Obesity, DM, Smoking, and other system effects on the CP system
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
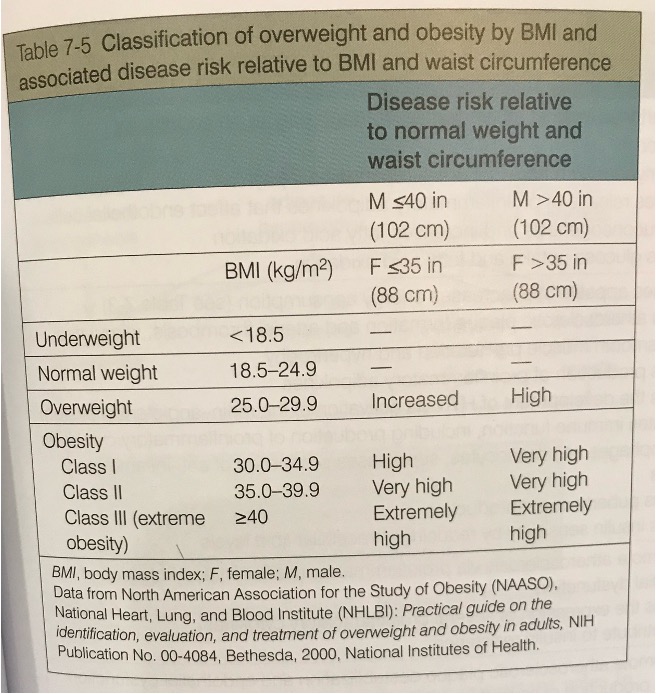
Obesity - BMI
-Obese: > 30kg/m2
-Overweight: 25.0-29.9 kg/m2
-Normal: 18.5-24.9 kg/m2
-Underweight: < 18.5 kg/m2
BMI not always an accurate portrayal of a patients health atatus
-Calculation of BMI: [(weight in lbs)/(height in inches)2] x 703
The cause of obesity
-Diet (increase in high-fat, high-sugar foods)
-Genetics
-Hormonal: affects energy expenditure and rate of metabolism
-Decreased activity level: sedentary lifestyle
-Medication: antidepressants, antispychotics, steroid hormones,antidiabetic drugs
-Metabolic medical conditions: hypothyroidism, Cushing syndrome, growth hormone deficiency
Health hazards of obesity
-Obesity is associated with GI diseases (GERD, gallstones, nonalcoholic fatty liver) and increased incidence of breast, colon, prostate cancers (unknown reason)
-Increased BMI, along with increased waist circumference, is directly related to the incidence of cardiovascular disease
Classification of overweight and obesity by BMI and waist circumference (chart)
Obesity is associated with the following:
-HTN
-Dyslipidemia (inc triglycerides, dec HDL cholesterol, increased LDL)
-DMII
-CAD
-Left ventricular dysfunction/heart failure
-Cardiomegaly
-Obstructive sleep apnea hypopnea syndrome (OSAHS)
-Orthopedic probs
-Decreased endurance
-Sedentary lifestyle
Obstructive sleep apnea
-5 or more episodes of disordered breathing lasting for at least 10 seconds per hour of sleep, in adults
-Hypopnea: temporary reduction of respiratory flow of at least 50%
-Apnea: complete absense of airflow
-Obesity is the strongest risk factor: excessive adipose accumulation in the neck results in pharyngeal narrowing
-Snoring or choking sounds are common
Pathophysiology of obstructive sleep apnea
-Apnea periods marked by impaired gas exchange
-Results in hypoxemia and hypercapnia
-Increases sympathetic nervous system tone
Obesity hypoventilation syndrome
-obesity combined with sleep disordered breathing and chronic daytime alveolar hypoventilation
-imbalance between ventilatory drive and ventilatory load
-increased at nigh in supin position
-causes hypoventilation, cyanosis, daytime somnolence, chronic hypoxemia, hypercapnia, respiratory acidosis, polycythemia (polycythemia: hematocrit and or hemoglobin concentrations are inc in blood)
-Hypercapnia can leaf to CO2 narcosis
-Hypoxemia and hypercapnia stimulate pulmonary artery vasoconstriction→ pulmonary HTN → Cor-pulmonale
Location of adipose tissue
-Substantial evidence indicates that abdominal (central) obesity, particularly intraabdominal or visceral adiposity is a better predictor of CVD and DM II when compared to BMI
→visceral adipose tissue associated with increased release of fatty acids which enter the circulation and may become deposited as ectopic fat in the liver, heart, skeletal muscle, and pancreas (ultimately induce insulin resistance)
→Conversely, the accumulation of adipose tissue in the gluteal-femoral areas is not associated with increased CVD risk
Tx of obesity
-Diet, increased physical activity, behavioral modifications, psychological counseling
-Bariatric surgery
-CPAP/BiPAP
-Rapid extreme weight loss is not healthy due to metabolic changes occurring
Exercise and obesity
-Exercise capacity is resuded
-Higher RR, HR, minute ventilation (V subscript E) and absolute oxygen consumption (VO2) at any given workload
-Dyspnea on exertion (DOE)
