congenital defects of the rt heart
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
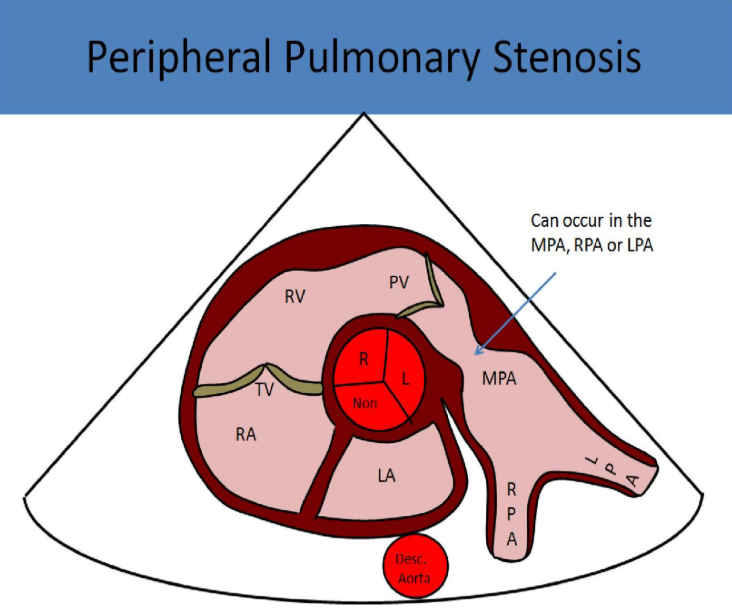
most common cause of congenital pulmonary stenosis
congenital malformation of cusps
acquired pulmonic stenosis is _____ seen in adults
rarely
when might acquired pulmonic stenosis be seen
in patients with carcinoid syndrome or rheumatic disease
congenital pulmonary stenosis is most commonly seen in
children
as a result to obstruction of flow what is commonly demonstrated in the rt heart
rt ventricular hypertrophy
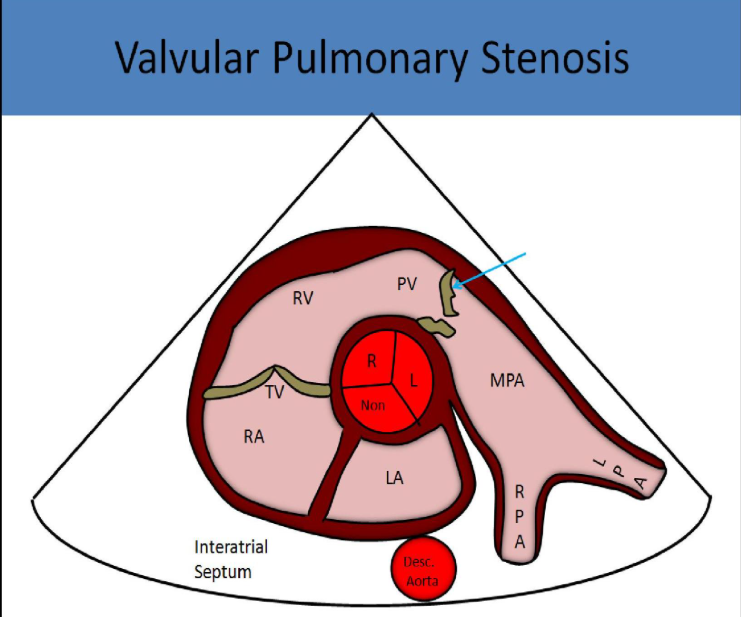
valvular stenosis is commonly associated with
maternal rubella
clubbing
turner syndrome
noonan syndrome
polycythemia vera
patients w moderate/severe pulmonic stenosis should have it corrected before becoming pregnant - why
increase in flow volume w pregnancy can cause significant complications
symptoms of pulmonic stenosis
dyspnea on exertion
sob
chest pain
syncope
fatigue
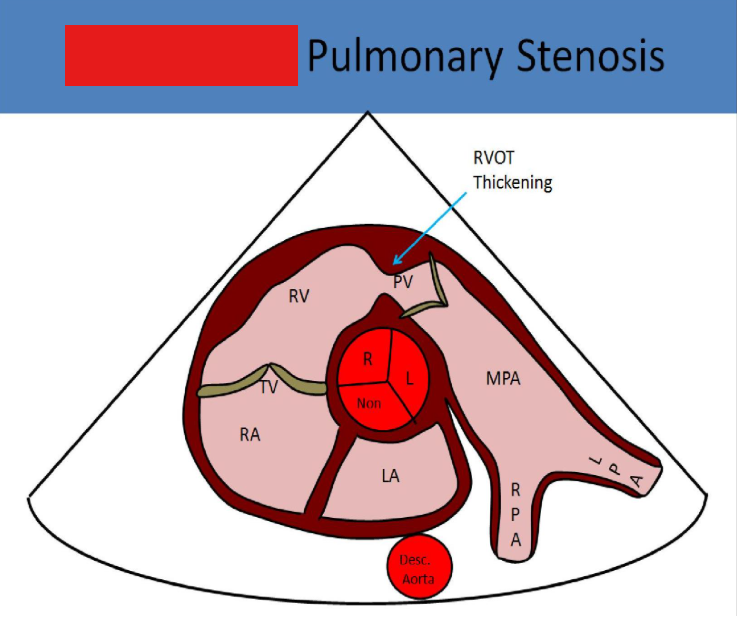
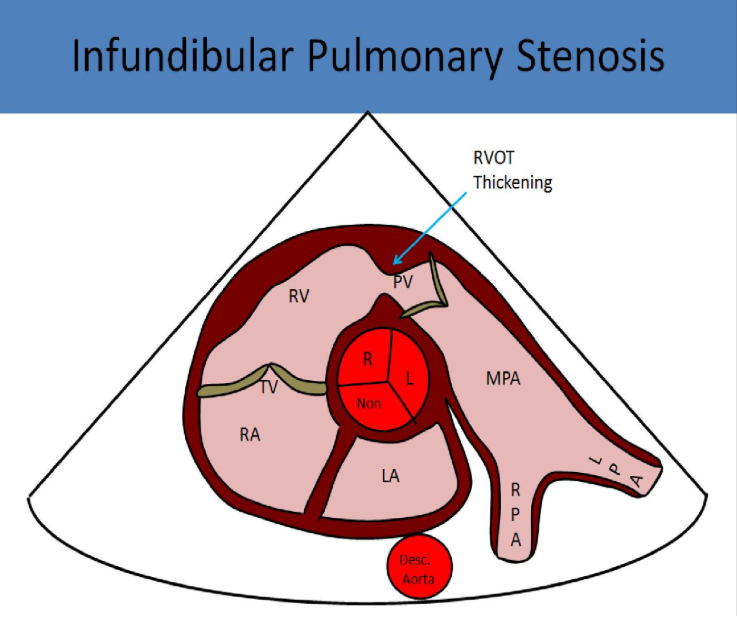
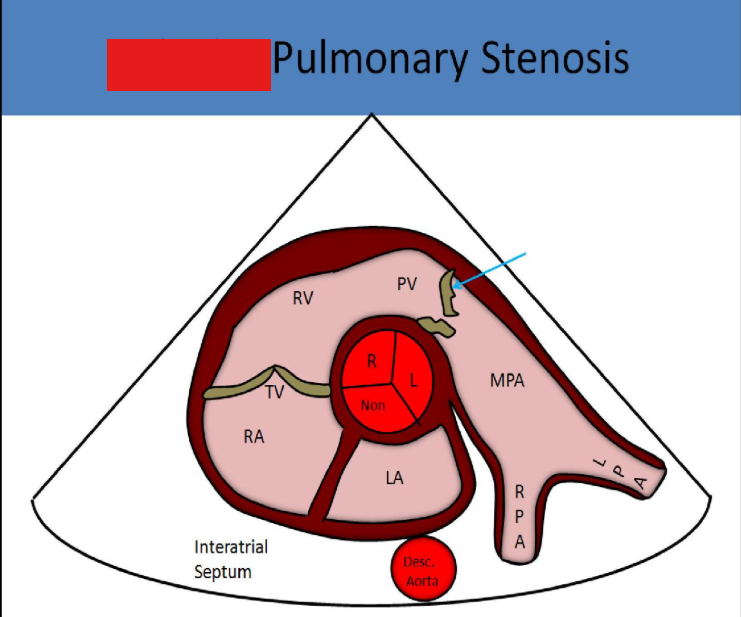
best views to demonstrate ps
left parasternal and subcostals, psax offers best insonation angle
with ps, m mode will show a significant increase in
the a wave
how will leaflets look w ps
thickened w systolic doming
how will the heart look w ps
rt ventricular hypertrophy
ra dilation
dilated main pa
mild, moderate, severe psv for ps
mild - .9 to 3 m/s
moderate - 3 to 4 m/s
severe - over 4 m/s
what ppg indicates severe ps
over 64 mmHg
this is associated with
tetralogy of fallot
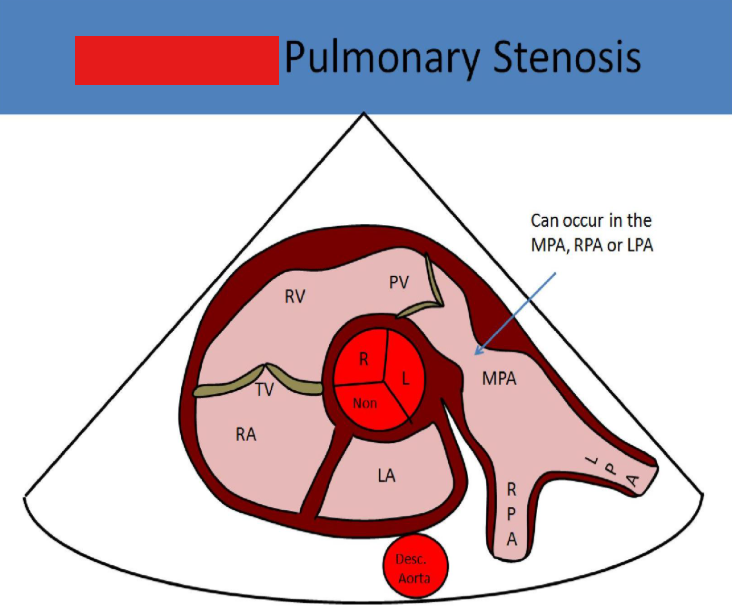
this is associated with
william syndrome
pulmonary atresia
absence of pulmonary valve opening, pulmonary artery is supplide by the ductus arteriosus
