Week 27: Bacteria responses and medicine
5.0(1)
Card Sorting
1/42
There's no tags or description
Looks like no tags are added yet.
Last updated 8:43 PM on 4/12/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
43 Terms
1
New cards
Media variations
1. What is the purpose of growing bacteria on different types of media?
2. How can bacteria be identified based on the type of media they grow on?
1. What is the purpose of growing bacteria on different types of media?
2. How can bacteria be identified based on the type of media they grow on?
1. By attempting to grow bacteria on different types of media, it is often possible to identify them based on the outcome.
2. Different types of media support the growth of different bacteria. For example, some media contain nutrients that only certain bacteria can metabolize, while others contain inhibitors that prevent the growth of certain bacteria. By observing which bacteria grow on which media, it is possible to identify them based on their metabolic capabilities and sensitivity to specific inhibitors.
2
New cards
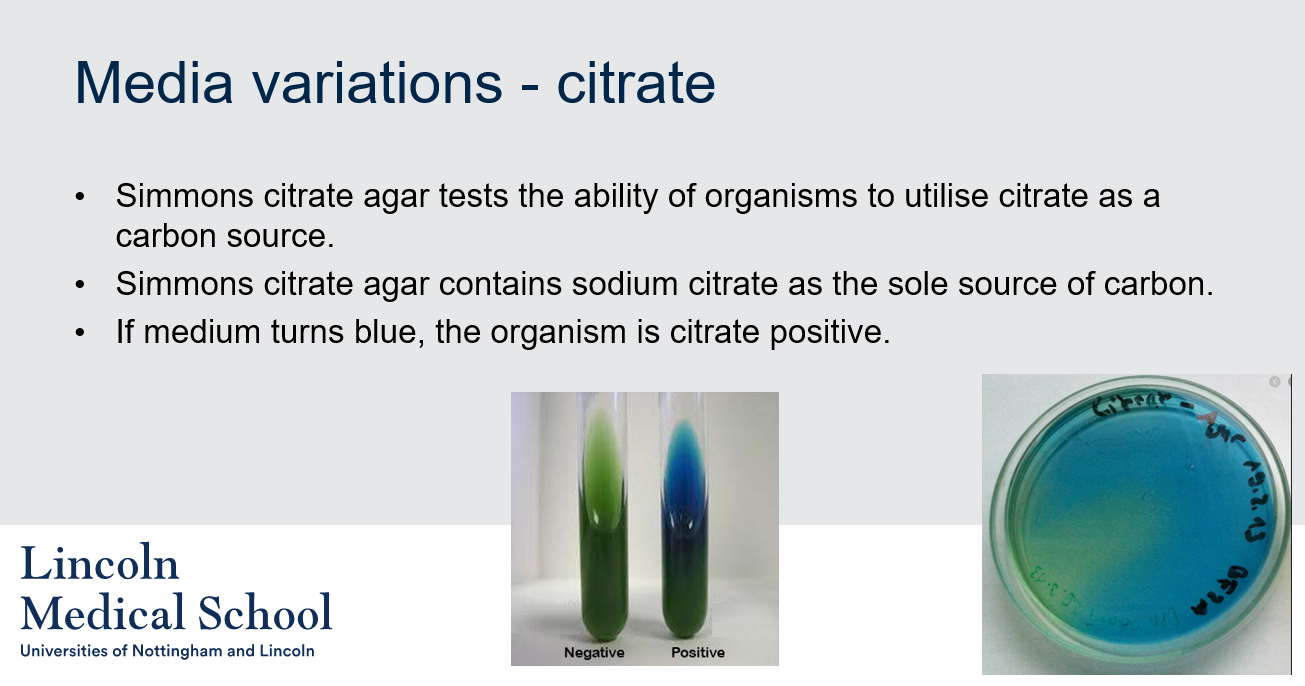
Media variations - citrate
What is Simmons citrate agar used for?
What is Simmons citrate agar used for?
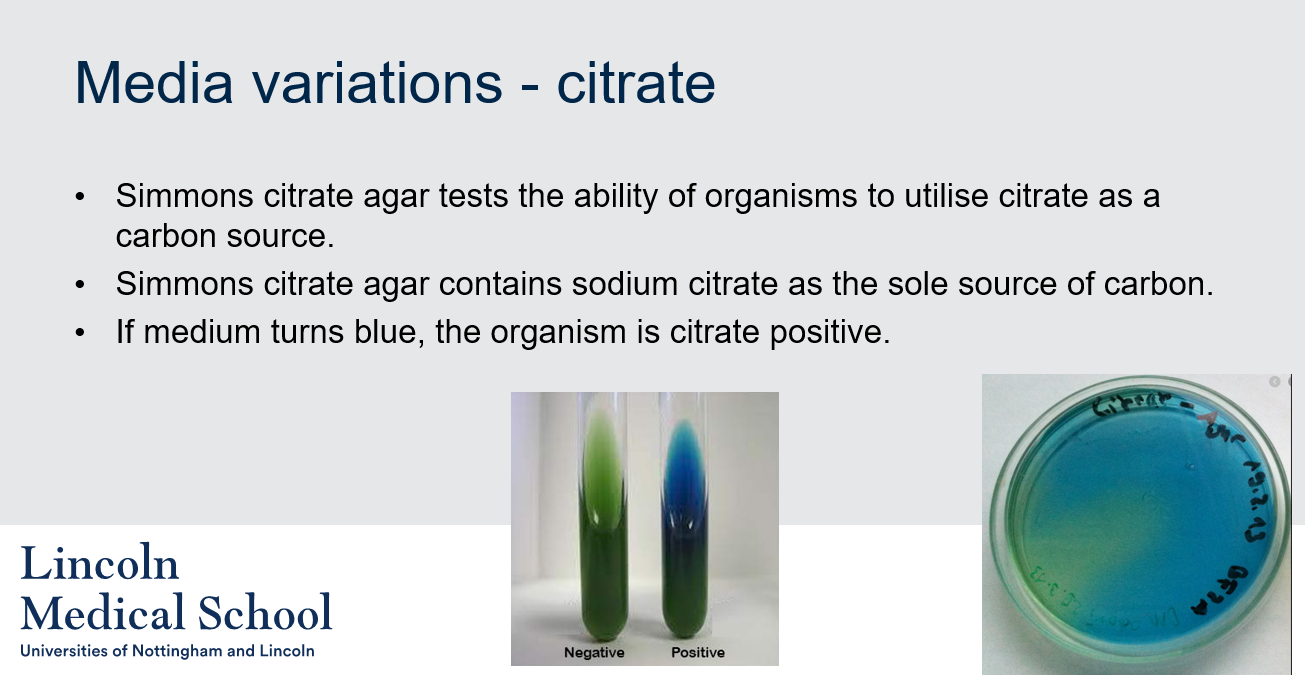
Simmons citrate agar tests the ability of organisms to utilize citrate as a carbon source. Simmons citrate agar contains sodium citrate as the sole source of carbon. If medium turns blue, the organism is citrate positive.
3
New cards
Media variations - citrate
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
4
New cards
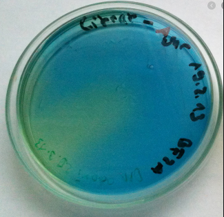
Media variations - citrate
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
5
New cards
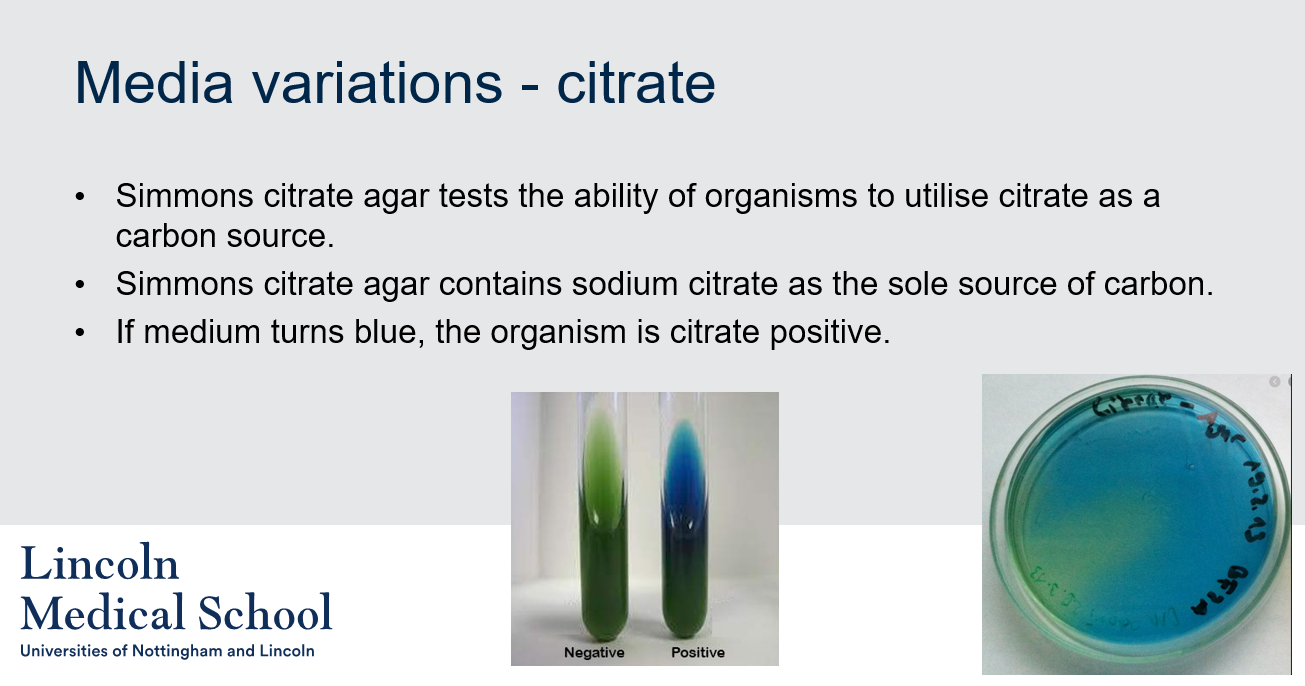
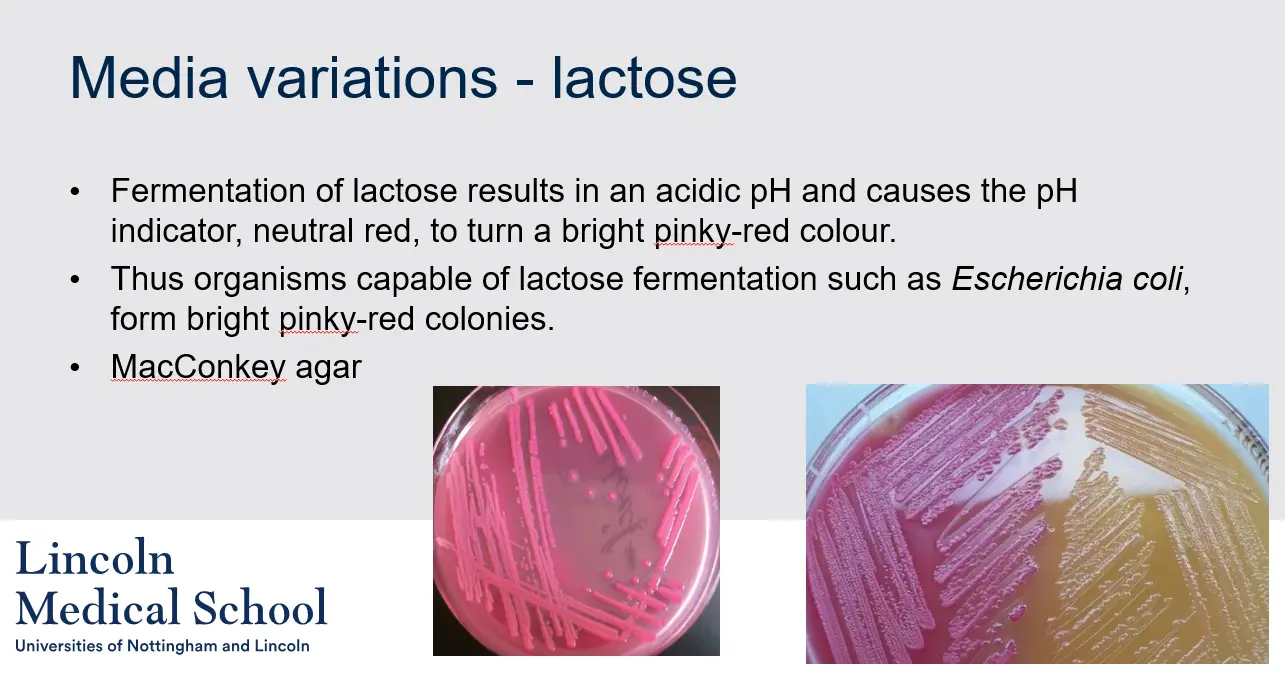
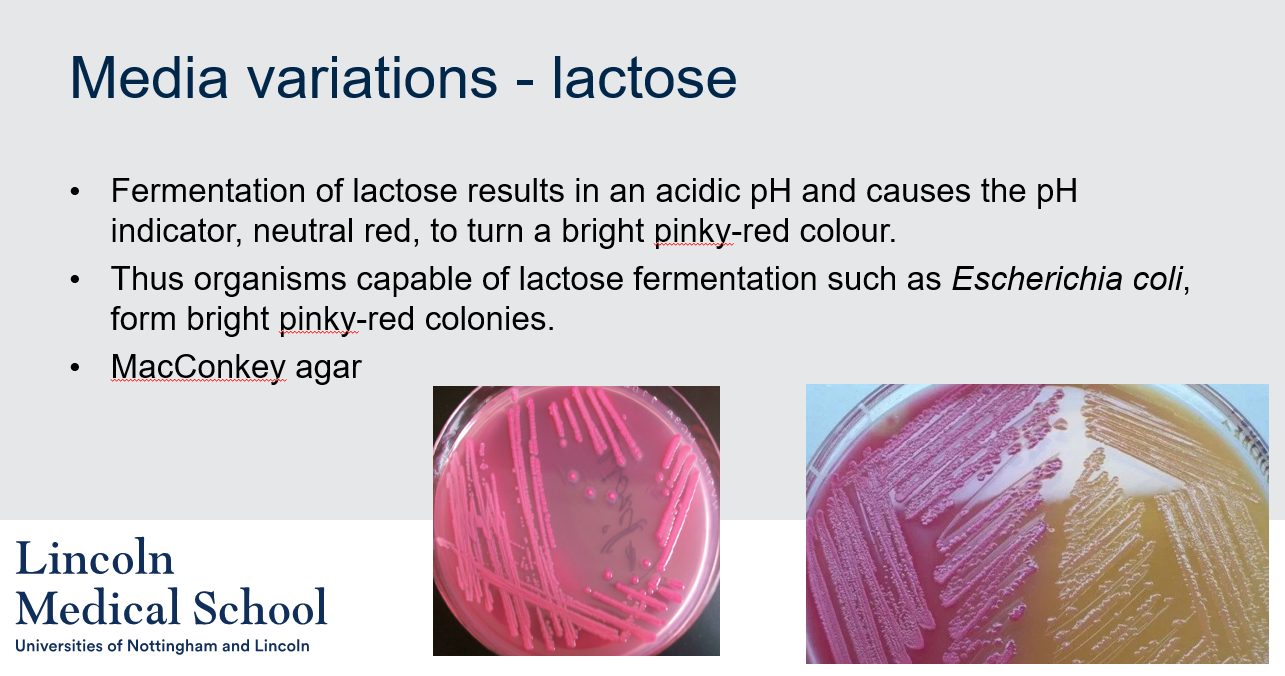
Media variations - lactose
What is the purpose of lactose media variation in microbiology?
