1,2&3 Respiratory Pathology
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
Obstructive vs. Restrictive Pulmonary Diseases
Obstructive: Increased resistance to airflow caused by obstruction at any level
Decreased total lung volume (TLV)
Forced Vital Capacity (FVC) normal
Expiratory Flow Rate (FEV) decreased
FEV to FVC ratio decreased
Restrictive: Reduced expansion of lungs and decreased total lung capacity
FEV and FVC both decreased
FEV to FVC ratio normal
Name the 4 Obstructive Lung Diseases
Chronic Bronchitis
Emphysema
Asthma
Bronchiectasis
Chronic Bronchitis
Defined as
Causes
Pathogenesis
Clinical Features
Defined as persistent productive cough for at least 3 consecutive months in at least 2 consecutive years
Causes include cigarette smokers (%90) and urban dwellers in smog-ridden cities
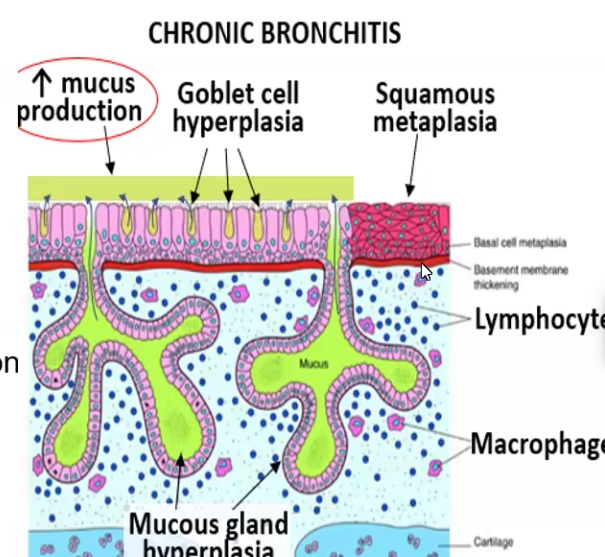
Pathogenesis: exposure to noxious inhalants causes goblet cell hyperplasia, hyperplasia/hypertrophy in submucosal mucinous glands, inflammation, squamous metaplasia leading to fibrosis and narrowing of lumen in smaller airways
Clinical Features: Mucus hypersecretion, productive cough for 3 months, “blue bloater” due to hypoxemia, may lead to Cor Pulmonale (Right Heart Failure) due to over-exertion of right ventricle
Emphysema
Defined as
Causes
Pathogenesis
Two types
Clinical Features
Emphysema is an irreversible enlargement of the air spaces distal to the terminal bronchioles (air sac, alveoli, alveolar ducts) accompanied by destruction of their walls without fibrosis
Cigarette smoking is the primary cause, followed by alpha1 antitrypsin (At1) deficiency (antiproteases defective cant fight oxidative stress)
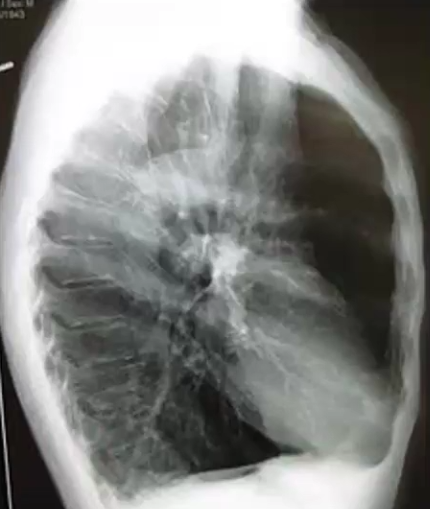
Pathogenesis: Noxious inhalation (or infection) causes too much oxidative damage and destructs lung alveoli, leading to decreased elastic recoil and overexpanded lungs
Types: Centrilobular emphysema affects primarily the upper lobes, Pacinar Emphysema affects both upper and lower
Clinical Features: Lungs are overinflated (“barrel chest”), diaphragm is depressed, pursed lip breathing (“pink puffers”) due to exertional dyspnea, can lead to Cor pulmonale
What are the overlapping features of Bronchitis and Emphysema?
Caused by smoking
Can lead to pulmonary hypertension
Asthma
Defined as
Causes
Pathogenesis
Two types
Clinical Features
Defined as intermittent and reversible airway obstruction
Caused by Type I hypersensitivity or Non-immune (non-atopic) things like infections, inhaled chemicals, drug induced, exercise and cold air
Pathogenesis: Inhaled allergen is phagocytosed by DC, presented to TH2 cell, then IL-4 causes B cells to class-switch to IgE and bind mast cells, then upon second exposure the mast cells degranulate uncontrollably and goblet cells produce mucus. This all leads to momentary airway narrowing due to hypertrophy of bronchial walls smooth muscle and mucus overproduction
Wheezing, dyspnea, chest tightness, cough, charcot-leiden crystals in sputum histologically
Bronchiectasis
Defined as
Causes
Predisposing Factors
Clinical Features
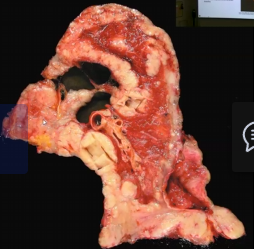
Defined as permanent dilation of the bronchi and bronchioles due to destruction of smooth muscle and elastic tissue
Caused by chronic necrotizing infections (Staph A. and Klebsiella)
Predisposing factors include bronchial obstruction, congenital conditions and necrotizing pneumonia (caused by Staph A. or Klebsiella!)
