Parasitology
1/56
Earn XP
Description and Tags
Parasitology
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
What is a Helminth
Parasitic worms
Biohelminths
Heteroxenous (development involves several host species) parasitic worms
Go through host independently of environmental factors
Geohelminths
Monoxenous (development is restricted to a single host species) parasitic worms
maggots become invasive in external env. under strictly defined factors – temp, humidity etc
Types of hosts
Definitive
Intermediate
Paratenic
Reservoir
Accidental
Definitive host
host ADULT parasite lives in
parasite undergoes SEXUAL REPRODUCTION
Intermediate host
host LARVAL STAGE of parasite lives in
ASEXUAL MULTIPLICATION takes place
2 types : 1st and 2nd immediate hosts
Paratenic host
Host in which the parasite STAYS IN LARVAL STAGE (no further development)
Host transmits infection to another host
Reservoir host
Host that harbors the parasite that it transmits to another host in an endemic area (disease constantly present)
Accidental host
Host in which parasite is not usually found
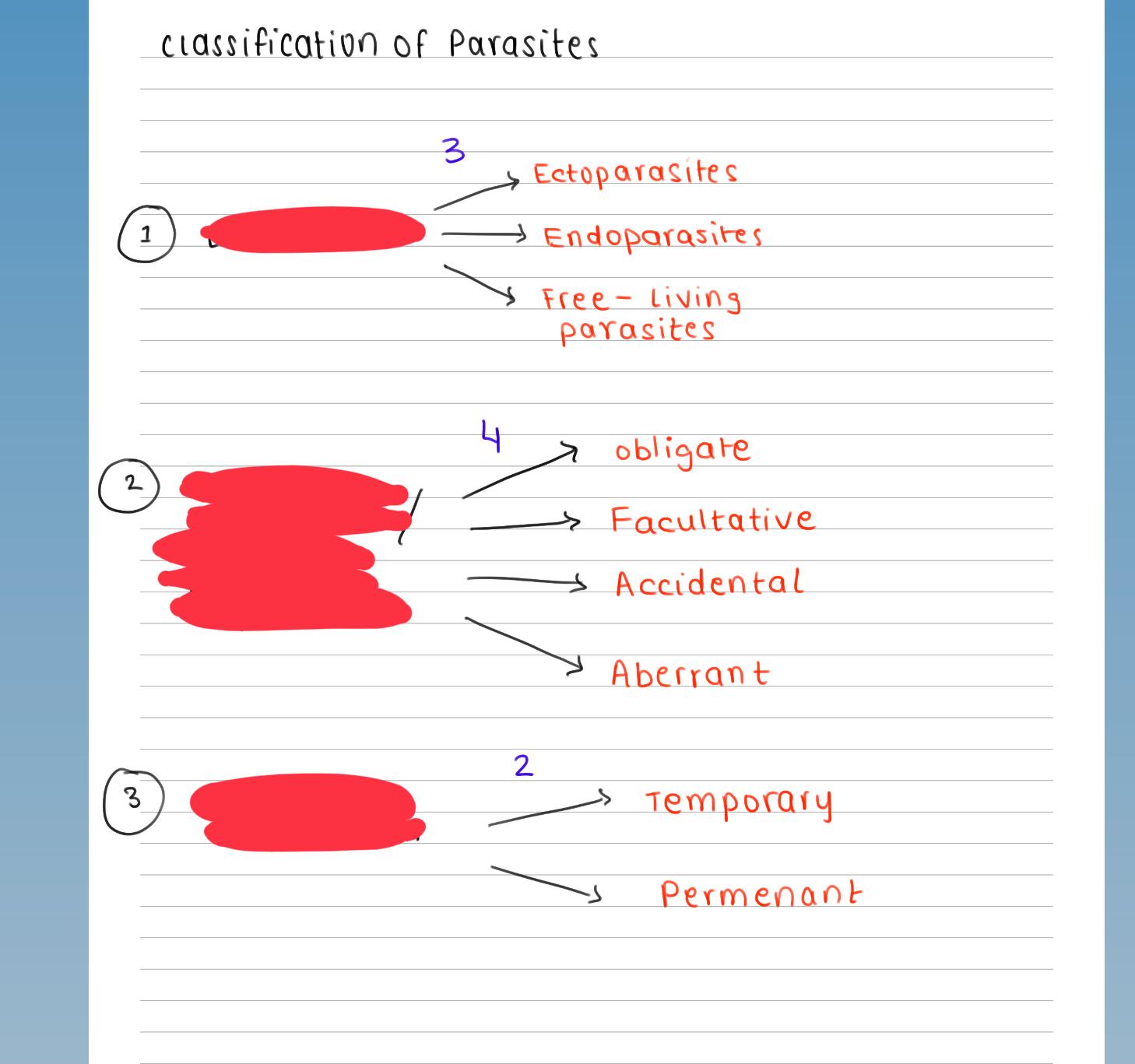
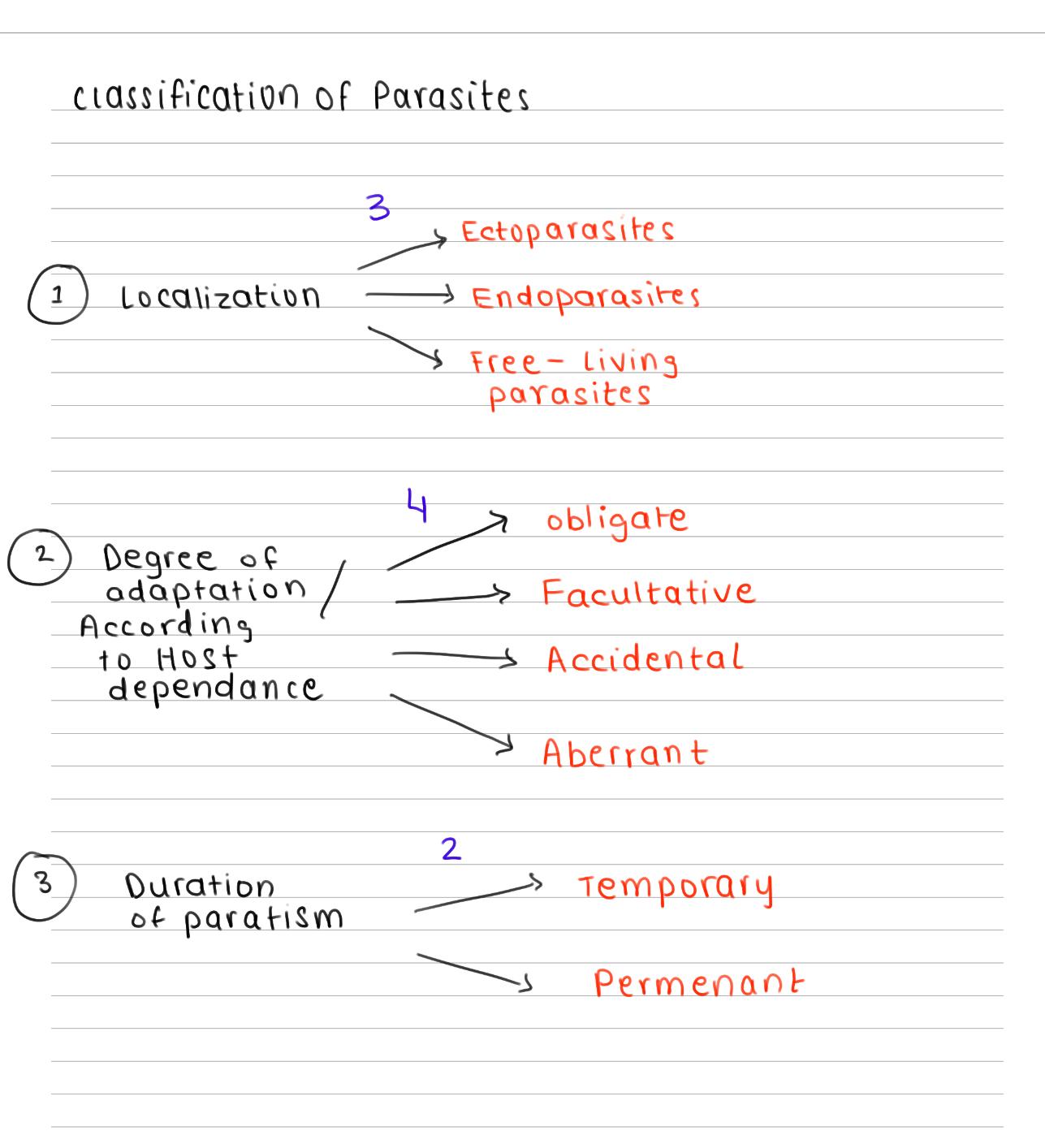
Ectoparasite
Parasite inhabits body surface of host
Doesn’t penetrate tissue
e.g. Fleas
Endoparasite
Parasite lives within body of host
e.g. Giardia lamblia, hookworm
Free living parasites
Parasites that hv non-parasitic stages of active existence
Can live independently of host
• E.g. fleas, lice
Obligate parasite
Cannot live without host
E.g. Toxoplasma gondii, Plasmodium
Facultative parasite
Live in parasitic form or free-living form
E.g. Candida, naegleria fowleri
Accidental parasites
Parasitize an organism other than usual host
E.g. Heartworms, crablouse