What is the purpose of lactose media variation in microbiology?
Lactose media variation is used to differentiate bacteria based on their ability to ferment lactose. The most commonly used lactose-containing medium is MacConkey agar, which contains lactose, bile salts, and a pH indicator. The fermentation of lactose results in an acidic pH and causes the pH indicator, neutral red, to turn a bright pinky-red colour. Bacteria that can ferment lactose, such as Escherichia coli, will produce pink or red colonies on MacConkey agar, while bacteria that cannot ferment lactose will produce colorless or pale colonies.
6
New cards

Media variations - lactose
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
7
New cards

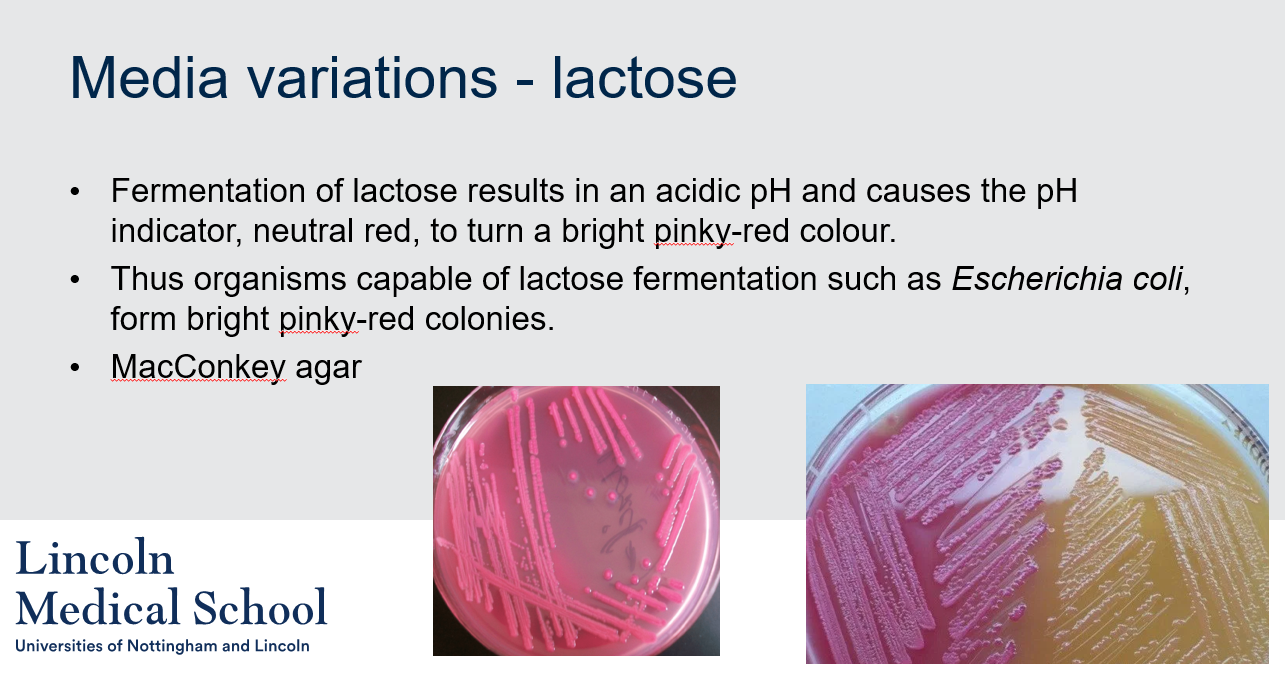
Media variations - lactose
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
8
New cards
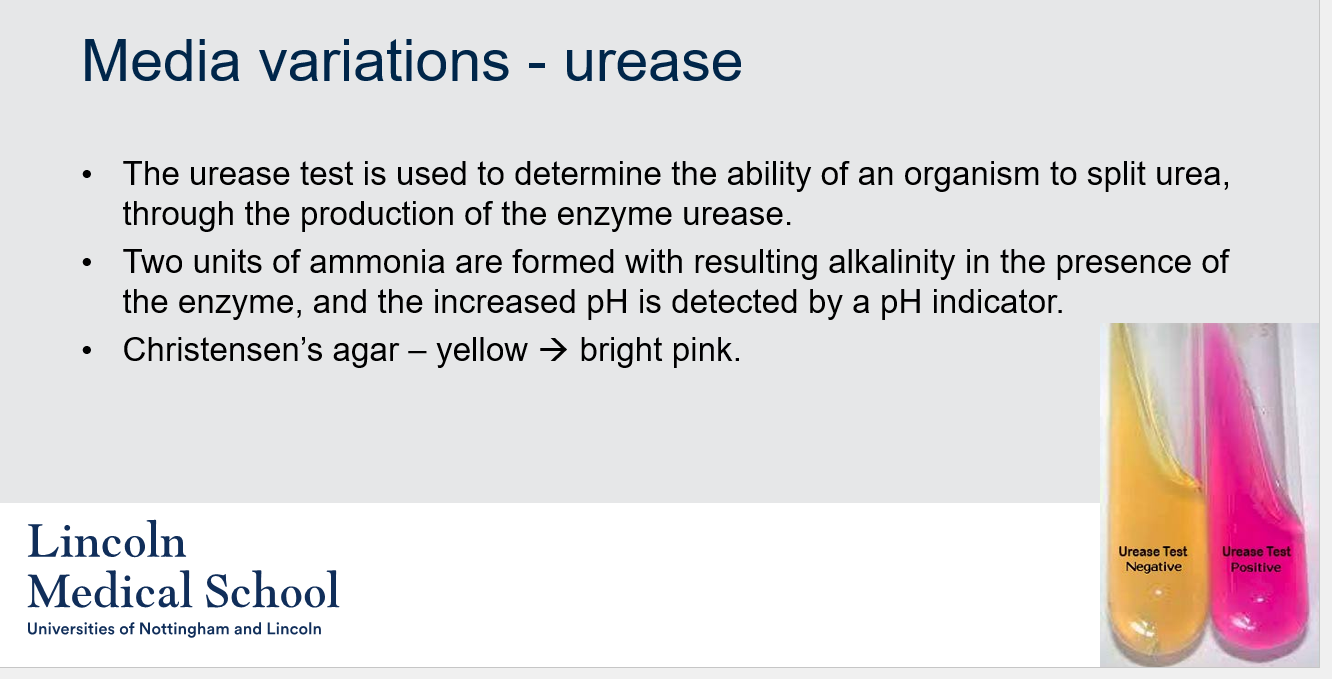
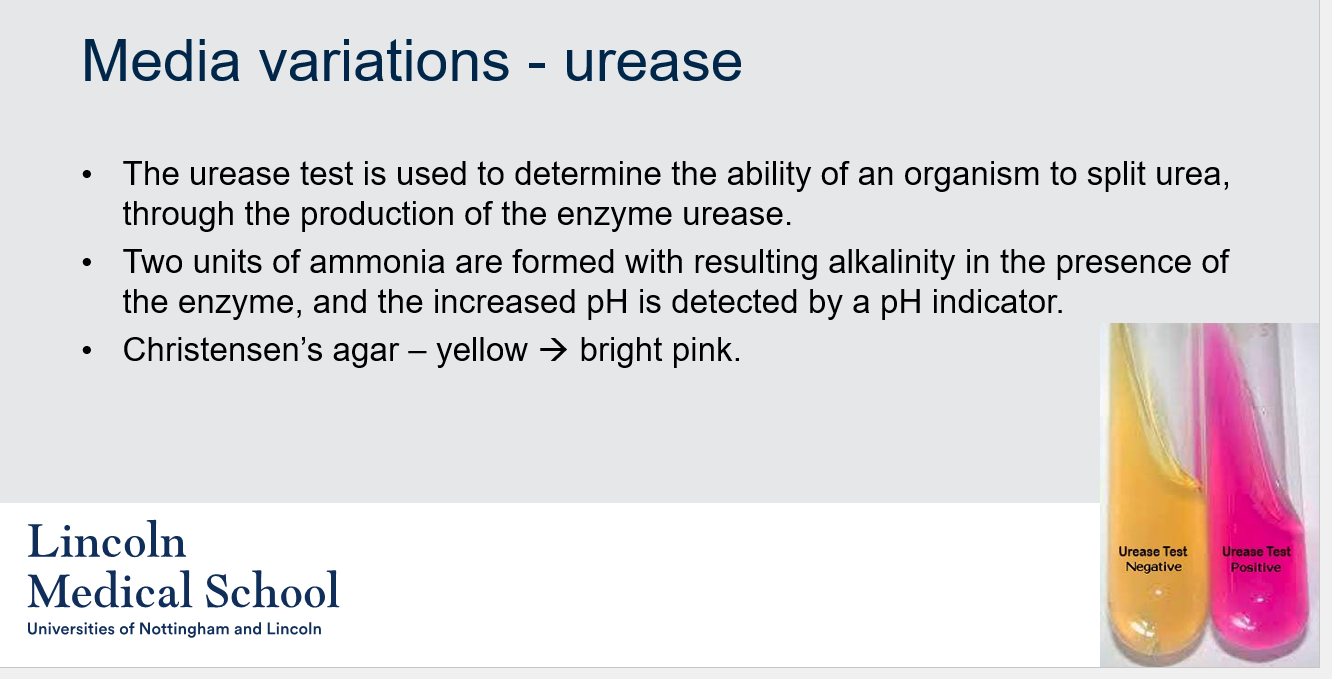
Media variations - urease
1. What is the urease test used for?
2. What happens in the urease test if an organism produces urease?
3. What is the name of the agar used in the urease test?
4. What is the color change that indicates a positive urease test?
1. What is the urease test used for?
2. What happens in the urease test if an organism produces urease?
3. What is the name of the agar used in the urease test?
4. What is the color change that indicates a positive urease test?
1. The urease test is used to determine the ability of an organism to split urea, through the production of the enzyme urease.
2. Two units of ammonia are formed with resulting alkalinity in the presence of the enzyme, and the increased pH is detected by a pH indicator.
3. The name of the agar used in the urease test is Christensen’s agar.
4. The color change that indicates a positive urease test is from yellow to bright pink.
9
New cards

Media variations - urease
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
10
New cards
Chemical reactions
How can bacteria be differentiated based on their behavior during chemical reactions?
How can bacteria be differentiated based on their behavior during chemical reactions?
By observing how bacteria behave during specific chemical reactions it may be possible to differentiate between species. The three commonly used methods are the Latex antibody test, Oxidase test, and Catalase test.