-Exercise training offers several benefits, even if weight is not lost
→Decreased BP
→Decreased insulin resistance
-Increased psychological well being
0Enhanced cardiorespiratory fitness
-Decrease abdominal fat
-Prevention of further weight gain
Losing weight
-A caloric deficit of 3,500 cal is required to lose 1 lb
-Reducing caloric intake by 500 cal/day would result in 1 lb weight loss in one week (500 × 7 =3,500)
-There are many websites that calculate the amount of caloric intake required/day for each individual (age, height, weight, activity level)
Metabolic syndrome
-Found in 1/3 of the adult population in the united states
-refers to a cluster of interrelated risk factors
→increased waist circumference
→elevated triglycerides, or on medication
→reduced HDLs or on meds
→HTN or on meds
→Elevated fasting glucose or on meds
DM
-Metabolic disease characterized by hyperglycemia: results from defects in insulin production, insulin action, or both
-The major role of insulin is to control glucose levels after eating a meal. A deficiency of insulin or resistance to it will lead to increased blood glucose levels
-An increase in blood glucose will eventually lead to damage to blood vessels, heart, kidneys, eyes, and peripheral nerves
DM 4 types
-DM I: insulin-dependent. auto-immune destruction of B-cells in the pancreas, resulting in a complete lack of insulin secretion.
-DM II: non-insulin dependent. progressive decline in B-cell function overtime (90-95% of DM cases)
-Gestational DM: develops during pregnancy and almost always resolves after parturition: studies show that women with gestational DM have a 40% to 60% risk of developing DM II in next 5-10 years
-Secondary DM: cystic fibrosis, hormonal syndromes, pancreatic disease, meds, etc
Macrovascular changes from DM
-PVD, CVA, CAD
Microvascular changes from DM
-Retinopathy, nephropathy
Signs of DM
-Polyuria
-Polydipsia
-Diabetic ketoacidosis
→very serious condition
→can develop quickly and lead to coma or death in a few hours time
→manifested by by marked hyperglycemia, nausea and vomiting, polydipsia, polyuria, abdominal pain, fruity-scented (ketotic) breath, dry skin, dry mouth, weakness, fatigue, rapid and deep breathing
-Respiratory problems associated with ketoacidosis: pneumomediastinum, hyperventilation, mucus plugging, pleuritic chest pain, pulmonary edema
*Hyperglycemia and insulin resistance accelerate the development of atherosclerosis
Diabetes and exercise
-Physical activity causes a reduction in insulin secretion and enhanced secretion of glucagon, resulting in hepatic glucose production, so there is adequate fuel to feed working muscle
-Reduced insulin production is compensated for by a heightened sensitivity and responsiveness of peripheral tissues to insulin, to allow for a rapid uptake of glucose: this rapid uptake of glucose draws the glucose from the blood into the working muscles, thus decreasing blood glucose
DM I Hypoglycemia
-confusion, dixxiness, feeling shaky, hunger, HAs, irritability, pounding heart, sweating, anxiety, weakness
DM I hyperglycemia
-restlessness, polyuria, polydipsia, fatigue, polyphagia, blurred vision, dry skin, dry mouth
Treatment of DM
-Major goal is to control glucose levels in the blood and avoid long-term damage
-Monitoring of blood glucose leves is recommened before, after, and several hours after new patterns of exercise are undertaken, at least until the glycemic response can be predicted