Clinical Features: Chronic cough, purulent sputum, dyspnea, hemoptysis and recurrent respiratory tract infections
Atelectasis
Defined as
Causes
Defined as alveolar collapse
Can be caused by Failure of expansion, obstruction, external constriction or lung immaturity in newborns (no surfactant)
Idiopathic Pulmonary Fibrosis (IPF)
Defined as
Causes
Pathogenesis
Clinical Features
Patchy, progressive bilateral interstitial fibrosis and respiratory failure, CRPD
Unknown etiology, said to have genetic component, seen after 50 yo
Germline MUC5B gene has telomerase loss and results in reduced mucin production and excessive fibroblastic proliferation → can be associated with smoking
Fibrotic lungs, patchy interstitial fibrosis, histology shows honeycomb shape, dry crackles during inspiration, dry cough, dyspnea on exertion, can lead to hypoxemia, cyanosis and clubbing
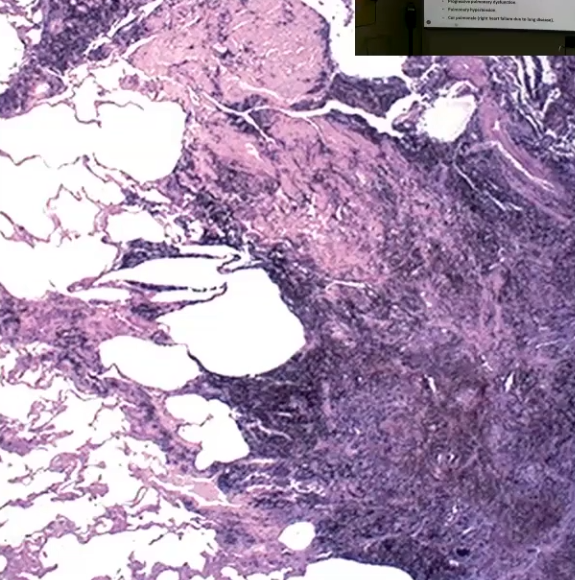
Simple Coal Worker’s Pneumoconiosis
Defined as
Causes
Pathogenesis
Clinical Features
Lung disorder caused by inhalation of coal dust
Caused by inhalation of carbon pigment
Carbon pigment/coal is inhaled and engulfed my alveolar and interstitial macrophages, causes inflammation and eventually leads to fibrosis and other complications
Starts as Pulmonary Anthracosis, a benign form → Progresses to Coal Worker’s Pneumoconiosis (CWP), where coal macules and coal nodules form, eventually leading to fibrosis and centrilobular emphysema → May complicate into Progressive Massive Fibrosis (PMF) which cause pulmonary dysfunction, pulmonary hypertension and Cor Pulmonale