Aberrant parasite
live in contact with the host for only a part of their cycle or occasionally at the time of feeding
E.g. Multilocular cyst, Toxocara
Temporary parasite
live in contact with the host for only a part of their cycle or occasionally at the time of feeding
E.g. mosquitoes/bedbugs
Permanent parasite
Remains on/in body of host from early life until maturity
E.g. headlice
Life cycle of Parasites
simple or complicated
with multiple morphological forms and developmental stages
Direct life cycle
parasite requires only a single host to complete development
Indirect life cycle
parasite requires 2 or more host species to complete development
What are the modes of transmission
Oral (per os)
Skin
Vector
Direct
Vertical
Latrogenic
Effects of parasite on host
Tissue necrosis
Trauma & physical obstruction
Allergic reaction
Inflammatory reaction
Nutritive effect
Cancerogenic effect
SUBPHYLUM SARCODINA.
a. Genus Entamoeba —> 3
i. Entamoeba histolytica
ii. Entamoeba coli
iii. Entamoeba gingivalis
PHYLUM CILIOPHORA
a. Genus Balantidium —> 1
i. Balantidium coli
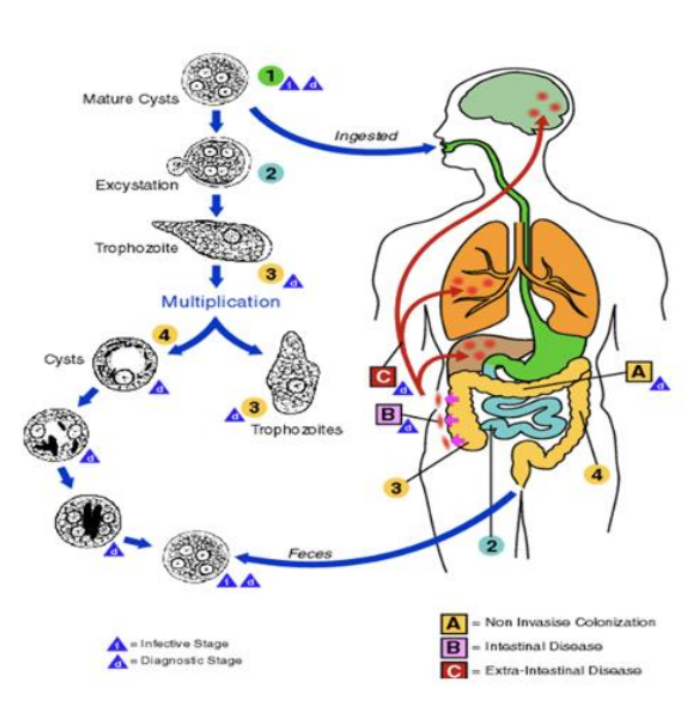
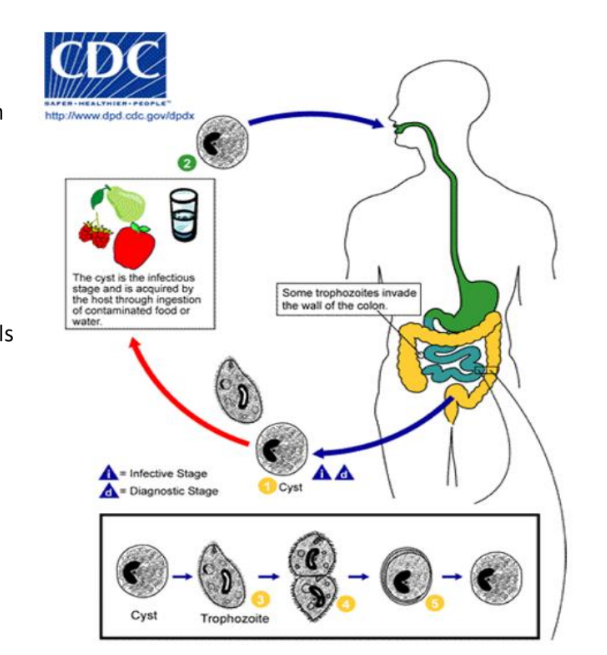
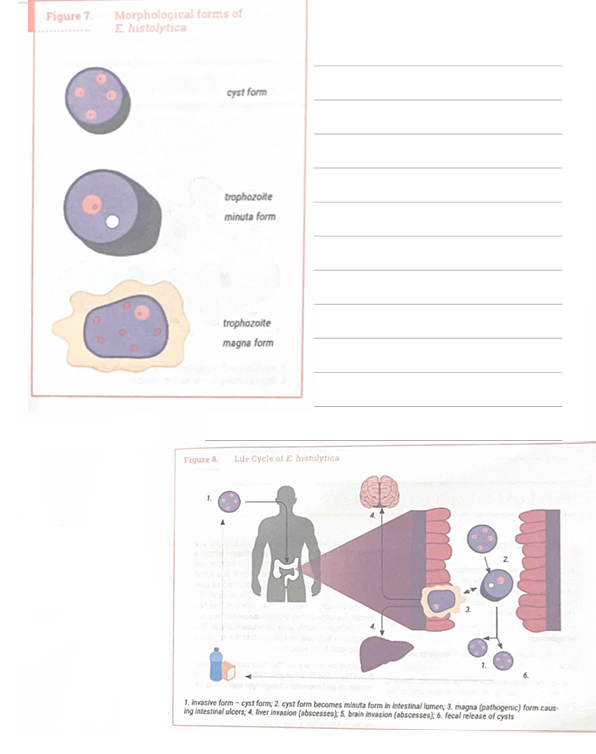
What is the life cycle of Entamoeba Histolytica
Mature quadrinucleated cells are ingested from contaminated food (per os). This passes from stomach to small intestine
This then travels to the stomach but the cysts have a protective barrier that prevents its coating from being broken down
The cysts then travel to the small intestine and the protective coating gets broken down by digestive enzymes (in small intestine). This process is called excystation
This releases trophozoites (which are the pathogenic form) which are carried to the caecum.
