Chapter 18: Respiratory Diagnostic and Therapeutic Procedures
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
20 Terms
Chapter 18: Respiratory Diagnostic and Therapeutic Procedures
Purpose
Evaluate respiratory status
Assess oxygenation of the blood
Assess lung function
Assess integrity of the airway
Common Respiratory Diagnostic Procedures
Pulmonary function tests (evaluate lung volumes, capacities, and airflow)
Arterial blood gases (assess oxygenation, ventilation, and acid base balance)
Bronchoscopy (visualize airway, obtain samples, remove obstructions)
Thoracentesis (remove pleural fluid for analysis or symptom relief)
Nursing Responsibilities
Ensure informed consent is signed prior to diagnostic procedures
Verify understanding of the procedure by the client
Prepare the client according to the specific test requirements
Monitor for complications during and after procedures (airway compromise, bleeding, respiratory distress)
A nurse is reviewing information with a client who is scheduled for pulmonary function tests. Which of the following statements should the nurse make?
a
“Do not use inhaler medications for 6 hr following the test.”
b
“Do not smoke tobacco for 6 to 8 hr prior to the test.”
c
“You will be asked to bear down and hold your breath during the test.”
d
“The arterial blood flow to your hand will be evaluated as part of the test.”
b
“Do not smoke tobacco for 6 to 8 hr prior to the test.”
Pulmonary Function Tests (PFTs)
Purpose
Determine lung function and breathing difficulties
Identify presence and severity of lung disease
Assess respiratory risk prior to surgery
Measures
Lung volumes and capacities
Diffusion capacity (gas transfer)
Gas exchange
Flow rates
Airway resistance
Distribution of ventilation
Clinical Indications
Dyspnea
Suspected or known lung disease
Preoperative respiratory risk assessment
Nursing Considerations
Instruct client not to smoke 6 to 8 hr prior to testing (smoking alters airflow and gas exchange)
If client uses inhalers, withhold 4 to 6 hr before testing (varies by facility policy)
Ensure client understands test instructions to ensure accurate results
Arterial Blood Gases (ABGs)
Assess oxygenation and acid base balance of the blood
ABG Components
pH: amount of free hydrogen ions in arterial blood (acid base status)
PaO₂: partial pressure of oxygen (oxygenation)
PaCO₂: partial pressure of carbon dioxide (ventilation)
HCO₃⁻: bicarbonate concentration (metabolic component of acid base balance)
SaO₂: percentage of hemoglobin saturated with oxygen
Collection Methods
Arterial puncture
Arterial line
Indications and Potential Diagnoses
Evaluate acid base imbalances
Monitor respiratory, renal, electrolyte, endocrine, or neurologic conditions
Assess effectiveness of treatments (e.g., acidosis management)
Guide oxygen therapy
Evaluate response to weaning from mechanical ventilation
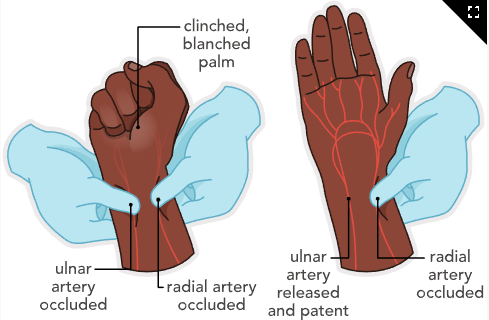
Arterial Puncture
Preprocedure Nursing Actions
Obtain a heparinized syringe
Perform Allen’s test to verify radial and ulnar artery patency
Compress radial and ulnar arteries while client makes a fist
Release ulnar artery and observe for capillary refill
Hand should turn pink within 15 seconds (adequate collateral circulation)
Explain the procedure and purpose to the client (reduces anxiety and improves cooperation)
Intraprocedure Nursing Actions
Use surgical aseptic technique
Collect arterial blood into a heparinized syringe
Cap the syringe and place specimen in ice and water immediately (preserves pH and oxygen levels)
Transport specimen to the lab promptly
Note that radial artery access may be more difficult in older adults due to decreased peripheral circulation
Arterial punctures are often performed by respiratory therapists in hospital settings
Postprocedure Nursing Actions
Apply direct pressure to the puncture site for at least 5 minutes
Hold pressure for at least 20 minutes if client is on anticoagulant therapy
Ensure bleeding has stopped before releasing pressure
Monitor site for:
Bleeding
Loss of pulse
Swelling
Changes in temperature or color
Document procedure, site condition, and client response
Report ABG results to the provider as soon as available
Implement prescribed respiratory interventions based on results (e.g., adjust oxygen or ventilator settings)
Allen's Test (Image)
Interpretation of ABG Findings
Blood pH
pH < 7.35 = Acidosis
pH > 7.45 = Alkalosis
ABG Measures and Expected Reference Ranges