in pulmonary atresia, if there is no vsd, how does blood get to the left heart from the right
a pfo or small asd needs to be patent
how does blood move w pulmonary atresia and vsd
deoxygenated blood moves from ra to rv, through vsd to lv, exits through aorta, a pda then moves blood from descending aorta to pulmonary arteries (left to right shunt)
how does blood move w pulmonary atresia and no vsd
deoxygenated blood moves from ra through atrial septum to la and then lv, blood exits the lv through aorta, then a pda moves blood from descending aorta to the pulmonary arteries (left to right shunt)
overall how will the heart appear w pulmonary atresia
small, slit like rv
dilated left heart structures
flow reversal mpa = flow from pda backfills mpa
pseudotruncus
pulmonary atresia w vsd and overriding aorta
how is pseudotruncus differentiated from truncus arteriosus
pulmonary branch artery origins must be located
surgical correction options for pulmonary atresia
blalock-taussig shunt
fontan procedure
blalock-taussig procedure
connects the subclavian artery to the pulmonary artery to provide blood flow to the lungs
fontan procedure
venous return goes directly to the lungs
part 1 - glenn shunt: connect svc to rt pulmonary artery
part 2 - ivc connected by a conduit to rt pulmonary artery
tricuspid atresia
absence of opening in the tricuspid valve, causing a lack of direct communication between the rt atrium and rt ventricle
how does tricuspid atresia appear on us
echogenic plate-like structure is documented btween ra and rv
hypoplasic rv w dilated ra
pfo must be present to allow flow
tricuspid atresia is best evaluated in what views
apical, subcostal 4
surgical correction options for tricuspid atresia
palliative pulmonary artery banding
norwood procedure