The best habitat for them is the caecal mucosa, where they lodge into glandular cysts and undergo binary fission
Some trophozoites then become pathogenic “forma magma” which invades the submucosal layer/intestinal wall destroying tissue and forming ulcers
They can also enter the blood stream, causing abscesses in the liver, lungs and brain
What is the life cycle of Entamoeba coli
First, cysts (invasive form) originate from animal reservoirs or human carriers. Examples include pig feces, polluted water or direct contact with infected animals/humans
Humans ingest cysts (invasive form) from contaminated food or water
Excystation occurs in small intestine and cyst walls breaks due to digestive enzymes. This releases trophozoites which travel to the large intestine
The trophozoites feed on the intestinal contents and multiply thru binary fission
Trophozoites typically remain as commensals (harmless presence), but in some cases they invade the mucosa leading to inflammation and ulcers
But trophozoites can also penetrate the intestinal wall and cause ulcers, diarrhea, abdominal pain and weight loss.
Some trophozoites form cysts, which are excreted in feces. These survive in the environment + infect new hosts
Draw Entamoeba Histolylica in its different forms
Draw an entamoeba coli
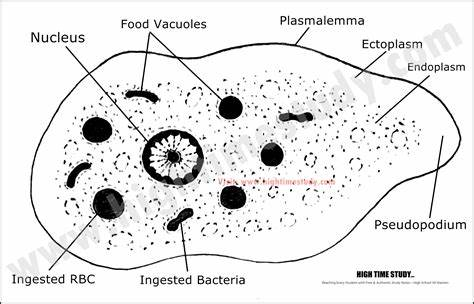
Entamoeba gingivalis localization, characteristics and transmission ?
It is found in oral cavity, transmission via oral cavity
Trophozoites are transmitted thru saliva
They colonize gingival tissues and feed on bacteria, WBCs and epithelial cells (lining of the gums)
They multiply by binary fission
They spread through oral contact (kissing, sharing utensils etc.)