Clinical features include multiple black scars in lungs, dense collagen and pigment due to fibrosis
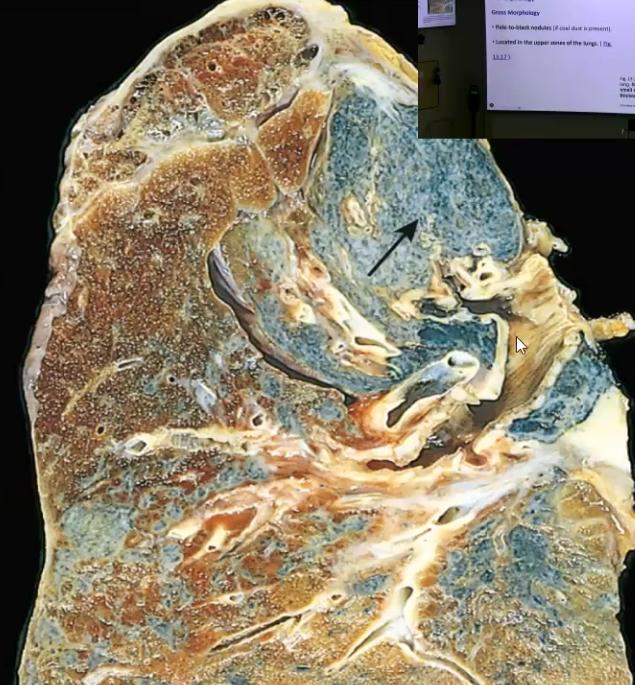
Silicosis
Defined as
Causes
Pathogenesis
Clinical Features
Lung disorder caused by inhalation of crystalline silica (quartz)
Inhalation of silica, most prevalent chronic occupational lung disease worldwide
Sandblasting and Hard-rock mining
Macrophages engulf silica particles and activate inflammasome, results in fibrosis and lung damage
Pale to black nodules in the upper zone of lungs, silicotic nodules arranged in whorled appearance and made of hyaline collagen fibers
Often asymptomatic until it has progressed to Progressive Massive Fibrosis (PMF) which includes pulmonary hypertension and cor pulmonale
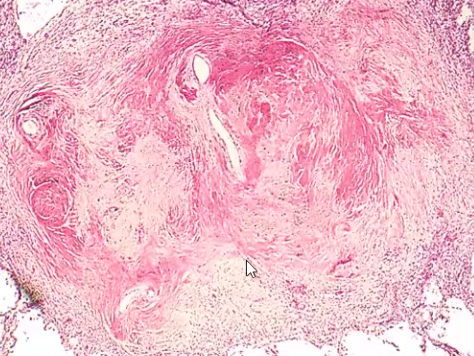
Asbestosis
Defined as
Causes
Pathogenesis
Clinical Features
Lung disorder (Pneumoconiosis)
Caused by heavy inhalation of asbestos fibers especially occupationally
Asbestos fibers are inhaled and phagocytosed by macrophages, which activates inflammasome → Also is a carcinogen
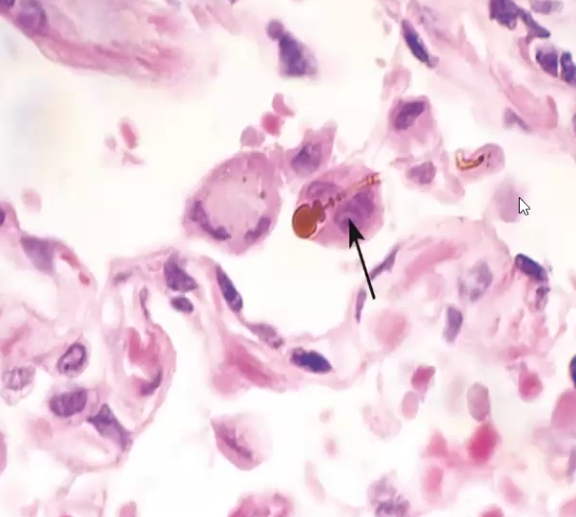
Diffused pulmonary interstitial fibrosis, asbestos bodies histologically that look like golden brown beaded rods with knobbed ends, pleural plaques, Dyspnea worsening, mesothelioma linked