11
New cards
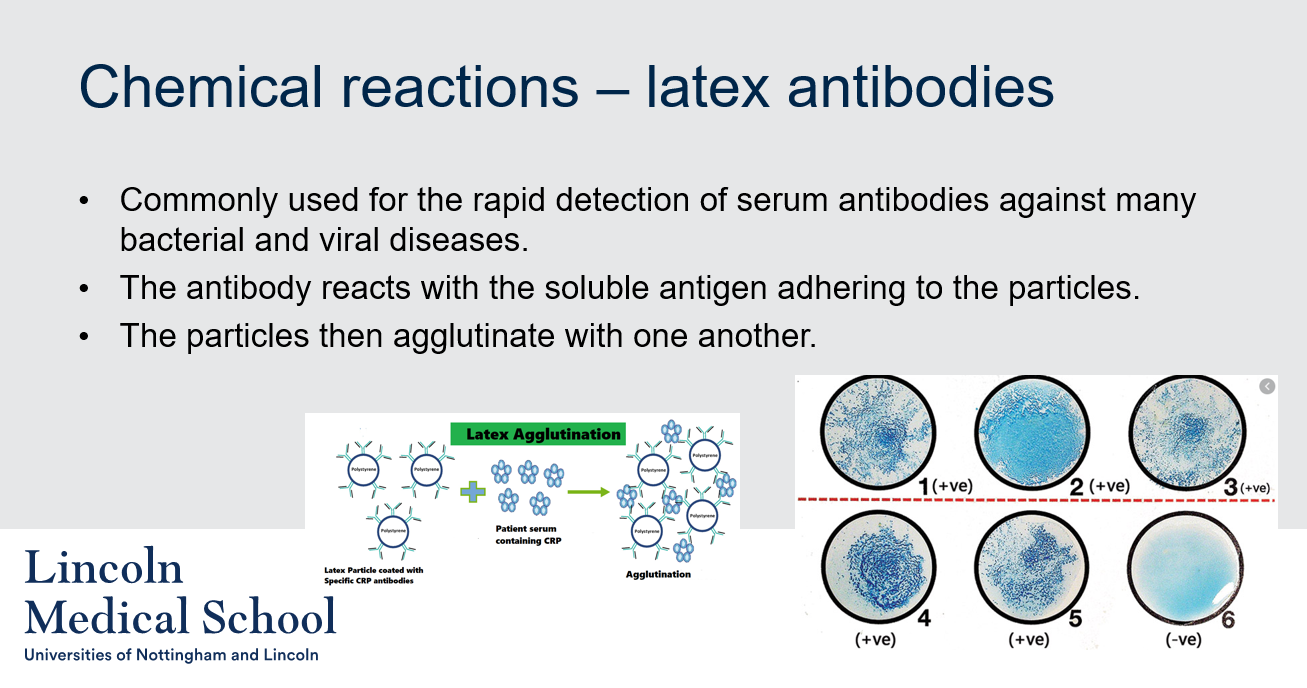
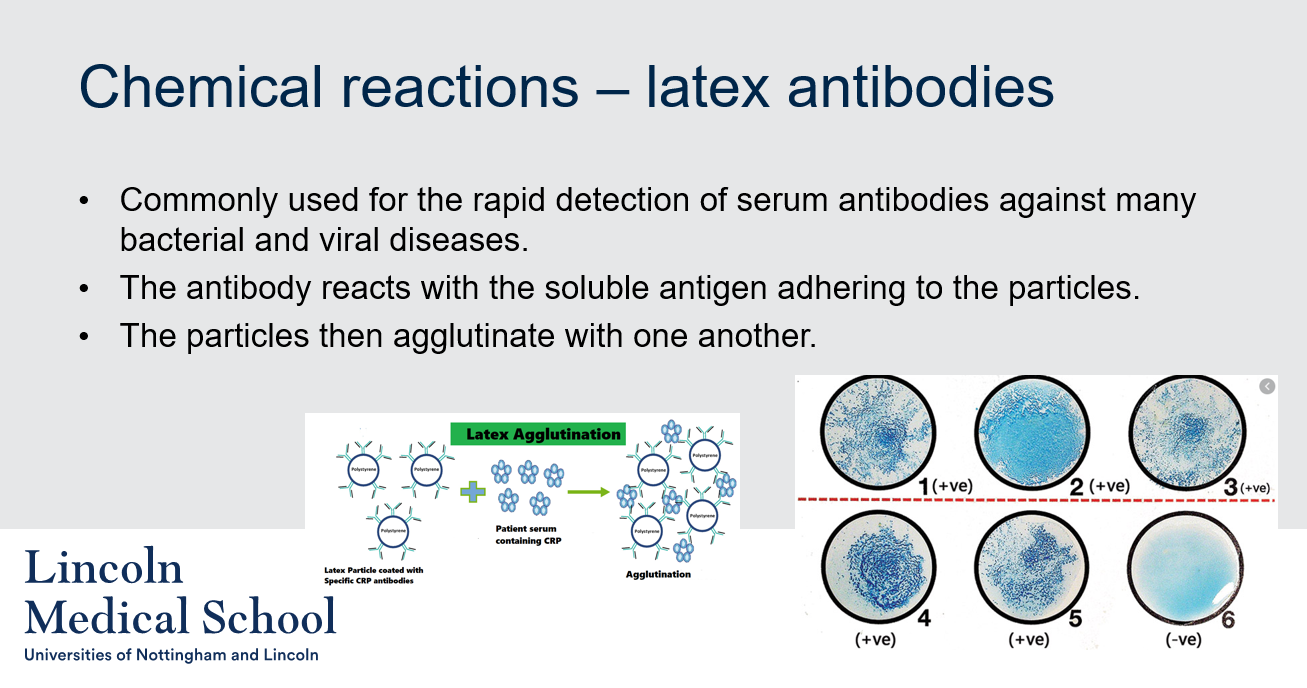
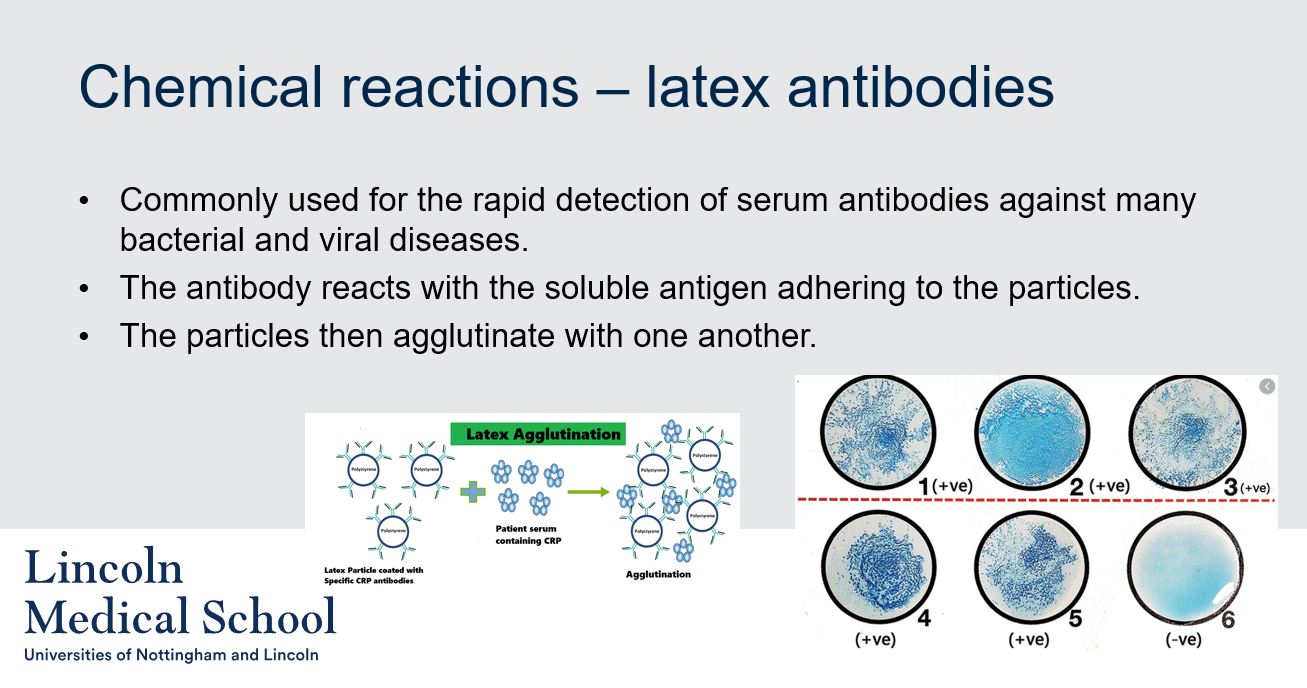
Chemical reactions – latex antibodies
What is the latex antibody test used for in bacterial detection?
What is the latex antibody test used for in bacterial detection?
The latex antibody test is commonly used for the rapid detection of serum antibodies against many bacterial and viral diseases. It involves the reaction of the antibody with the soluble antigen adhering to the particles, which then agglutinate with one another.
12
New cards

Chemical reactions – latex antibodies
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
13
New cards
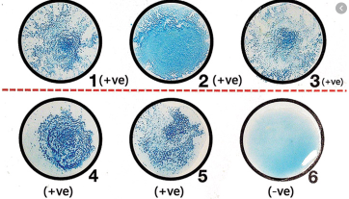
Chemical reactions – latex antibodies
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
14
New cards
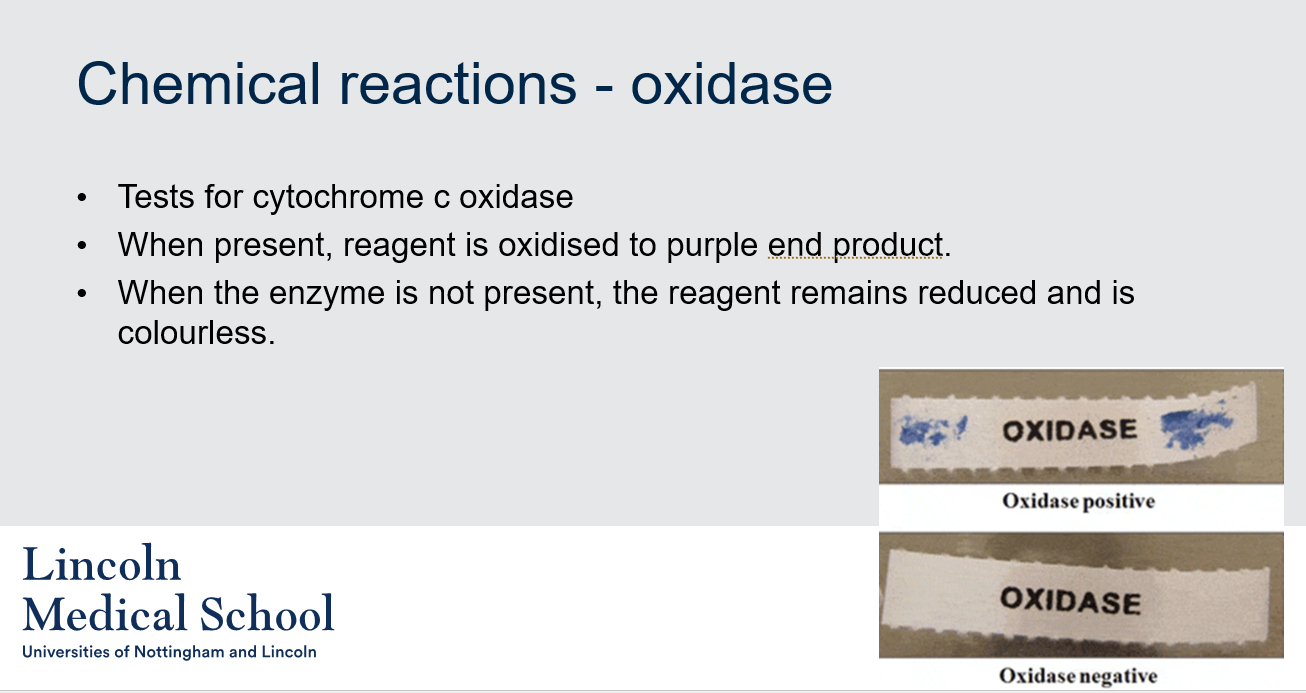
Chemical reactions - oxidase
1. What is an oxidase?
2. What are tests for cytochrome c oxidase?
3. What is the significance of the purple end product in the test for cytochrome c oxidase?
4. Why does the reagent remain colorless in the absence of cytochrome c oxidase?
1. What is an oxidase?
2. What are tests for cytochrome c oxidase?
3. What is the significance of the purple end product in the test for cytochrome c oxidase?
4. Why does the reagent remain colorless in the absence of cytochrome c oxidase?
1. An oxidase is an enzyme that catalyzes an oxidation-reduction reaction, in which oxygen acts as the electron acceptor.
2. Tests for cytochrome c oxidase typically involve adding a reagent that is oxidized to a purple end product in the presence of the enzyme. If the enzyme is not present, the reagent remains reduced and is colorless.
3. The purple end product indicates the presence of cytochrome c oxidase. It is formed when the enzyme oxidizes the reagent.
4. The reagent remains colorless in the absence of cytochrome c oxidase because the enzyme is necessary for its oxidation. Without the enzyme, the reagent remains reduced and does not produce the purple end product.