palliative pulmonary artery banding
may be performed first to reduce flow to lungs in cases w a large vsd, allows patient to wait until they are older for correction
norwood procedure
part 1 - atrial septectomy, blalock taussig shunt
part 2 - glenn shunt: connect svc to rt pulmonary artery
part 3 - fontan procedure: ivc connected by conduit to rt pulmonary artery
ebstein anomaly
congenital malformation where tricuspid leaflets are more inferior and toward the apex of the heart
symptoms of ebstein anomaly
dyspnea
cyanosis
pedal edema
hepatomegaly
ascites
best view to diagnose ebstein
apical 4
mitral valve and tricuspid valve insertion points are normally under _____ apart
20 mm or 8 mm/m²
how does ebstein anomaly appear on us
tv annulus in normal position, only leaflets displaced
small rt ventricle
very large rt atrium
small d shaped left ventricle
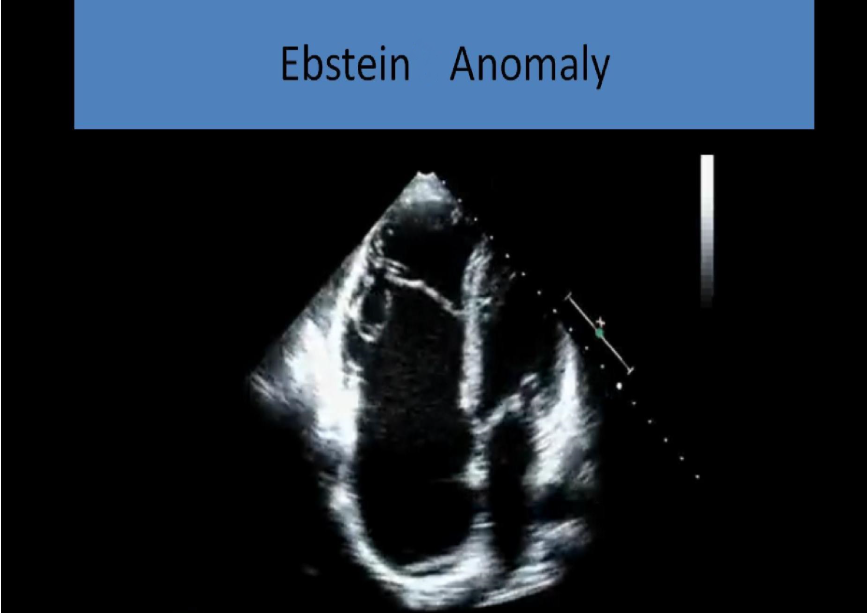
what is ebstein anomaly associated with
secundum asd (rt to left flow)
30% also have wolff-parkinson-white
how is ebstein anomaly treated
cone procedure to repair tv
glenn shunt used in cases that have functional pulmonary atresia due to malpositioned leaflets
eisenmenger syndrome
normal shunt flow is from rt to left, but chronic shunt flow can lead to increased rt heart pressures. eventually right ventricular pressures rise to exceed left and the shunt flow reverses
w eisenmenger syndrome, rvsp will be
over 120 mmHg
what does eisenmenger syndrome lead to
cyanosis and rt heart failure
most common cause of eisenmenger syndrome
vsd
persistent left svc
blood from left arm drains directly into coronary sinus through brachiocephalic vein
primary finding of persistent left svc
significantly dilated coronary sinus
how to see persistent left svc on us