pH: 7.35 to 7.45 (overall acid base balance)
PaO₂: 80 to 100 mm Hg (arterial oxygenation)
PaCO₂: 35 to 45 mm Hg (ventilation status)
HCO₃⁻: 22 to 26 mEq/L (metabolic component of acid base balance)
SaO₂: 95% to 100% (hemoglobin oxygen saturation)
Clinical Nursing Focus
pH reflects overall status, but PaCO₂ and HCO₃⁻ identify respiratory vs metabolic cause
PaO₂ and SaO₂ assess adequacy of oxygenation
Trends over time are more important than single values (treatment response monitoring)
Arterial Blood Gases (ABGs) Complications
Hematoma and Arterial Occlusion
Blood accumulates under the skin at the puncture site
Can impair distal circulation
Nursing Actions
Observe for:
Swelling
Color changes
Temperature changes
Pain
Loss of pulse (arterial compromise)
Apply firm pressure to the site
Notify the provider immediately if manifestations persist
Air Embolism
Air enters the arterial system during catheter insertion
Nursing Actions
Place the client in a flat or Trendelenburg position (prevents air migration)
Instruct the client to bear down and hold their breath (Valsalva maneuver)
Monitor for:
Sudden shortness of breath
Decreased SaO₂
Chest pain
Anxiety
Air hunger
Notify the provider immediately
Administer oxygen as prescribed
Obtain ABGs
Continuously assess respiratory status for deterioration
Bronchoscopy
Allows visualization of the larynx, trachea, and bronchi
Performed using a flexible fiber-optic or rigid bronchoscope
Can be done:
Outpatient
In a surgical suite under general anesthesia
At bedside with local anesthesia and moderate (conscious) sedation
Can be performed on mechanically ventilated clients via the endotracheal tube
Indications and Potential Diagnoses
Visualization of abnormalities:
Tumors
Inflammation
Strictures
Biopsy of suspicious tissue (lung cancer)
Increased risk for bleeding and perforation
Aspiration of deep sputum or lung abscesses:
Culture and sensitivity
Cytology (e.g., pneumonia)
Therapeutic Uses
Removal of foreign bodies
Removal of secretions from the tracheobronchial tree
Treatment of postoperative atelectasis
Destruction or excision of lesions
Bronchoscopy Considerations
Preprocedure Nursing Actions
Assess for:
Allergies to anesthetic agents
Use of anticoagulants
Ensure informed consent is signed
Remove dentures prior to procedure
Maintain NPO status 4 to 8 hr (prevents aspiration when cough reflex is suppressed)
Administer prescribed preprocedure medications:
Anxiolytic
Atropine (reduces secretions)
Viscous lidocaine
Local anesthetic throat spray
Intraprocedure Nursing Actions
Position client sitting or supine
Assist with specimen collection and labeling
Ensure prompt transport of specimens to the lab
Continuously monitor:
Vital signs
Respiratory pattern
Oxygenation status
Use caution with older adult clients:
Sedation can precipitate respiratory arrest in those with respiratory insufficiency
Postprocedure Nursing Actions
Monitor:
Respirations
Blood pressure
Heart rate
Pulse oximetry
Level of consciousness
Assess for confusion or lethargy, especially in older adults
Assess for return of gag and cough reflex before oral intake
Withhold oral intake until reflexes return
Gag reflex may be delayed in older adults
Once gag reflex returns:
Offer ice chips
Progress to fluids
Monitor for complications:
Fever lasting more than 24 hr (infection)
Productive cough
Significant hemoptysis (small blood-tinged sputum is expected)
Hypoxemia
Be prepared to manage:
Aspiration
Laryngospasm
Provide oral hygiene
Encourage coughing and deep breathing every 2 hr
Older adults have increased risk of pneumonia due to reduced cough effectiveness and secretion clearance
Do not discharge until adequate cough reflex and respiratory effort are present
Client Education
Gargling with salt water or using throat lozenges may reduce throat soreness
Bronchoscopy Complications
Laryngospasm
Uncontrolled contraction of vocal cords causing airway obstruction
Nursing Actions
Continuously monitor for respiratory distress
Keep resuscitation equipment readily available
Pneumothorax
Can occur after rigid bronchoscopy
Nursing Actions
Assess breath sounds and oxygen saturation
Obtain follow-up chest x-ray
Aspiration
Occurs when oral or gastric contents enter the airway
Nursing Actions
Keep client NPO until gag reflex returns (usually about 2 hr)
Suction airway as needed
A nurse is assessing a client following a bronchoscopy. Which of the following findings should the nurse report to the provider?