15
New cards
Chemical reactions - oxidase
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
16
New cards
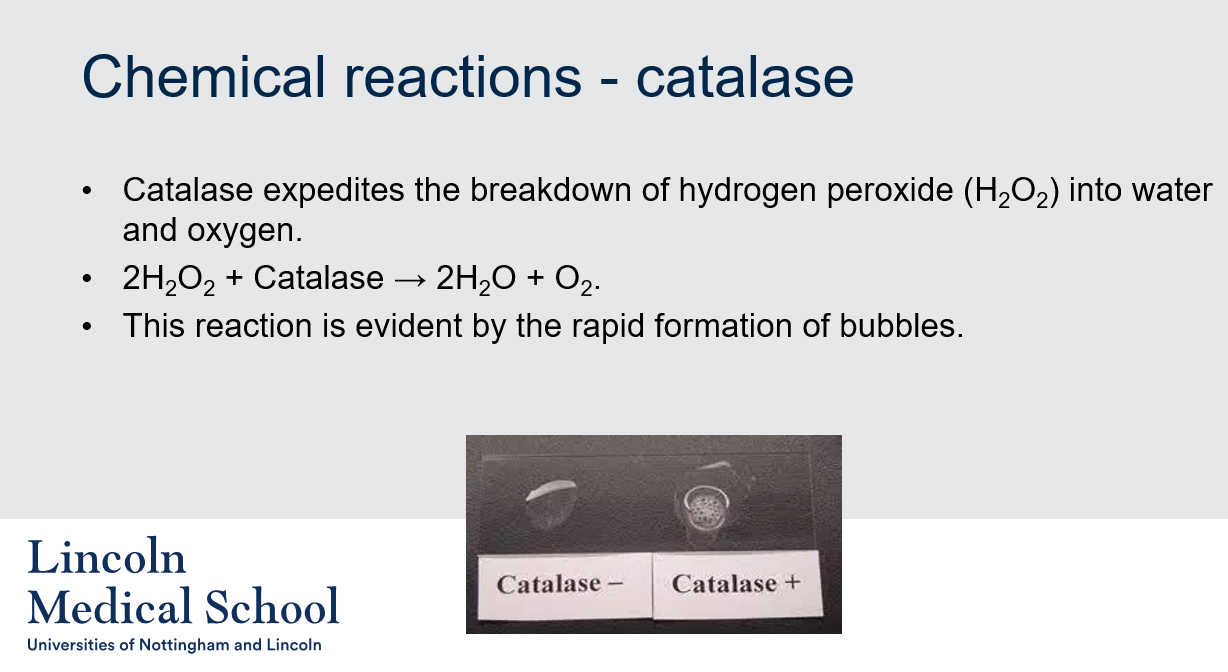
Chemical reactions - catalase
1. What is catalase?
2. What is the chemical reaction catalyzed by catalase?
3. How can you detect the presence of catalase?
4. What causes the formation of bubbles when hydrogen peroxide is added to a sample containing catalase?
1. What is catalase?
2. What is the chemical reaction catalyzed by catalase?
3. How can you detect the presence of catalase?
4. What causes the formation of bubbles when hydrogen peroxide is added to a sample containing catalase?
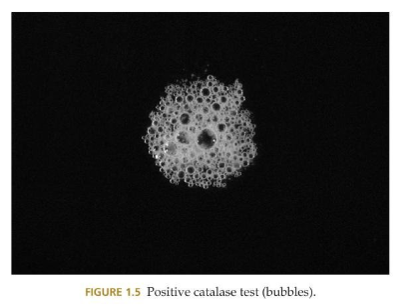
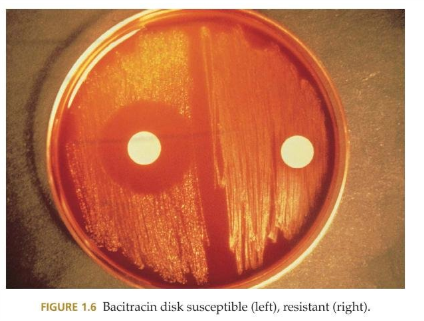
1. Catalase is an enzyme that catalyzes the breakdown of hydrogen peroxide (H2O2) into water and oxygen.
2. The chemical reaction catalyzed by catalase is the breakdown of hydrogen peroxide into water and oxygen: 2H2O2 + Catalase → 2H2O + O2.
3. The presence of catalase can be detected by observing the rapid formation of bubbles when hydrogen peroxide is added to a sample containing the enzyme.
4. The formation of bubbles when hydrogen peroxide is added to a sample containing catalase is caused by the breakdown of hydrogen peroxide into water and oxygen, which produces gas bubbles of oxygen.
17
New cards
Chemical reactions - catalase
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
18
New cards
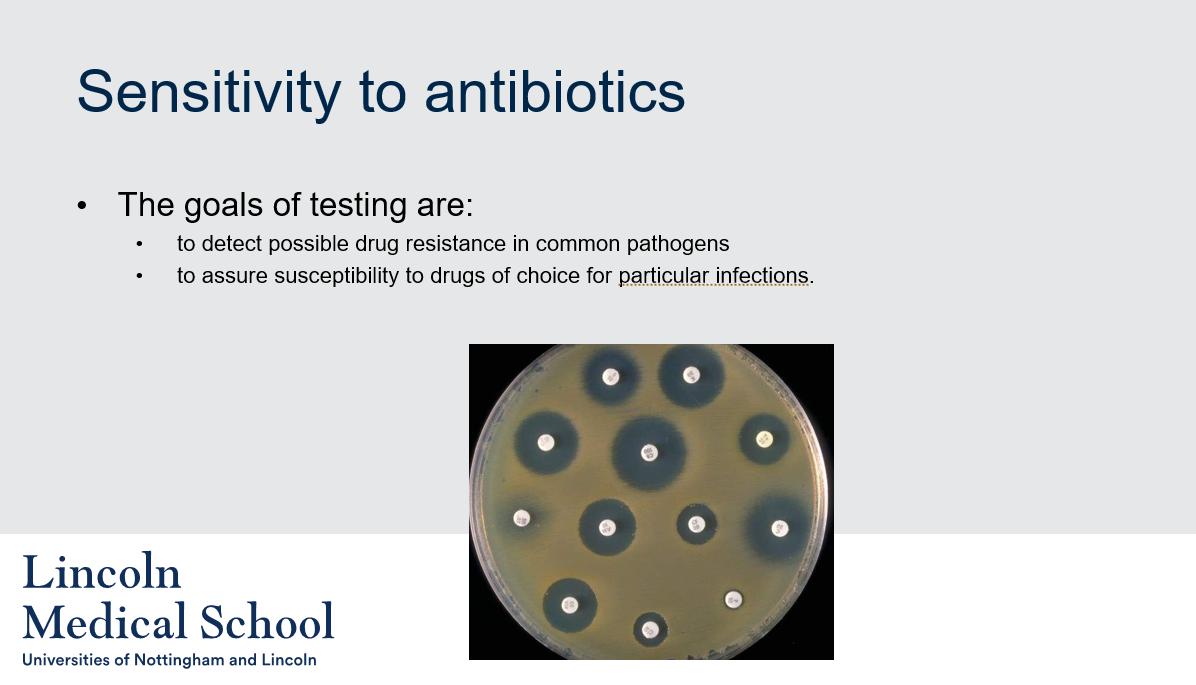
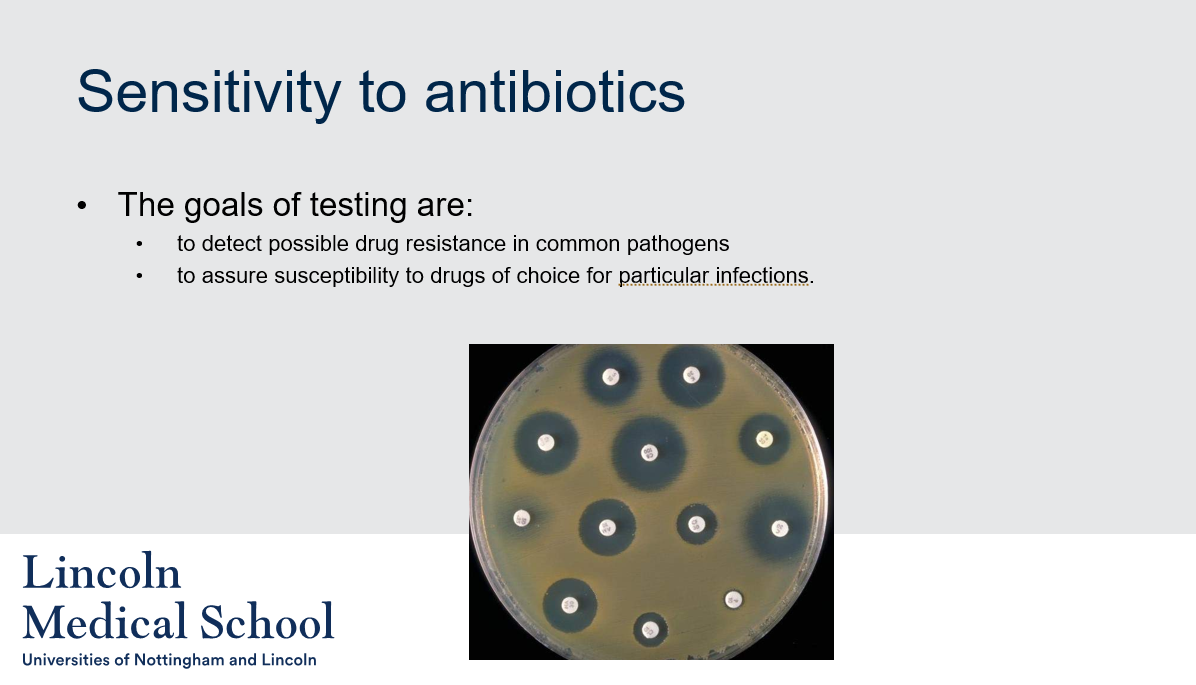
Sensitivity to antibiotics
1. What is antibiotic sensitivity testing?
2. What are the goals of antibiotic sensitivity testing?
1. What is antibiotic sensitivity testing?
2. What are the goals of antibiotic sensitivity testing?
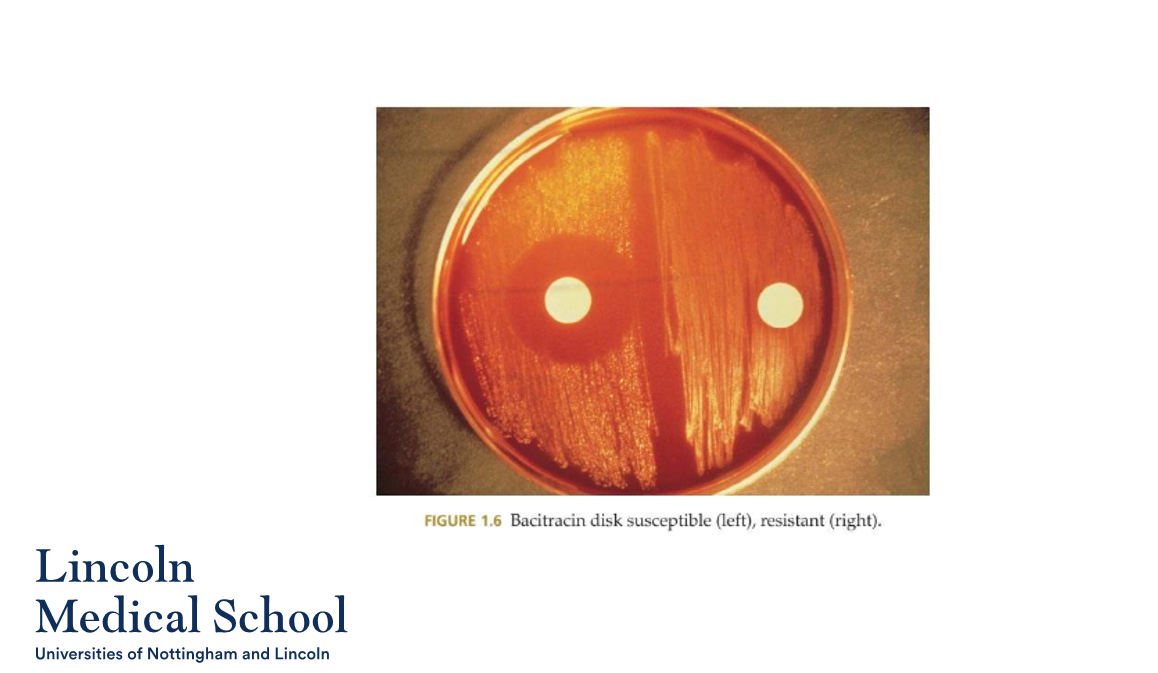
1. Antibiotic sensitivity testing is a laboratory procedure used to determine the susceptibility of bacteria to different antibiotics.
2. The goals of antibiotic sensitivity testing are to detect possible drug resistance in common pathogens and to assure susceptibility to drugs of choice for particular infections.