Sarcoidosis
Defined as
Cause
Clinical Features
Systemic Disease
Unknown Etiology, said to be caused by dysregulated T cell response to the environment, viruses, bacteria, etc.
Bilateral hilar lymphadenopathy, non-caseating granulomas in multiple organs, giant cells can be seen on microscope within the epithelioid granulomas → dyspnea, diffuse interstitial fibrosis and pulmonary hypertension, hypercalcemia and hypercalciuria, Langerhans cells have asteroid bodies
Pneumonia
Defined as
Predisposing Factors
Two main anatomic patterns of bacterial pneumonia
Routes of Infection
Broad term for infection in the lung/s
Predisposing factors include, pre-existing lung diseases, defects in immunity, loss of cough reflex/mucociliary apparatus, accumulation of secretions, things are easily inhaled
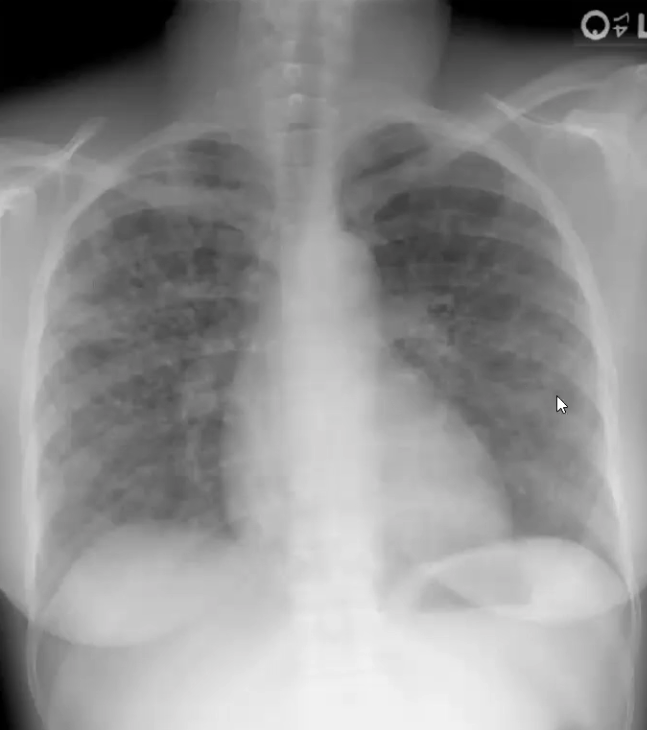
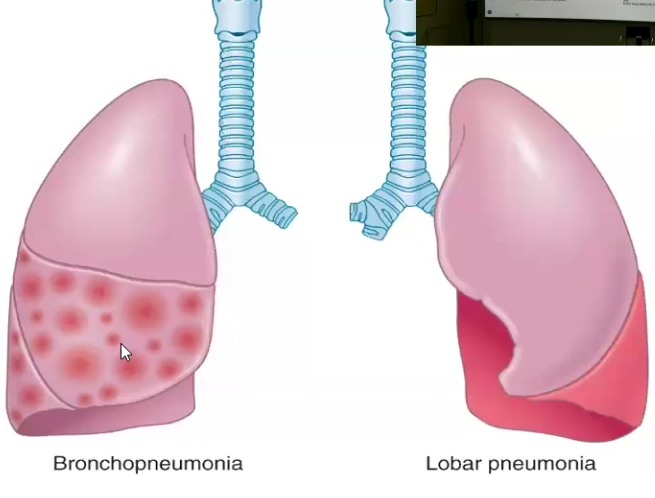
Bronchopneumonia (consolidation in patchy consistency) and Lobar (Consolidation of entire lobe)
Aspiration, Inhalation, Hematogenous
Community-acquired, Nosocomial, Opportunistic
Community-Acquired Bacterial Pneumonias
Describe each
Describe Clinical features of them as a group
Strep pneumoniae: most common cause of community-acquired pneumoniae
gram +, diplococci
Staphylococcus aureus: causes secondary pneumonia after viral respiratory illnesses
High incidence of lung abscess and empyema (pockets of pus)