→measurements should be taken 60 minutes and 30 minutes before exercise to identify the trend of blood glucose (based on the trend, it will be clear whether the patient is likely to require adjustments in glucose or insulin to avoid hypoglycemia or hyperglycemia)
→ Measurements of blood glucose should also be taken every two hours after exercise to avoid late-onset hypoglycemia
Exercise and DM - when BG levels are elevated before PT
-If BG levels are 250-300 mg/dL and the patient is using insulin, she/he should check for ketosis (via urine stick or BG meter that measures ketone)
→if not ketones detected, the BG is stable or falling. If the individual feels good and is well hydrated, low to moderate exercise is indicated for 10-15 minutes, followed by a re-check of BG
→ After the exercise, if the BG has risen, exercise should be terminated. If the BG has dropped, exercise can be continued for another 10-15 min, again checking the BG after
Exercise and DM - when BG levels are low before PT
-If BG values are low (<70 mg/dL), the individual should eat a carbohydrate snack and wait 20-30 minutes to re-check BG levels. If the BG level has risen to appropriate levels, then mild-to-moderate exercise is warranted for 10-15 minutes, checking BG levels are each 10-15 minute interval of exercise
→If BG has not risen after the carbohydrate snack, exercise is contraindicated
-Because BG levels can change quickly, it is important for a PT to watch for S&S during tx: to reduce hypoglycemia, diabetics should avoid injecting insulin near the exercising muscles- abdomen or arm recommended
HbA1C
-Used to assess whether or not DM is controlled
-Measures average blood sugar levels over the last three months
-Normal 2.5-6%
-Goal for DM is to be < 7%
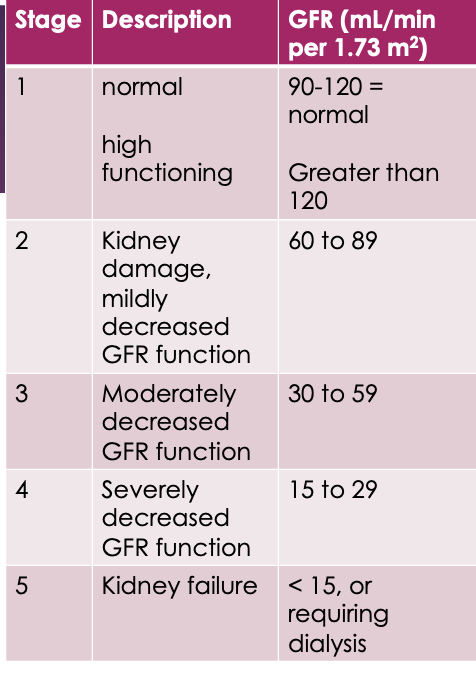
Chronic Kidney disease and failure
-the function of the kidneys is to control extracellular fluid volume, regulate electrolytes balance, regulate acid-base balance, along with secreting hormones
-Glomerular Filtration Rate: impairment with this results in renal dysfunction or failure: Normal GFR: 90-120 mL/min per 1.73 m2
-Risk factors for CKS include HTN, DM, CVD, obesity, glomerulonephritis, lupus, polycystic kidney disease, overuse of aspirin, ibuprofen, acetaminophen, and cocaine
CKD staged
Tx of CKD
-The primary goal is to slow down the progression of the disease: medications, diet, lifestyle changes
-With kidney failure, the tx is hemodialysis
→dialysis is a process that replaces the excretory function of the kidneys through the use of a semipermeable membrane and rinsing solution (dialysate) to filter out toxic waste from the blood
→dialysis also controls the fluid imbalances; however does not control the endocrine functions, which the kidneys are responsible for: could lead to anemia, thromboses, pericarditis, and ascites
-In standard hemodialysis, pts go to an outpatient center 3x/week. eah tx takes about 3-4 hours. the same is used for patients who are hospitalized (inpatient)
→patients do well on dialysis for about 10 years or so (according to research): depending on the patient’s age, a kidney transplant may be best for ESRD
Continuous renal replacement therapy (CRRT)
-Benefit: removing water and waste for patients who are hemodynamically unstable for abrupt removal from dialysis
-Blood is removed from the A-line, cleaned/filtered, and returned through the venous line
Exercise and ESRD
-in most patients with ESRD, exercise capacity is reduced to approximately 50-60% of normal
-patients who have ESRD are likely to have diabetic neuropathy, thus effecting balance and sensation to the LE
