MOD 4 - hip fractures
1/52
Earn XP
Description and Tags
Flashcards for hip dislocations and fractures, covering causes, classifications, complications, and imaging techniques.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
What are the most common causes of traumatic hip dislocations?
Motor vehicle accidents, falls from height, and sports injuries.
Why are hip dislocations less common than hip fractures?
Due to the hip's stable ball-and-socket joint and strong surrounding muscles.
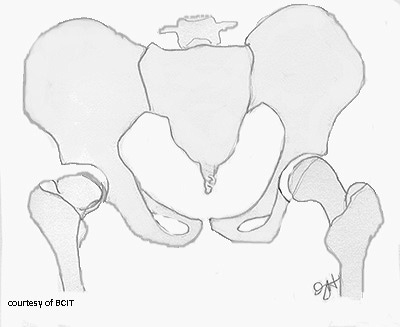
How are hip dislocations classified?
Based on the femoral head's position relative to the acetabulum: anterior, posterior, or central.
Where is the femoral head located in an anterior dislocation?
Over the obturator foramen or pubic bone (anterior, inferior, medial to the acetabulum).
What is the typical limb presentation in anterior hip dislocation?
Mildly flexed, abducted, externally rotated hip.
What causes an anterior dislocation?
A downward and forward force applied to a flexed hip.
What are complications of anterior hip dislocations?
Avascular necrosis, sciatic nerve damage, vascular damage.
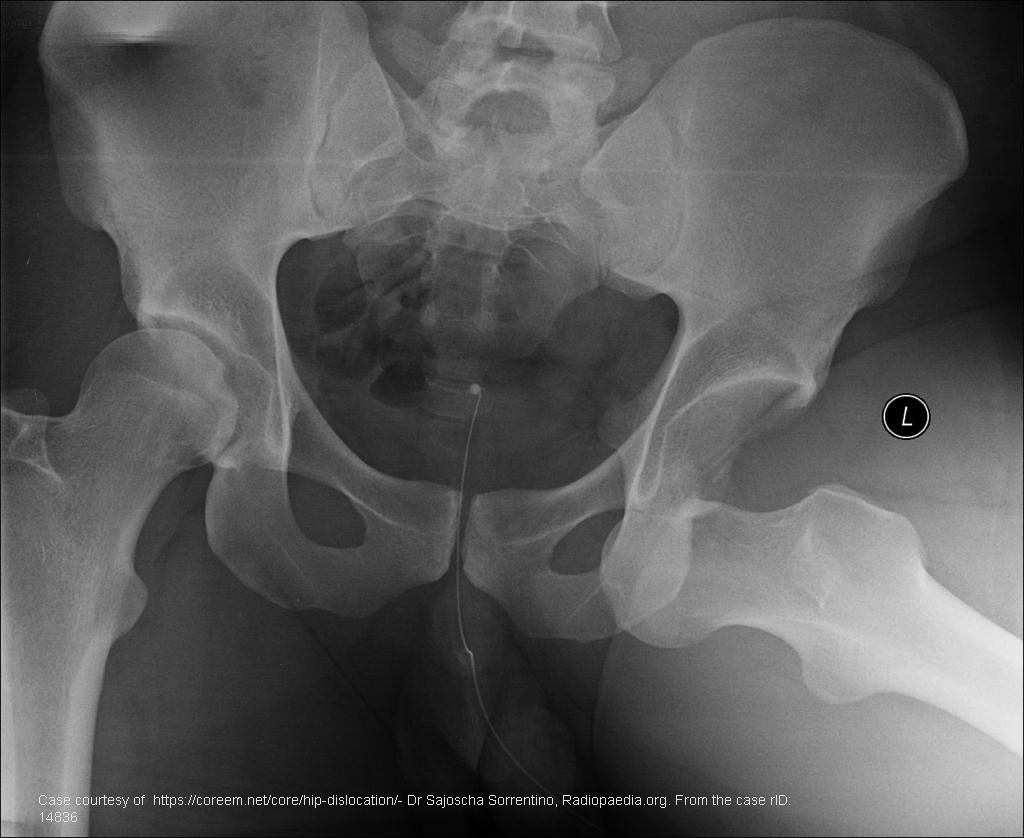
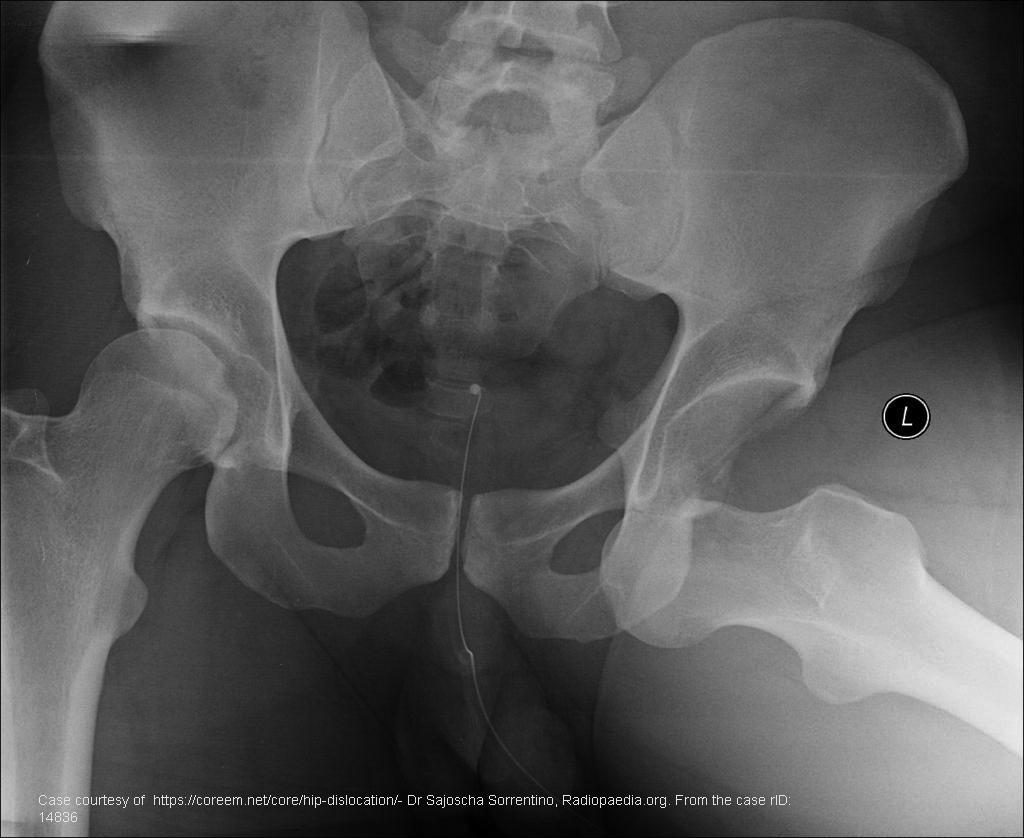
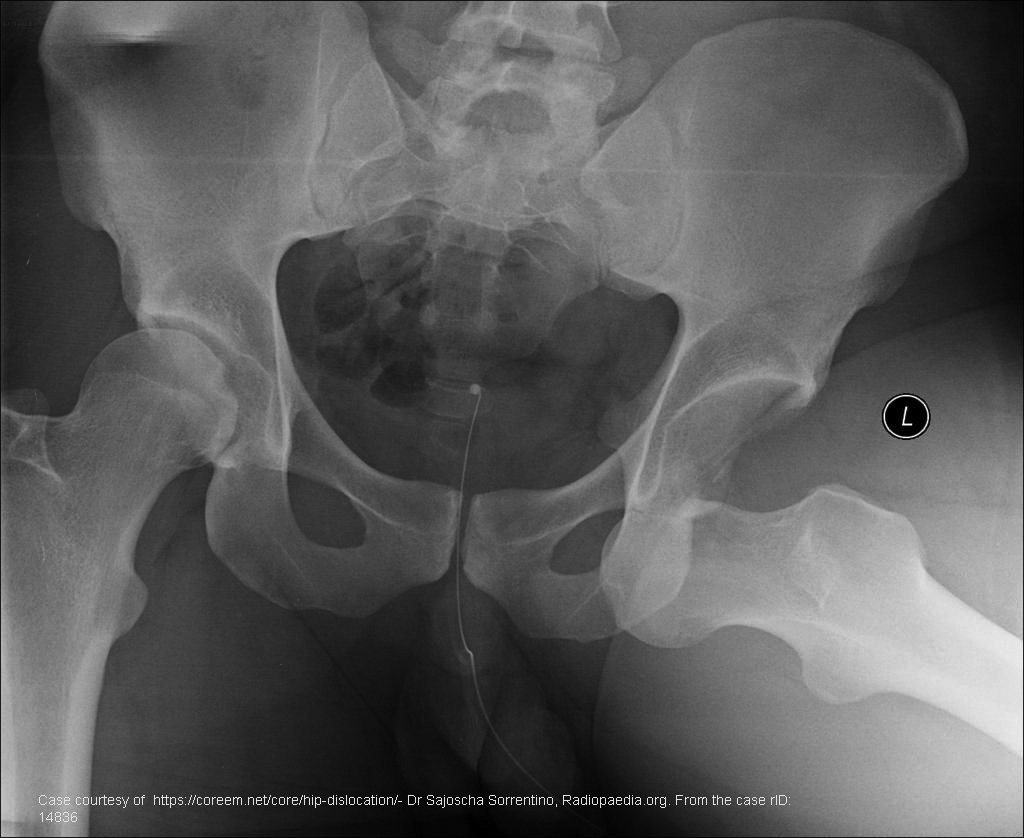
Where is the femoral head in a posterior dislocation?
Posterior and superior to the acetabulum.

What is the most common type of hip dislocation?
Posterior dislocation.

How does the limb typically present in a posterior dislocation?
Flexed, adducted, and internally rotated hip with a shortened leg.
What are complications of posterior dislocation?
Avascular necrosis, sciatic/vascular damage, chronic pain, arthritis.

What mechanism often causes posterior hip dislocation?
Force applied to a flexed and adducted hip (e.g., dashboard injury).
Where is the femoral head in a central hip dislocation?
Forced through the acetabulum into the pelvic cavity.

What usually accompanies a central dislocation?
Associated pelvic fractures.

What causes a central dislocation?
Lateral force to an adducted hip (e.g., MVA side impact or fall).
What are complications of central dislocation?
Avascular necrosis, nerve/vascular damage, damage to abdominal organs.
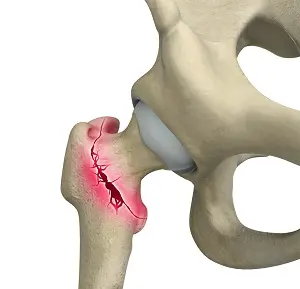
What part of the femur is affected in a “hip fracture”?
The proximal femur (not the hip joint itself).
Who is most at risk for hip fractures and why?
Elderly females due to osteoporosis, vision loss, and balance issues.
