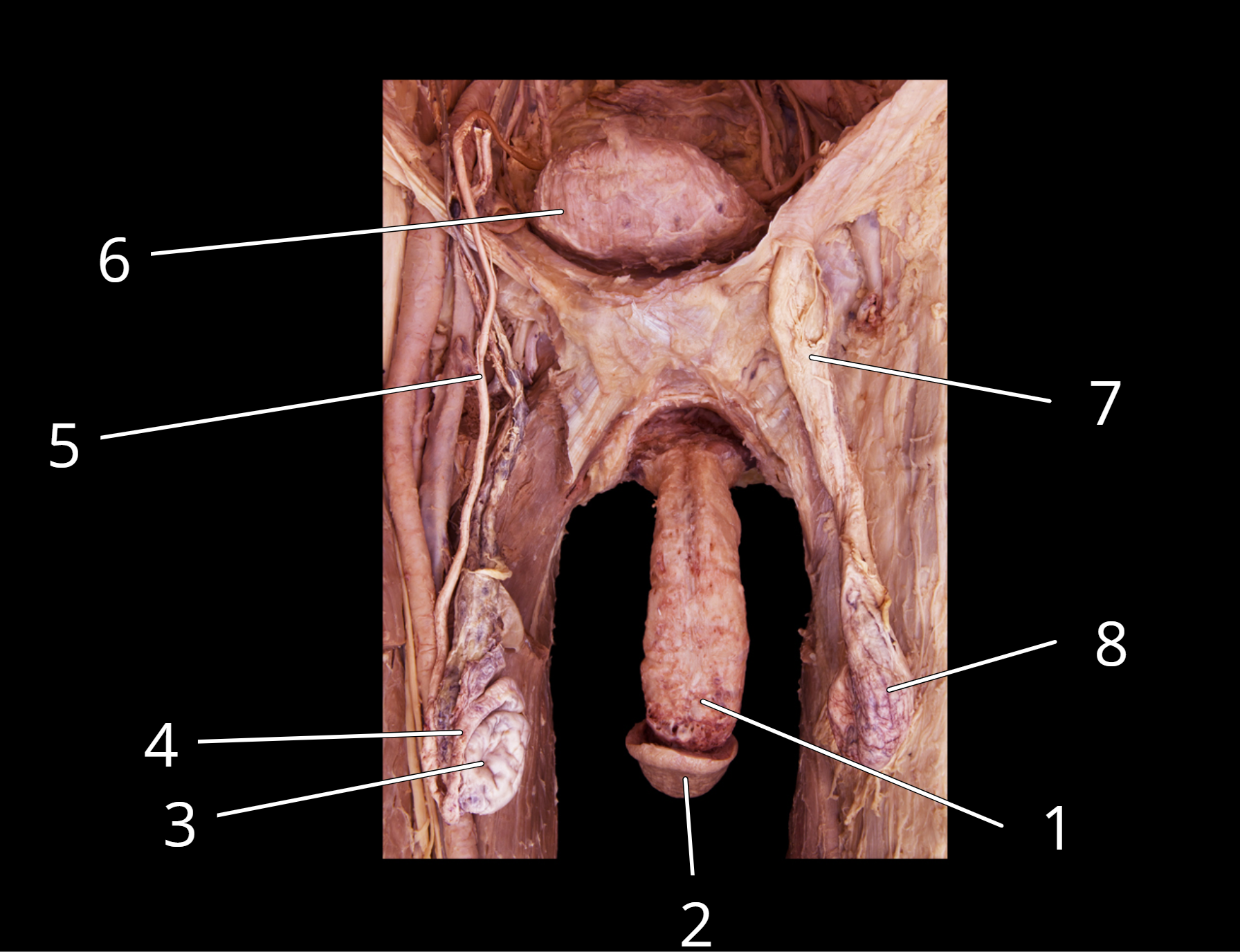
Male reproductive structures
1. Penis
2. Glans penis
3. Testis
4. Epididymis
5. Ductus deferens
6. Urinary bladder
7. Spermatic cord
8. Testis in external spermatic fascia
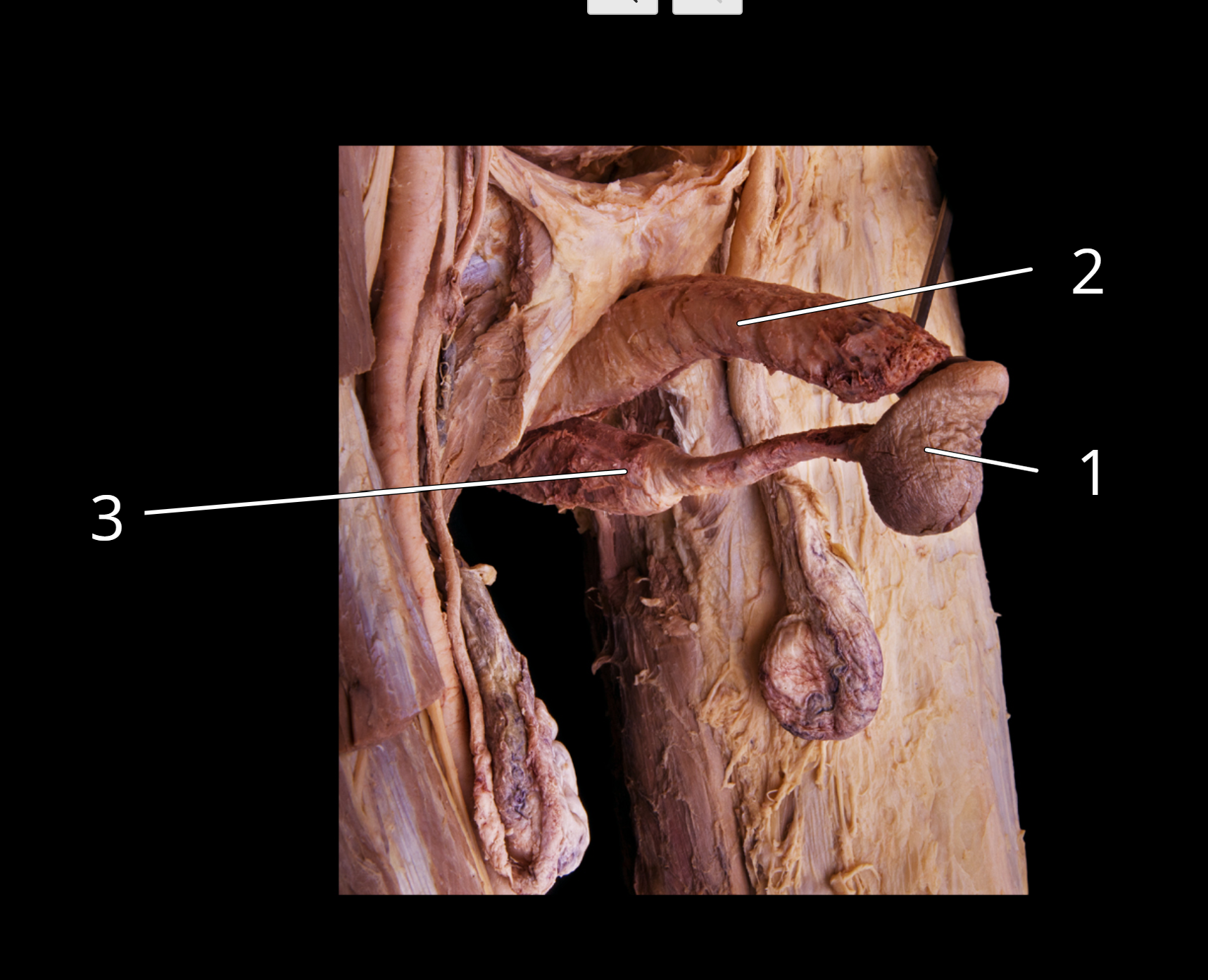
Structures of the penis
1. Glans penis
2. Corpora cavernosa
3. Corpus spongiosum
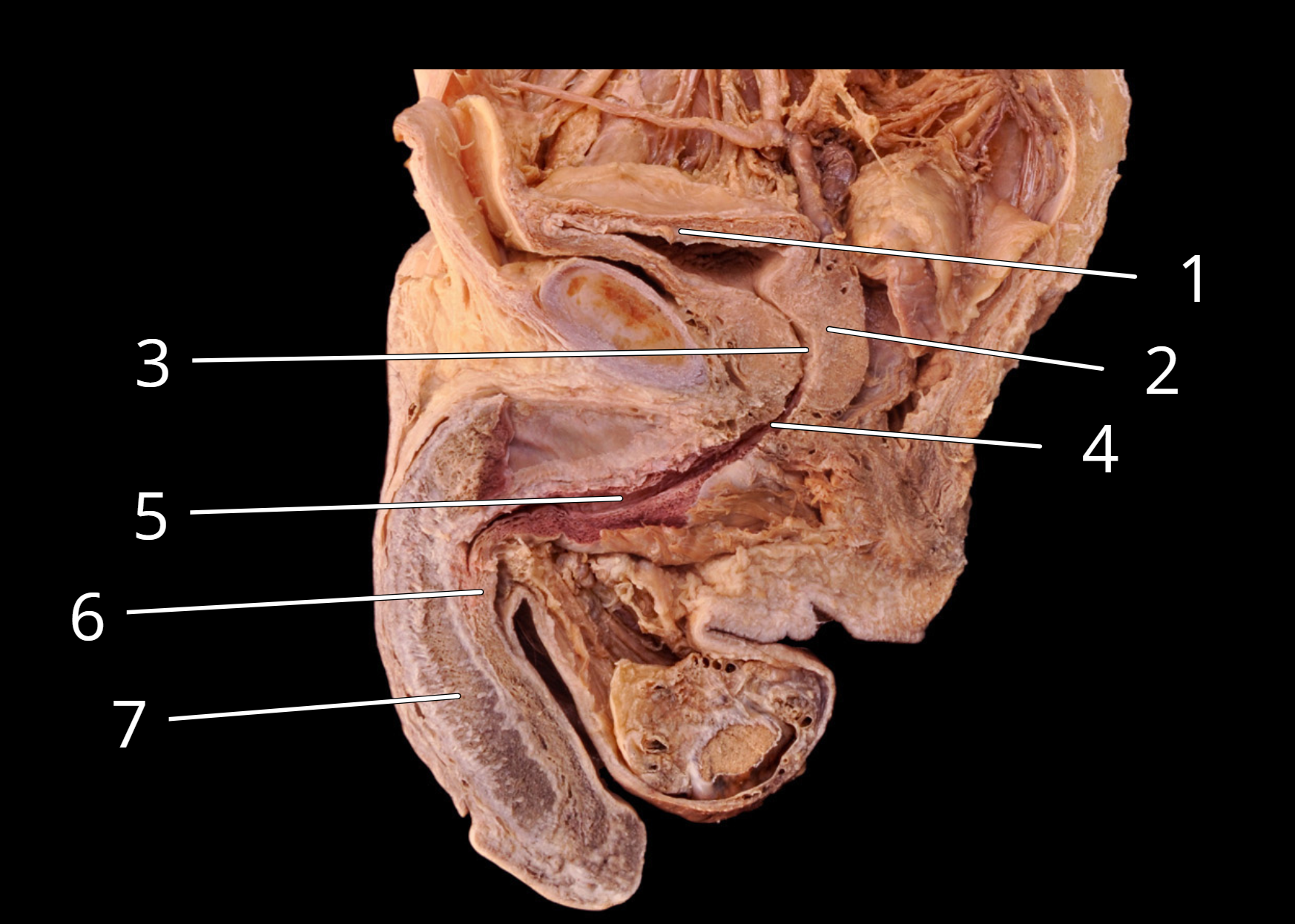
Male reproductive structures, sagittal view
1. Urinary bladder
2. Prostate
3. Prostatic urethra
4. Intermediate part of urethra (Membranous urethra)
5. Spongy urethra
6. Corpus spongiosum
7. Corpus cavernosum
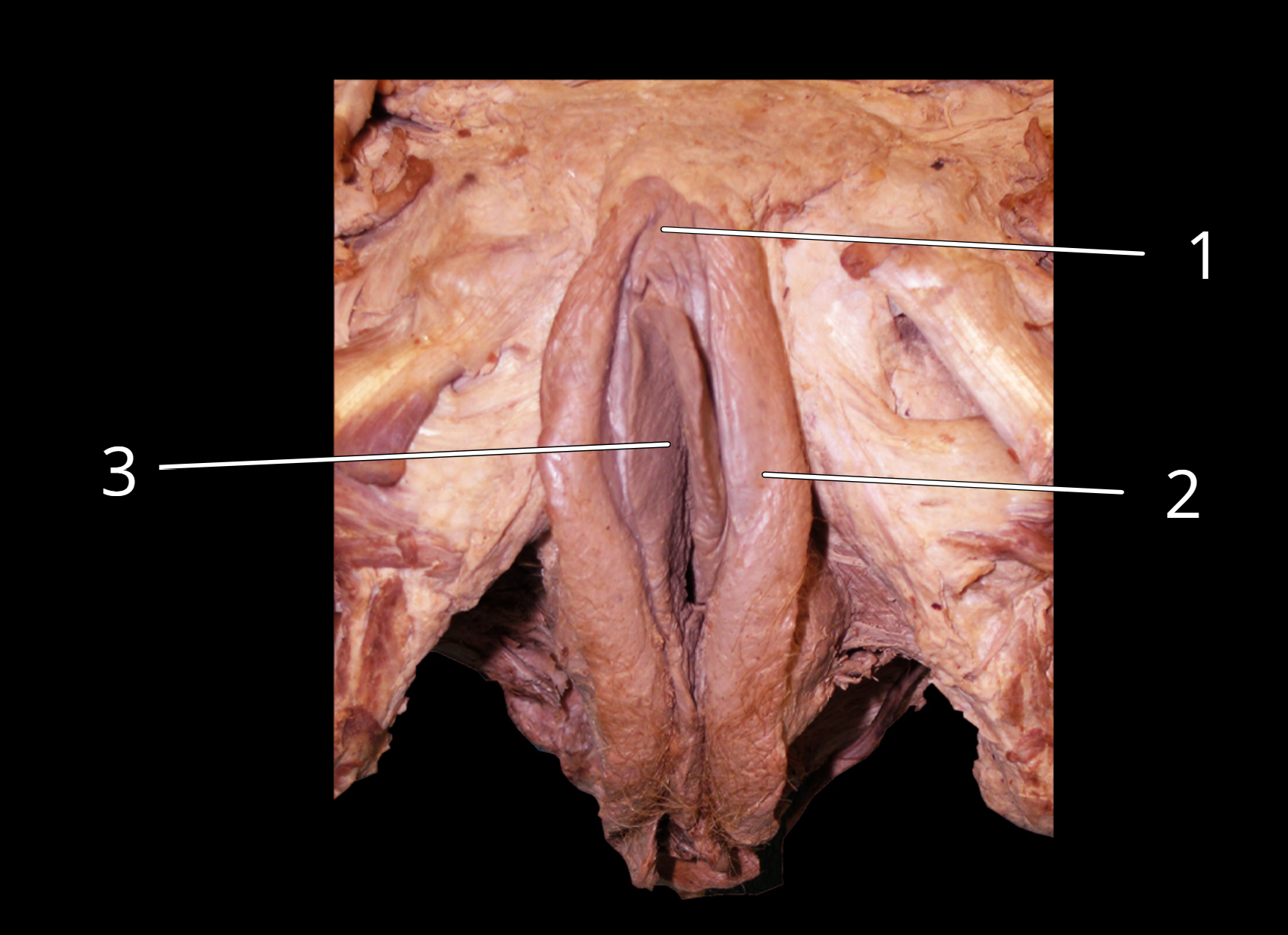
