Psychopathology Midterm
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
specific phobias
a. marked fear or anxiety about a specific object or situation (e.g. flying, heights, animals. receiving an injection, seeing blood)
b. the phobic object or situation almost always provokes immediate fear or anxiety
c. the phobic object or situation is actively avoided or endured with intense fear or anxiety
d. the fear or anxiety is out of proportion to the actual danger posed by the specific object or situation and to the sociocultural context
e. the fear, anxiety, or avoidance is persistent, typically lasting 6 months or more
f. causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
g. the disturbance is not better explained by symptoms of another mental disorder
types of specific phobias
-animal (e.g. spiders, insects, dogs)
-natural environment (e.g. heights, storms, and water)
- blood-injection-injury (e.g. needles, invasive medical procedures)
-situational (e.g. airplanes, elevators, or enclosed places
-other
panic disorder
a. recurrent unexpected panic attacks
b. at least one of the attacks has been followed by 1 month (or more) of one or both of the following:
1. persistent concern or worry about additional panic attacks
2. a significant maladaptive change in behavior related to attacks (e.g. to avoid panic attacks)
c. the disturbance is not do to substance or medical condition
d. not better explained by another mental disorder (e.g. does not only occur in social situations or else it would be social anxiety disorder)
panic attack symptoms
an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which 4 or more symptoms occur
13 symptoms of panic attacks
1. palpitations, pounding heart, or accelerated heart rate
2. sweating
3. trembling or shaking
4. sensations of shortness of breath or smothering
5. feelings of choking
6. chest pains or discomfort
7. nausea or abdominal distress
8. feeling dizzy, unsteady, light-headed, or faint
9. chills or heat sensations
10. paresthesia (numbness or tingling sensations)
11. derealization (feelings of unreality) or depersonalization (being detached from oneself)
12. fear of losing control or "going crazy"
13. fear of dying
social anxiety disorder
a. marked fear or anxiety about one or more social situations in which the individuals is exposed to possible scrutiny by others. ex: social interactions, being observed, and performing in front of others
b. the individual fears that he or she will act in a way or show anxiety symptoms that will be negatively evaluated
c. the social situations almost always provoke fear or anxiety
d. the social situations are avoided or endured with intense fear or anxiety
e. the fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context
f. the fear, anxiety, or avoidance is persistent, typically lasting 6+ months
g. causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
h. not attributable to the physiological effects of a substance or medical condition
i. not better explained by the symptoms of another mental disorder, such as panic disorder.
j. if another medical condition is present, the fear, anxiety, or avoidance is clearly unrelated or is excessive
Performance only: if the fear is restricted to speaking or performing in public
generalized anxiety disorder
a. excessive anxiety and worry (apprehension expectancy), occurring more days than not for at least 6 + months, about a number of events or activities (such as work or school performance)
b. the individual finds it difficult to control the worry
c. the anxiety and worry are associated with 3 or more of the following for more days than not:
1. restlessness or feeling keyed up or on edge
2. being easily fatigued
3. difficulty concentrating or mind going blank
4. irritability
5. muscle tensions
6. sleep disturbance (difficulty falling or staying asleep, or restless, unsatisfying sleep)
7. the anxiety, worry, or physical symptoms causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the disturbance is not attributable to the physiological effects of a substance or medical condition
e. the disturbance is not better explained by another mental disorder
agoraphobia
a. marked fear or anxiety about two or more situations
1. using all forms of transportation
2. being in open spaces
3. being in enclosed places
4. standing in line or being in crowd
5. being outside of the home alone
b. the individual fears or avoids these situations bc of thoughts that escape might be difficult or help might not be available in the vent of developing panic like symptoms or other incapacitating or embarrassing symptoms
c. the agoraphobic situations almost always provoke fear or anxiety
d. the agoraphobic situations are actively avoided, require the presence of a companion, or are endured with intense fear or anxiety
e. the fear or anxiety is out of proportion to the actual danger posed by the agoraphobic situations and to the sociocultural context
f. the fear, anxiety , or avoidance is persistent, lasting 6+ months
g. causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
h. if another medical condition is present, the fear, anxiety, or avoidance is clearly excessive
i. not better explained by another mental disorder
“false alarms”
Has a nearly identical fear response , but happens in a context that is not dangerous
Can be situationally bound or situationally predisposed
In panic, the contextual reason for the fear is not identified in the moment
Learning history that unpredictable bodily sensations should be feared also contributes
Learned Alarms
Physiological sensations of alarm (false or true) become associated with fear responding
Fear of fear (i.e., fear arousal in response to the physical sensations of fear arousal) takes hold
Learned alarm perpetuates fear responding in ways that individuals find difficult to predict
Mowrer’s two-factor learning theory (classical and operant conditioning)
Fear is learned through classical conditioning (associations)