Severe necrotizing pneumonia and infective endocarditis
Klebsiella pneumoniae
gram -
Affects debilitated and malnourished individuals, particularly chronic alcoholics
Thick gelatinous sputum, empyema
Legionella pneumophila
gram -
Causes Legionnaire disease and Pontiac fever (self limited U res tract infection)
Thrives in aquatic environments and spreads through aerosol
Clinical features: fever, chills, cough and sputum, pleuritis, abcess formation, empyema, bacteremia
Viral Pneumonias
Causes
Affects
Caused by Influenza types A and B → or any of the ones causing common colds
Affects immunocompromised such as children and elderly
Clinical Features: alveolar edema and fibrosis, affected areas are red-blue and congested, interstitial inflammation, may not include cough, fever, headache, myalgia
Tuberculosis
Defined as
Causes
Pathogenesis
Clinical Features
Communicable chronic granulomatous disease
Mycobacterium tuberculosis, an acid-fast bacilli
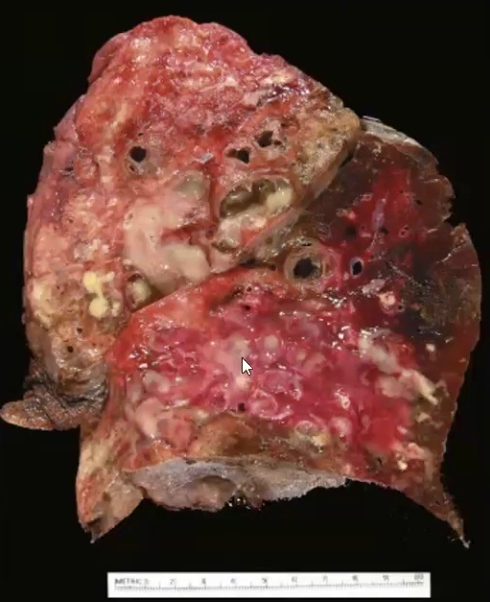
Triggers cell-mediated immunity after inhalation. Enters macrophages and proliferate, causing bacteremia, most times it can be resolved by Th1 cells
Caseating granulomas and cavitation
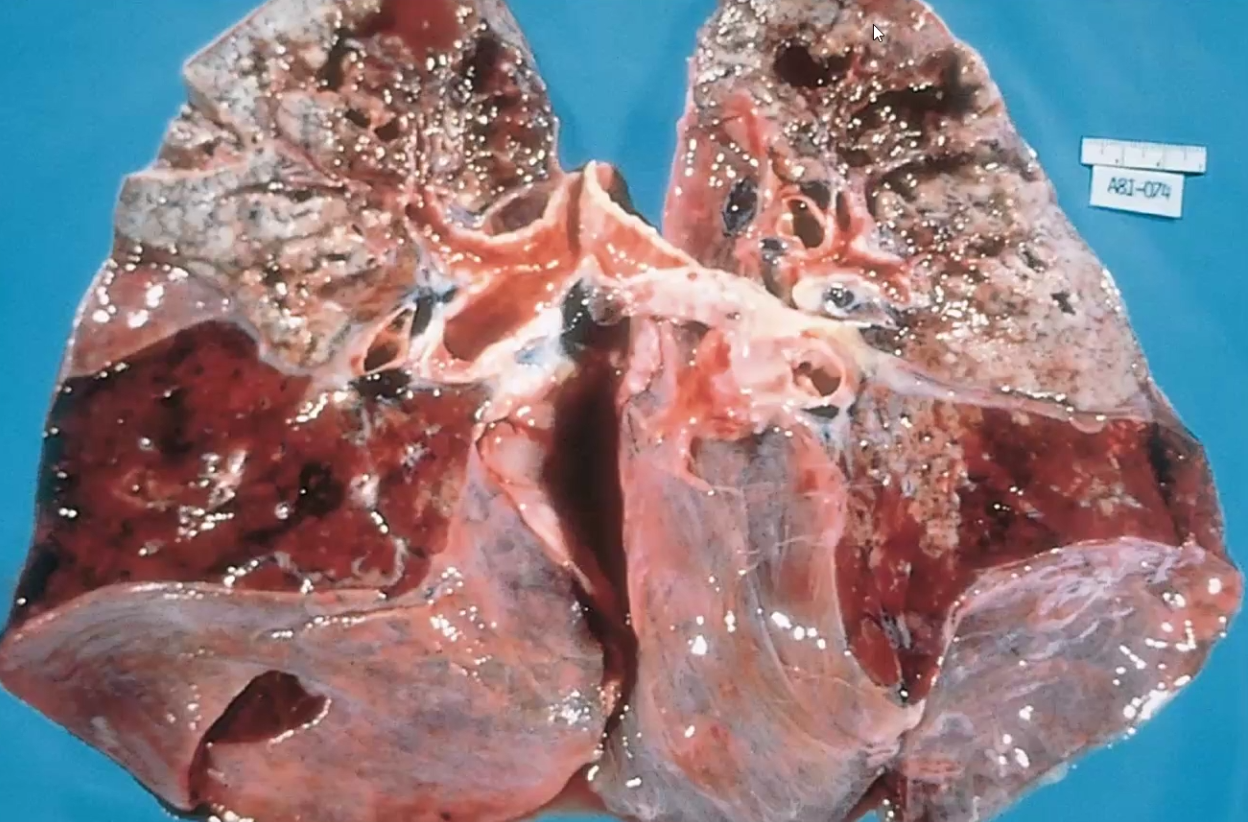
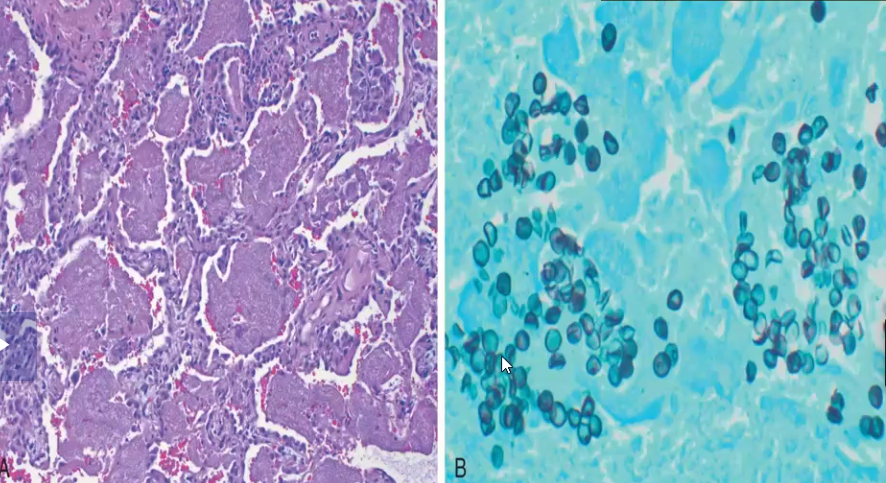
Opportunistic Fungal Pneumonia
Occurs in what kind of patient
Cause
Characteristics
Occurs in AIDS patients because they are very vulnerable
Caused by Pneumocystis jirovecii