They ONLY exist as a trophozoite, no cyst stage
Trophozoites are 10-20 micrometers, mobile w. multiple pseudopodia
Their cytoplasm has food vacuoles w. ingested bacteria, leucocytes and epithelial cells
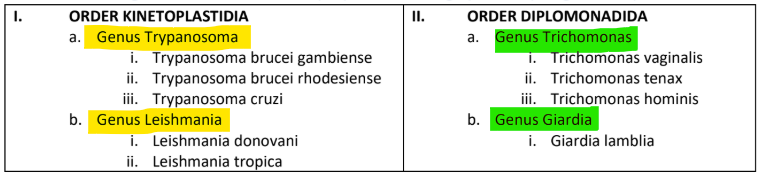
ORDER KINETOPLASTIDIA VS ORDER DIPLOMONADIDA
Order KINETOPLASTIDIA
Genus Trypanosoma
i. Trypanosoma brucei gambiense
ii. Trypanosoma brucei rhodesiense
iii. Trypanosoma cruzi
Genus Leishamania
i. Leishmania donovani
ii. Leishmania tropica
Order DIPLOMONADIDA
Genus Trichomonas
i. Trichomonas vaginalis
ii. Trichomonas tenax
iii. Trichomonas hominis
Genus Giardia
i. Giardia lamblia
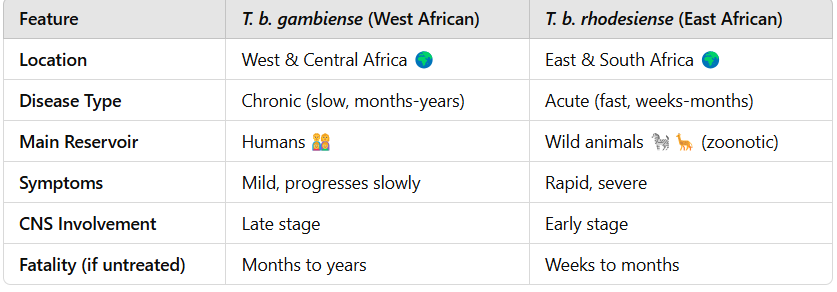
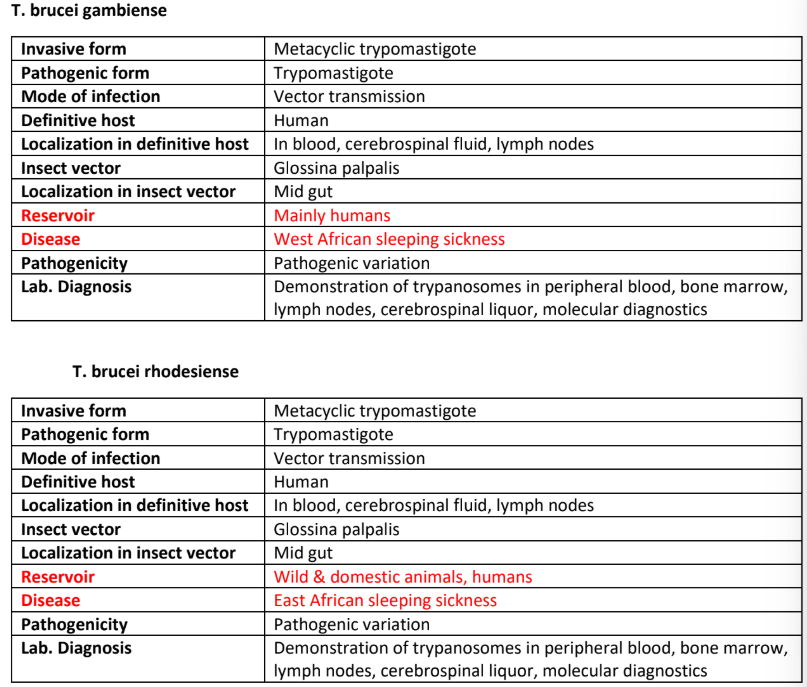
What is the lifecycle for Trypanosoma brucei (gambiense and rhodesiense)? —> SLEEPING SICKNESS
Vector Tsetse fly bites and injects metacyclic trypomastigotes (infective form) into human blood. These parasites enter the bloodstream + tissues
The metacyclic trypomastigotes transform into bloodstream trypomastigotes and they multiply in body fluids (blood lymph, cerebrospinal fluid) by binary fission
The bloodstream trypomastigotes spread to different organs
When another tsetse fly bites an infected person, it ingests bloodstream trypomastigotes
Inside the fly, parasite undergoes several transformations
Trypomastigotes → Procyclic Trypomastigotes in the midgut (multiply by binary fission).
Procyclic Trypomastigotes migrate to the salivary glands, transforming into epimastigotes.
Epimastigotes multiply and fill the glands, eventually becoming metacyclic trypomastigotes (infective stage).
Now when infected tsetse fly bites new human, it injects metacyclic trypomastigotes, continuing the cycle
What are the symptoms of T. b. gambiense & T. b. rhodesiense
🧠 "G for Gambiense = Grows Slowly" (Chronic)
🧠 "R for Rhodesiense = Rapid Death" (Acute & Severe)

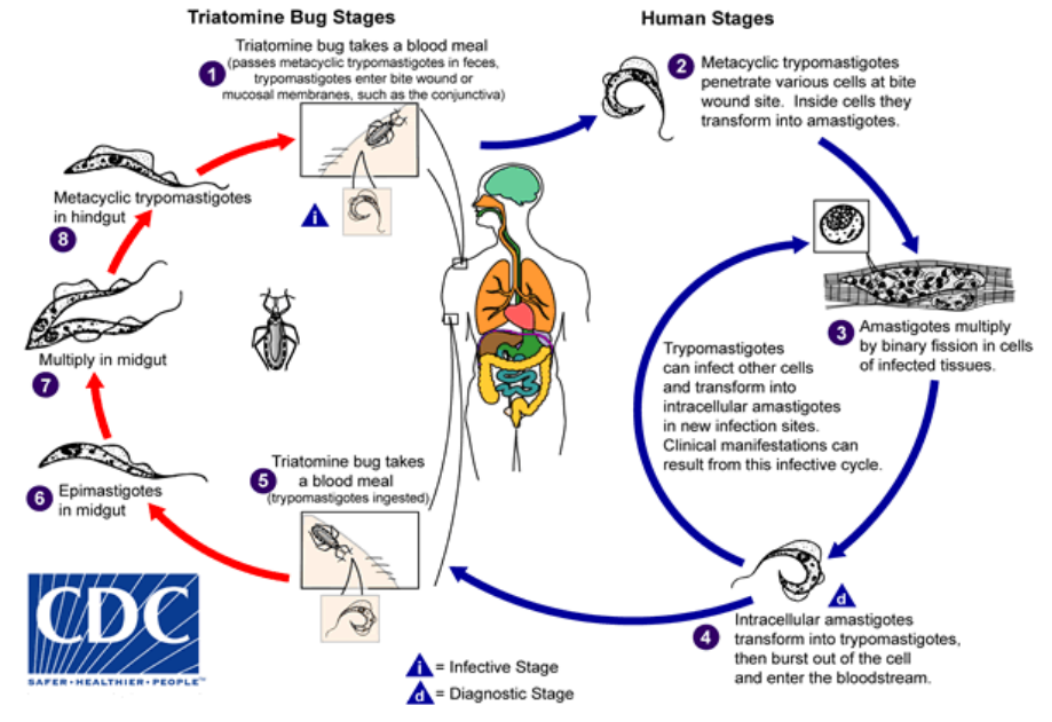
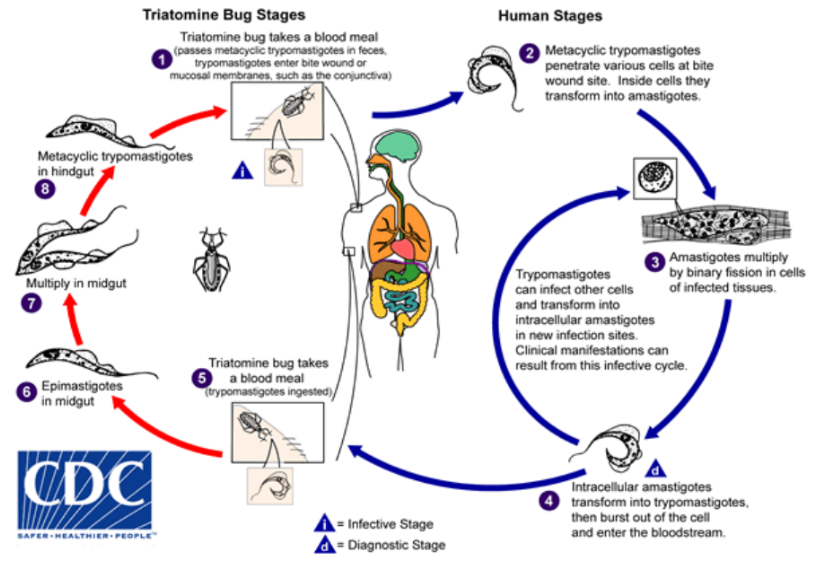
What is the lifecycle for Trypanosoma cruzi? (CHAGAS disease)
Vector Triatomine bug (kissing bug) bites and defecates near bite
Feces contain metacyclic trypomastigotes (infective stage). The parasites enter the body through bite wound (scratched in) or mucosal membranes (eye, mouth, etc.)