Female external genitalia
1. Clitoris
2. Labia majora
3. Labia minora
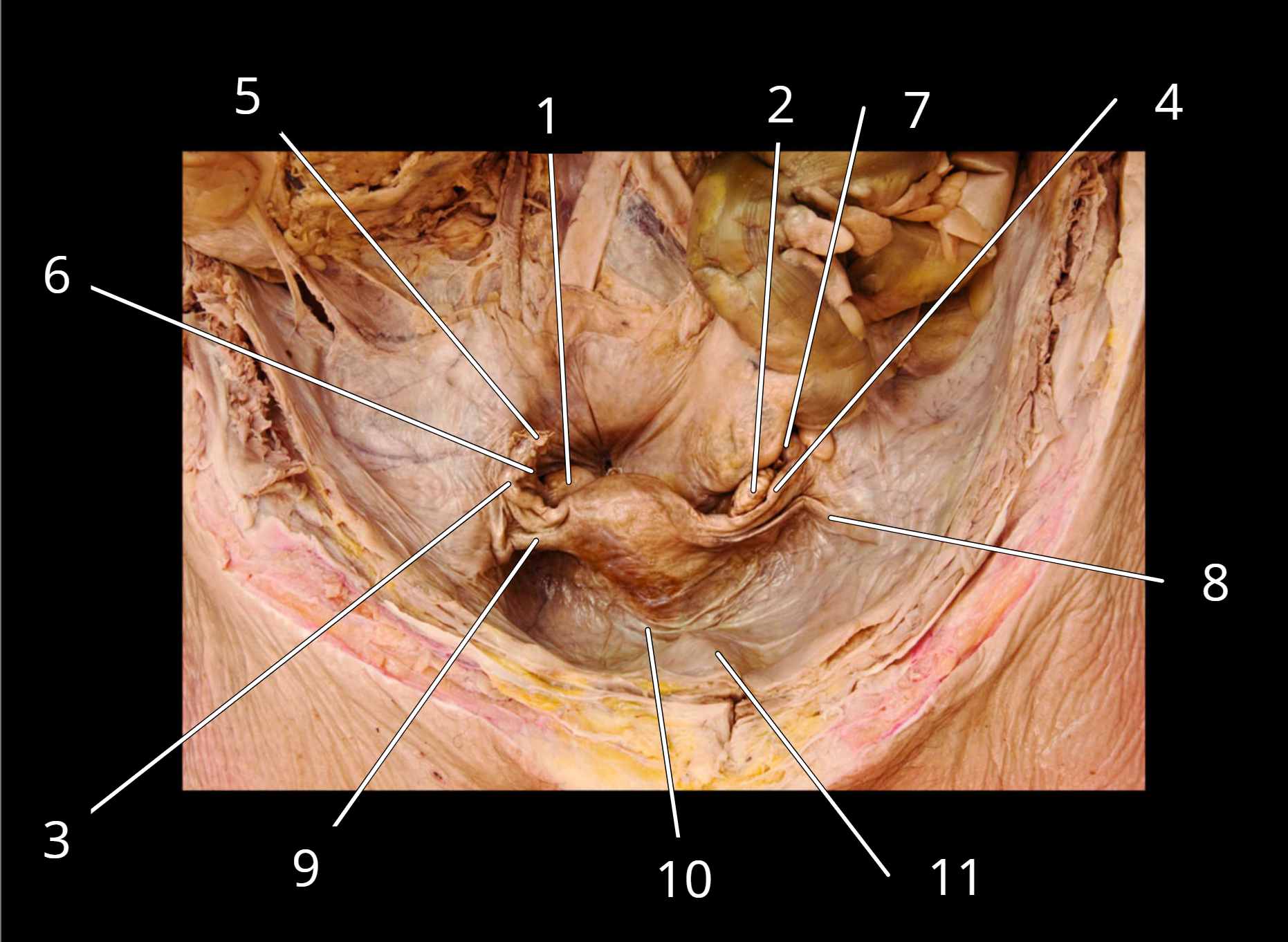
Uterus
1. Right ovary
2. Left ovary
3. Right uterine tube
4. Left uterine tube
5. Fimbriae of right uterine tube
6. Right ovarian ligament
7. Left ovarian ligament
8. Left round ligament
9. Right round ligament
10. Broad ligament
11. Urinary bladder
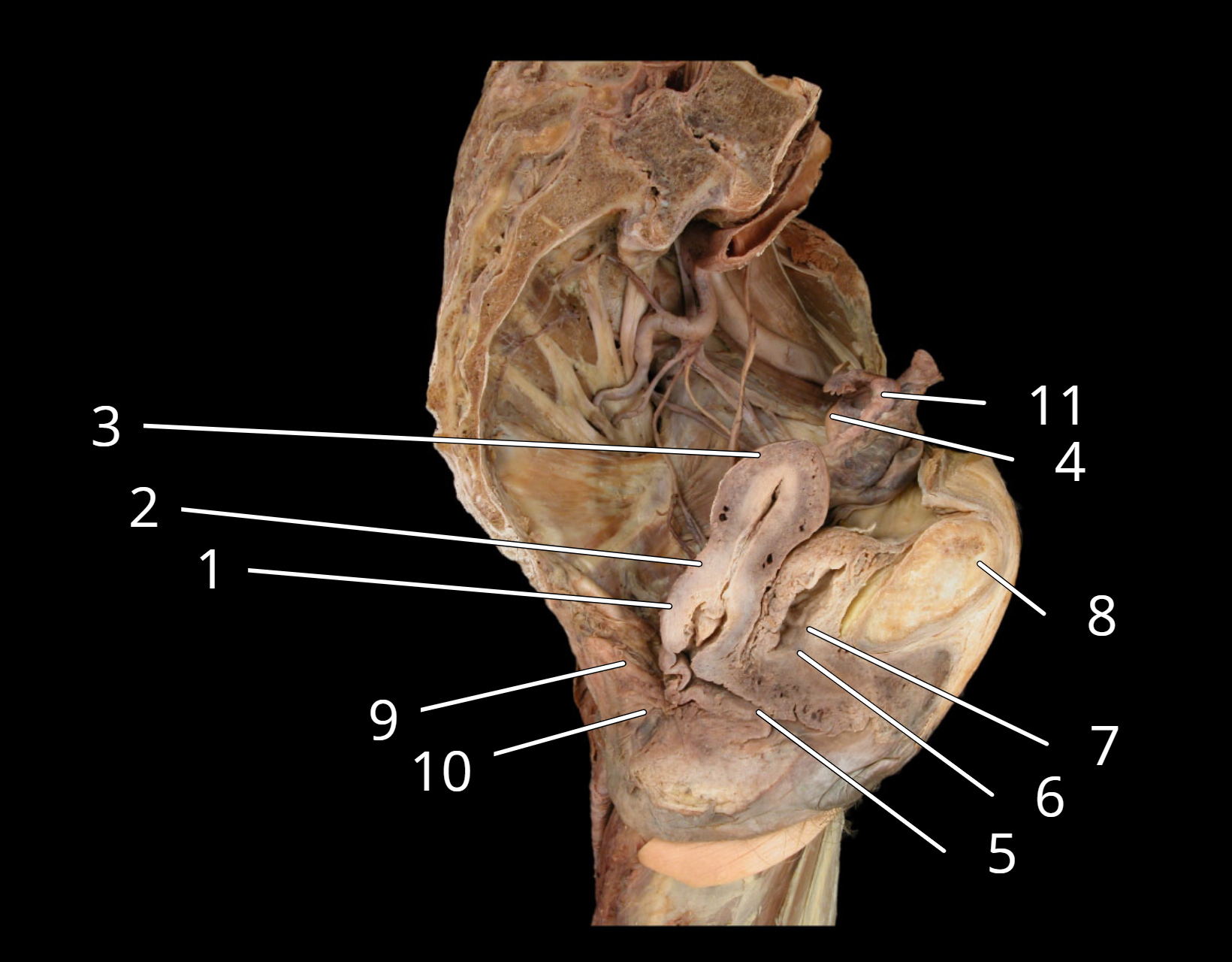
Female reproductive structures, sagittal view
1. Cervix of uterus
2. Body of uterus
3. Fundus of uterus
4. Ovary
5. Vagina
6. Urethra
7. Urinary bladder
8. Pubic symphysis
9. Rectum
10. Anus
11. Uterine tube