Characterized by pink frothy intraalveolar exudate and rounded-to-cup-shaped cysts with a central dimple → seen using silver stain
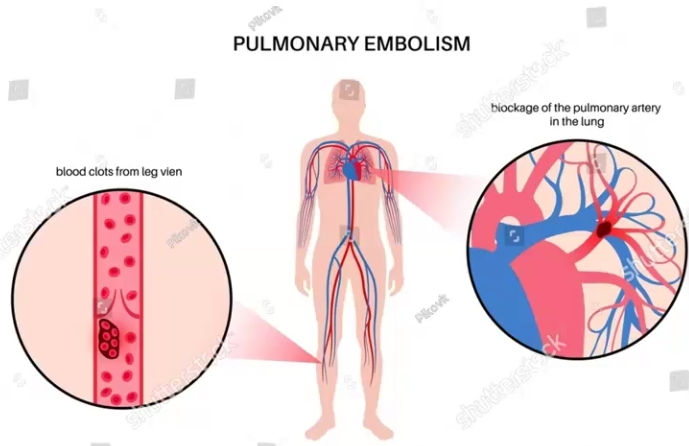
Pulmonary Embolism (PE)
Defined as
Pathophysiology
Clinical Features
Defined by thrombi that occludes the large pulmonary arteries
Causes pulmonary hypertension and ischemia of downstream pulmonary parenchyma
Most embolisms are clinically silent
Some are non-thrombotic, that means the blockage is not caused by blood, but by other things such as amniotic fluid, fat/marrow, foreign bodies and air
May result in right heart failure or shock/death
Pulmonary Edema
Defined as
Causes
Clinical Consequences
Symptoms
Fluid accumulation in alveolar spaces that reduces gas exchange
Causes include increased hydrostatic pressure, decreased osmotic pressure, lymphatic obstruction
Clinical Consequences include hypoxia, hypercapnia
Symptoms include dyspnea, cough, fluid retention, orthopnea
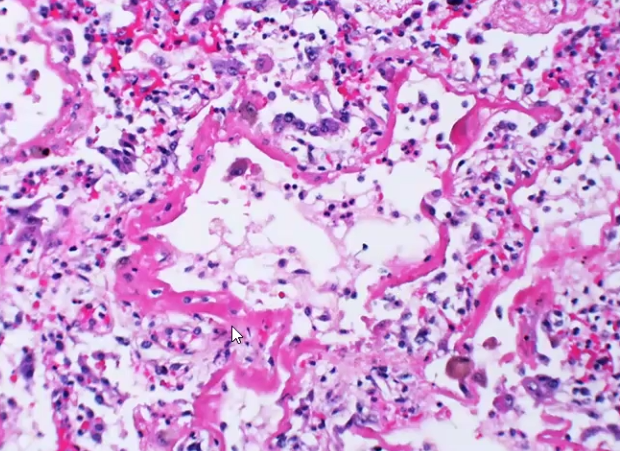
Acute Respiratory Distress Syndrome (ARDS)
Define
Causes
Pathophysiology
Clinical Features
Respiratory failure due to injury to alveolar epithelial and capillary endothelial cells
Causes include viral or bacterial responses, shock, trauma, drugs, etc
Pathophysiology:
Acute Phase: destruction of type I and some type 2 pneumocytes, edema, hyaline membrane forms
