Neurological History Taking
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
69 Terms
What are the three fundamentals of neurological history taking?
Listening is more important than talking
The patient is more important than you
But...listening is not enough you must ask the right questions and be curious
How can you optimise communication in neurological history taking?
Quiet environment, minimise distractions
Is the hearing aid working?
Are you speaking clearly & articulately?
Can the patient see you & your mouth? (masks)
Do you need paper / pen?
(carer?)
How can you optimise communication in a phone or video consultation
• Can you see me/hear me
• Who else is in the room...is that OK?
• Think about appearance & background
- Plain wall best / think about back lighting
• Confirm pt ID
• Document phone / video & reason e.g. covid triage
- Ask and document red flags
• If repeat consultation may need face to face
What are some important observations to make in neurological history taking?
Observations: state of health, mode of dress, age, eye contact, mood, tics, are they clean and tidy/ taking care of themselves?
Content of conversation: level of education, intelligence, mood.
Articulation of speech (dysarthria), dysphasia, slurring their words, does their thought pattern go off on tangents?
Why is it important to ask a patient about their dominant hand?
If they have a unilateral disability and it's on their dominant side they are going to be much more disabled and vice versa.
Almost all right handed people are left hemisphere dominant for language so can be important in diagnosing neurological conditions
The skills for neurological history taking lie in...
Clarifying
Being curious
Sifting & sorting
Analysing the information
Recognising the value of negatives
Observing how things are said, not just listening to what is said
Succinctly documenting the story
What is the presenting complaint
The symptom that has brought the patient to the doctor
How should you record the presenting complaint
Ideally record it in the patient's own words e.g. "dizzy"
But clarify and expand on it. Patients don't always use terminology to mean what you think it means!
What is a common cause of dizziness
Benign positional vertigo
Give an example of a typical history of benign positional vertigo
The dizziness started suddenly when I was in bed and rolled over...
Feels like I am on a roundabout...lasts a couple minutes then settles
OK if I keep my head still but if I look up suddenly it can start again
What are some follow up questions for the presenting complaint?
• Duration of symptoms
• Speed of onset
• Location
• Variation
• Intensity
Give examples of some common neurological presentations
• Altered cognitive ability
• Fits, faints & funny turns
• Headache
• Dizziness
• Weakness or movement disorders
• Numbness or sensory disorders
• Visual impairments
What is a common diagnosis for a PC of increasing difficulty doing up buttons
Parkinsons - issues with fine motor movement
What follow up questions can you ask if someone presenting with difficulty doing up buttons
Have you noticed any changes in your writing?
Any differences in the way you walk?
Some Parkinson's patients also notice a difference in their sense of smell
What origin can fits, faints and funny turns have
Cardiovascular, neurological or possibly endocrine
It's orientation week at the Principal's reception your parents are listening to wise words being spoken. There are no seats and wine is being served. One of the mothers falls to the floor. Is this collapse likely to be of cardiovascular origin, endocrine origin or neurological origin?
Cardiovascular - typical vasovagal faint
In which condition may a history be diagnostic?
Epilepsy
Why can a history be diagnostic for epilepsy
Sodium, glucose, magnesium, urea, neuroimaging and electroencephalogram may all be normal
What is epilepsy?
Abnormal, excessive paroxysmal discharge of
cerebral neurons
What percentage of the population is affected by epilepsy
Approx 1%
What can cause a seizure in a normal healthy person?
Abnormal electrolytes and blood glucose can cause fits in anyone - these can be caused by poor sleep. They cause a decrease in the seizure threshold
What are the best ways to go about diagnosing fits, faints and funny turns?
Good history from patient
A description from witness
If recurrent think of asking to record the event (smartphone)
What questions can you ask about fits?
What was happening immediately before?
What factors might have lowered the seizure
threshold?
What position was the patient in?
Any prodromal symptoms?
What happened during the episode?
After? - did they wake up in an ambulance, on the floor?
What was the last thing they remember?
What questions should you ask about a headache?