Fear is maintained via operant conditioning - avoidance negatively reinforced through anxiety reduction
learning can help navigate through what one fears, but reinforcing avoidance is only a temporary mediation. This is how it is reinforced and maintained. Avoidance is the operant conditioning part, learning what will cause the fear is the classical conditioning part
Classical conditioning: fear is acquired from the warning signal
o A neutral stimulus is presented and is followed by electric shock (what will be fear by the rat) after the pairing the rat shows fear responses from the neutral stimulus
· Operant conditioning: fear is maintained despite “problem solving”
o The shock is delayed after the warning signal and learns to avoid the shock, but the fear is still there
o The avoidant behavior is reinforced by the removal of the anticipated shock
o Negative reinforcement, avoidance maintains
obsessive-compulsive disorder (OCD)
a. presence of obsessions, compulsions, or both:
b. the obsessions or compulsions are time-consuming (e.g., take more than 1 hour per day) or cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
c. the symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical conditions
d. the disturbance is not better explained by the symptoms of another mental disorder
obsessions
1. recurrent and persistent thoughts, urges, or images that are experienced, at some time during the disturbance, as intrusive and unwanted, and that in most individuals cause marked anxiety or distress
2. the individual attempts to ignore or suppress such thoughts, urges, or images, or to neutralize them with some other thought or action (i.e., by performing a compulsion)
compulsions
1. repetitive behaviors (e.g., hand washing, ordering, checking) or mental acts (e.g., praying, counting, repeating words silently) that the individual feels drive to perform in response to an obsession or according to rules that must be applied rigidly
2. the behaviors or mental acts are aimed at preventing or reducing anxiety or distress, or preventing some dreaded event or situation; however, these behaviors or mental acts are not connected in a realistic way with what they are designed to neutralize or prevent, or are clearly excessive
specify if (for OCD)
-with good or fair insight: the individual recognizes that obsessive-compulsive disorder beliefs are definitely or probably not true or that they may or may not be true
-with poor insight: the individual thinks obsessive-compulsive disorder beliefs are probably true
-with absent insight/delusional beliefs: the individual is completely convinced that obsessive-compulsive disorder beliefs are true
-tic related: the individual has a current or past history of a tic disorder
hoarding disorder
a. persistent difficulty discarding or parting with possessions, regardless of their actual value
b. this difficulty is due to perceived need to save the items and to distress associated with discarding them
c. the difficulty discarding possessions results in the accumulation of possessions that congest and clutter active living areas and substantially compromises their intended use. if living areas are uncluttered, it is only because of the interventions of third parties
d. the hoarding causes clinically significant distress or impairment in social, occupational, or other important areas of functioning (including maintaining a safe environment for self and others)
e. the hoarding is not attributable to another medical condition (e.g., brain injury, cerebrovascular disease, Prader-willi syndrome)
f. the hoarding is not better explained by the symptoms of another mental disorder (e.g., obsessions in obsessive-compulsive disorder, etc.)
specify if (hoarding)
-with excessive acquisition: if difficulty discarding possessions in accompanied by excessive acquisition of items that are not needed or for which there is no available space
-with good or fair insight: the individual recognized that hoarding-related beliefs and behaviors (pertaining to difficulty discarding items, clutter, or excessive acquisitions) are problematic
-with poor insight: the individual is mostly convinced that hoarding-related beliefs and behaviors (pertaining to difficulty discarding items, clutter, or excessive acquisition) are not problematic despite evidence to the contrary
-the absent insight/delusional beliefs: the individual is completely convinced that hoarding-related beliefs and behaviors (pertaining to difficulty discarding items, clutter, or excessive acquisitions) are not problematic despite evidence to the contrary
body dysmorphic disorder
a. preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others
b. at some point during the course of the disorder, the individual has performed repetitive behaviors (e.g., mirror checking, excessive grooming, skin picking, reassurance seeking) or mental acts (e.g., comparing his or her appearance with that of others) in response to the appearance concerns
c. the preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the appearance preoccupation is not better explained by concerns with body fat or weight in an individual whose symptoms meet diagnostic criteria for an eating disorder
specify if (body dysmorphic)
-with muscle dysmorphia: the individual is preoccupied with the idea that his or her body build is too small or insufficiently muscular. this specifier is used even if the individual is preoccupied with other body areas, which is often the case
indicate degree of insight regarding body dysmorphic disorder beliefs (e.g., "i look ugly" or "i look deformed")
-with good or fair insight: the individual recognizes that the body dysmorphic disorder beliefs are definitely or probably not true or that they may or may not be true
-with poor insight: the individual thinks that the body dysmorphic disorder beliefs are probably true
-with absent insight/delusional beliefs: the individual is completely convinced that the body dysmorphic disorder beliefs are true.
