ISAP WK 5 - How is Blood Circulation Regulated?
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
What are the 5 functions of the circulatory system?
carries blood from the heart to tissues and back
exchange nutrients, waste products and gases with tissues
transports substances such as hormones and enzymes
helps to regulate blood pressure within a normal range
directs blood flow to the tissues
Describe the structure of blood vessels from lumen to outer wall.
Tunica interna, tunica media, tunica externa
Tunica intima
inner-most layer, consists of 4 layers: endothelium (simple squamous), basement membrane, lamina propria (connective tissue layer), internal elastic membrane consisting of fenestrated layer of elastic fibres
What separates the tunica intima from tunica media?
the internal elastic membrane
Tunica media
the middle layer, consists of smooth muscle cells that are arranged circularly around the blood vessel. Only arteries have an external elastic membrane within the tunica media layer.
What is the purpose of the internal and external elastic membrane?
Present in arteries which helps them handle the high pressure via expanding and recoiling. They provide structural support and elasticity, allowing arteries to accommodate changes in blood pressure.
Tunica externa
outermost layer. composed of connective tissue that ranged from dense (near tunica media) to loose connective tissue that merges with the surrounding connective tissue
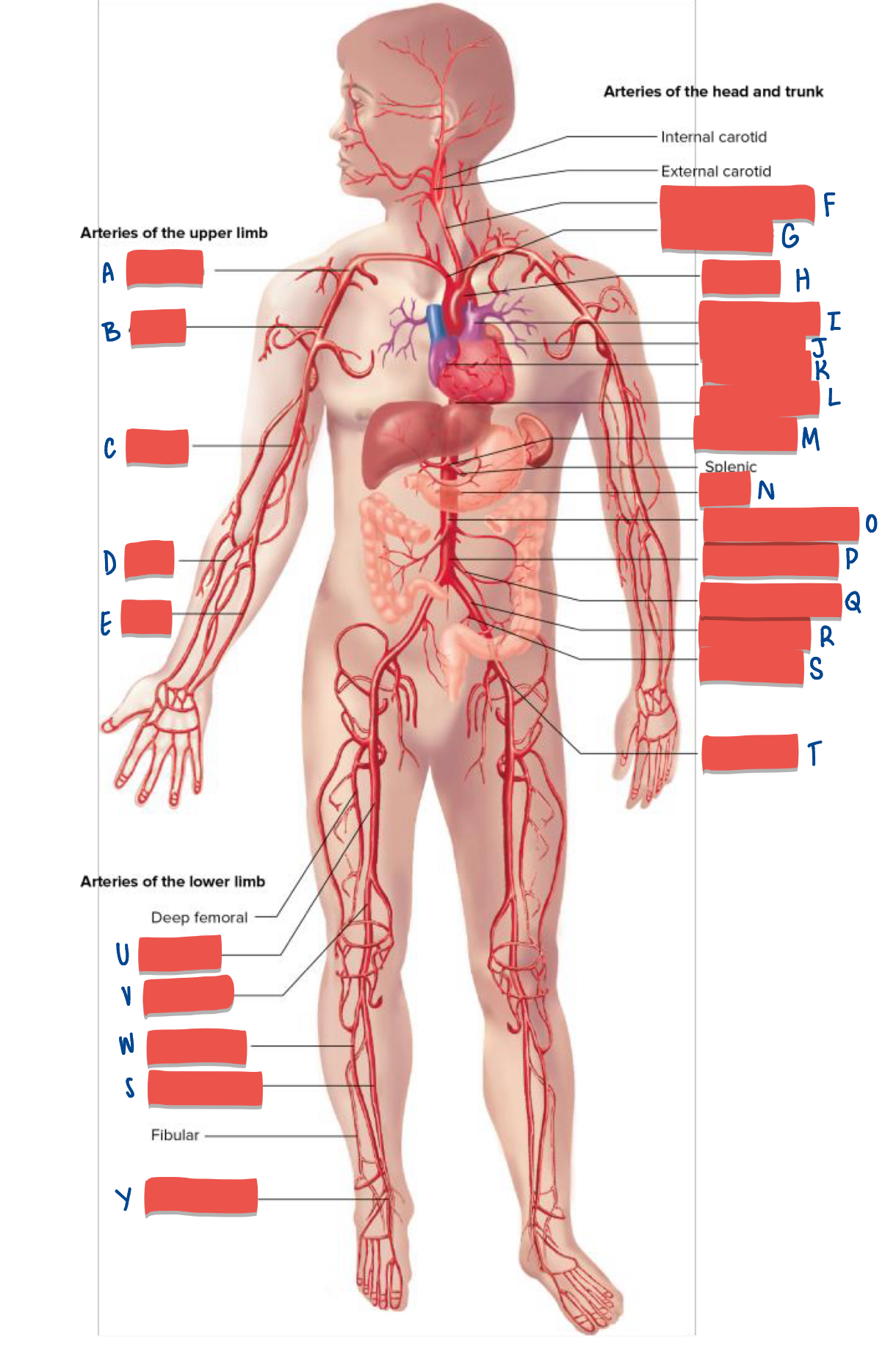
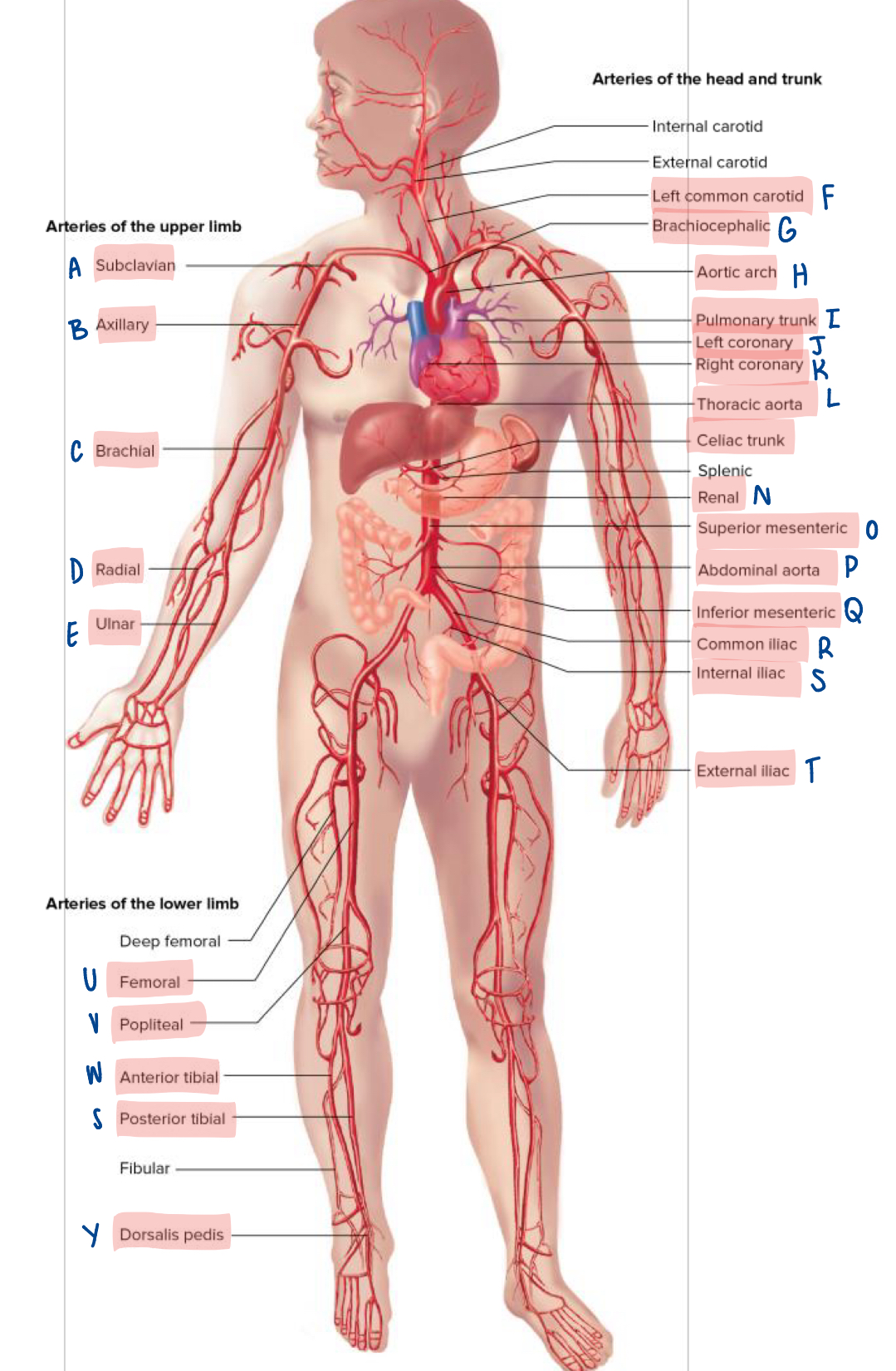
What are the three types of arteries?