a
Blood-tinged sputum
b
Dry, nonproductive cough
c
Sore throat
d
Bronchospasms
d
Bronchospasms
The nurse should notify the provider immediately. Blood-tinged sputum, a dry, nonproductive cough, and a sore throat
Thoracentesis
Surgical perforation of the chest wall and pleural space using a large-bore needle
Used to:
Obtain pleural fluid for diagnostic evaluation
Instill medication into the pleural space
Remove fluid (effusion) or air for therapeutic relief of pleural pressure
Performed under local anesthesia at the bedside, procedure room, or provider’s office
Ultrasound guidance decreases risk of complications
Indications and Potential Diagnoses
Determine cause of pleural effusion:
Transudates (heart failure, cirrhosis, nephrotic syndrome, hypoproteinemia)
Exudates (inflammatory, infectious, neoplastic conditions)
Empyema
Pneumonia
Blunt, crushing, or penetrating chest trauma
Postoperative complications from lung or cardiac surgery
Client Presentation
Large pleural effusions compress lung tissue causing:
Chest pain
Shortness of breath
Cough
Other signs of pleural pressure
Assessment findings:
Abnormal or diminished breath sounds
Dullness to percussion
Decreased chest wall expansion
Pain related to inflammation
Interpretation of Findings
Aspirated fluid analyzed for:
Appearance
Cell count
Protein and glucose levels
Enzymes (LDH, amylase)
Abnormal cells
Culture
transudates vs exudates
Thoracentesis Considerations
Preprocedure Considerations
Percussion, auscultation, x-ray, or ultrasound used to locate effusion and insertion site
Older adults may require assistance maintaining position due to arthritis, tremors, or weakness
Preprocedure Nursing Actions
Verify informed consent
Gather all required supplies
Obtain preprocedure chest x-ray
Position client:
Sitting upright
Arms and shoulders supported on pillows or overbed table
Feet and legs well supported
Client education:
Remain absolutely still
Do not cough or talk unless instructed (prevents needle injury)
Intraprocedure Nursing Actions
Assist provider using strict surgical aseptic technique
Prepare client for pressure sensation during needle insertion and fluid removal
Monitor:
Vital signs
Skin color
Oxygen saturation
Measure and document amount of fluid removed
Label specimens at bedside and send promptly to laboratory
Fluid removal limited to 1 L at a time (prevents re-expansion pulmonary edema)
Postprocedure Nursing Actions
Apply dressing to puncture site and assess for bleeding or drainage
Monitor vital signs and respiratory status hourly for first several hours:
Respiratory rate and rhythm
Breath sounds
Oxygenation status
Auscultate lungs for decreased breath sounds on affected side
Encourage deep breathing to promote lung expansion
Obtain postprocedure chest x-ray:
Confirm resolution of effusion
Rule out pneumothorax
effusion
A nurse is caring for a client who is scheduled for a thoracentesis. Which of the following supplies should the nurse ensure are in the client’s room?
Select all that apply.
a
Oxygen equipment
b
Incentive spirometer
c
Pulse oximeter
d
Sterile dressing
e
Suture removal kit
a
Oxygen equipment
c
Pulse oximeter
d
Sterile dressing
Thoracentesis Complications
Mediastinal Shift
Shift of thoracic structures to one side
Nursing Actions
Monitor vital signs
Auscultate lungs for decreased or absent breath sounds
Pneumothorax
Collapsed lung due to lung injury during procedure
Nursing Actions
Monitor for:
Diminished breath sounds
Distended neck veins
Chest wall asymmetry
Respiratory distress
Cyanosis
Review postprocedure chest x-ray results
Client Education
Can occur within first 24 hr
Report:
Deviated trachea
Sharp chest pain
Affected side not moving with breathing
Increased heart rate
Rapid, shallow respirations
Nagging cough
Air hunger
Bleeding
Risk increased with movement or bleeding disorders
Nursing Actions
Monitor for coughing and hemoptysis
Assess vital signs and labs:
Hypotension
Decreased hemoglobin
Inspect thoracentesis site for bleeding
Infection
Bacterial introduction at needle site
Nursing Actions
Maintain sterile technique
Monitor temperature after procedure
A nurse is caring for a client who is scheduled for a thoracentesis. Prior to the procedure, which of the following actions should the nurse take?
a
Position the client upright, leaning over the bedside table.
b
Explain the procedure to the client.
c
Perform an Allen’s test on the client.
d
Administer benzocaine spray to the client.
a
Position the client upright, leaning over the bedside table.
When taking actions, the nurse should identify that positioning the client in an upright position, bent over the bedside table, widens the intercostal space for the provider to access the pleural fluid.
A nurse is assessing a client following a thoracentesis. Which of the following findings should the nurse report?
Select all that apply.
a
Dyspnea
b
Localized bloody drainage on the dressing
c
Fever
d
Hypotension
e
Report of pain at the puncture site
a
Dyspnea
c
Fever
d
Hypotension