• Site - "show me where"
• Radiation - "does it go anywhere else?
• Sort - "what kind of pain"
• Severity
• Timing
• Aggravating & relieving factors
• Associated features (especially nausea)
What questions should you ask about the time course and evolution of symptoms of a headache?
• Sudden e.g. "thunder clap" headache
• Recurrent (but well between episodes)
• Deterioration over hours
• Relapsing / remitting
• Deterioration over weeks/months
What does a headache that deteriorates over hours suggest?
An infection
What does a relapsing/remitting headache suggest?
MS
What does a headache that deteriorates over weeks/months suggest?
Parkinsons
What questions should you ask about weakness?
What does the patient mean... chronic "aesthenia" "fatigue" or specific muscle weakness.
What activities are they finding difficult?
Is the problem in the muscle or in the nerve supply to the muscle?
What does weakness of sudden onset suggest?
Stroke until proven otherwise
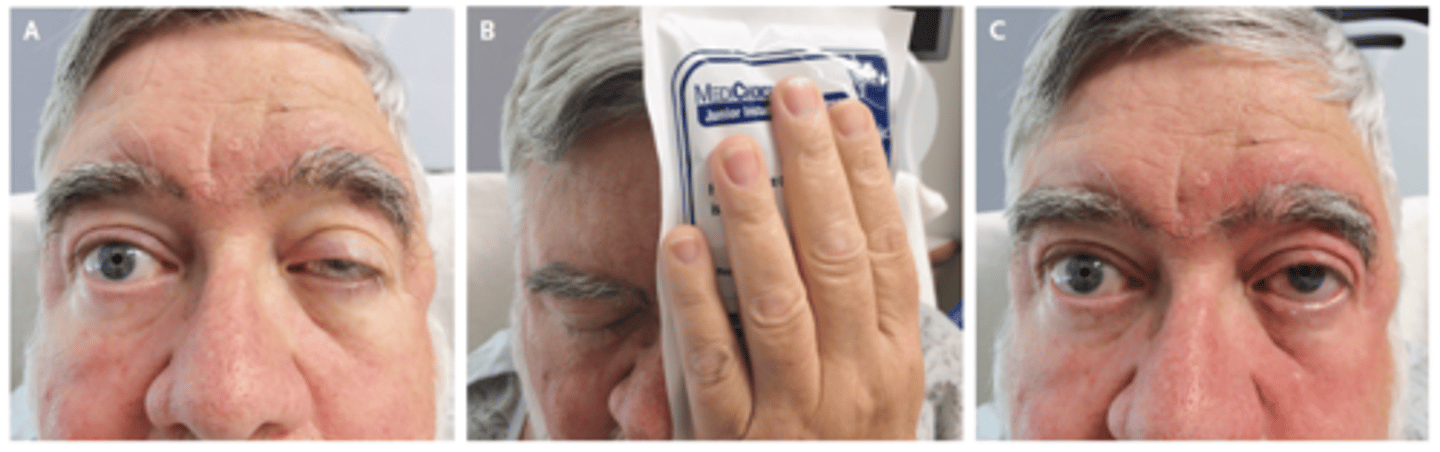
What is the ice pack test?
Compression over ptosis with ice pack - test for myasthenia gravis. Positive if the ptosis improves
Focal weakness suggests
Neurological origin
Give examples of proximal muscle weakness
rising from sitting
drying hair
Give examples of distal muscle weakness
standing on tip toes
fine finger movements
What questions should you ask about walking, in terms of weakness?
• Has the distance they can manage changed?
• Why? What makes them stop?
• What about hills?
• One leg or both legs?
• Any sensory symptoms?
What does too little movement suggest
Parkinson's disease...slowing of movement, stiffness
What is the most common cause of too much movement
Huntingtons chorea
What is choreoathetosis?
Decreased tone...rapid, writhing changes in movement (consider over treatment of PD)
What is paraesthesia?