trichotillomania (hair-pulling disorder)
a. recurrent pulling out one's hair, resulting in hair loss
b. repeated attempts to decrease or stop hair pulling
c. the hair pulling causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the hair pulling or hair loss is not attributable to another medical condition (e.g., a dermatological condition)
e. the hair pulling is not better explained by the symptoms of another mental disorder (e.g., attempts to improve a perceived defect or flaw in appearance in body dysmorphic disorder)
excoriation (skin-picking disorder)
a. recurrent skin picking resulting in skin lesions
b. repeated attempts to decrease or stop skin picking
c. the skin picking causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the skin picking is not attributable to the physiological effects of a substance (e.g., cocaine) or another medical condition (e.g., scabies)
e. the skin picking is not better explained by symptoms of another mental disorder (e.g., delusions or tactile hallucinations in a psychotic disorder, etc.)
Bipolar I
For a diagnosis of bipolar I disorder, it is necessary to meet the following criteria for a manic episode.
The manic episode may have been preceded by and may be followed by hypomanic or major
depressive episodes.
If the manic episode is not in the presence of the psychotic disorder or psychosis
Incarceration can substitute hospitalization, there needs to be some sort of institutional control
Manic Episode
A. A distinct period of abnormally and persistently elevated, expansive, or irritable mood and abnormally and persistently increased activity or energy, lasting at least 1 week and present most of the day, nearly every day (or any duration if hospitalization is necessary).
B. During the period of mood disturbance and increased energy or activity, three (or more) of the following symptoms (four if the mood is only irritable) are present to a significant degree and represent a noticeable change from usual behavior:
Inflated self-esteem or grandiosity.
Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
More talkative than usual or pressure to keep talking.
Flight of ideas or subjective experience that thoughts are racing.
Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation (i.e.,purposeless non-goal-directed activity).
Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
C. The mood disturbance is sufficiently severe to cause marked impairment in social or occupational functioning or to necessitate hospitalization to prevent harm to self or others, or there are psychotic features.
D. The episode is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication, other treatment) or another medical condition.
Note: A full manic episode that emerges during antidepressant treatment (e.g., medication,electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a manic episode and, therefore, a bipolar I diagnosis.
Note: Criteria A–D constitute a manic episode. At least one lifetime manic episode is required for the diagnosis of bipolar I disorder
hypomanic episode
a. a distinct periof of abnormally and persistently elevated, spansive, or irritable mood and abnormally persistently increased activity or energy lasting at least 4 consecutive days and present most of the days nearly every day
b. during the period of mood disturbance and increased energy and activity three (or more) of the following symptoms (four if the mood is only irritable) have persisted, represent a noticeable change from usual behavior and have been present to significant degree:
1. inflated self esteem or grandiosity
2. decreased need for sleep (e.g., feels rested after only 3 hours of sleep)
3. more talkative than usual or pressure to keep talking
4. flight of ideas or subjective experience that thoughts are racing
5. distractibility (i.e., attention too easily drawn to unimportant or irrelevant stimuli) as reported or observed
6. increase in goal-directed activity (either socially, or at work or school or sexually) or psychomotor agitation
7. excessive involevment in acitvities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments)
c. the episode is associated withan unequivocal change in functioning that is characteristic of the individual when not symptomatic
d. the disturbance in mood and the change is functioning are observable by others
e. the episode is not severe enough to cause marked impairment in social or occupational functioning or to necessitate hospitalization. if there are psychotic features, the episode is by definition manic
f. the episode is not attributable to the physiological effects of a substance or medical disorder
Bipolar with mixed features (mania/hypomania)
a. full criteria are met for a manic episode or hypomanic episode and at least three of the following symptoms are present during the majority of days of the current or most recent episode of mania or hypomania (this means mania with 3 depressive symptoms):
1. prominent dysphoria or depressed mood as indicated by either subjective report (e.g., feels sad or empty) or observation made by others (e.g., appears tearful)
2. diminished interest or pleasure in all, or almost all, activities (as indicated by either subjective account or observation made by others)
3. psychomotor retardation nearly every day (observable by others; not merely subjective feelings or being slowed down)
4. fatigue or loss of energy
5. feelings of worthlessness or excessive or inappropriate guilt ( not merely self-approach or guilt about being sick)
6. recurrent thoughts of death (not just fear of dying); recurrent suicidal ideation without a specific plan; a specific suicide plan; or a suicide attempt)
b. mixed symptoms are observable by others and represent a change from the person's usual behavior