19
New cards
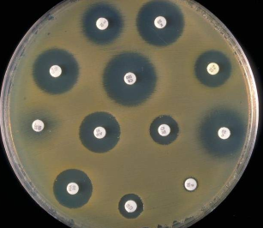
Sensitivity to antibiotics
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
20
New cards
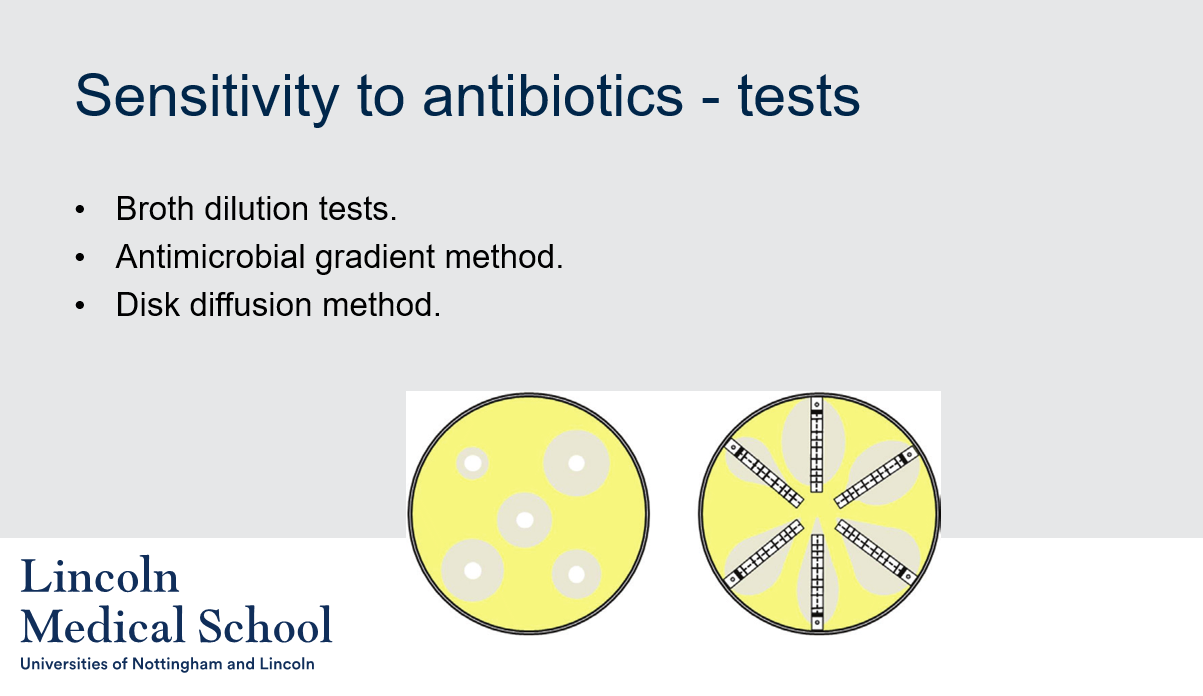
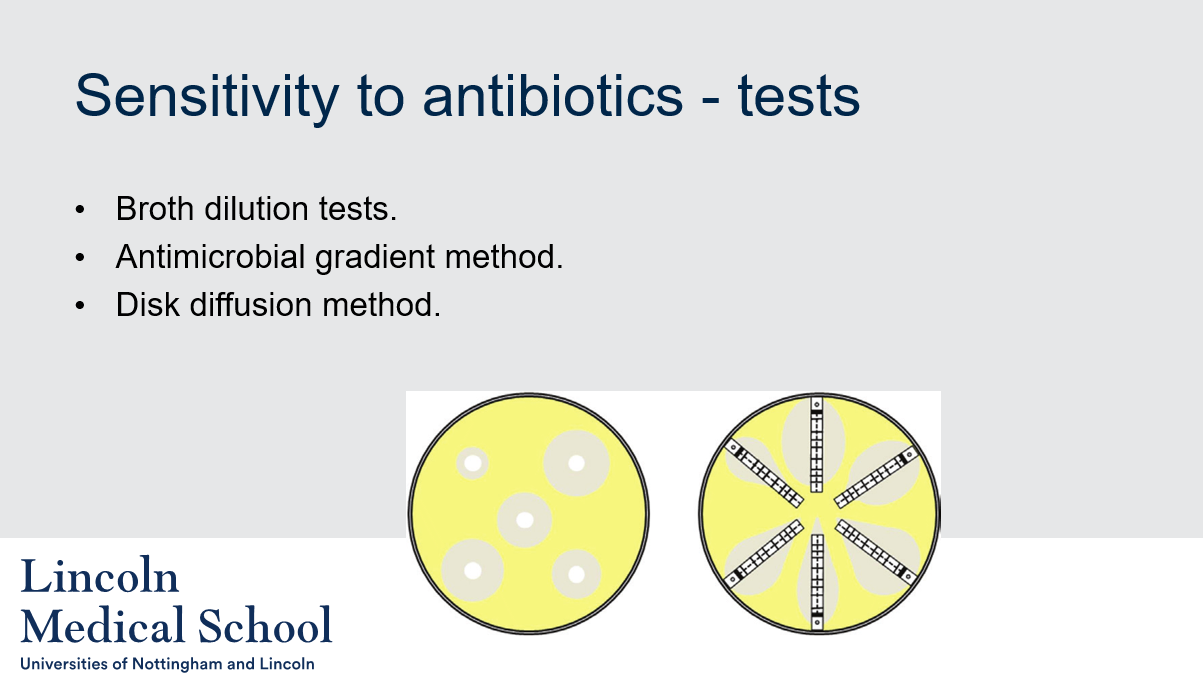
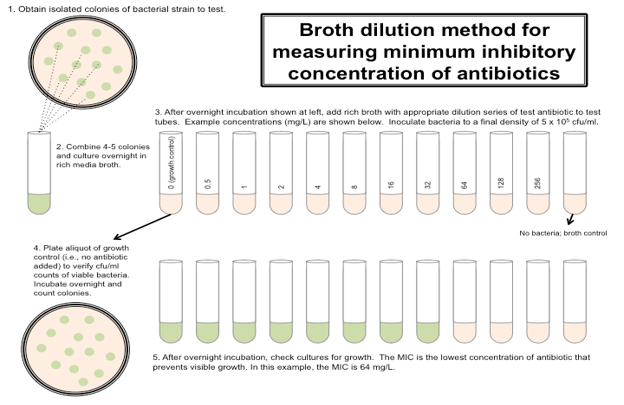
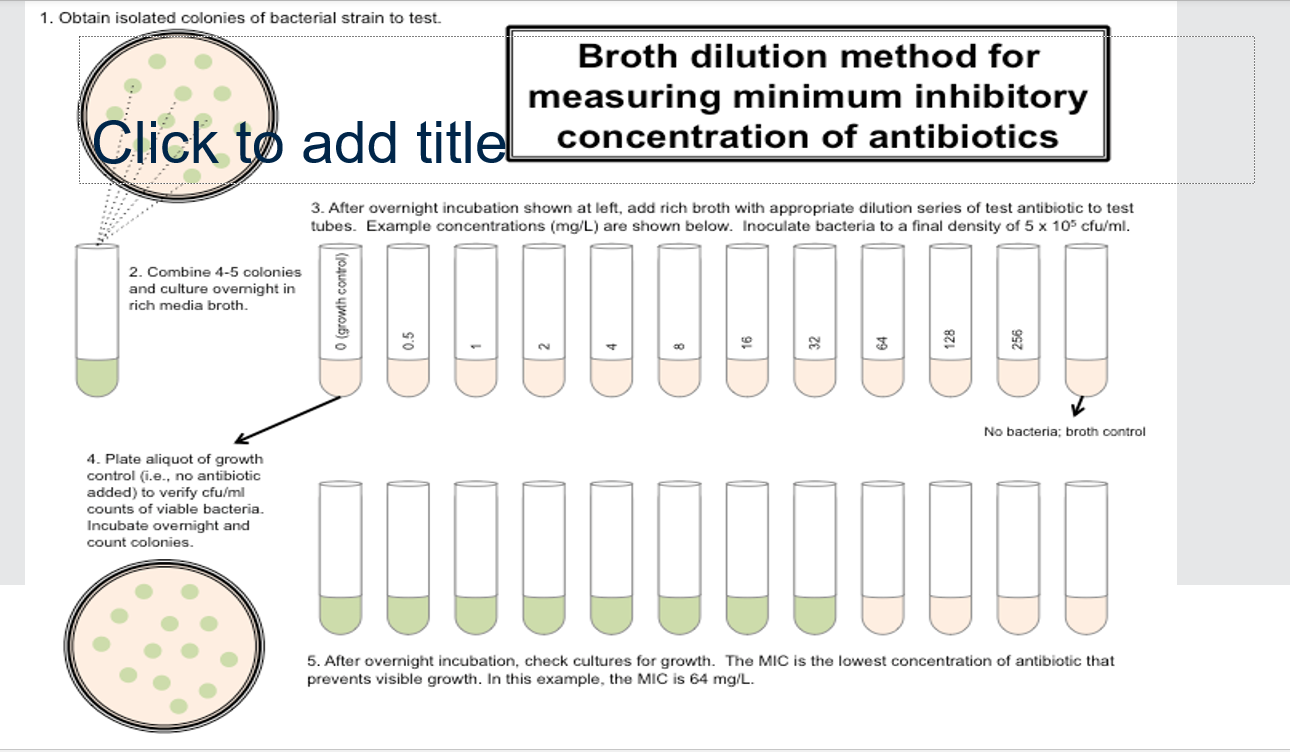
Sensitivity to antibiotics - tests
1. What are some methods used for antibiotic sensitivity testing?
2. What is the broth dilution test?
3. What is the antimicrobial gradient method?
4. What is the disk diffusion method?
1. What are some methods used for antibiotic sensitivity testing?
2. What is the broth dilution test?
3. What is the antimicrobial gradient method?
4. What is the disk diffusion method?
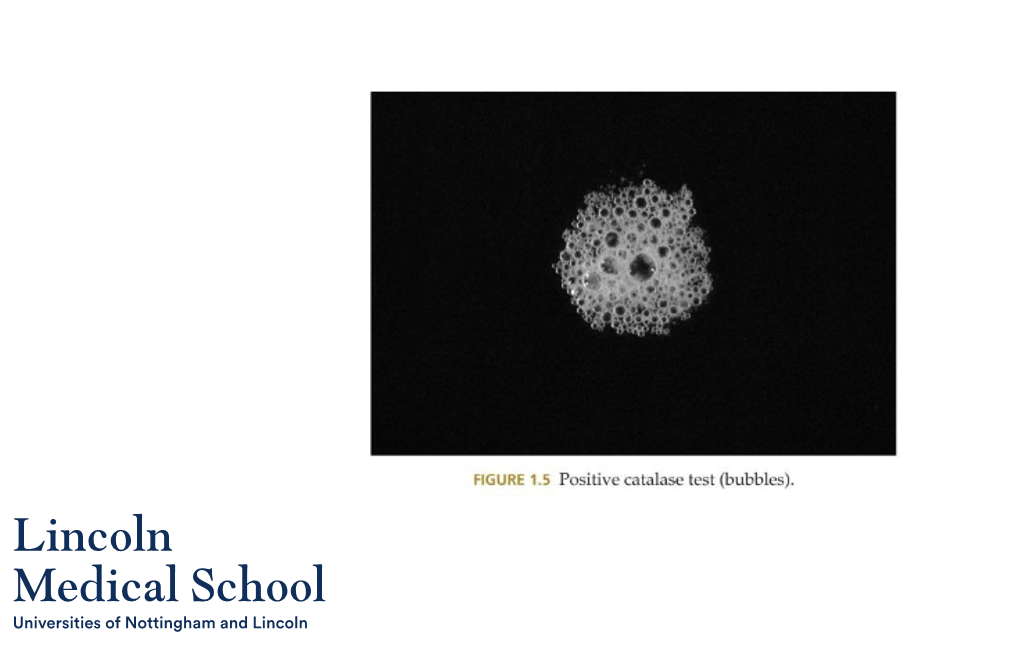
1. Some methods used for antibiotic sensitivity testing include broth dilution tests, antimicrobial gradient method, and disk diffusion method.
2. The broth dilution test is a method used for antibiotic sensitivity testing in which different concentrations of antibiotics are added to bacterial cultures in liquid media. The lowest concentration of antibiotic that prevents visible bacterial growth is the minimum inhibitory concentration (MIC), which is used to determine antibiotic susceptibility.
3. The antimicrobial gradient method is a method used for antibiotic sensitivity testing in which paper strips impregnated with different concentrations of antibiotics are placed on an agar plate that has been inoculated with bacteria. As the antibiotic diffuses into the agar, a gradient of antibiotic concentration is established, and the zone of bacterial growth inhibition is used to determine antibiotic susceptibility.
4. The disk diffusion method is a method used for antibiotic sensitivity testing in which paper disks containing different antibiotics are placed on an agar plate that has been inoculated with bacteria. As the antibiotic diffuses into the agar, a zone of bacterial growth inhibition is formed around the disk, which is used to determine antibiotic susceptibility.
21
New cards
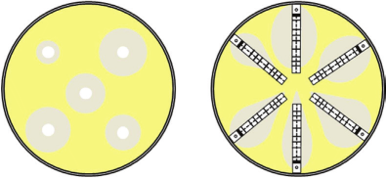
Sensitivity to antibiotics - tests
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
22
New cards
Can you label, describe and explain what this diagram is/shows?
23
New cards
Key terminology
1. What is a pandemic?
2. What is an epidemic?
3. What is an endemic disease?
1. What is a pandemic?
2. What is an epidemic?
3. What is an endemic disease?
1. A pandemic is when an epidemic spreads throughout the world.
2. An epidemic is an outbreak of a disease that attacks many people at the same time and may spread throughout communities.