Abnormal tingling or prickling sensation (caused by damage to peripheral nerves) - "feels like a tight bandage wrapped around my leg"
What is allodynia?
Severe pain sensation evoked with a stimulus that doesn't normally induce pain e.g. brushing against someones skin can cause them intense pain
Complete sensory loss is likely to be of what origin?
Functional origin
A patient complains of "Wake up in the middle of the night with ache and numbness in my thumb and first two fingers" Which nerve is affected?
Median nerve
What chronic illnesses may result in neurological impairment?
Diabetes, sarcoid, TB
What are activities of daily living (ADLs)?
ADL's are the activities required to maintain a daily life existence. They are eating, dressing, transferring, toiling, walking or moving around and bathing
What should you think about when taking a history from a younger patient?
Milestone i.e. Was there any evidence of developmental delay?
What can birth asphyxia/a difficult birth cause?
Cerebral palsy
What are some normal ages for milestones
1 to walk & 2 to talk but can be earlier or later - bum shuffling is very normal
What does regression in a child suggest e.g. started walking or talking but has regressed
ALWAYS abnormal and must be investigated
When do children normally smile first?
6-8 weeks
What questions should you ask about prescribed drugs?
What treatment(s) are they on?
Are they compliant?
Is it optimal?
Allergies?
Could it be the cause of the problem?
Is there any interaction between the drugs?
Is the patient thinking of becoming pregnant?
What are anti-convulsants contra-indicated in?
Pregnancy
What can analgesic overuse cause?
Headaches
What questions should you ask about non-prescribed drugs?
What other drugs are you taking?
How often, how much, how long?
Tell me about your pattern of drinking alcohol
What symptoms do you have if you don't take drugs / drink?
What should you ask about in your systems enquiry?
Psychological...depressed?
Autonomic nervous system...bowel, bladder function, sexual dysfunction, light headedness?
Recent infection?
Why is it important to take a family history for a neurological history
Genetic component to many neurological disorders.
You must ask & document
What should you ask about in a social history?
Who is at home?
Home circumstances
Are home circumstances contributing to medically unexplained symptoms?
Occupational history e.g. bed and bathroom all on one level?
Give examples of cranial nerve screening questions
Change in your sense of smell?
Vision?
Double vision?
Dry eyes?
Dry mouth?
Change in taste?
Hearing?
Dizziness?
Change in voice?
Articulation?
What impact does COVID-19 have on the olfactory nerve
Changes sense of smell - can have lasting damage
How should you document a neurological history?
Not a verbatim record of what the patient has told you
Filtered and critically analysed record
Often important to record negatives
Conclude with a summary, differential diagnosis & action plan
How should you come up with a differential diagnosis in neurology?
The neurological system is logical so think logically!
Age, gender, pattern of onset
Risk factors
Relative incidence...common things are common
Assess probability
What percentage of symptoms are medically unexplained
30%
Why might some people consider further investigations following a history
- To complete a checklist?
- To increase your certainty of diagnosis?
- To exclude important things?
- To reassure you?
- To reassure the patient?
