Thyroid chemistry
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
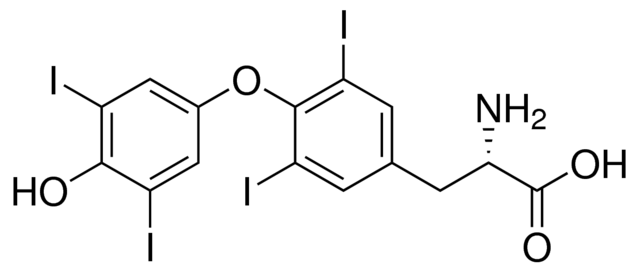
what is this?
thyroxine/ T4
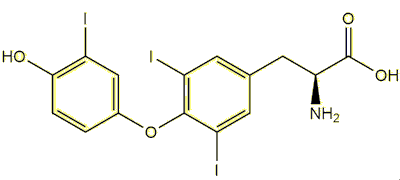
what is this?
Triiodothyronine/ T3
how is T3 formed from T4?
deiodinase= removal of iodine
which is more potent T3 or T4?
T3 is more potent (by 5x)
which amino acid is the thyroid hormone synthesized from?
L-tyrosine
what is the function of the 2 inner iodine molecules?
Creates a skewed conformation needed for activity
what effect does Iodine have on the phenyl ether bond?
restricts its movement
what is the necessary bond angle for the phenyl ether bond?
120o so the inner and outer ring are perpendicular to each other
what is the role of the O-bridge on the phenyl ether bond?
to maintain orientation of the phenyl rings (120o), the oxygen atom has nothing to do with it
can the oxygen on the phenyl ether bond be replaced/substituted? or is it an essential molecule
it can be replaced! by -S or -CH2 as long as the bond angle remains 120o
which part of the thyroid hormone is responsible for a majority of the mass?
Iodine
in which peripheral tissues is the prohormone Thyroxine (T4) deiodinated?
liver and kidneys
what is the predominate circulating form of the thyroid hormone? and why
Thyroxine (T4)
more ionized = able to form ionic bonds with protein carriers
where is thyroxine (T4) formed?
thyroid gland ONLY
where is Triiodothyronine (T3) formed?
T4 conversion= 80%
thyroid gland= 20%
what isomer are ALL natural thyroid hormones?
L
does Iodine act as an EWG or a EDG?
EWG
makes phenolic -OH more acidic
what happens to most of the phenolic -OH located on T4?
ionized to -O (80% of the time)
due to more ionic binding
what happens to most of the phenolic -OH located on T3?
remains unionized (only 10% ionized at body pH)
due to more hydrogen bonding
which thyroid hormone is usually more ionized at body pH? and why
T4
iodine increase electronegativity —> increases molecule’s acidity —> more deprotonated/ionized at lower pHs
which thyroid hormone is the active form? and why
T3
not ionized at body pH —> better able to transport into nucleus —> can hydrogen bind to thyroid hormone receptor
is T3 preferred by receptors or by transport proteins?
receptors (hydrogen binding)
is T4 preferred by receptors or by transport proteins?
transport proteins (ionic binding)
what is the first step of thyroid hormone synthesis?
iodine taken into thyroid follicular cell by N/I symporter
what does the Na/I symporter do?
taken iodine from the blood up into the thyroid follicular cell
what drives the Na/I symporter? does it require energy?
sodium gradient
doesn’t require energy
what is the role of the thyroid peroxidase (TPO)? where is this located?
oxidizes iodine in the apical membrane (for MIT/DIT production)
after TPO, where does the now oxidized iodine bind to?
thyroglobulin
what is the role of thyroglobulin? after binding the oxidized iodine
forms MIT (monoiodotyrosine) and DIT (diiodotyrosine)
what catalyzes the coupling reaction?
TPO
which reaction is a target for some antithyroid drugs/ high-dose iodine treatments to treat hyperthyroidism?
coupling reaction
what is endocytosis? what is it facilitated by?
MIT/DIT/T3/T4 bound to thyroglobulin goes back into follicular cell
facilitated by TSH
what is proteolysis?
T4 and T3 released from the follicular cell into the bloodstream
the basal membrane is located between the follicular cell and the ______?
blood
the apical membrane is located between the follicular cell and the ______?
follicular colloid
where is thyroglobulin synthesized?
endoplasmic reticulum
where is thyroglobulin stored?
follicular colloid
are thyroid hormones soluble in water?
NO!
where is T4 deiodinated?
liver/kidney peripheral tissues and target cells
what does T3 play an important role in? (think: why is it important that pregnant mothers get enough iodine)
regulating metabolism
growth/development
maintaining homeostasis
where is Thyroid Stimulating Hormone TSH produced?
hypothalamus
what are the 3 carrier proteins?
thyroxine binding globulin (75%)
transthyretin (10-15%)
albumin (least)
why are thyroid hormones bound to carriers during transportation?
protect from thyroxine metabolism and secretion
which carrier binds most of the thyroid hormones?
thyroxine binding globulin
is there lots of free thyroid hormone is circulation? or is most of it bound
very little free thyroid hormone
almost 99% are bound
T3 vs. rT3 —> which is the active/inactive form?
T3= active
rT3= inactive (rings turn freely)
what does the thioamide propylthiouracil (PTU) do?
inhibits type I 5’D enzymes
catalyzes T4 —> T3
what is the ubiquitination mechanism?
inhibits type 2 5’D enzymes
type I 5’D generates T3 for _______? where are the enzymes located?
circulation in the thyroid, kidney, and the liver
type 2 5’D generates T3 for _______? where are the enzymes located?
local use in target tissues
what do type 1 & 2 5’Deiodinases generate?
T3
what does type 3 5’D do? where are the enzymes located?
INACTIVATES T3 (results in rT3) in all tissues
which enzyme converts T4 to T3 in peripheral tissue?
iodothyronine deiodinases (D)
aka: 5’D
thyroid hormone release pathway from hypothalamus ——→ target cells
hypothalamus releases TRH
TRH moves through hypophyseal portal system to pituitary glan, which stimulates release of TSH
TSH travels through bloodstream to the thyroid, which stimulates release of thyroid hormone
do thyroid hormones give a positive or negative feedback loop to the hypothalamus/pituitary gland?
NEGATIVE
too much T3/T4 leads to less TRH/TSH released
where is the Thyroid Releasing Hormone (TRH) located?
anterior pituitary gland
where is the Thyroid Stimulating Hormone (TSH) located?
basal membrane of thyroid
what type of receptors are TRH and TSH?
G-coupled Protein Receptors (GPCRs)
what 3 amino acids make up TRH?
histidine, proline, glutamate
which TSH subunit give specificity to the hormone?
beta
what types of bonds are present between the thyroid hormones and their receptors?
IONIC (carboxylate/arginine)
H-BOND (phenol/histidine)
where is the Thyroid Receptor located? what superfamily do they belong to?
nucleus of target cells in the nuclear superfamily
what are Thyroid Response Elements (TREs)?
what the Thyroid Receptors bind to