Organizing Phase: increase in reactive type 2 pneumocytes, resorption of hyaline membrane and thickening of alveolar septum by fibroblasts
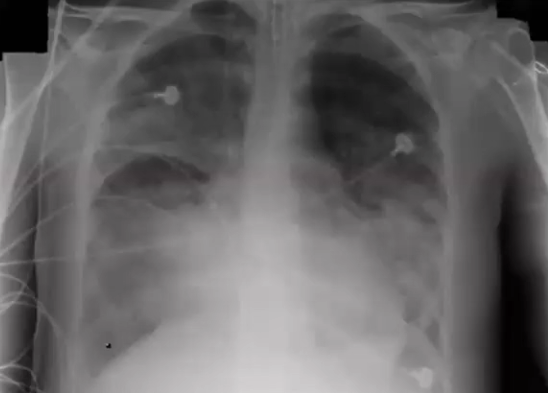
Hypoxemia (fibrosis and edema impair oxygen exchange) and bilateral pulmonary infiltrates, diffuse alveolar damage (both lungs show “white out” on x-ray), presence of hyaline membrane
Neonatal Respiratory Distress Syndrome
Define
Causes
Clinical Features
Respiratory Failure in Newborn
Caused by immaturity of the surfactant system in preterm babies
Hyaline membrane, “white out” in both lungs on x-ray, collapsed lungs and inadequate gas exchange, tachypnea, cyanosis
Non-small cell carcinoma vs. Small-cell carcinoma
Non-small: slow spreading and includes adenocarcinoma, squamous cell carcinoma and large cell carcinoma
Small cell carcinoma: very aggressive and fast growing
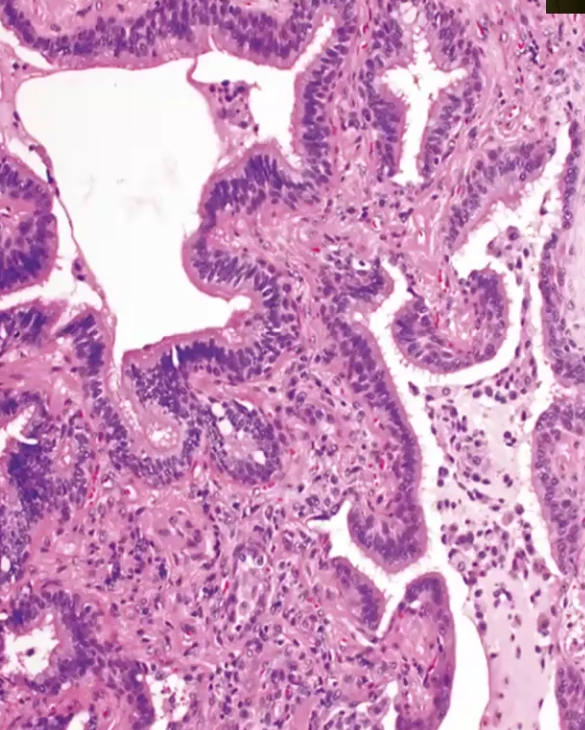
Primary Lung Adenocarcinoma and Primary Lung Squamous Carcinoma
Common in
Location
Characteristics
Adenocarcinoma
Most common type in women and non-smokers
Located peripherally
Slow growing but metastases at an early stage
Squamous
Same exact thing except it is centrally located
Large Cell Carcinoma
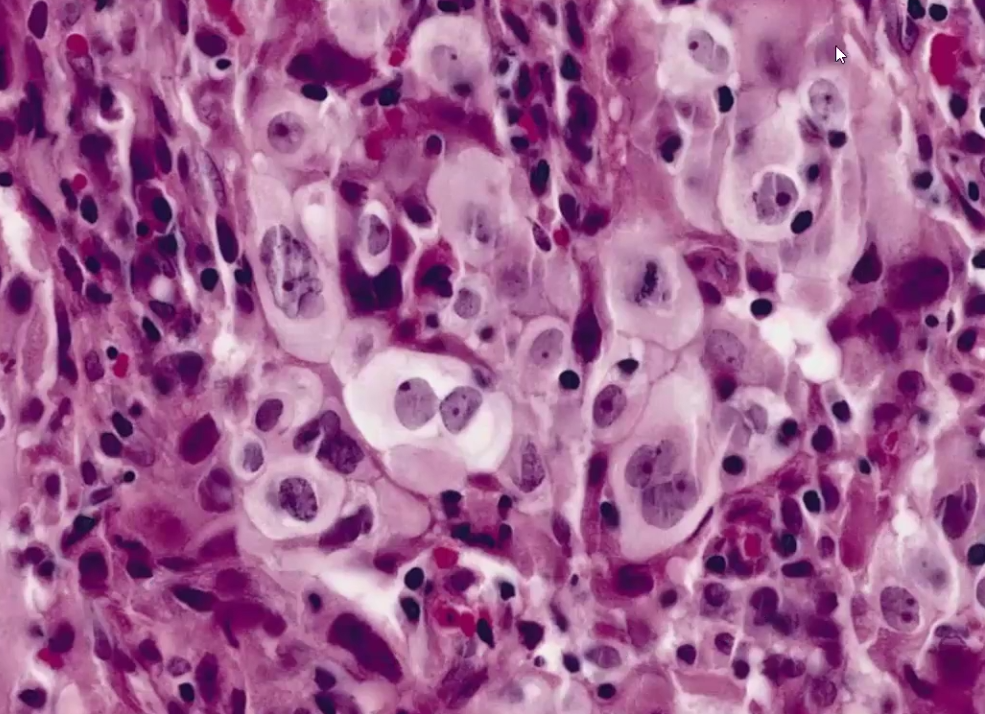
Undifferentiated epithelial tumors with no microscopic features allowing classification into any other category
Small cell Carcinoma
Location
Characteristics
Centrally located
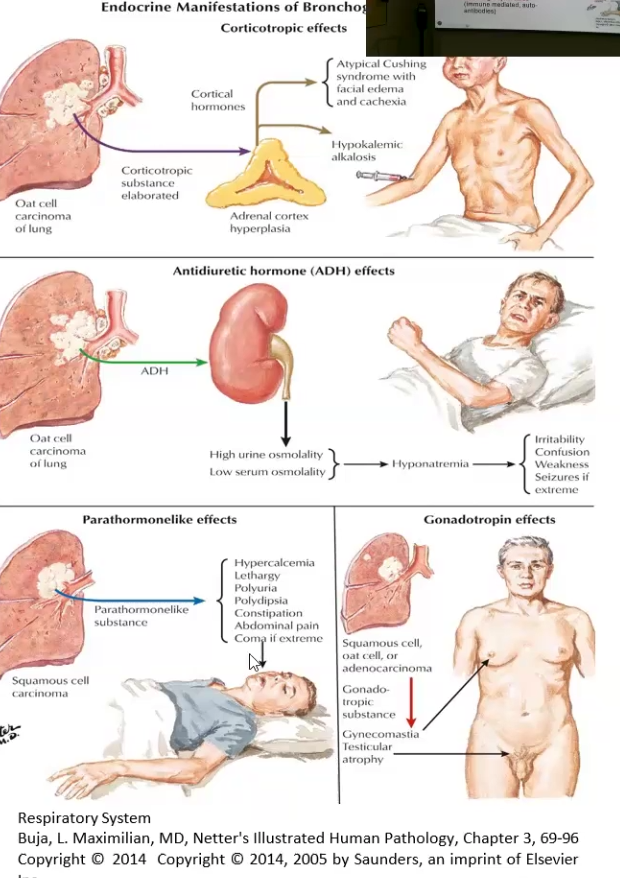