- The results should guide / change management
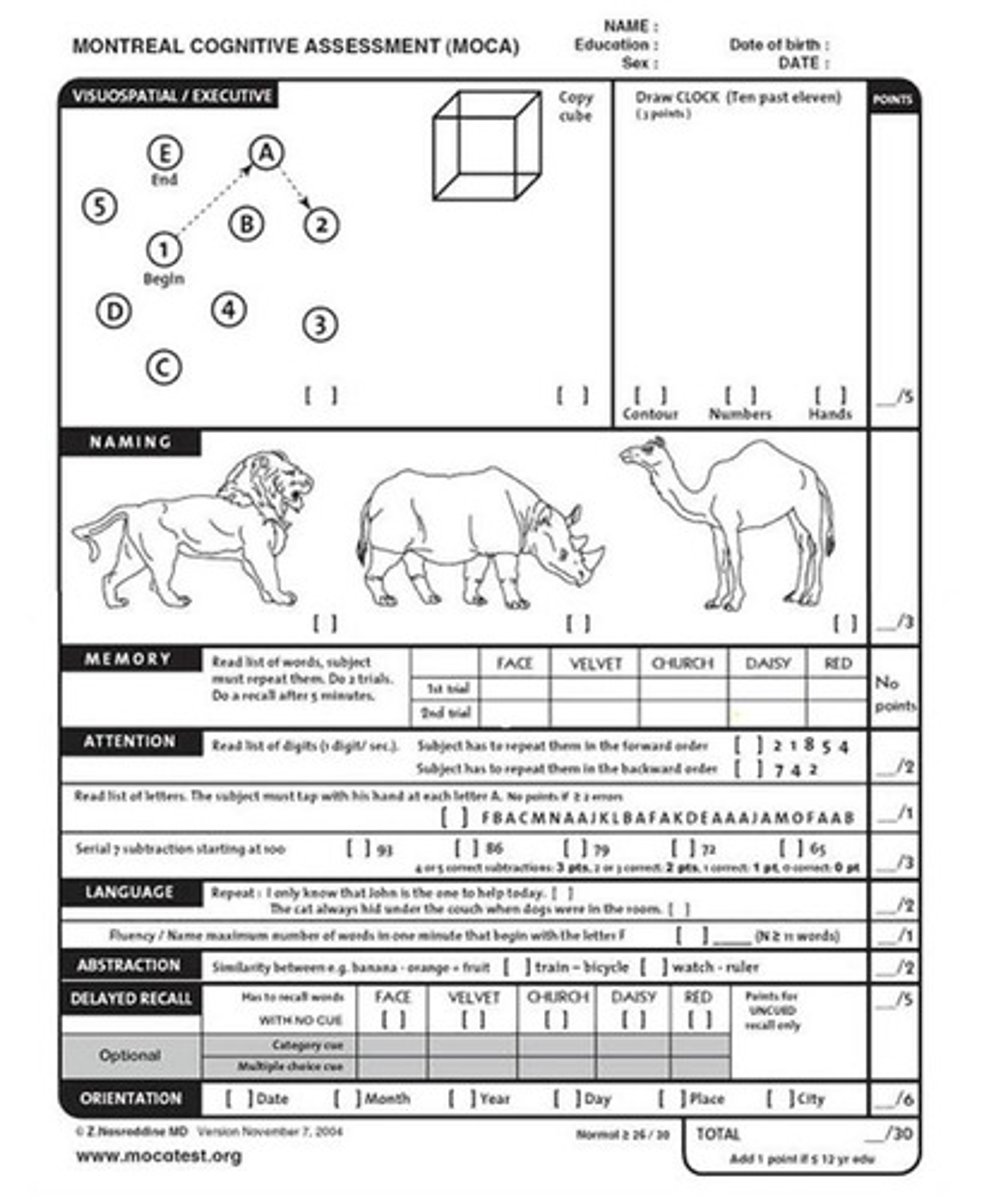
Give examples of assessment tools for cognitive assessment
• 4As test (rapid, initial screen for delirium)
• Mini Mental State Examination (MMSE)
• Montreal Cognitive Assessment (MOCA)
• Addenbrookes Cognitive examination (ACE III)
What is delirium?
• Mental confusion that can happen if someone becomes medically unwell. Can also be called "acute confusional state"
How common is delirium?
Common 1:10 hospital patients
What is the Montreal Cognitive Assessment (MoCA)?
• No copyright!
• Better at identifying mild levels of impairment
• Less bias ethnicity / age/ education
What is the Addenbrookes Cognitive examination (ACE III)
• About 20 minutes to do
• Scored out of 100
• 5 cognitive domains:
- Attention
- Memory
- Verbal fluency
- Language
- Visuospatial abilities
What is confabulation?
Fabricates events to fill in memory gaps
• Great authority, great certainty
• Often autobiographical in nature
• No intent to deceive
What conditions often present with confabulation?
• Korsakoff's syndrome
• Alzheimer's dementia