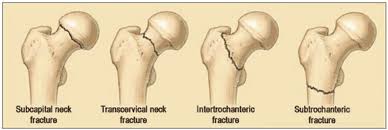
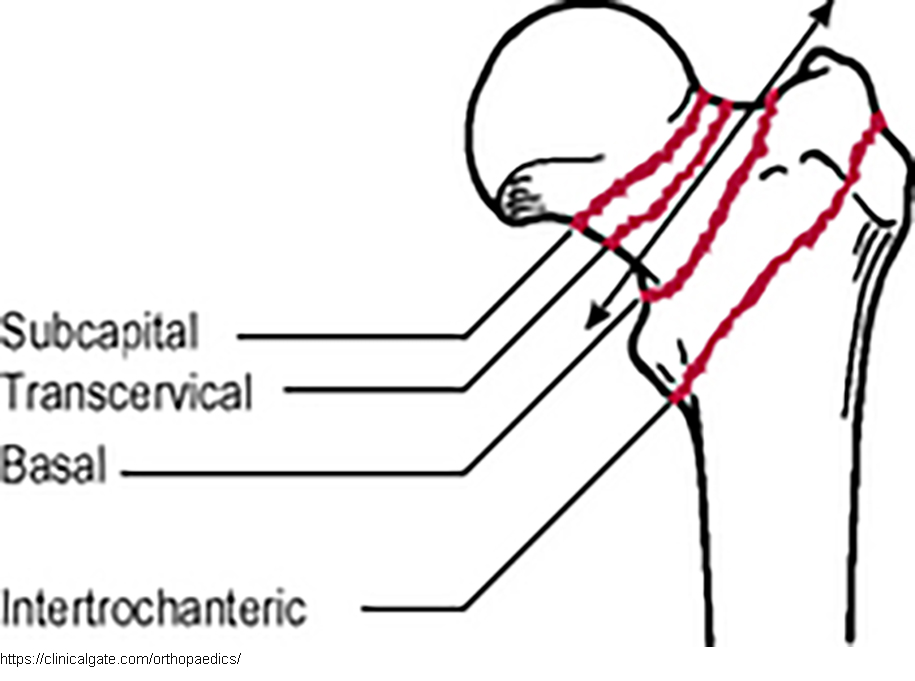
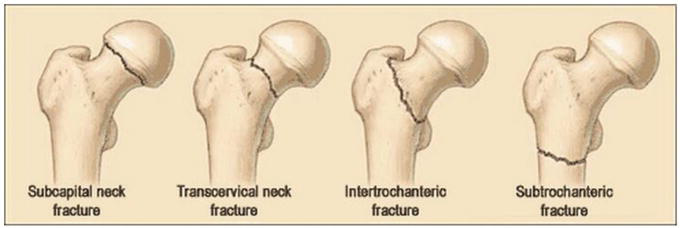
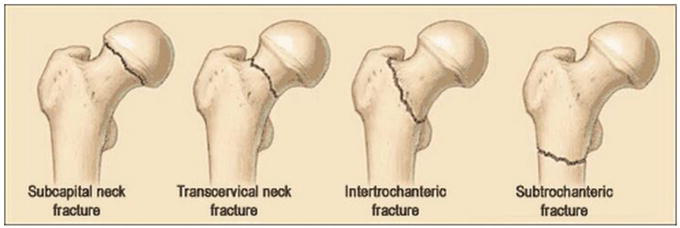
How are hip fractures classified?
Intracapsular (e.g., subcapital) and extracapsular (e.g., intertrochanteric).
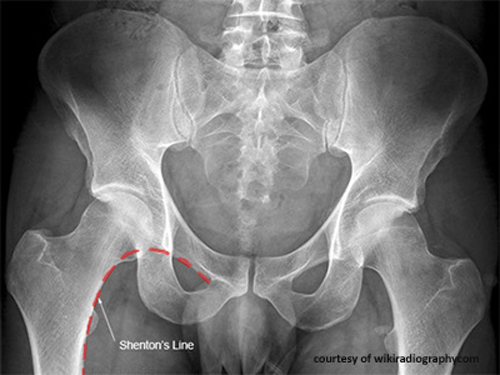
What is Shenton’s Line used for?
To help identify femoral neck fractures on AP pelvis images.