Small tumor cells, very aggressive and fast growing, may secrete hormones, unlike the other, it needs systemic therapy
Carcinoid Tumor
Location
Characteristics
Most originate in the main bronchi
Low grade neuroendocrine tumor, resectable and curable, carcinoid syndrome may occur (intermittent diarrhea, flushing and cyanosis)
Lung Cancer Related Phenomena
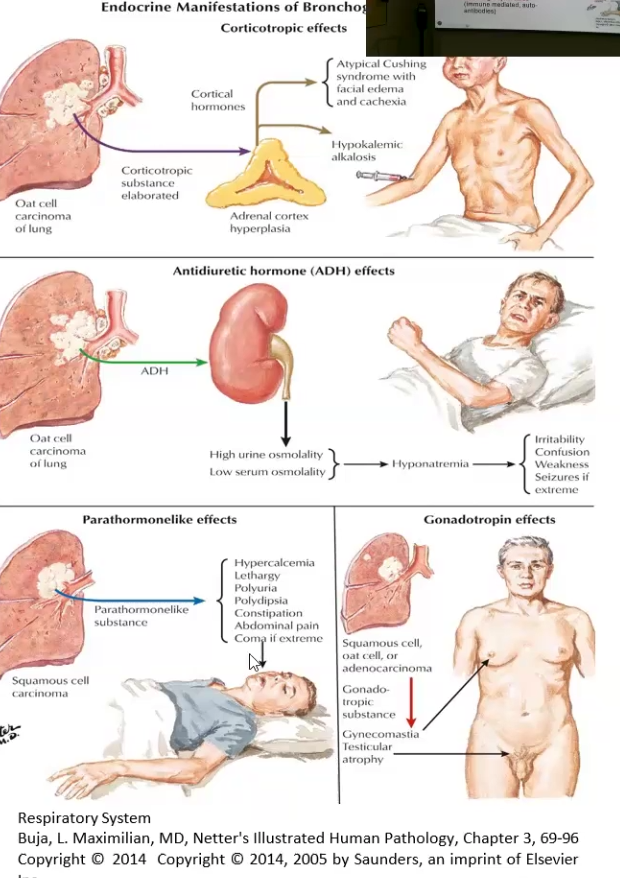
Paraneoplastic syndrome: remote effects such as hypercalcemia, ADH abnormal secretion, Corticotropic effects (cushing’s), neurologic syndromes
Pancoast Syndrome: tumor in apical segment of upper lung lobe compresses recurrent laryngeal nerve (hoarseness) and cervical plexus
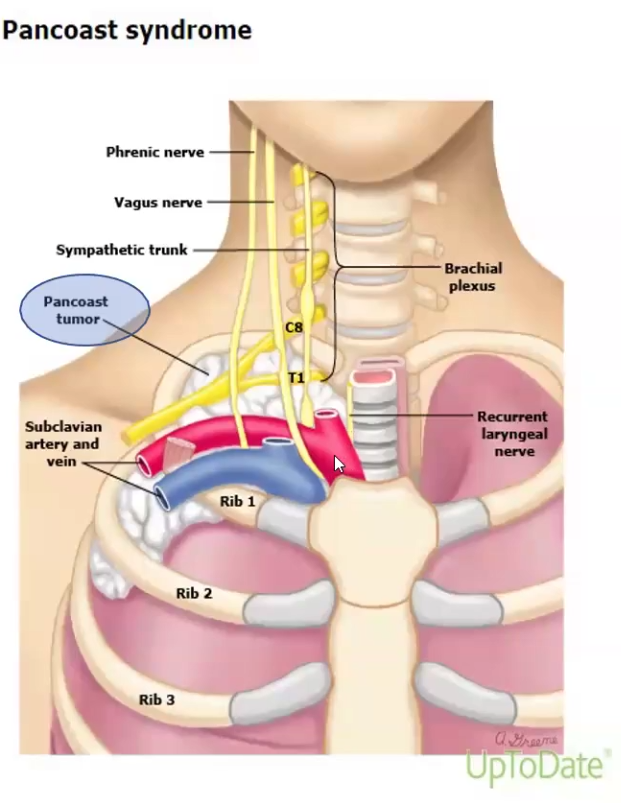
Horner Syndrome: tumor in apical segment of upper lung lobe compresses cervical sympathetic plexus and leads to miosis, ptosis, anhidrosis
Lung Cancer Clinical Features
Most patients with symptoms already have advanced disease and metastasis
Cough, hemoptysis, dyspnea, chest pain
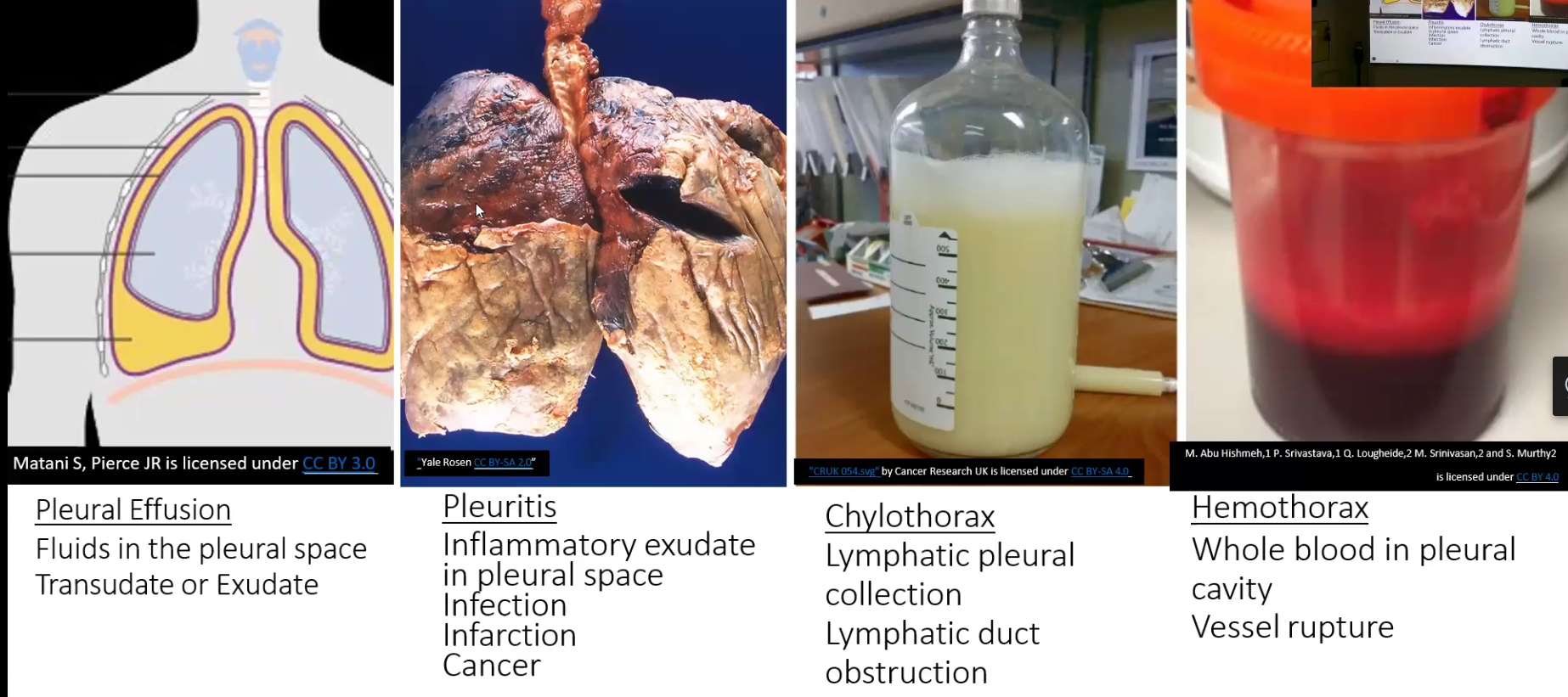
Pleural effusion
Two types
Transudate: thin, watery with few cells/proteins, causes hydrothorax, most commonly caused by congestive heart failure
Exudate: protein content is high and contains inflammatory cells, suggests pleuritis (inflammation of pleura)
Malignant Mesothelioma
Strongly associated with asbestos exposure (80-90%)
Has a long latent period of 25 to 40 years
Preceded by pleural fibrosis and plaque formation