-Patients with CKD often have skeletal muscle fatigue and notable skeletal muscle atrophy
→impaired protein synthesis and impaired amino acid metabolism (patients with CKD should be placed on a higher protein diet, secondary to losing protein via urination)
Renal failure, aka acute kidney failure
-Sudden and often loss of kidney function
-Function of kidneys: filter blood, remove waste; maintain body‘s salt and water balance; regulate BP; RBC production
-Three causes
→pre-renal: problem is before kidneys (HF, liver failure, shock, etc)
→Renal: damage to kidney itself (renal cancer, renal infection, meds, nephrotoxins [drugs])
→Post renal: obstruction of flow of urine (prostate cancer, urinary tract cancer, pelvic/abdominal CA)
Renal failure, continued
-Tx is directed at mainlining BP, flow of blood to the kidneys, removal of waste, and balancing water-sodium
-If damage is irreversible, then patient may need permanent dialysis or kidney transplant
-S&S of acute failure: weakness, SOB, lethargy, swelling, confusion: potassium imbalance from sodium-water imbalance can lead to cardiac arrhythmias and sudden death
-Dx: blood tests: BUN, creatinine, GFR
-Controlling BP and DM is the main goal in prevention
-No matter what, kidney function decreases as we age
Cardiorenal Disease
-Worsening heart function leading to kidney injury and vice versa
5-types
-Type 1: a rapid decline in heart function leads to an acute decrease in kidney function (most common) (bc MI)
-Type 2: chronic heart problems result in a continued reduction in kidney function
-Type 3: a rapid decline in kidney function causes an acute reduction in heart function
-Type 4: chronic decline in kidney function results in long-term heart problems
-Type 5: systemic diseases, such as lupus, diabetes or sepsis, cause heart and kidney failure
Renal failure and anemia
-Anemia may occur in patients with renal failure; here’s how:
-Healthy kidneys produce a hormone called erythropoietin (EPO)
-EPO prompts the bone marrow to make RBC’s which carry O2 throughout the body
-Anemia is most present when a patient has 20-50% of normal kidney function
-Anemia tends to worsen as CKD worsens
-Other common causes for anemia in patients with kidney disease include loss of blood from hemodialysis and low levels of the following nutrients found in food (iron, vitamin B12, folic acid; all imporant nutrients necessary for RBCs to make hemoglobin)
Pre-renal syndrome (type ! and II cardiorenal disease)
-BUN is a waste product filtered out of the blood by the kidneys: BUN value increases with pre-renal syndrome or any type of kidney failure
-Creatinine is a waste product in the muscles and is filtered out of the blood by the kidneys: value increases with pre-renal syndrome/kidney failure
-GFR is the amount of blood that is filtered by the glomeruli per minute: value decreases secondary to kidney failure
3 things know: BUN increases, creatinine increases, GFR decreases
-classic signs of CHF seen during this (BUN and creatinine increases; GFR decreases)
-changes in BNP values seen during this pre-renal syndrome (BNP increases when heart stretched): normal < 100; compensated chronic HF 100-500 ; uncompensated chronic HF > 500
Autoimmune Rheumatic Diseases (ARD)
-systemic disease characterized by inflammatory abnormalities which affect joints, muscle, and connective tissues
-can affect all pulmonary and cardiovascular structures (respiratory muscles, pleura, small airways, endocardium, myocardium, coronary arteries, etc.)