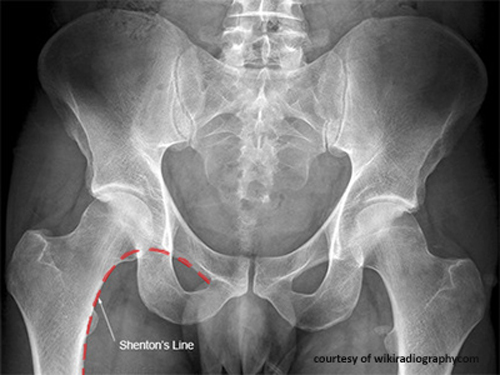
What does a disrupted Shenton’s Line suggest?
A fracture of the femoral neck.
Where is a subcapital fracture located?
Just below the femoral head.

What are key complications of subcapital fractures?
AVN, sciatic nerve damage, acetabular rim fracture, PE, pneumonia.

What is another name for a transcervical (femoral neck) fracture?
Femoral neck fracture.
What symptoms are associated with transcervical fractures?
Groin pain, hip deformity, limited movement.
Where is a basilar hip fracture located?
At the base of the femoral neck, near the trochanters.
What extra complication may occur with basilar fractures?
Possible avulsion fractures of the greater or lesser trochanter.
Where does an intertrochanteric fracture occur?
Between the greater and lesser trochanters.
What are potential complications of intertrochanteric fractures?
Malunion, AVN, nerve damage, PE, pneumonia, arthritis.
What is the pattern of subtrochanteric fractures?
Transverse or oblique fracture below the trochanters.
How are subtrochanteric fractures treated?
Surgical reduction and stabilization of the femur.
What causes avulsion fractures of the trochanters?
Sudden, forceful muscle contraction (e.g., sports or trauma).
Who is most at risk for trochanteric avulsion fractures?
Young athletes.
What is the usual treatment for avulsion fractures?
Rest for 4–6 weeks.

What determines the type of surgical hardware used for hip fractures?
The fracture type and location.
What are pins used for in hip fracture repair?
Stabilizing fractures along the femoral neck.
What is a Dynamic Hip Screw (DHS) and its purpose?
A compression screw that tightens as the bone heals, promoting union.
What are intramedullary rods used for?
Stabilizing shaft fractures; inserted inside the femoral canal.
When is hip replacement performed?
For irreparable damage to the femoral head or joint.
What is the difference between total and partial hip replacement?
Total replaces femoral stem, ball, and acetabular cup; partial replaces only femoral components.
How are hip dislocations classified on diagnostic images?
By the position of the femoral head relative to the acetabulum—anterior, posterior, or central.
What key imaging feature distinguishes posterior hip dislocation?
Internally rotated and shortened limb with femoral head displaced superior and posterior to the acetabulum.
What clinical information is important to adapt a hip X-ray for a trauma patient?
Mechanism of injury, pain location, ability to bear weight, visible deformity, and limb positioning.
What positioning adaptations may be necessary when imaging a patient with a suspected hip fracture?
Avoid moving the limb; use cross-table lateral view instead of standard lateral to prevent further injury.
Which imaging sign can help detect femoral neck fractures?
Disruption or absence of Shenton’s Line on AP pelvis projection.
What serious complication can occur if hip dislocation reduction is delayed over 6 hours?
Avascular necrosis of the femoral head.
What nerve is at risk of damage in hip dislocations and fractures?
The sciatic nerve.
What are common systemic complications of hip fractures in elderly patients?
Pulmonary embolism, pneumonia, and complications from immobility or surgical anesthesia.
What long-term complication may result from damage to the articular capsule?
Early-onset arthritis due to premature wear and tear.
What mechanism typically causes posterior hip dislocation?
Force applied to a flexed and adducted hip, such as the knee hitting a dashboard.
What mechanism commonly causes anterior hip dislocation?
Downward and forward force to a flexed, abducted hip.
What mechanism leads to central hip dislocation?
Lateral impact to an adducted hip, driving the femoral head through the acetabulum.
How do avulsion fractures of the trochanters appear radiographically?
Small bony fragments pulled away from the trochanteric regions.