c. for individuals whose symptoms meet full episode criteria for both mania and depression simultaneously, the diagnosis should be manic episode, with mixed features, due to marked impairment and clinical severity of full mania (in order to have mixed features, you need a manic episode with 3 depressive symptoms during the episode)
d. the mixed symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication or other treatment)
Bipolar with mixed features (depressive)
a. full criteria are met for a major depressive episode, and at least three of the following manic/hypomanic symptoms are present during the majority of days of the current or most recent episode of depression (this means mainly depressive with 3 mania features)
1. elevated, expansive mood
2. inflated self-esteem or grandiosity
3. more talkative than usual or pressure to keep talking
4. flight of ideas or subjective experience that thoughts are racing
5. increase in energy or goal-directed activity (either socially, at work or school, or sexually)
6. increased or excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unregulated buying sprees, sexual indiscretions, or foolish business investments)
7. decreased need for sleep (feeling rested despite sleeping less than usual; to be contrasted with insomnia)
b. mixed symptoms are observable by others are represent a change from the person's usual behavior
c. for individuals whose symptoms meet full episode criteria for both mania and depression simultaneously, the diagnosis should be manic episode, with mixed features (mania trumps all)
d. the mixed symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication or other treatment)
Bipolar with rapid cycling
presence of at least four mood episodes in the previous 12 months that meet the criteria for manic, hypomanic, or major depressive episode in bipolar I or that meet the criteria for hypomanic or major depressive episode in bipolar II disorder. need two months separation if same polarity. doesn't need to be 2 months if different polarity
Bipolar II disorder
for the diagnosis of bipolar II disorder, it is necessary to meet the following criteria for a current or past hypomanic episode and the following criteria for a current or past major depressive episode
(4 or more mood episodes in 12 months; if mood episodes are of same polarity, must be separated by 2 months)
bipolar II disorder (major depressive episode)
A. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
1. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, or hopeless) or observation made by others (e.g., appears tearful).
2. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
3. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day.
4. Insomnia or hypersomnia nearly every day.
5. Psychomotor agitation or retardation nearly every day (observable by others; not merely subjective feelings of restlessness or being slowed down).
6. Fatigue or loss of energy nearly every day.
7. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
8. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
9. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, a suicide attempt, or a specific plan for committing suicide.
b. met criteria for hypomanic episode & depressive episode
c. never been a manic episode
d. not better explained by psychotic disorder
e. Symptoms of depression or unpredictability caused by frequent alternation between periods of depression and hypomania cause distress/impairment
cyclothymic disorder
a. for at least 2 years there have been numerous periods with hypomanic symptoms that do not meet criteria for a hypomanic episode (don't last 4 days or not enough episodes) and numerous periods with depressive symptoms that do not meet criteria for a major depressive episode (don't last two weeks)
b. during the 2 year period, criteria a symptoms have been present for at least half the time and the individual has not been without the symptoms for more than 2 months at a time
c. criteria for a major depressive, manic, or hypomanic episode have never been met
d. the symptoms in criteria a are not better explained by a psychotic disorder
e. the symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse) or another medical condition
f. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
Obsessive-compulsive disorder (OCD) distinguished from obsessive-compulsive personality disorder (OCPD)
No obsessions in personality disorder. Just rule governed and very strict. egosyntonic.
Preoccupation with orderliness, perfectionism, and control, which interferes with flexibility, openness, and efficiency.
Compulsions: Behaviors are not a reaction to intrusive obsessions, but rather a way to maintain the order and control that is central to the personality.
Obsessions in OCD distinguished from worry in generalized anxiety disorder
•Obsessions
•Primarily ego-dystonic
•Thoughts are recognized as irrational or considered bizarre by the person experiencing them
•Thoughts are unwanted and provoke resistance
•Worry
•Primarily ego-syntonic
•Usually rational (i.e., focused on current real-life problems), but exaggerated
•Thoughts may be seen as useful (e.g., problem solving) and are seldom resisted
worry in GAD: primarily ego-syntonic (ok with having thought because it fits into the world, not unwanted), rational but exaggerated, thoughts may be seen as useful (problem solving)band are seldom
obsessions in OCD: primarily ego-dystonic, thoughts are recognized as irrational, thoughts are unwanted and provoke resistance
sometimes people diagnose GAD when it's "pure O" (just obsessions) and vice versa
ego-dystonic is in OCD. the thought are not wanted and are in conflict with the self
Obsessions in OCD distinguished from rumination in depression
OCD obsessions are unwanted, egodystonic, a thought they wish they didn’t have keeps returning
rumination is about regret about the past, why am i so bad, why do i feel bad?