plax view will demonstrate dilated coronary sinus between la and descending ao
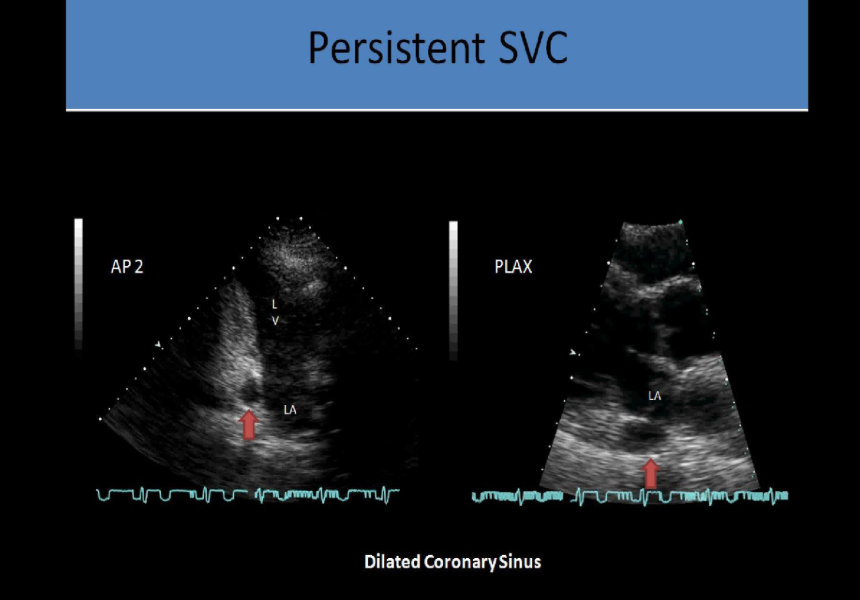
how is persistent left svc imaged
image at ssn longitudinally, tilt left to view vertical vein adjacent to the aortic arch
if bubbles are used to confirm persistent left svc, what will happen in a positive study
bubbles will fill the coronary sinus before the rt atrium
aortopulmonary window
direct connection between the ASCENDING aorta and mpa
how does aortopulmonary window appear w doppler
diastolic flow reversal in descending thoracic aorta
continuous murmur
symptoms of aortopulmonary window
respiratory infection
tachypnea
tachycardia
what does aortopulmonary window lead to
chf
pulmonary htn
what kind of shunting does aortopulmonary window cause
left to right unless eisenmenger syndrome is present
best view for evaluating aortopulmonary window
psax
patent ductus arteriosus
ductus arteriosus doesn’t close after birth, should close after 2 to 3 weeks, causing blood to be shunted through the ductus from the descending aorta to the pulmonary artery
what is pda associated w
premature birth
how does pda sound
continuous, high pitched machinery type murmur
symptoms of pda
cyanosis, esp in lower extremities
best view to demonstrate pda
high psax
what does pda cause in the heart
left ventricular volume overload
dilated hyperkinetic left ventricle
dilated left atrium
may see diastolic flow reversal in descending thoracic aorta
when can normal cardiac pressures be assumed
if the gradient revealed from shunt flow is equivalent to 100 mmHg, which is the normal different in pressure between pulmonary artery and aorta
treatment for pda
medical closure for newborns w indomethacin or device closure w a coil, occluder, or plug