-Most common manifestation is pericarditis
→ involvement of the pericardium can induce dysrhythmias, pericardial effusion, and pericardial thickening
Connective tissue - Rheumatoid arthritis (RA)
-Type of ARD
-Most prevalent pulmonary complication is pleural effusions (40-70% of pts)
Connective tissue - Systemic Lupus erythematosus (SLE)
-Type of ARD
-Inflammation of all serous membranes (skin, joints, brain, heart)
-Cardiovascular disease is the most common caue of death
-Classic characteristic is a "butterfly rash"
Connective tissue - Scleroderma
-Type of ARD
-Produced slowly progressive fibrosis and vascular obliteration of the skin, subcutaneous tissues, and often visceral organs
-Known for its pulmonary complications, which is the leading cause of morbidity
Neurologic - Postural Orthostats Tachycardia Syndrome (POTS)
-Form of dysautonomia, a disorder of the autonomic nervous system
-Frequently occurs when standing upright, more occurrence in morning
-Characterized by HR increase from horizontal to standing of at least 30 bpm in adults or 40 bpm in adolescents, during the first ten minutes of standing: does not always accompany changes in BP like OH
—S&S: lightheadedness, fainting, difficulty thinking or concentrating, fatigue, exercise intolerance, HA, blurred vision, palpitations, nausea
-Not fully understood, however, more common in women (5:1 women:men)
-Likely to develop in adolescents and young adults
Hematologic - Sickle Cell Disease
-characterized by structurally abnormal hemoglobin that causes RBC to become less pliable and some, crescent shaped, thus causing an inability to carry O2
Hematologic - Anemia
-reduced amount of circulating RBC: hemoglobin is a protein inside a RBC that transports O2
Vascular pathology that are ARTERIAL in nature
-popliteal entrapment syndrome
-raynaud’s phenomenom
-Buerger’s disease
-Fibromuscular dysplasia (FMD)
Vascular - Popliteal entrapment syndrome
-Rare vascular disease that affects the legs of some young athletes. The muscle and tendons near the knee compress the popliteal artery, restricting blood flow to the lower leg and possibly damaging the artery
-S&S: leg and foot cramps, N/T, discoloration
Vascular - Raynoud’s phenomenon
-Consists of spasms of the small arteries in your fingers, and sometimes toes, from exposure to cold or stress
-S&S: fingers and toes look red, blue, or white, throbbing, tingling, redness
Vascular - Buerger’s disease
-most commonly affects the small and medium-sized arteries, veins, and nerves
-Idiopathic; strong association with tobacco use or exposure
-Arteries of your arms and legs become narrowed or blocked, causing a lack of blood supply (ischemia) to your fingers, hands, toes, and feet.
-With severe blockages, the tissues may die (gangrene), making it necessary to amputate affected fingers and toes. Superficial vein inflammation and symptoms of Raynaud’s can occur as well
-S&S: pain in your arms, hands, legs, and feet, even at rest. blue or pale finger or toes
Vascular - Fibromuscular dysplasia (FMD)
-Rare medical condition
-Abnormal cellular growth in the walls of the medium and large arteries; can cause the arteries to have abnormal growth to look beaded and become narrow (aneurysms and dissection)
-S&S: neck pain, vision changes, high BP, dizziness, hearing a “whooshing sensation” (bruit) or hearing your heartbeat in your ears.
Vascular - Vascular pathologies that are VENOUS in nature
-klippel-Trenaunay Syndrome (KTS)
-May-thurner syndrome (MTS)
-Paget-Schroetter Syndrome
Vascular - Klippel-Trenaunau syndrome (KTS)
-Rare congenital vascular disorder
-Abnormal development of certain blood vessels, soft tissues (skin & muscle), bones, and sometimes the lymphatic system
-Affects the venous system more
-Other notes: red birthmark from pink to reddish purple; most often affects one leg but may occur in an arm or elsewhere; S&S: pain or heaviness in leg/arm
Vascular - May-Thurner syndrome (MTS)
-The right common iliac artery compresses your left common iliac vein, which increases the risk of DVT in the left extremity