elastic, muscular and arterioles
Elastic arteries
they have the largest diameter and have greater amount of elastic tissue which allows for expand and recoil. Small amount of muscular tissue. Example includes the aorta and major branches.
Muscular arteries
Thick tunica media, 25-40 layers of smooth muscles which allows for vasoconstriction and vasodilation to regulate blood supply. Examples include medium and small sized arteries.
Arterioles
They decrease in size, diameter and wall thickness with gradual loss of wall layers down to terminal arterioles. Transportation of blood to capillaries
Venules
Tubes of endothelial cells resting on a basement membrane with a few smooth muscle cells. As diameter of venules increases, amount of smooth muscles increases and they become veins.
What are the properties of veins?
thin walls and large lumen, thin tunica interna and tunica media. Tunica externa is the predominant layer. Veins have valves that are created due to folds in the tunica interna.
Veins are compliant and capacitance. What does this mean?
Compliant - veins can easily stretch and expand due to a change of pressure. They can accept a large increase in blood volume with only a small increase in pressure.
Capacitance - veins hold a lot of blood at very low pressure
Explain the structure of capillaries
Endothelial cells sitting on a basement membrane and delicate layer of loose connective tissue on the outside
Function of capillaries?
Rapid exchange of nutrients and metabolites between blood and interstitial fluid
How do substances move cross capillaries?
via diffusion. lipid-soluble and small water-soluble molecules diffuse through the plasma membrane, while larger water-soluble molecules pass through fenestrae (gaps between endothelial cells)
What are the three types of capillaries and what are they classified based on?
Classified based on size and permeability. The three types include continuous, fenestrated and sinusoidal.
Continuous capillaries
no gaps in between endothelial cells eg. muscle, nervous tissue and skin

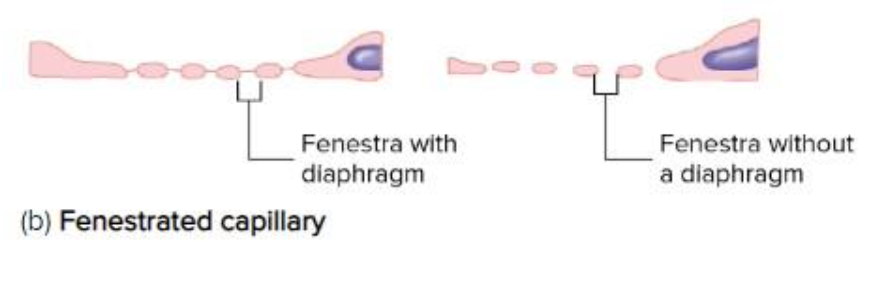
Fenestrated capillaries
highly permeable due to numerous fenestrae eg. intestinal villi, glomeruli in kidney and endocrine glands
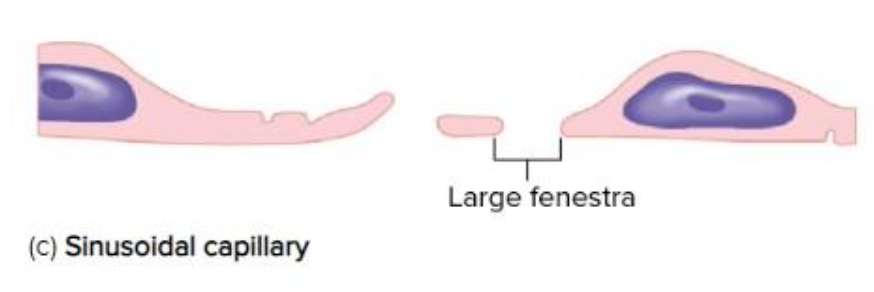
Sinusoidal capillaries
larger in diameter and large fenestrae and basement membrane is sparse or often missing eg. bone marrow and liver
Describe steps of blood flow in capillaries
arterioles —> metarteriole —> thoroughfare channel —> arterial capillaries —> venous capillaries —> vanule
What is the opening and closing of capillaries controlled by?