3. An endemic disease is a disease that exists permanently in a particular region or population.
24
New cards
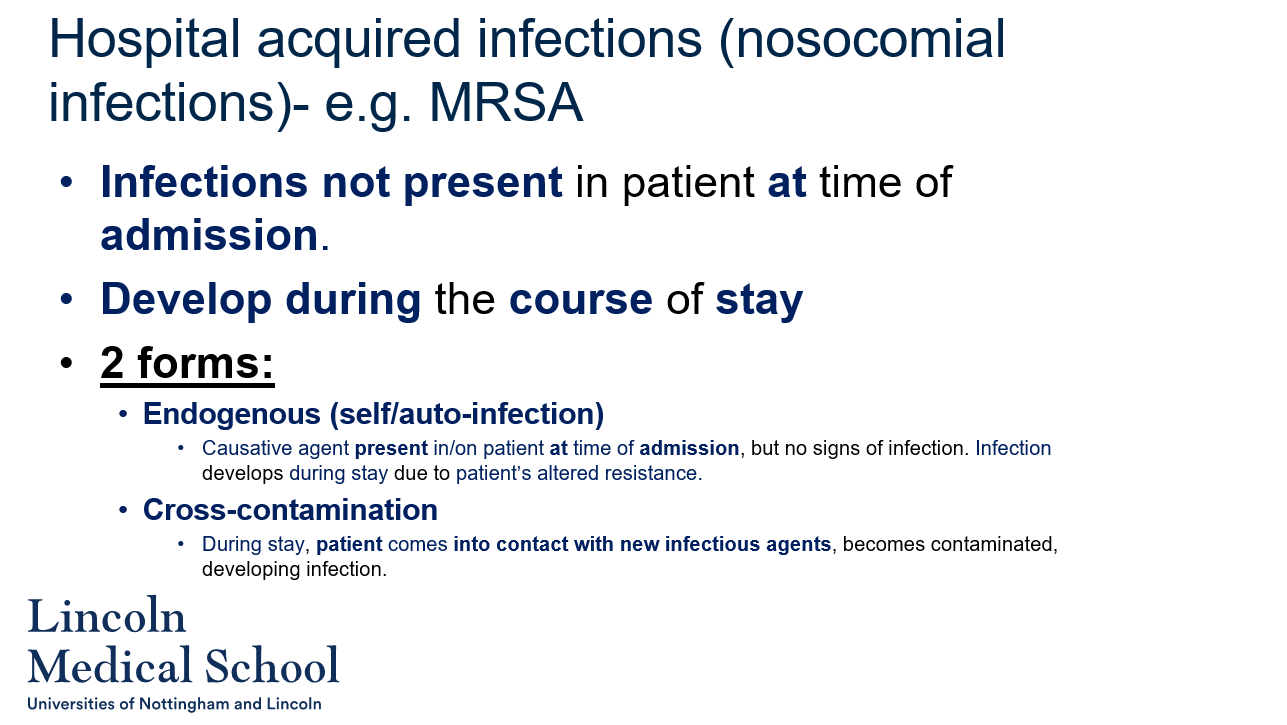
Hospital acquired infections (nosocomial infections)- e.g. MRSA
1. What are hospital-acquired infections?
2. What are the two forms of hospital-acquired infections?
3. What is an endogenous infection?
4. What is cross-contamination infection?
5. What is an example of a hospital-acquired infection?
1. What are hospital-acquired infections?
2. What are the two forms of hospital-acquired infections?
3. What is an endogenous infection?
4. What is cross-contamination infection?
5. What is an example of a hospital-acquired infection?
1. Hospital-acquired infections, also known as nosocomial infections, are infections that are not present in a patient at the time of admission to a healthcare facility, but develop during the course of their stay.
2. The two forms of hospital-acquired infections are endogenous (self/auto) infections and cross-contamination infections.
3. An endogenous infection is a type of hospital-acquired infection in which the causative agent is present in or on the patient at the time of admission, but the patient shows no signs of infection. The infection develops during the patient's stay due to factors that alter their resistance to the pathogen, such as the use of antibiotics or other medications, surgical procedures, or immune system suppression.
4. Cross-contamination infection is a type of hospital-acquired infection in which the patient comes into contact with new infectious agents during their stay in the healthcare facility. This can happen through contact with contaminated medical equipment or surfaces, healthcare workers, or other patients.
5. Methicillin-resistant Staphylococcus aureus (MRSA) is an example of a hospital-acquired infection that can cause serious infections in patients who are already ill or have weakened immune systems. It is often spread through contact with contaminated surfaces or people, and can be difficult to treat with antibiotics.
25
New cards
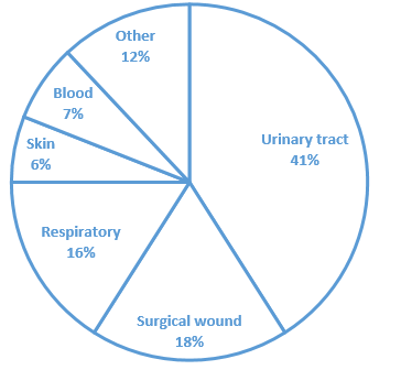
INCIDENCE of hospital acquired infections (SITE)
Can you label, describe and explain what this diagram is/shows?
Can you label, describe and explain what this diagram is/shows?
26
New cards
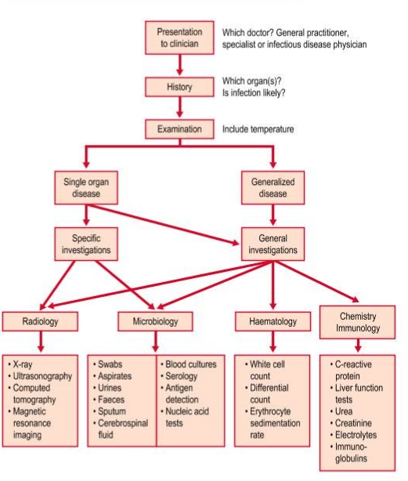
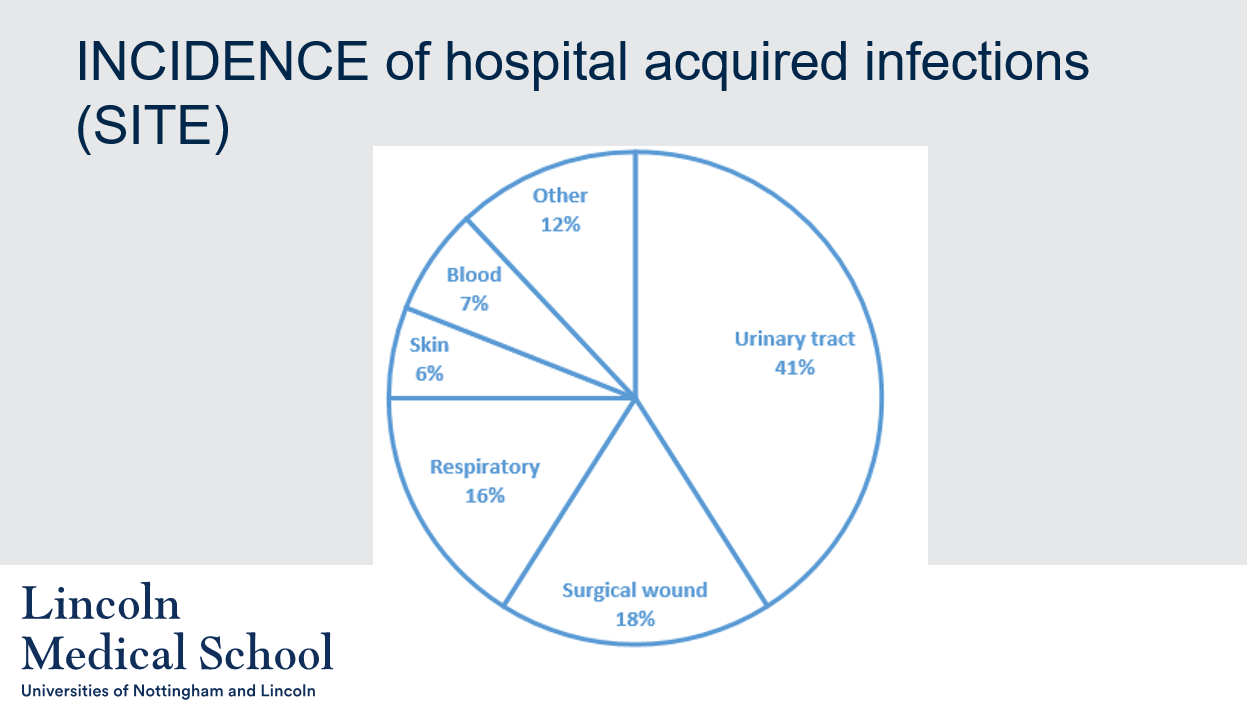
Can you label, describe and explain what this diagram is/shows?
27
New cards
Can you label, describe and explain what this diagram is/shows?