ego syntonic
behaviors/thoughts align with personal values and goals, it is okay to have a thought, usually rational
•Worry
•Primarily ego-syntonic
•Usually rational (i.e., focused on current real-life problems), but exaggerated
•Thoughts may be seen as useful (e.g., problem solving) and are seldom resisted
ego dystonic
you do not want to have this thought
Disruptive Mood Dysregulation Disorder
a. severe recurrent temper outbursts manifested verbally (e.g., verbal rages) and/or behaviorally (e.g., physical aggression toward people or property) that are grossly out of proportion in intensity or duration to the situation or provocation
b. the temper outbursts are inconsistent with development level
c. the temper outbursts occur, on average, three or more times per week
d. the mood between temper outbursts is persistently irritable or angry most of the day, nearly every day, and is observable by others (e.g., parents, teachers, peers)
e. criteria a-d have been present for 12 or more months. Throughout that time, the individual has not had a period lasting 3 or more consecutive months without all of the symptoms in criteria a-d
f. criteria a and d are present in at least two of three settings (i.e., at home, at school, with peers) and are severe in at least one of these
g. the diagnosis should not be made for the first time before age 6 years or after 18 years
h. by history or observation, the age of onset of criteria a-e is before 10 years
i. there has never been a distinct period lasting more than 1 day during which the full symptom criteria, except duration, for a manic or hypomanic episode have been met
j. the behaviors do not occur exclusively during an episode of major depressive disorder and are not better explained by another mental disorder
k. the symptoms are not attributable to the physiological effects of a substance or another medical or neurological condition
Major Depressive Disorder (MDD)
a. five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning; at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure
1. depressed mood most of the day, nearly every day
2. marked diminished interests or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation)
3. significant weight loss when not dieting or weight gain (e.g., a change or more than 5% of body weight in a month), or a decrease or increase in appetite nearly every day
4. insomnia or hypersomnia nearly every day
5. psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings or restlessness or being slowed down)
6. fatigue or loss of energy nearly every day
7. feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self reproach or guilt about being sick)
8. diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others)
9. recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide
b. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
c. the episode attributable to the physiological effects of a substance or another medical condition
d. at least one major depressive episode is not better explained a psychotic disorder
e. there has never been a manic episode
persistent depressive disorder
a. depressed mood for most of the day, for more days than not, as indicated by either subjective account or observation by others for at least 2 years
b. presence while depressed of two (or more) of the following:
1. poor appetite or over eating
2. insomnia or hypersomnia
3. low energy or fatigue
4. low self esteem
5. poor concentration or difficulty making decisions
6. feelings of hopelessness
c. during the 2 year period of the disturbance the individual has never been without the symptoms in criteria a and b than 2 months at a time
d. criteria for a major depressive disorder may be continuously present for 2 years
e. there has never been a manic episode or a hypomanic episode
f. the disturbance is not better explained by a psychotic disorder
g. the symptoms are not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication) or another medical condition (e.g., hypothyroidism)
h. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
posttraumatic stress disorder (a criteria)
a. exposure to actual or threatened death, serious injury, or sexual violence in 1 or more ways
1. directly experiencing the traumatic event
2. witnessing, in person, the events as it occurred to others
3. learning that the traumatic event occurred to a close family member or a close friend. in cases of actual threatened death of a family member or friend the events must have been violent or accidental
4. experiencing repeated or extreme exposure to aversive detailed or traumatic event (e.g., first responders collecting human remains; police officers repeatedly exposed to details of child abuse)
posttraumatic stress disorder (b criteria, intrusion)
b. presence of one (or more) of the following intrusion symptoms associated with the traumatic events, beginning after the traumatic event occurred:
1. recurrent, involuntary, and intrusive distressing memories of the traumatic event
2. recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event
3. dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic events were recurring
4. intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic events
5. marked physiological reactions to internal or external cues that symbolize or resemble an aspect of the traumatic events
posttraumatic stress disorder (c criteria, avoidance of stimuli)
c. persistent avoidance of stimuli associated with the traumatic events, beginning after traumatic events occurred as evidenced by one or both of the following:
1. avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic events
2. avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event
posttraumatic stress disorder (d criteria, negative alterations in cognition and mood)
d. negative alterations in cognitions and mood associated with the event, beginning or worsening after the traumatic event occurred as evidenced by 2 (or more) or the following:
1. inability to remember an important aspect of the traumatic event (typically due to dissociative amnesia and not to other factors such as a head injury, alcohol, or drugs)
2. persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (e.g., "I am bad," "no one can be trusted", "the world is completely dangerous,")
3. persistent, distorted cognitions about the cause or consequences of the traumatic event that lead the individual to blame himself/herself or others
4. persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame)
5. markedly diminished interest or participation in significant activities
6. feelings of detachment or estrangement from others
7. persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings)
posttraumatic stress disorder (e criteria, alterations in arousal/reactivity)
e. marked alterations in arousal and reactivity associated with the traumatic events, beginning or worsening after the traumatic event occurred, as evidenced by 2 (or more of the following:
1. irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects
2. reckless or self-destructive behavior
3. hypervigilance
4. exaggerated startle response
5. problems with concentration
6. sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep)
posttraumatic stress disorder (f-H criteria)
f. duration of the disturbance (criteria b, c, d, and e) is more than 1 month
g. the disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
h. the disturbance is not attributable to the physiological effects of a substance (e.g., medication, alcohol) or another medical condition
acute stress disorder (duration 3 days to 1 month)
a. exposure to actual or threatened death, serious injury, or sexual violence in 1 (or more) of the following ways:
1. directly experiencing the traumatic event
2. witnessing, in person, the event as it occurred to others
3. learning that the event occurred to a close family member or close friend
4. experiencing repeated or extreme exposure to aversive details of the traumatic event (e.g., first responders collecting human remains, police officers repeatedly exposed to details of child abuse)
b. presence of 9 (or more) of the following symptoms from any of the 5 categories of intrusion, negative mood, dissociation, avoidance, and arousal, beginning or worsening after the traumatic event occurred:
c. duration of the disturbance (symptoms in criterion b) is 3 days to 1 month after trauma exposure
d. the disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
e. the disturbance is not attributable to the physiological effects of a substance (e.g., medication or alcohol) or another medical condition (e.g., mild traumatic brain injury) and is not better explained by brief psychotic disorder
acute stress disorder: intrusion symptoms
1. recurrent, involuntary, and intrusive distressing memories of the traumatic events
2. recurrent distressing dreams in which the content and/or affect of the dream are related to the events
3. dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event were recurring
4. intense or prolonged psychological distress or marked physiological reactions in response to internal or external cues that symbolize or resemble an aspect of the traumatic event
acute stress disorder: negative mood symptoms
5. persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings)
acute stress disorder: dissociative symptoms
6. An altered sense of the reality of one's surroundings or oneself (e.g., seeing oneself from another's perspective, being in a daze, time slowing).
7. Inability to remember an important aspect of the traumatic event(s) (typically due to dissociative amnesia and not to other factors such as head injury, alcohol, or drugs).
acute stress disorder: avoidance symptoms
8. Efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
9. Efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s).
acute stress disorder: arousal symptoms
10. Sleep disturbance (e.g., difficulty falling or staying asleep, restless sleep).
11. Irritable behavior and angry outbursts (with little or no provocation), typically expressed as verbal or physical aggression toward people or objects.
12. Hypervigilance.
13. Problems with concentration.
14. Exaggerated startle response.
adjustment disorders
a. The development of emotional or behavioral symptoms in response to an identifiable stressor occurring within 3 months of the onset of the stressor
b. these symptoms or behaviors are clinically significant, as evidenced by one or both of the following:
1. marked distress that is out of proportion to the severity or intensity of the stressor, taking into account the external context and the cultural factors that might influence symptoms severity and presentation
2. significant impairment in social, occupational, or other important areas of functioning
c. the stress-related disturbance does not meet the criteria for another mental disorder and is not merely an exacerbation of a preexisting mental disorder
d. the symptoms do not represent normal bereavement and are not better explained by prolonged grief disorder
e. once the stressor or its consequences have terminated, the symptoms do not persist for more than an additional 6 months (6 months after the stressor is gone)
adjustment disorders specify if…
F43.21 With depressed mood: Low mood, tearfulness, or feelings of hopelessness are predominant.
F43.22 With anxiety: Nervousness, worry, jitteriness, or separation anxiety is predominant.
F43.23 With mixed anxiety and depressed mood: A combination of depression and anxiety is predominant.
F43.24 With disturbance of conduct: Disturbance of conduct is predominant.
F43.25 With mixed disturbance of emotions and conduct: Both emotional symptoms (e.g., depression, anxiety) and a disturbance of conduct are predominant.