precapillary sphincters
Where are capillaries more numerous and highly extensive?
In highly metabolic tissues like lungs, liver, kidney and skeletal muscles
Arteriovenous anastomoses
are connections between arterioles and venules that allow blood to bypass capillaries, regulating blood flow and temperature. located at palm of hands and sole of feet
Net hydrostatic pressure
blood pressure within capillaries as a result of the heart’s contraction force
Net osmotic pressure
different in osmotic pressure between the blood and interstitial fluid
Describe the net filtration pressure in relation to net hydrostatic pressure and net osmotic pressure
At the arterial end of capillaries, the net filtration pressure is positive because the net hydrostatic pressure (pressure within capillaries) is greater than the osmotic pressure. More fluid moves out of the capillaries
At the venous end of capillaries, the net filtration pressure is negative because the net hydrotatic pressure is less than the net osmotic pressure. More fluid moves into the capillary
What is blood circulation determined by and what are the two different types?
Determined by pressure, flow and resistance. The two types are laminar flow and turbulent flow.
Laminar flow
blood flows in a streamline - through long, smooth-walled, equal diameter tubes. Blood closes to the outmost layer flows the slowest due to greatest resistance, and blood within the centre flows the fastest due to less resistance
Turbulent flow
blood passes a constriction, a sharpe turn or rough surface caused by numerous small crosswise currents. Common in heart as blood flows past valves.
Blood flow is directly proportional to __________ and inversely proportional to _________. What does this mean?
the difference in pressure; resistance. Blood flows from an area of high pressure to low pressure and when resistance decreases, blood flow increases
Resistance is directly proportional to _______ and _________. And inversely proportional to __________
length of the vessel; viscosity of blood; diameter of the vessel
The rate of blood flow through a tube can be expressed as…..
the volume that passes a specific point per unit of time. mL per min
what is the rate of cardiac output at rest?
approximately 5 liters per minute
equation for blood flow
is defined as the difference in pressure divided by resistance.
(P1 - P2) / R. Where P1 and P2 are pressures in the vessel at points 1 and 2
Equation for resistance
128vl/pieD^4 where v is viscosity of blood, l is length and d is diameter of the vessel
Cardiac Output (CO)
amount of blood pumped by the heart per minute
Blood Pressure (BP)
the force blood exerts against blood vessels walls measured in mmHg
What are the two homeostatic mechanisms involved to control blood flow
local control and extrinsic (nervous and hormonal)
Local control - local metabolic factors
vasodilation increases with increased amount of carbon dioxide, temperature, nitric oxide and decreased oxygen. blood flow increases when tissue metabolism increases
Local control - other local vasoactive substances
vasodilators: histamine, bradykinins, prostacyclins
vasoconstrictors: endothelin-1, leukotrienes, thromboxane-A2
Local control - myogenic control
about blood pressure
passive stretch of blood vessels, due to blood flow, causes vasocontriction
decreased stretch, due to sudden drop in blood flow, causes vasodilation
Extrinsic control - nervous control
controlled by the ANS, particularly the sympathetic division
rapid (1-30sec)
sympathetic vasomotor fibres - innervate blood vessels and control vasoconstriction
the vasomotor centre at lower pons and upper medulla oblongata regulates this constriction
Extrinsic control - hormonal control
noradrenaline and adrenaline causes vasoconstriction
adrenaline can also act on beta-2 receptors to cause vasodilation
angiotensin II and ADH are vasoconstrictors
ANP (atrial natriuretic peptide) is a vasodilator
Blood pressure
a measure of the force blood exerts against blood vessels walls. it fluctuates between systolic and diastolic pressure with an average of 120/80 for an adult
Mean Arterial Pressure (MAP)
important to ensure blood flow to all areas of the body and is calculated as the average blood pressure in a person's arteries during one cardiac cycle. It is commonly estimated using the formula: MAP = DBP + 1/3(PP), where PP = SBP - DBP.