28
New cards
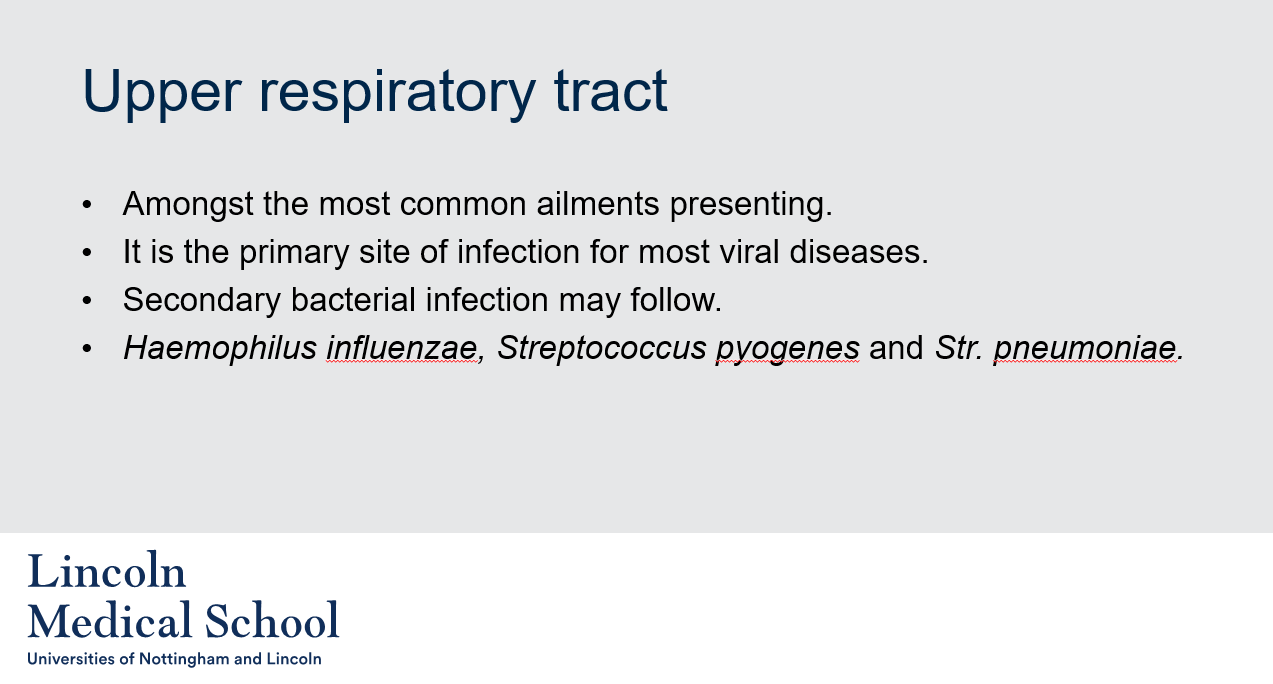
Upper respiratory tract
1. What is the upper respiratory tract?
2. Why are upper respiratory tract infections common?
3. What is a secondary bacterial infection?
1. What is the upper respiratory tract?
2. Why are upper respiratory tract infections common?
3. What is a secondary bacterial infection?
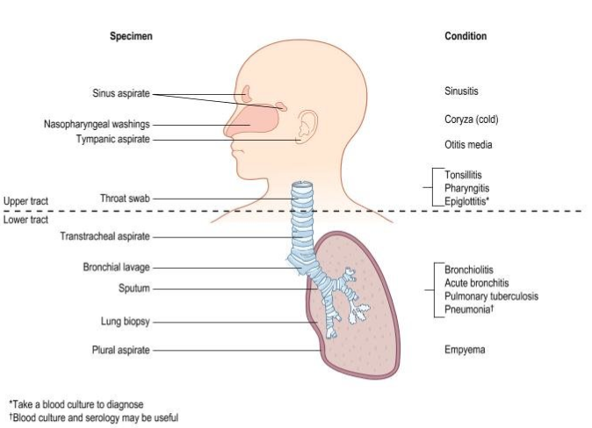
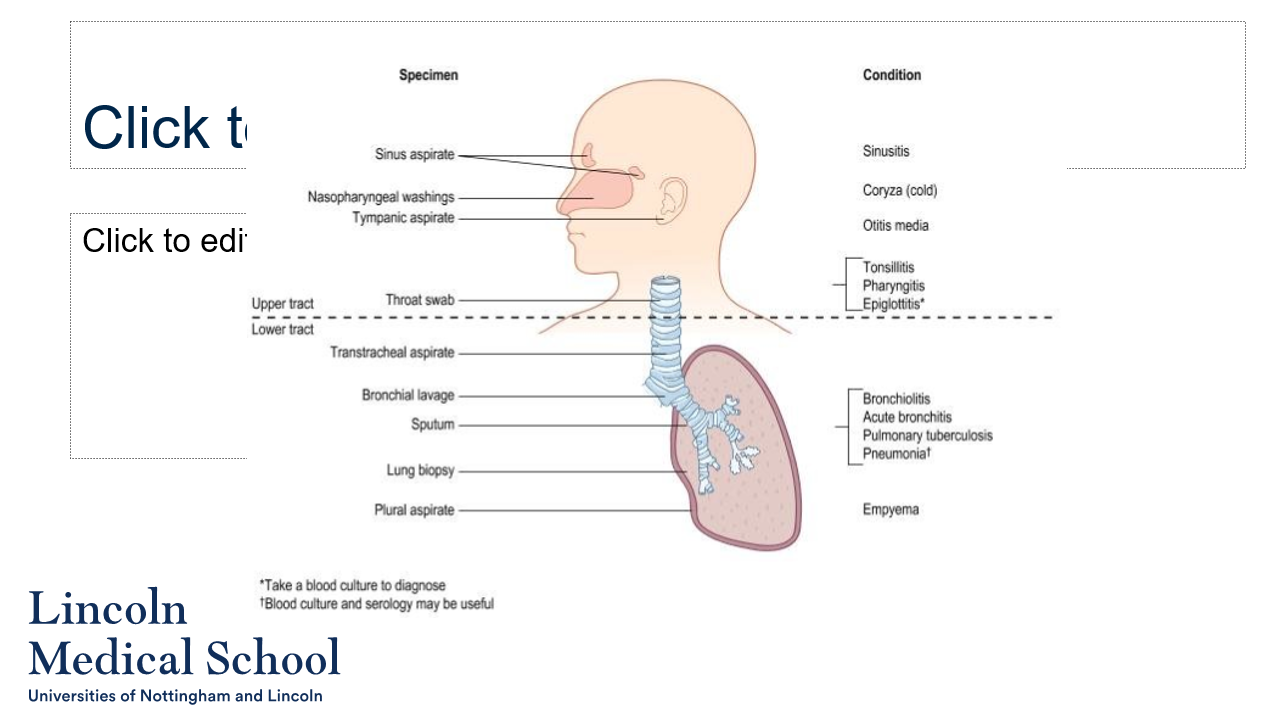
1. The upper respiratory tract refers to the parts of the respiratory system that are located above the trachea, including the nose, sinuses, pharynx, and larynx.
2. Upper respiratory tract infections are among the most common ailments that present in the upper respiratory tract. Upper respiratory tract infections are common because the upper respiratory tract is the primary site of infection for most viral diseases.
3. A secondary bacterial infection is an infection that occurs after a primary infection, usually caused by a virus, has weakened the body's immune system and made it more susceptible to bacterial invasion. In the case of upper respiratory tract infections, bacterial infections can follow viral infections and may be caused by bacteria such as Haemophilus influenzae, Streptococcus pyogenes, and Streptococcus pneumoniae.
29
New cards
Sore throat
1. What is bacterial acute tonsillitis or pharyngitis?
2. Why is it important to make a definitive diagnosis of streptococcal pharyngitis?
3. What is penicillin?
4. Why is there less need to make a virological diagnosis for sore throat?
5. What other bacteria may need to be tested for in cases of sore throat?
1. What is bacterial acute tonsillitis or pharyngitis?
2. Why is it important to make a definitive diagnosis of streptococcal pharyngitis?
3. What is penicillin?
4. Why is there less need to make a virological diagnosis for sore throat?
5. What other bacteria may need to be tested for in cases of sore throat?
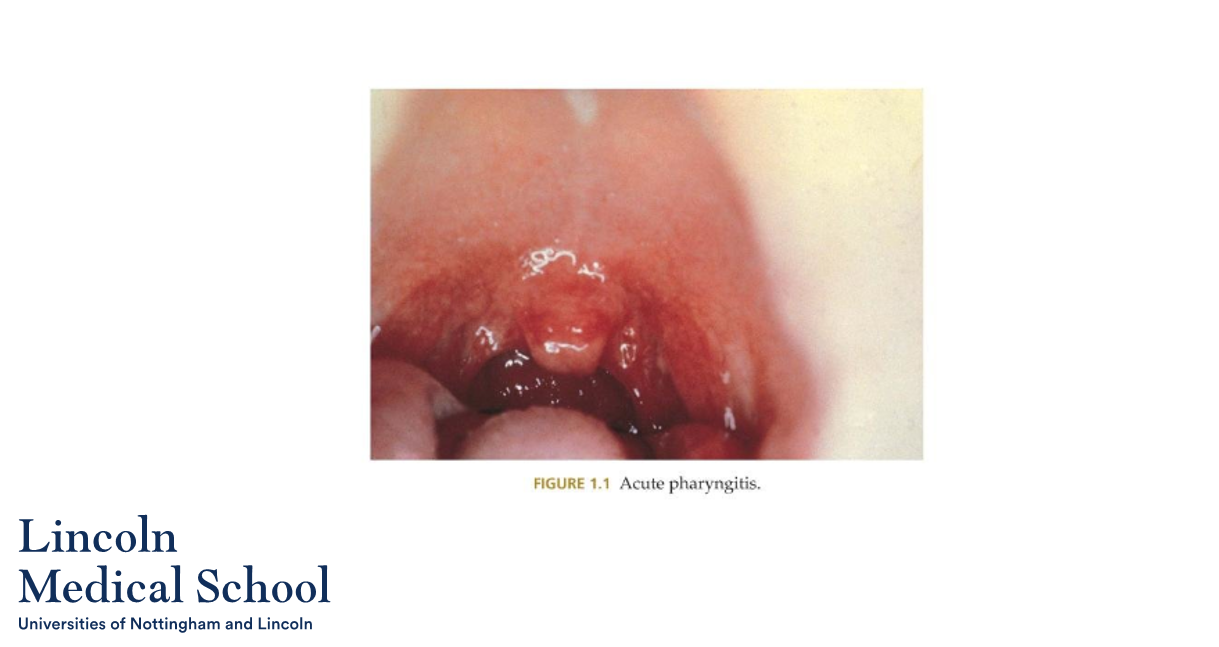
1. Bacterial acute tonsillitis or pharyngitis is a bacterial infection of the tonsils or pharynx (back of the throat) that can cause symptoms such as sore throat, difficulty swallowing, fever, and swollen lymph nodes. Streptococcus pyogenes is a common bacterial cause of acute tonsillitis or pharyngitis.
2. It is important to make a definitive diagnosis of streptococcal pharyngitis because this bacterial infection can lead to serious complications if left untreated, such as rheumatic fever, kidney disease, and heart damage. In addition, antibiotic therapy is required to treat streptococcal pharyngitis and prevent the spread of infection.
3. Penicillin is an antibiotic medication that is commonly used to treat bacterial infections such as streptococcal pharyngitis. It works by killing the bacteria or preventing their growth.
4. There is less need to make a virological diagnosis for sore throat because most cases of sore throat are caused by viral infections, and there are limited treatment options for viral infections. Symptomatic relief is often the main approach for managing viral sore throat, with pain relievers and rest being recommended.
5. Other bacteria that may need to be tested for in cases of sore throat as testing for these bacteria can help guide appropriate antibiotic therapy and prevent the spread of infection.
30
New cards
Common cold
1. How often do people typically experience clinical infections of the common cold?
2. Can bacterial superinfection occur with the common cold?
3. What other conditions can occur with the common cold or develop in more susceptible individuals?
1. How often do people typically experience clinical infections of the common cold?
2. Can bacterial superinfection occur with the common cold?
3. What other conditions can occur with the common cold or develop in more susceptible individuals?
1. People typically experience three or four clinical infections of the common cold each year.
2. Yes, bacterial superinfection can occur with the common cold. The weakened immune system and damaged respiratory tract caused by the viral infection can create an environment in which bacteria can thrive and cause a secondary bacterial infection.
3. Pharyngitis (sore throat) can occur with the common cold, and occasionally tracheobronchitis (inflammation of the trachea and bronchi) may develop in more susceptible individuals. These conditions can cause additional symptoms such as coughing, fever, and difficulty breathing.
31
New cards
Sinusitis
1. What are some possible complications of sinusitis?
2. Why is obtaining adequate material for microbiology difficult in sinusitis cases?
3. What types of bacteria are often found in sinus washings of adults with recurrent or chronic sinusitis?
1. What are some possible complications of sinusitis?
2. Why is obtaining adequate material for microbiology difficult in sinusitis cases?
3. What types of bacteria are often found in sinus washings of adults with recurrent or chronic sinusitis?
1. Direct extension into the frontal and maxillary sinuses in adults and into the middle ear in children is not uncommon with sinusitis. This can cause additional symptoms and complications such as ear infections, facial pain, and difficulty breathing.
2. Obtaining adequate material for microbiology in sinusitis cases is difficult because the sinuses are located deep in the skull and are difficult to access. This requires the expertise of ear, nose, and throat (ENT) specialists to properly collect and analyze samples.
3. Anaerobes such as peptostreptococci or bacteroides are often found in sinus washings of adults with recurrent or chronic sinusitis.
32
New cards
Acute bronchitis
1. What are some common causes of acute bronchitis?
2. Why is sputum examination valuable in cases of acute bronchitis?
1. What are some common causes of acute bronchitis?
2. Why is sputum examination valuable in cases of acute bronchitis?
1. Acute bronchitis is commonly caused by pneumococci, non-encapsulated haemophili, or both. It can also follow a viral infection.
2. Sputum examination is valuable in cases of acute bronchitis because the causative bacteria may show variable antimicrobial resistance, and appropriate therapy is essential. By analyzing the sputum, the causative bacteria can be identified, and the appropriate antibiotics can be prescribed to effectively treat the infection.
33
New cards
Acute pneumonias
1. Is it possible to distinguish between different types of acute pneumonias?
2. Why is it important to distinguish between different types of acute pneumonias?
3. What diagnostic tools can be used to diagnose acute pneumonias?
1. Is it possible to distinguish between different types of acute pneumonias?
2. Why is it important to distinguish between different types of acute pneumonias?
3. What diagnostic tools can be used to diagnose acute pneumonias?
1. Yes, it is possible to distinguish between different types of acute pneumonias, including lobar pneumonia, bronchopneumonia, and 'atypical' pneumonias.
2. It is important to distinguish between different types of acute pneumonias because this can guide primary treatment. Different types of pneumonia may respond better to different antibiotics or treatments, so accurately identifying the type of pneumonia can help ensure effective treatment.
3. Sputum examination, blood cultures, and antigen detection can all be used to diagnose acute pneumonias. By analyzing these samples, the causative bacteria or virus can be identified, and appropriate treatment can be prescribed.
34
New cards
GI infections
1. What is a common complaint associated with GI infections?
2. Are microbial causes important reasons for acute gastrointestinal upset in healthy individuals?
3. Is it necessary to search for all causes of GI infections?
4. Can consuming fugu fish cause gastrointestinal infections?
1. What is a common complaint associated with GI infections?
2. Are microbial causes important reasons for acute gastrointestinal upset in healthy individuals?
3. Is it necessary to search for all causes of GI infections?
4. Can consuming fugu fish cause gastrointestinal infections?
1. Acute diarrhea with or without vomiting.
2. Yes, microbial causes are the most important reasons for acute gastrointestinal upset in an otherwise healthy individual.
3. Searching for all causes of GI infections involves extensive and expensive laboratory effort, and is often considered unnecessary for a condition which is usually self-limiting and relatively harmless.
4. Yes, fugu (also known as pufferfish) can cause gastrointestinal infections if it is not prepared properly.
35
New cards
Meningitis
1. What is meningitis?
2. What are common tests used to diagnose meningitis?
3. How is acute bacterial meningitis treated?
4. How is viral meningitis treated?
1. What is meningitis?
2. What are common tests used to diagnose meningitis?
3. How is acute bacterial meningitis treated?
4. How is viral meningitis treated?
1. Meningitis is an inflammation of the membranes that surround the brain and spinal cord, known as the meninges. It can be caused by either viral or bacterial infections.
2. Common tests used to diagnose meningitis include blood cultures, imaging (such as a CT or MRI scan), and a lumbar puncture (also known as a spinal tap). PCR amplification can also be used to detect the presence of viral or bacterial DNA.
3. Acute bacterial meningitis must be treated immediately with intravenous antibiotics and sometimes corticosteroids. In some cases, a sinus drain may also be necessary to remove infected material.
4. Viral meningitis typically requires bed rest, fluids, and possibly corticosteroids to help reduce inflammation and relieve symptoms. Unlike bacterial meningitis, antiviral medications are not usually effective in treating viral meningitis.
36
New cards
Genital tract infections
1. What are some common genital tract infections in males?
2. What are some common genital tract infections that cause genital ulcers in both males and females?
3. What are some common genital tract infections in females?
1. What are some common genital tract infections in males?
2. What are some common genital tract infections that cause genital ulcers in both males and females?
3. What are some common genital tract infections in females?
1. Acute urethritis is a common genital tract infection in males. It is usually caused by a sexually transmitted infection (STI), such as Chlamydia, Gonorrhea, or Mycoplasma genitalium.