Arrange the structures at right according to the pathway of sperm. Start with its origin in the testis (1) and end with the external environment (7).
1. ___ a. membranous urethra
2. ___ b. ductus deferens
3. ___ c. prostatic urethra
4. ___ d. epididymis
5. ___ e. spongy urethra
6. ___ f. seminiferous tubule
7. ___ g. ejaculatory duct
1.seminiferous tubule
2.epididymis
3.ductus deferens
4.ejaculatory duct
5.prostatic urethra
6.membranous urethra
7.spongy urethra
What is the name of the tough fibrous layer that surrounds both the testes and the ovaries?
tunica albuginea
What is the name of the complex venous network that arises from the testicular veins?
pampiniform plexus
What is the name of the finger like projections of the uterine tubes that caress each ovary?
fimbriae
The ovary is connected to the uterine wall via which ligament?
ovarian ligament
Which structure of the female is homologous to the penis in the male?
the clitoris
What are the two major functions of the ovaries?
producing oocytes
secreting sex hormones
A vasectomy is a surgical form of male birth control and a very common procedure. The purpose is to prevent the release of sperm from the male reproductive tract.
1. In a vasectomy, which structure of the male reproductive tract is cut?
2. Does this procedure prevent the production of sperm? Why or why not?
3. How are sperm affected by this procedure? What happens to them?
4. Is this procedure reversible? Why or why not?
In a vasectomy, the vas deferens (also called the ductus deferens) is cut. This is the tube that carries sperm from the epididymis to the urethra.
No, a vasectomy does not prevent sperm production. The testes continue to produce sperm normally after a vasectomy because the procedure only blocks the transport pathway, not the production sites. Testosterone production also remains unaffected.
After a vasectomy, sperm are still produced in the testes but cannot travel through the reproductive tract to be ejaculated. The sperm cells that are produced are eventually broken down and reabsorbed by the body. This happens naturally as part of normal cell turnover.
Vasectomies are potentially reversible through a procedure called a vasovasostomy, where the cut ends of the vas deferens are surgically reconnected. However, success rates vary (typically 40-90%) depending on:
Time elapsed since the vasectomy
Surgical technique used
Development of anti-sperm antibodies
Presence of other fertility factors