Name the 4 short term regulations and the overall function
function: responds quickly for a short period of time, sec/mins, neural and hormones
chemoreceptor reflex
adrenal medullary mechanism
CNS’s ischemic response
baroreceptor reflex
Name the 3 long term regulation and the overall function
function: mechanisms that do not adapt rapidly to altered blood pressures, primarily by mechanisms that influence kidney function, hours to days
renin-angiotension-aldosterone mechanism
antidiuretic hormone
artial natriuretic mechanism
Baroreceptor reflexes
Baroreceptors that are sensitive to stretch and can detect small changes. Receptors are scattered along the walls of most major arteries such as neck, thorax, carotid and walls of aortic arch.
baroreceptors in the carotid sinus and aortic arch monitor blood pressure
the GLOSSOPHARYNGEAL (from carotid sinus baroreceptor) and VAGUS NERVES (from aortic arch baroreceptor) conduct action potentials to the cardioregulatory and vasomotor centers in the medulla oblongata.
increased parasympathetic stimulation of heart decreases heart rate OR increased sympathetic stimulation of the heart increases the heart rate and stroke volume
increased sympathetic stimulation of blood vessels increases vasoconstriction therefore increasing blood pressure
Adrenal Medullary Mechanism
Increase in sympathetic stimulation of the heart and blood vessels which is triggered by increase in physical activity, stress or decrease in blood pressure. Sympathetic nerve fibres stimulates the adrenal medulla which secrete epinephrin and noraepinephrin
Chemoreceptor reflex
Chemoreceptors in the carotid, aortic bodies and medulla oblongata are sensitive to low oxygen levels, low pH levels and increase in carbon dioxide levels. When detected, the parasympathetic is inhibited which increased heart rate. Sympathetic stimulation also increases heart rate, stroke volume, and vasoconstriction.
CNS’s Ischemic Response
An increase in blood pressure in response to lack of blood flow to the medulla oblongata of the brain. An emergency function which results in the vasomotor centre stimulating vasoconstriction.
Renin-Angiotensin-Aldosterone (+ADH) mechanism (RAAS)
low blood volume, low MAP or poor renal flow causes renin secretion from juxtaglomerular cells in the kidneys
renin catalyses the formation of angiotensin 1 in the blood from a precusror plasma protein, angiotensinogen
angiotensin 1 is converted to angiotensin 2 as the blood flows through the lungs
angiotensin 2 stimulates aldosterone and anti-diuretic hormone secretion which increase Na, Cl and water reabsorption from renal tubules, which leads to increased blood volume and MAP
ADH mechanism
ADH is a vasopressin that works in harmony with RAAS
decrease blood pressure detected by baroreceptors release ADH
ADH acts on the blood vessels to cause vasoconstriction. It also decreases the rate of urine production by kidneys to help maintain blood pressure (water reabsorption)
Atrial Natriuretic mechanism
Atrial Natriuretic Hormone (ANH) is a polypeptide released from cells in the atria of the heart
it acts on the kidneys to increase rate or urine production and Na loss via urine
dilates arteries and veins
causes decrease in blood volume, venous return and decrease in peripheral resistance
Poiseuille’s Law
flow = pie(p1-p2)d^4 / 128vl