F43.20 Unspecified: For maladaptive reactions that are not classifiable as one of the specific subtypes of adjustment disorder
prolonged grief disorder (12 months in adults; 6 months in children)
a. the death, at least 12 months ago, of a person who was close to the bereaved individual
b. since the death, the development of a persistent grief response characterized by one or both of the following symptoms, which have been present most days to a clinically significant degree. in addition, the symptom has occurred nearly every day for at least the last month:
1. intense yearning/longing for the deceased person
2. preoccupation with thoughts or memories of the deceased person
c. since the death, at least 3 of the following symptoms have been present most days to a clinically significant degree. in addition, the symptoms have occurred nearly every day for at least the last month:
1. identity disruption (e.g., feeling as though part of oneself has died) since the death
2. marked sense of disbelief about the death
3. avoidance of reminders that the person is dead
4. intense emotional pain (e.g., anger, bitterness, sorrow) related to the death
5. difficulty reintegrating into one's relationships and activities after the death (e.g., problem engaging with friends, pursuing interests, or planning for the future)
6. emotional numbness (absence or marked reduction of emotional experience) as a result of the death
7. feeling that life is meaningless as a result of the death
8. intense loneliness as a result of the death
d. the disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
e. the duration and severity of the bereavement reaction clearly exceed expected social, cultural, or religious norms for the individual's culture and context
f. the symptoms are not better explained by another mental disorder or medical condition
dissociative identity disorder
a. disruption of identity characterized by two or more distinct personality states, which may be described in some cultures as an experience of possession. The disruption in identity involves marked discontinuity sense of self and sense of agency, accompanied by related alterations in affect, behavior, consciousness, memory, perception, cognition, and/or sensory motor functioning. these signs and symptoms may be observed by others or reported by the individual
b. recurrent gaps in the recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting
c. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the disturbance is not a normal part of a broadly accepted cultural or religious practice
e. the symptoms are not attributable to the physiological effects of a substance or other medical condition
dissociative amnesia
a. an inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting
b. the symptoms cause clinically significant distress or impairment in social, occupational, or important areas of functioning
c. the disturbance is not attributable to the physiological effects of a substance (e.g., alcohol or other drug of abuse) or a neurological or other medical condition
d. the disturbance is not better explained by a neurocognitive disorder
depersonalization
experiences of unreality, detachment, or being an outside observer with respect to one's thoughts, feelings, sensations, body, or actions
ex: perceptual alterations, distorted sense of time, unreal or absent self, emotional and/or physical numbing)
Derealization
experiences of unreality or detachment with respect to surroundings (e.g., individuals or objects are experienced as unreal, dreamlike, foggy, lifeless, or visually distorted)
depersonalization/derealization disorder
a. the presence of persistent or recurrent experiences of depersonalization, derealization, or both:
b. during the depersonalization or derealization experiences, reality testing remains intact
c. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
d. the disturbance is not attributable to the physiological effects of a substance or another medical condition
e. the disturbance is not better explained by another mental disorder or dissociative disorder
Bereavement and adjustment vs. prolonged grief disorder
there is a difference in time, symptoms of bereavement/adjustment do not last more than 6 months.
Bereavement/adjustment have symptoms of sadness, anxiety, crying, etc
Prolonged grief disorder characterized by intense yearning, disbelief, etc
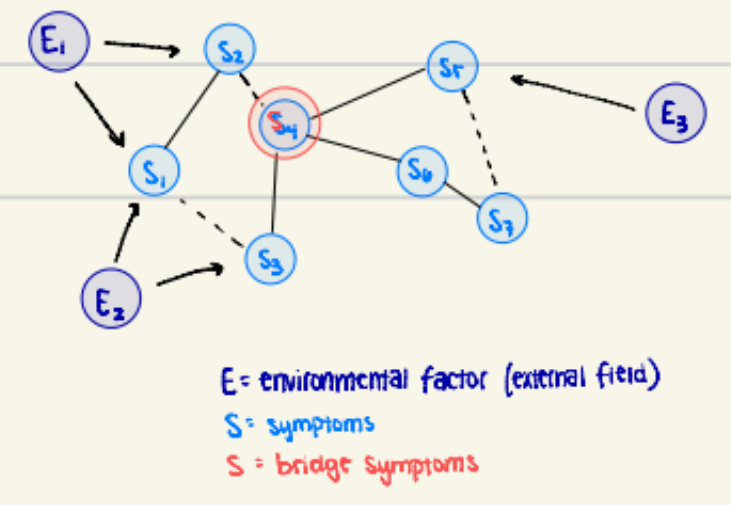
Borsboom's network theory (self-sustaining patterns of distress -- "hysteresis")
When the external factor is no longer playing a role and the nodes or symptoms are in a self sustaining cycle of distress.
many diff causes for a disorder rather than bio
symptom network: symptoms are connected in a network
external field: things in/out body, but out of network, that trigger
big boom(bang) theory (little planets of symptoms everywhere)
Borkovec; Roemer/Orsillo - avoidance theories of worry in GAD.
· Excessive thought in worry as avoidance
· Worry
o suppresses somatic responding and affect
§ somatic response is muted by verbal "problem solving" (e.g., if this happens then ill do y)
o distracts from more emotional topics
o maintained by positive beliefs about worry
§ worry motivates me, helps anticipate negative events, reduces likelihood of negative events, helps problem solve
o reinforced when feared negative consequences don't happen
o prevents emotional processing
· those with GAD have more thoughts when worried and when relaxed than controls, have less imagery than controls, less concrete + less vivid = less distressing imagery
Avoiding:
somatic fear response (stay at constant middle)
emotional topics (worry about other things to avoid talking about what they’ve gone through)
Maintenance:
beliefs about worry
non-occurrence of fears
less concrete + less vivid = less distressing
Newman and Llera - contrast avoidance theory of GAD
o Contrast avoidance model as an extension of established GAD literature and theory. Not avoiding negative emotions, but avoiding negative emotional shift/contrast. This means that people with GAD are constantly worried, so they never experience a peak in symptoms compared to someone who was in a positive state. Then, something happens, and their anxiety peaks, then goes away when the stressor is removed. This avoids the full psychological experience of fear (e.g. rapid heart rate, heightened arousal state, etc.)