This causes local inflammation (chagoma)
The metacyclic trypomastigotes invade cells at the infection site
Inside cells, they transform into amastigotes (replicating from) which multiply by binary fission and eventually burst out of cells transforming into trypomastigotes which enter the bloodstream.
Another Triatomine bug bites the infected person, ingesting trypomastigotes. The infected bug defecates near its next bite wound, spreading the parasite.
The cycle continues.
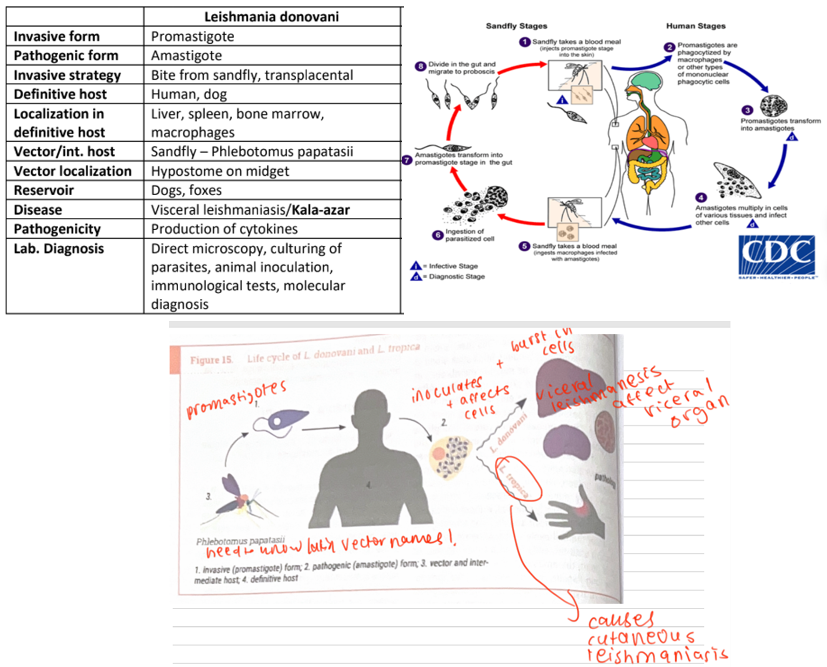
What is the lifecycle for Leishmania donovani (Kala-azar) AND Leishmania Tropica ?
The sandfly (PLEBOTOMUS PAPATASII) injects promastigotes through human skin, which travel into blood stream
Macrophages ingest (phagocytose) promastigotes, but instead of killing them, the parasite survives
Inside macrophages, promastigotes transform into amastigotes (intracellular stage)
Amastigotes divide inside macrophages, macrophages burst releasing new amastigotes which infect other macrophages
Another sandfly bites the infected person and ingests macrophages containing the amastigotes
Inside the sandfly’s gut, amastigotes change back into promastigotes
They multiply in the sandfly’s midgut and move to its proboscis (feeding organ)
The infected sandfly bites another human, injecting promastigotes into skin and the cycle repeats
What are the 3 genus names of the order Trichomonas and their localizations?
• T. vaginalis – vagina & uterine cervix in females
• T. tenax – oral cavity
• T. hominis – caecum
What are some morphological characteristics of Trichomonas sp.
No cystic stage
Pear shaped
4 anterior flagella and the 5th one running along the undulating membrane and axostyle
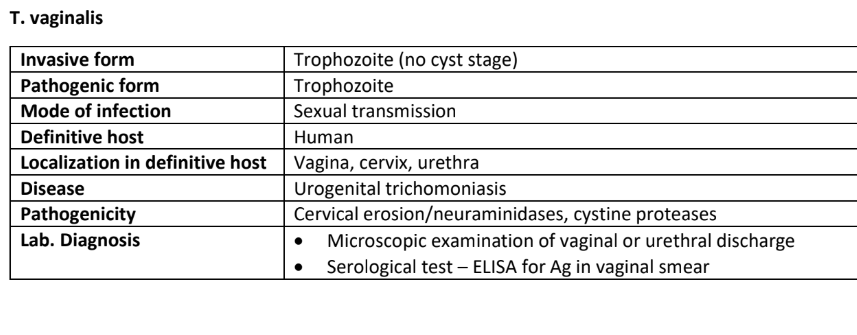
What is the lifecycle for Trichomonas vaginalis?
Trophozoite in vaginal, prostatic secretions and urine
Trophozoite reproduces by longitudinal binary fission
Spread through sexual intercourse (no intermediate host)
Trophozoites move to the vagina or urethra of new host
The disease name is Trichomoniasis
What are the symptoms of Trichomonas vaginalis?