-S&S: swelling, TTP, pain in the leg, red or discolored skin
Vascular - Paget-Schroetter syndrome
-AKA axial-subclavian vein thrombosis
-Most common vascular condition to affect young, competitive athletes
-Develops when your clavicle, first rib, or surrounding muscle compresses a vein in your armpit (axilla) or in front of your shoulder (the subclavian vein)
→increases risk of blood clot
-S&S: swelling, heaviness, or pain in the arm or hand, skin that looks blue
Vascular - How to dx vascular pathology
-blood work
-vascular U/S
-catheter angiography
-CT angiography
-MR angiography
Lymphatic- Milroy’s disease
-Idiopathic, rare, often associated with FLT4 gene mutation
-Abnormal development of lymphatic anatomic structures: small or absent lymphatic vessels
-Typically seen at birth or early infancy
-Other features aside from extremity swelling: males: hydrocele (accumulation of fluid in scrotum)
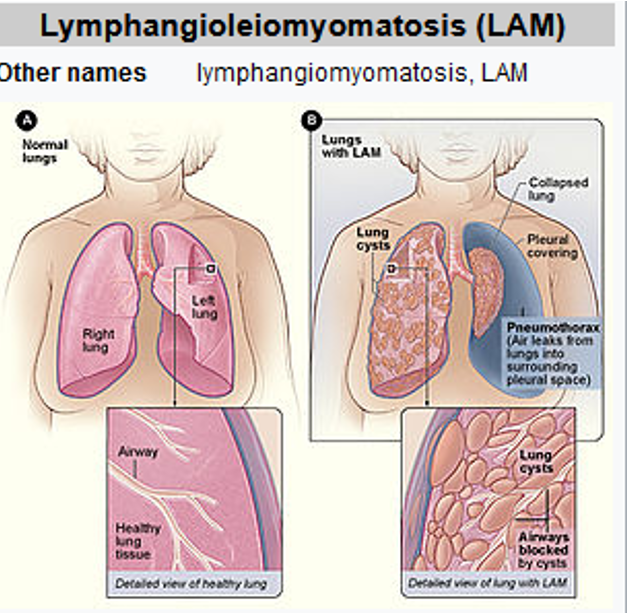
Lymphangioleiomyomatosis (LAM)
-Rare disease that usually affects females in their late 20s, early 30’s
→cause by mutations in tuberous sclerosis complex (TSC) genes: abnormal cells spread to kidneys, lungs, and lymphatic system through blood stream
-Abnormal growth of smooth muscle cell, especially in the lymphatic system, lungs, and kidneys
-No cure, tx to focus on management of sxs
-S&S: SOB, fatigue, and cough
Cigarette smoking
-most common risk factor worldwide contributing to the development of COPD
-Smokers lose lung function as a result of damaged tissue
-Approximately 15% of all deaths related to heart disease are result of smoking cigarettes
-Cigarette smoking has been linked to atherosclerosis
-as few as 4 cigs/day increases risk of developing CAD
-Compared to non-smokers, smokers have been shown to develop low HDL levels and increased BP
Vaping
-POPCORN LUNG
→medical condition that damages bronchioles, causing scarring and narrowing
-Breathing difficulties
-Vaping releases formaldehyde and acetaldehyde
-Causes respiratory distress and lung damage. The additives common in vapes can cause: COPD, acute lung injury, asthma, cancer, bronchiolitis obliterans
-E-cigs are more addicitive because they release more nicotine to the brain faster
-Vaping causes BP to rise. This raises the risk of heart attack, stroke, and heart disease
Types of shock
-Distributive (due to severe peripheral vasodilation: septic shock (infection); anaphylactic shock (allergic run); neurogenic shock (damage to nervous system); drug/toxic shock; endocrine (metabolic ketoacidosis)
-Cardiogenic (due to heart problems): mechanical arrhythmic, cardiomyopathic
-Hypovolemic (too little blood volume): injury/trauma
-Obstructive (blood cannot reach vital organs): tamponade, PE, pneumothorax
-*Combines
Stages of shock
-Injury/infection
-Pre-shcok (compensated)
-Shock (S&S begin to present)
-End organ dysfunction (irreversible without intervention; multi system failure)
-Death
S&S shock
-cool, clammy skin
-pallor or cyanotic skin
-tachycardia
-tachypnea
-nausea/vomiting
-enlarged pupils
-weakness/fatigue
-decreased urine output
-altered mental status
-decreased alertness or LOC
-anxiety
-seizures
-chest pain
-dizziness/fainting
APACHE II
-MD monitoring tool used to predict mortality risk due to shock
-used within first 24 hours of ICU
-score ranges from 0-71
-higher scores indicate increased severity and are associated with a higher risk of death
Elevated serum lactate
-Indicator of shock
-measurements are useful markers for hypoperfusion and indicate a poor prognosis
-Individuals who have MI can go into a state of cardiogenic shock (#! reason for mortality): rising lactate values during resuscitation indicate very high mortality rate
-Normal serum lactate = < 1mmol/L
→>2 mmol/L cause hypotension (heart cannot contract harder even if it wanted to)
→>4 mmol/L consistent with septic shock and associated with poor prognosis (78% mortality rate)
-Rehab implications: if lactate is >4 mmol/L, you should be asking the MD if rehab is a good idea, as the patient has a 78% chance of death