· State of worry as "baseline"/preceding negative stimulus dampens negative experience; worry and negative stimulus elicit similar negative states (little contrast).
· Contrast is going from a positive state to a negative state
· This theory is only applicable to GAD
a new-man would be scared of contrasting emotions but they’d lie about it
people with GAD use worry as a way to cope, always staying distressed
staying at medium level of stress to avoid the contrast between positive and negative feelings
this model helps people adjust to emotions rather than avoid
Kashdan – experiential avoidance as a generalized psychological vulnerability
title is the takeaway: everyone experiences some aspect of avoidance; propensity for experimental avoidance
Experiential avoidance (EA): tendency to avoid psychological processes that an individual perceives as negative and unwanted private events. Mediates the relationship between dispositional self-regulation strategies and psychosocial outcomes
· Inflexibility and rigidity (psychopathology)
· Private events: feelings, thoughts, etc.
polar bear, thinking of the polar bear
active effort to hide unpleasant thoughts/feelings/etc
pushing thoughts down increases the amount and intensity
this causes and maintains the anxiety
Lewinsohn’s behavioral theory of depression (reward deprivation/insensitivity)
Characterized depression by a low rate of response contingent positive reinforcement (RCPR)
Three factors of RCPR
· Number of events that are reinforcing to the individual
· The availability of these events
· Focuses mainly on behavioral, no cognition
depression → low energy + fatigue → decrease activity, neglect responsibilities → guilt, hopelessness ←
reward deprivation
previously enjoyed activities no longer provide joy
person who rewarded now punishing
Abramson and Alloy’s cognitive vulnerability hypothesis (helplessness/hopelessness) – internal, stable, global
Hopelessness is a proximal sufficient cause and not a symptom of hopelessness.
Proximal causes:
· Internal: focuses on personal flaws rather than external factors. within, from the person. Ex: this happened because of me
· Stable: problem will persist into the future. lifelong, maintenance factor.
· Global: goes into multiple areas of life, affects many areas of life
Distal causes: cognitive styles
· Diathesis-stress model: a vulnerability; in this model, the depressogenic style is the vulnerability. This is how culture begins to produce the possibility for depression.
Emphasizes the importance of environment AND cognitive processes in the etiology, maintenance, and treatment of depressive symptoms
negative / negative cognitive style
proximal causes: core beliefs
stable - things won’t change
global - world is against me
internal - it’s a me thing i deserve it
→ hopelessness → depression
Beck’s cognitive model – core beliefs, intermediate beliefs, automatic thoughts
· Automatic thoughts:
o quick, evaluative thoughts
o Reflexive preprogrammed
o Not aware of them
o Don't follow logic
· Conditional beliefs
o Attitudes, rules, assumptions
o Unreasonable, rigid, overgeneralized, extreme
o Prevent goal attainment
Conditional beliefs
attitudes, rules, assumptions that are unreasonable and overgeneralized, prevent goal attainment
· Core beliefs/schemas
o About self, others, and environment
o Learn from childhood, develop through experience
o Situations are interpreted through the lenses of core beliefs
Beck’s cognitive triad - self, world, future
· Automatic thoughts are fueled by underlying beliefs about loss, personal deficiency, worthlessness, and hopelessness
o Anticipate harm and danger
· Negative event negative cognitive schema and dysfunctional attitudes
-->cognitive distortions (e.g., catastrophizing, mind reading, emotional reasoning)-
->negative cognitive triad (negative automatic thoughts)
-->depression
depressed people have automatic thoughts about self, world, future
Alloy and Nusslock etiology of bipolar spectrum disorders - immune/inflammatory processes, sleep disruption, heightened BAS/reward sensitivity
Those with bipolar spectrum disorders (BSDs) have over active reward symptoms.
Ex: reward activation events such as job promotion may cause manic/hypomanic symptoms. Reward deactivating events such as failure can trigger depressive episodes.
Heightened sensitivity to reward and onset to bipolar during adolescence (e.g., vulnerable to change, social media in this day and age, hormonal changes)
Reward circadian model: link between reward dysregulation and disrupted sleep/social rhythms may explain mood instability.
Immune system models: high and low reward sensitivity may promote inflammation-->alter brain reward circuits-->forms feedback loop that contributes to bipolar symptoms
o Pinciotti and fisher: percieved trauma and OCD
Individuals with perceived traumatic etiologies consistently endorsed engagement in more obsessions and compulsions, particularly in the past, and implicated themes of symmetry/exactness, repeating, checking, scrupulosity, pathological doubt, and hoarding. Findings suggest that events that occur pre-OCD onset may be likely to be perceived as the catalyst for OCD and may ultimately impact the theme and severity of symptoms in intuitive ways.