Foul smelling, yellow-green vaginal discharge
Itching, burning and painful urination (dysuria)
Strawberry cervix
Men —> Often asymptomatic but may cause mild symptoms
Increased risk of HIV transmission (due to inflammation)
Infertility in both sexes
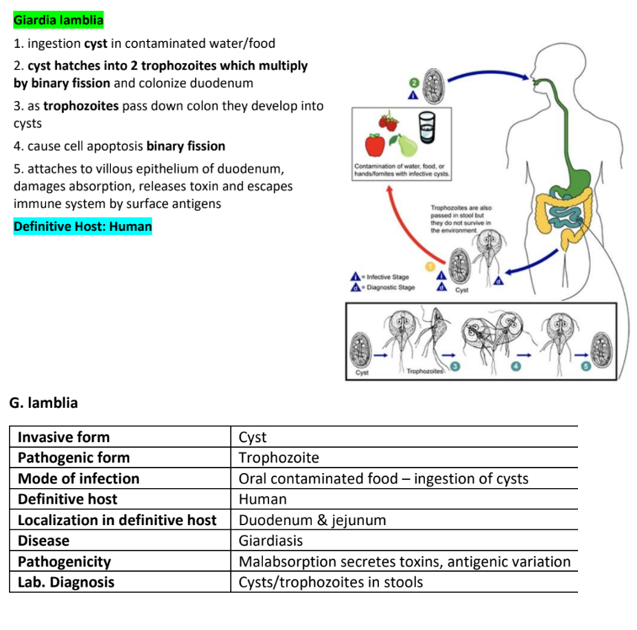
What is the life cycle of Giardia Lamblia?
Injection of cyst from contaminated water, food or surfaces (Common in areas w. poor sanitation)
Excystation occurs in small intestine which hatch into 2 trophozoites
The trophozoites multiply by binary fission and colonize the duodenum
As trophozoites move to the large intestine, they encyst again to survive outside the body
Trophozoites attach to the villous epithelium of the small intestine
They damage absorption, release toxins and cause diarrhea
Cysts are excreted in feces and can survive in the environment.
Trophozoite can also be excreted but do not survive outside the body
What’s the name of the disease caused by Giardia Lamblia?
Giardiasis
What are the symptoms of Giardia Lamblia?
Watery foul-smelling diarrhea
Malabsorption —> weight loss, fatty stools (steatorrhea)
No blood in stool (non invasive)
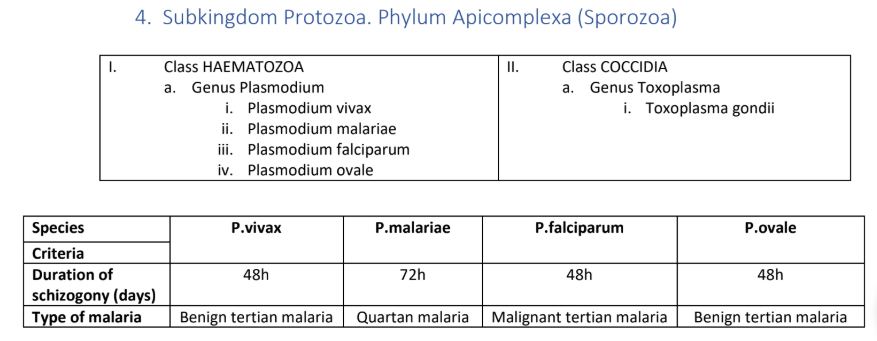
For Class Haematozoa, Genus Plasmodium, what are the 4 diff. types of plasmodiums
i. Plasmodium vivax
ii. Plasmodium malariae
iii. Plasmodium falciparum
iv. Plasmodium ovale

Class Coccidia, Genus Toxoplasma, what is the name of the parasite?
Toxoplasma gondii
Plasmodium Vivax
The definitive host, Female anopheles mosquito injects sporozoites (localised in their salivary glands) into the bloodstream of the intermediate host human
The invasive form, Sporozoites travel to the liver within minutes
Liver Stage
The sporozoites invade hepatocytes
Schizonts form —> divide and release merozoites
P. vivax & P. ovale ONLY: Some sporozoites become hypnozoites, which can stay dormant in the liver and reactivate later, causing relapses.
Blood Stage
The merozoites (pathogenic form) invade RBCs and become Ring Form trophozoite
Ring Form → Amoeboid Form → Mature Trophozoite.
Mature Schizonts develop, burst RBCs, releasing more merozoites → infect new RBCs.
This cycle repeats every 48 hours, causing fever spikes (tertian malaria).
Sexual stage
Some merozoites turn into gametocytes (male: microgametocytes, female: macrogametocytes).
These do not cause symptoms but wait for a mosquito to ingest them.
Mosquito Stage (Sporogony)
Mosquito takes a blood meal, ingesting gametocytes.
Male microgametocyte produces 8 flagellated microgametes.
Female macrogamete fuses with a microgamete → zygote.
Zygote elongates into a motile ookinete, which penetrates the mosquito’s stomach wall.
Oocyst forms and undergoes division, releasing sporozoites.
Sporozoites migrate to the mosquito’s salivary glands → ready to infect a new human host.
Definitive Host: Mosquito (where sexual reproduction occurs).
Intermediate Host: Human (where asexual reproduction occurs).
Disease: Tertian Malaria (fever every 48 hrs).
Key Feature: Relapses due to hypnozoites in the liver.
Destruction of erythrocytes
• Releasing of cellular components
• Hemolysis – anemia, antigenic variation
Lab. diagnosis • Different stages of parasite (trophozoites, schizonts, and
gametocytes) demonstrated in blood
• PCR
• ELISA
Symptoms:
Cyclic fevers & chills (tertian fever).
Anemia (due to RBC destruction).
Splenomegaly (enlarged spleen).
Diagnosis: Blood smear (Ring Form, Schizonts, Enlarged RBCs with Schüffner’s Dots).
Treatment:
Chloroquine (for blood stages).
Primaquine (for hypnozoites in liver, to prevent relapse).