2. Genital ulcers can be caused by a number of infections, including Herpes Simplex Virus (HSV), Syphilis, and Chancroid.
3. Common genital tract infections in females include vaginitis (inflammation of the vagina), thrush (an overgrowth of the fungus Candida), Human Papillomavirus (HPV) infections (which can cause genital warts and cervical cancer), and cervical cancer (caused by the Human Papillomavirus).
37
New cards
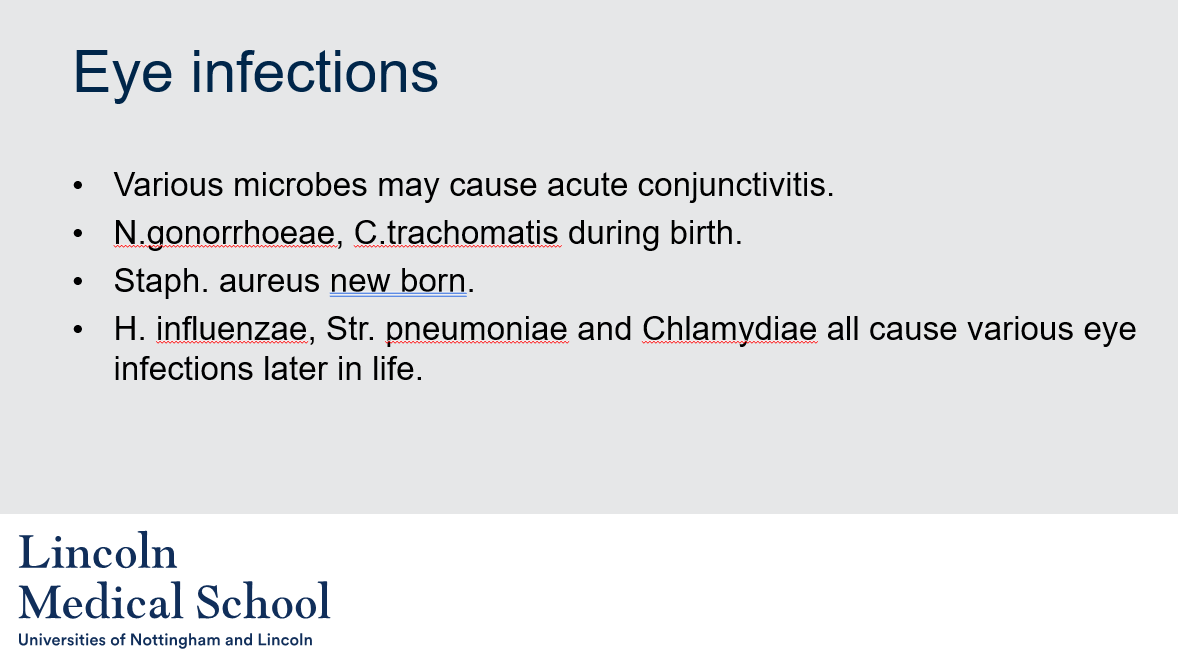
Eye infections
1. What are some microbes that can cause acute conjunctivitis?
2. What are some microbes that can cause eye infections during birth?
3. What microbe can cause eye infections in newborns?
4. What are some microbes that can cause various eye infections later in life?
1. What are some microbes that can cause acute conjunctivitis?
2. What are some microbes that can cause eye infections during birth?
3. What microbe can cause eye infections in newborns?
4. What are some microbes that can cause various eye infections later in life?
1. Various microbes can cause acute conjunctivitis, including viruses (such as Adenovirus), bacteria (such as Streptococcus pneumoniae or Haemophilus influenzae), and fungi.
2. N. gonorrhoeae and C. trachomatis are two microbes that can cause eye infections during birth.
3. Staphylococcus aureus is a microbe that can cause eye infections in newborns.
4. Haemophilus influenzae, Streptococcus pneumoniae, and Chlamydia are some of the microbes that can cause various eye infections later in life.
38
New cards
Patient history
6 year-old male who had been in good health with no significant medical problems.
In late September he presented to his GP with a complaint of sore throat, fever, headache and swollen glands in his neck for the past 36hr.
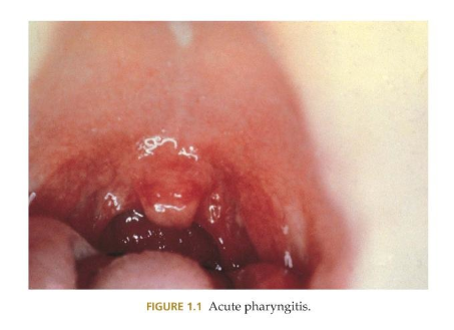
On examination, he had a fever of 38°C (100.4°F), a red posterior pharynx, yellowish exudate on his tonsils, and multiple, enlarged, tender cervical lymph nodes. There were no other pertinent symptoms.
1. What was the differential diagnosis for this patient?
2. What are the major infectious causes of pharyngitis in an immunocompetent host?
3. What are some bacterial causes of pharyngitis?
4. What are some viral causes of pharyngitis?
5. What tests were performed to diagnose the patient's condition?
6. What is the treatment for Streptococcus pyogenes?
7. What is the prevention for Streptococcus pyogenes?
6 year-old male who had been in good health with no significant medical problems.
In late September he presented to his GP with a complaint of sore throat, fever, headache and swollen glands in his neck for the past 36hr.
On examination, he had a fever of 38°C (100.4°F), a red posterior pharynx, yellowish exudate on his tonsils, and multiple, enlarged, tender cervical lymph nodes. There were no other pertinent symptoms.
1. What was the differential diagnosis for this patient?
2. What are the major infectious causes of pharyngitis in an immunocompetent host?
3. What are some bacterial causes of pharyngitis?
4. What are some viral causes of pharyngitis?
5. What tests were performed to diagnose the patient's condition?
6. What is the treatment for Streptococcus pyogenes?
7. What is the prevention for Streptococcus pyogenes?
1. The differential diagnosis for this patient was acute pharyngitis, which is the painful inflammation of the pharynx and surrounding lymphoid tissues.
2. The major infectious causes of pharyngitis in an immunocompetent host are bacterial and viral. Mycobacteria, fungi, and parasites do not cause acute pharyngitis in a normal host.
3. Some bacterial causes of pharyngitis include Arcanobacterium haemolyticum, Corynebacterium diphtheria, Mycoplasma pneumoniae, Neisseria gonorrhoeae, and Streptococcus pyogenes.
4. Some viral causes of pharyngitis include Adenovirus and Epstein-Barr virus.
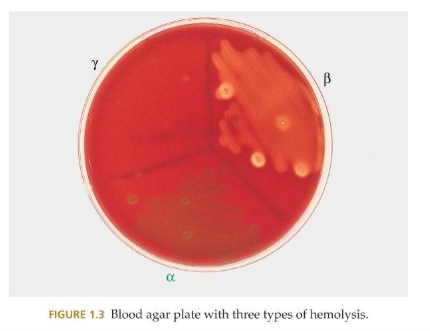
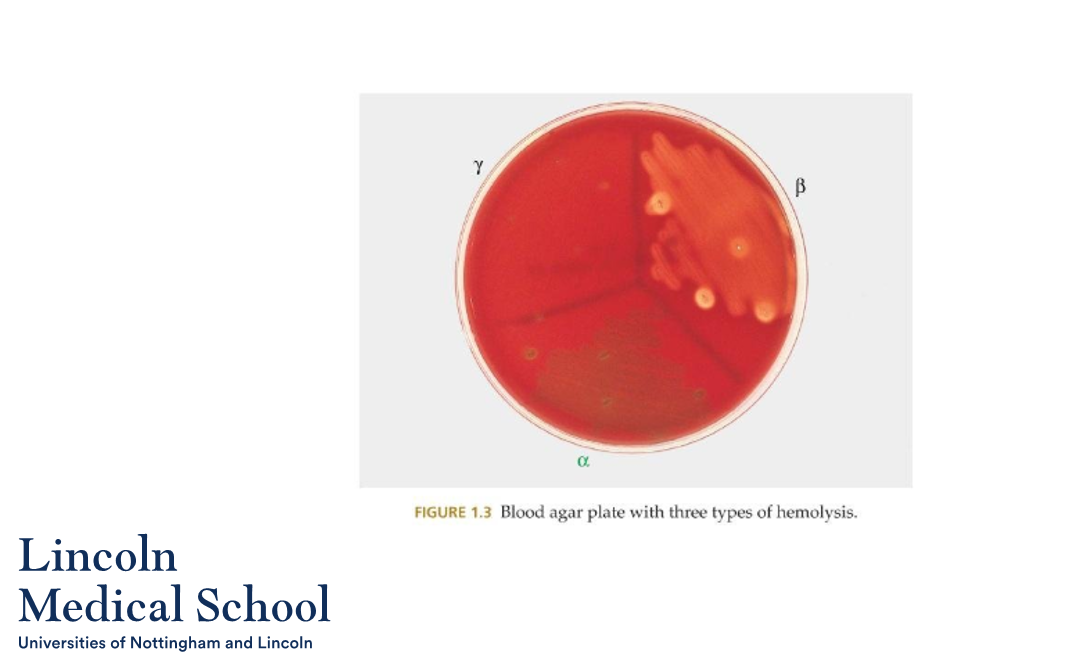
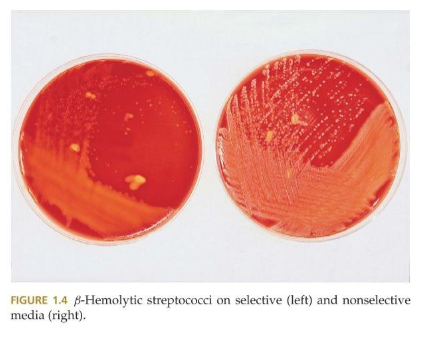
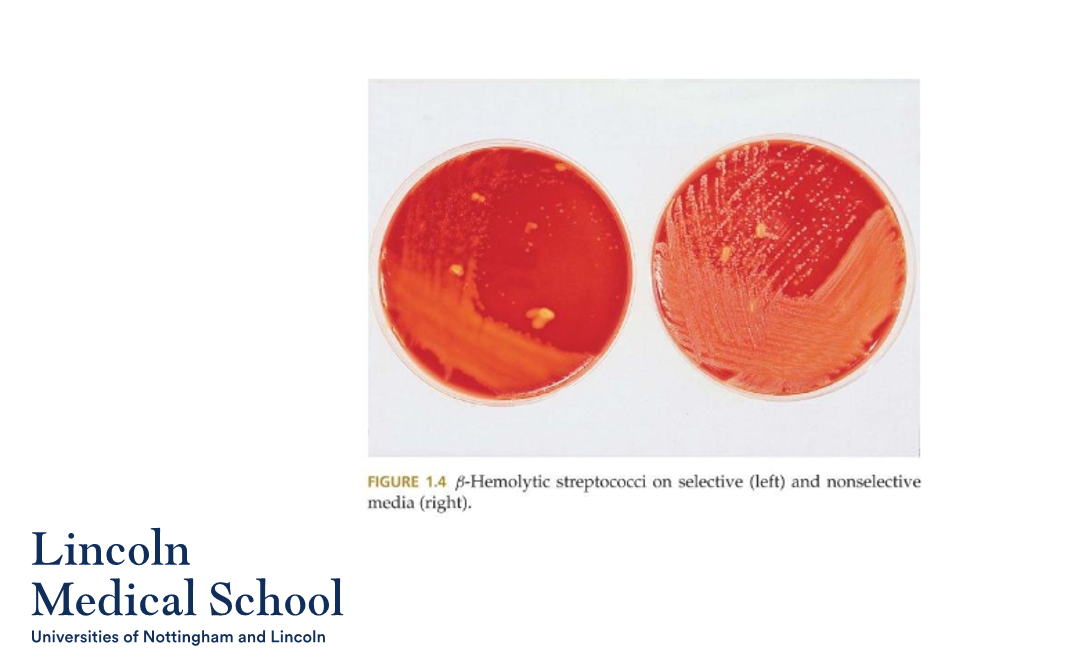
5. Given the age of this patient, the absence of travel, and the lack of suspicion of child abuse the patient underwent a rapid strep test and a throat culture. The results showed β-Hemolysis (complete lysis and destruction of the red blood cells resulting in a distinct clear zone around the colony) , a negative catalase test, and a positive Gram stain, indicating the presence of Streptococcus pyogenes.
6. Streptococcus pyogenes can be effectively treated with penicillin (amoxicillin) or erythromycin for those with an allergy.
7. It is important not only to relieve symptoms but also prevent transmission to others. Streptococcus pyogenes has 80 serotypes of M protein, so reinfection is common. There is possible rapid molecular testing available with improving technology.
39
New cards
Can you label, describe and explain what this diagram is/shows?
40
New cards
Can you label, describe and explain what this diagram is/shows?
41
New cards
Can you label, describe and explain what this diagram is/shows?
42
New cards
Can you label, describe and explain what this diagram is/shows?
43
New cards
Can you label, describe and explain what this diagram is/shows?