2 types of merozoites, one affects liver one effects RBCs
Bradizotes = slow parasites
Tachizotes go to RBCs n interact w receptor on RBCs, first recognition occurs, erythrocytes engulf parasites (vaculoe inside). This is first stage of endo - Ex aka. ring trophozoite
The parasites then start to produce pseudopodia,
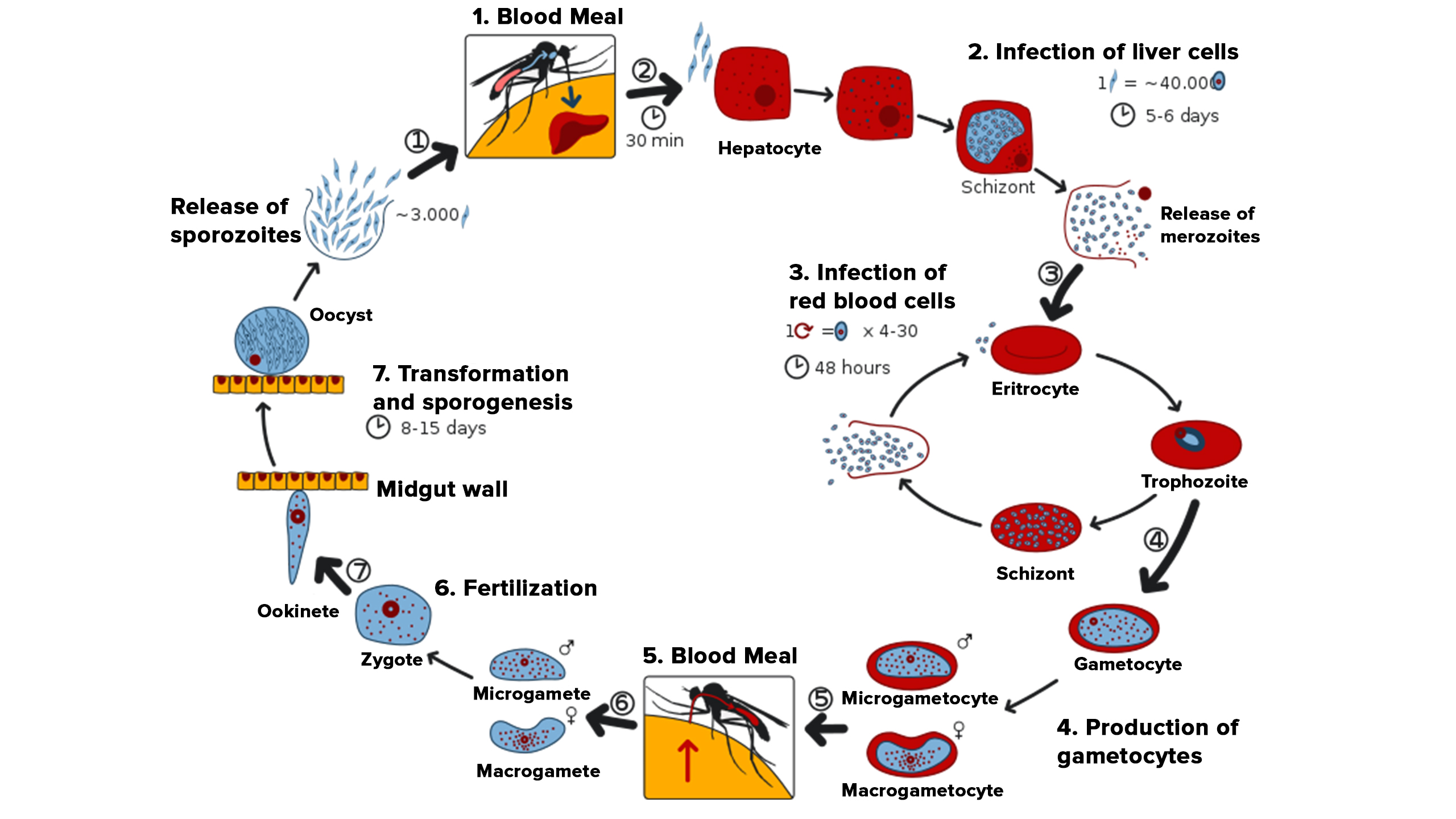
Plasmodium Vivax
Asexual Phase (Schizogony) – In Humans 🔹 Pre-Erythrocytic Schizogony (Liver Stage)
Sporozoites enter the bloodstream when an infected mosquito bites.
They travel to the liver and infect hepatocytes.
Inside hepatocytes, they transform into schizonts, which undergo multiple rounds of division.
In P. vivax (and P. ovale), some sporozoites become hypnozoites (dormant stage) and remain in the liver for months/years before reactivating.
Schizonts rupture, releasing merozoites into the blood.
Endoerythrocytic Schizogony (Blood Stage – RBC Infection) 🔴
Merozoites invade red blood cells (RBCs) and undergo the following transformations:
Ring Form (Immature Trophozoite): Small, with a vacuole and nucleus at one pole.
Amoeboid Form (Mature Trophozoite): Enlarged, irregular shape, showing motility.
Schizont: Undergoes nuclear division, forming many merozoites.
Schizont bursts, releasing merozoites → Invade new RBCs and repeat the cycle.
This RBC destruction causes fever cycles (tertian fever, every 48 hours).
Sexual Phase (Gametogony) – In Humans & Mosquitoes 🔹 Gametocyte Formation (In Humans)
After multiple rounds of RBC infection, some merozoites differentiate into gametocytes:
Macrogametocytes (Female) – Larger
Microgametocytes (Male) – Smaller
Gametocytes remain in the blood and wait to be ingested by a mosquito.
🔹 Mosquito Stage (Sporogony – Sexual Reproduction)
When an Anopheles mosquito bites an infected human, it ingests gametocytes.
Microgametocyte (Male) produces 8 motile microgametes (Exflagellation).
Macrogametocyte (Female) matures into a macrogamete.
Fertilization occurs → Forms Zygote.
Zygote elongates into a motile ookinete → Penetrates mosquito’s stomach wall.
Ookinete transforms into an oocyst, which matures and releases sporozoites.
Sporozoites travel to the mosquito’s salivary glands → Mosquito becomes infective.
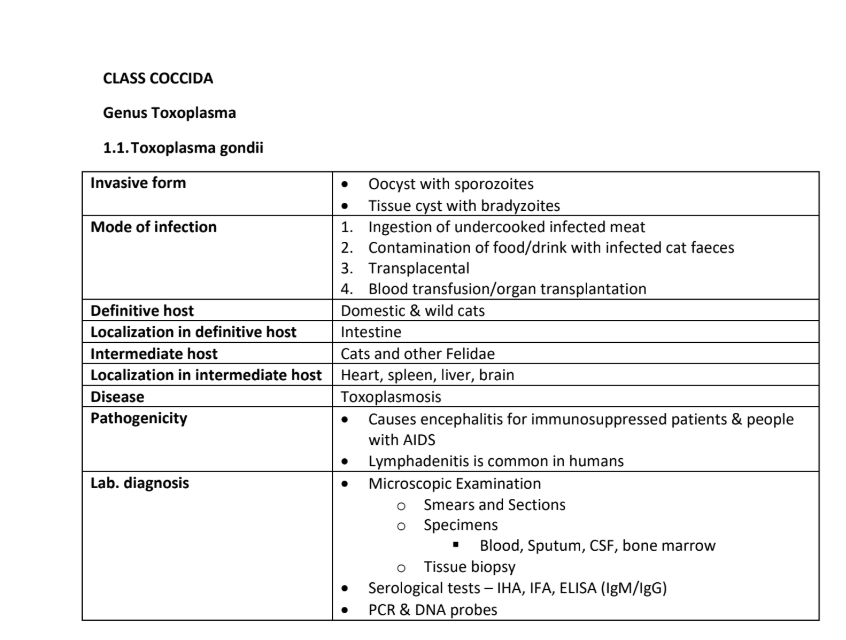
Life cycle Toxoplasma gondii
Definitive host Cats - The Starting Point
Sexual reproduction (schizogony & gametogony) in cat’s small intestine → produces oocysts.
Oocysts are shed in feces and contaminate soil, water, food.
Environmental & Intermediate Host Infection
Oocysts mature in soil/water and become infective.
New hosts/ Intermediate host (humans, pigs, sheep, rodents) ingest oocysts from contaminated food, water, or surfaces.
Oocysts release sporozoites → invade epithelial cells + host cell ruptures releasing trophozoites in blood n lymph
transform into tachyzoites/ chronic tissue cysts produces within muscles and tissues .
Tissue Cysts & Reinfection
Tachyzoites spread via blood & lymph, infecting organs.
Acute phase: Active infection (esp. dangerous in pregnancy or weak immunity).
Chronic phase: Tachyzoites → bradyzoites (slow-growing form) inside tissue cysts (muscles, brain).
If another animal eats infected tissue (e.g., a mouse eaten by a cat, or humans eating undercooked meat), the cycle repeats.
Cats get infected again → new oocysts shed in feces → cycle continues.
Key Ways Humans Get Infected
✔ Ingesting oocysts (contaminated food, water, unwashed veggies, cat litter).
✔ Eating undercooked infected meat (pork, lamb, etc.).
✔ Mother-to-baby transmission (congenital toxoplasmosis).
✔ Blood transfusion/organ transplant (rare cases).
Disease name: TOXOPLASMOSIS
Lab. diagnosis • Microscopic Examination
Smears and Sections
Specimens
Blood, Sputum, CSF, bone marrow
Tissue biopsy
Serological tests – IHA, IFA, ELISA (IgM/IgG)
PCR & DNA probes
Class Trematoda (Flukes), Genus Fasciola, Discrocoelium, Opisthorchis, what is the name of the parasites ?
1. Genus Fasciola
Fasciola hepatica
2. Genus Dicrocoelium
.Dicrocoelium dendriticum
3. Genus Opisthorchis
Opisthorchis felineus
Class Trematoda (Flukes), Genus Schistoma, What are the 3 parasites?
Schistoma haematobium
Schistoma japonicum
Schistoma mansoni
Fasciola hepatica
Definitive Hosts: Humans, Sheep, Cattle
🐌 Intermediate Host: Snail (Lymnaea species)
Life Cycle in 3 Clear Phases
Eggs & Snail Infection (Water Stage)
Unembryonated eggs are shed in feces into water.
In water, eggs develop into embryonated eggs → hatch into miracidia (larvae).
Miracidia penetrate a snail (Lymnae species) and develop through stages:
Sporocyst → First & Second Generation Rediae → Cercariae (infective stage).
In snail, miracidia progress through
sporocyst, first generation rediae, second
generation redia to become cercariae
2. Cercariae to Metacercariae (Water to Plants Stage)
Free-swimming cercariae leave the snail and attach to water plants (e.g., watercress, grass).
They encyst and become metacercariae (dormant, infective form).
3. Infection & Maturation in Host (Animal/Human Stage)
Host ingests contaminated water plants (sheep, cattle, or humans).
Metacercariae hatch in the duodenum, penetrate the intestinal wall, and travel to the liver.
Inside the liver, they mature into adult flukes, feeding on tissue and causing disease (liver rot in animals).
Eggs are laid in bile ducts → passed into feces → cycle repeats.
🛑 Key Ways Humans Get Infected
✔ Eating raw water plants (e.g., watercress, unwashed veggies).
✔ Drinking contaminated water containing metacercariae.

🐑 Definitive Hosts: Cow, Human, Sheep, Goat
🐌 Intermediate Hosts:
Land Snail (Zebrina or Helicella)
Ant
Life Cycle in 3 Clear Phases
Snail Infection & Cercariae Release (Land Stage) 🐌
Embryonated eggs (already containing miracidia) are shed in feces onto land.
Snail ingests eggs → Inside the snail, miracidia hatch and go through:
Sporocyst → 1st Generation Redia → 2nd Generation Redia → Cercariae.
Cercariae are released from the snail via its respiratory pore in slime balls (a protective mucus secretion).
Ant Infection (Second Intermediate Host) 🐜
Ants eat the slime balls containing cercariae.
Inside the ant, cercariae develop into metacercariae (infective stage).
Some metacercariae migrate to the ant’s nervous system, making the ant climb up grass blades at night and latch on → This increases chances of ingestion by grazing animals (sheep, cows, etc.).
3⃣ Host Infection & Maturation (Inside Animal/Human) 🐑👤
Definitive host (sheep, cow, goat, or human) ingests the infected ant.
Metacercariae excyst in the duodenum, travel to the bile ducts and mature into adult flukes.
Adult flukes lay eggs → Passed in feces → Cycle repeats.
🛑 How Humans Get Infected
✔ Accidentally eating infected ants on raw vegetables.
✔ Consuming contaminated food or water.
4 subphyla of Phylum Arthropoda
Trilobitomorpha
Chelicerata (ticks and mites)
Crustacea
Hexapoda (insects)
Complete metamorphosis
Typical of higher insects
Life cycle : Egg—> larva —>pupa —> imago (adult stage)